Search
- Page Path
- HOME > Search
- Usefulness of Charlson comorbidity index-adjusted mortality prediction tools and factors influencing mortality in intensive care unit patients: a retrospective medical record review–based study
- Jai Jung Lee, Dong Yeon Kim, Min Ji Lee, Ji Young Kim
- J Korean Acad Nurs 2026;56(1):27-38. Published online February 11, 2026
- DOI: https://doi.org/10.4040/jkan.25094
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
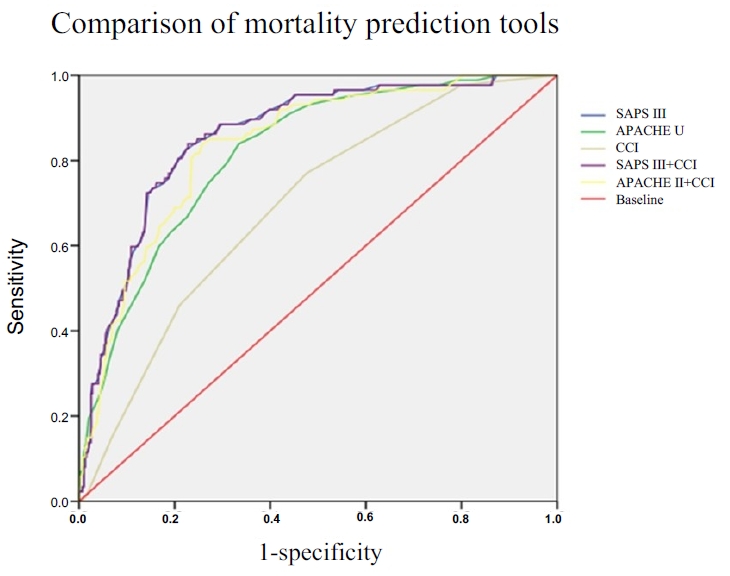
This study aimed to estimate the mortality rate in adult intensive care units (ICUs) using the Charlson comorbidity index (CCI)-adjusted Acute Physiology and Chronic Health Evaluation (APACHE) II and Simplified Acute Physiology Score (SAPS) III models, and to identify factors influencing mortality.
Methods
This retrospective cohort study included adult patients admitted to the ICU at a tertiary hospital between June 1 and August 31, 2022. Among the 1,098 screened patients, those younger than 18 years, those discharged within 48 hours, and those with missing medical records were excluded. In total, 482 patients were analyzed using the chi-square test, independent t-test, and multivariate logistic regression. Model performance was evaluated using the c-statistic and the Hosmer-Lemeshow goodness-of-fit test.
Results
The predictive accuracy of the mortality models was shown by c-statistic values of 0.817 for APACHE II, 0.857 for SAPS III, 0.697 for CCI, and 0.834 for CCI-adjusted APACHE II (0.834). Mechanical ventilation, cardiopulmonary cerebral resuscitation, continuous renal replacement therapy, and the presence of leukemia or lymphoma were significant predictors of mortality in adult ICU patients. Among the evaluated models, SAPS III and CCI-adjusted APACHE II demonstrated the highest predictive power.
Conclusion
The findings indicate that incorporating comorbidity indices such as the CCI with acute physiological parameters improves the accuracy of mortality prediction in ICU patients. Understanding mortality prediction models is essential for nurses to provide individualized, evidence-based, and high-quality care in adult ICUs.
- 233 View
- 8 Download

- Effectiveness of the Eye Care Protocol in the Intensive Care Unit Patients: A Randomized Controlled Trial
- Kyu Won Lim, Shin Young Ha, In Soon Kang
- J Korean Acad Nurs 2024;54(3):432-445. Published online August 31, 2024
- DOI: https://doi.org/10.4040/jkan.24017
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study investigated the effects of an eye care protocol (ECP) on patients in the intensive care unit (ICU).
Methods
This study utilized a randomized controlled design. Participants were patients who met the inclusion criteria and were admitted to the ICU (36 in the experimental group and 38 in the control group). The experimental group received an ECP, while the control group received standard eye care, starting the day after admission, for a duration of 10 days. The ECP classifies the degree of eyelid obstruction into three stages based on the degree of exposure to the lower eyelid conjunctiva and cornea. The protocol included cleansing with normal saline gauze, administering eye drops, applying silicone and polyurethane films, and recommending consultation with an ophthalmologist if necessary. The effectiveness of ECP was assessed by analyzing tear volume, hyperemia, chemosis, and eye discharge. Data analysis was conducted using SPSS 27.0, employing the Mann-Whitney U-test and generalized estimating equations.
Results
On day 5, the experimental group demonstrated a significant increase in tear volume in both eyes compared with the control group. However, no statistically significant differences were observed in the incidence of hyperemia, chemosis, and eye discharge on days 5 and 10 of the intervention.
Conclusion
The application of the ECP in this study increased tear volume in ICU patients, thereby reducing discomfort caused by dry eyes. It has the potential to prevent complications such as damage to the surface of the eyeball resulting from decreased tear volume. -
Citations
Citations to this article as recorded by- A systematic review of pulmonary rehabilitation nursing interventions for patients with chronic obstructive pulmonary disease
Da-Jung Kim
Journal of Exercise Rehabilitation.2025; 21(5): 234. CrossRef
- A systematic review of pulmonary rehabilitation nursing interventions for patients with chronic obstructive pulmonary disease
- 1,408 View
- 199 Download
- 1 Web of Science
- 1 Crossref

- Analysis of ROX Index, ROX-HR Index, and SpO 2 /FIO 2 Ratio in Patients Who Received HighFlow Nasal Cannula Oxygen Therapy in Pediatric Intensive Care Unit
- Sun Hee Choi, Dong Yeon Kim, Byung Yun Song, Yang Sook Yoo
- J Korean Acad Nurs 2023;53(4):468-479. Published online August 31, 2023
- DOI: https://doi.org/10.4040/jkan.22152
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to evaluate the use of the respiratory rate oxygenation (ROX) index, ROX-heart rate (ROX-HR) index, and saturation of percutaneous oxygen/fraction of inspired oxygen ratio (SF ratio) to predict weaning from high-flow nasal cannula (HFNC) in patients with respiratory distress in a pediatric intensive care unit.
Methods
A total of 107 children admitted to the pediatric intensive care unit were enrolled in the study between January 1, 2017, and December 31, 2021. Data on clinical and personal information, ROX index, ROX-HR index, and SF ratio were collected from nursing records. The data were analyzed using an independent t-test, χ2 test, Mann–Whitney U test, and area under the curve (AUC).
Results
Seventy-five (70.1%) patients were successfully weaned from HFNC, while 32 (29.9%) failed. Considering specificity and sensitivity, the optimal cut off points for predicting treatment success and failure of HFNC oxygen therapy were 6.88 and 10.16 (ROX index), 5.23 and 8.61 (ROX-HR index), and 198.75 and 353.15 (SF ratio), respectively. The measurement of time showed that the most significant AUC was 1 hour before HFNC interruption.
Conclusion
The ROX index, ROX-HR index, and SF ratio appear to be promising tools for the early prediction of treatment success or failure in patients initiated on HFNC for acute hypoxemic respiratory failure. Nurses caring for critically ill pediatric patients should closely observe and periodically check their breathing patterns. It is important to continuously monitor three indexes to ensure that ventilation assistance therapy is started at the right time. -
Citations
Citations to this article as recorded by- Non-invasive SpO2/FiO2 ratio (SFR) as surrogate for PaO2/FiO2 ratio (PFR): A scoping review
Madhura Reddy, Malavika Kulkarni, Sushma Thimmaiah Kanakalakshmi, Laxmi Shenoy, Rama Rani KrishnaBhat
The Journal of Critical Care Medicine.2025; 11(3): 221. CrossRef - Can the ROX index predict high‐flow nasal cannula failure in children under 2 with lower respiratory tract infection?
Pablo Vasquez‐Hoyos, Alvaro L. Jacome‐Orozco, Andrea P. Rodriguez‐Mayorga, Leidy E. Sepulveda‐Forero, Diana P. Escobar‐Serna, Juan S. Barajas, Evelyn Obando‐Belalcazar, Claudia M. Salinas‐Jaimes, Juan J. Peralta‐Palmezano, Alexandra Jimenez‐Chavez, Rafael
Pediatric Pulmonology.2024; 59(5): 1246. CrossRef - Impact of Surgical Mask Placement Over High-Flow Nasal Cannula on Oxygenation Parameters in COVID-19 Patients Experiencing Hypoxemic Respiratory Failure
Aadila Coatwala, Mayank Dhir, Sagar Sinha, Dattatray Bhusare
Cureus.2024;[Epub] CrossRef
- Non-invasive SpO2/FiO2 ratio (SFR) as surrogate for PaO2/FiO2 ratio (PFR): A scoping review
- 5,796 View
- 166 Download
- 2 Web of Science
- 3 Crossref

- Delirium Experience of the Intensive Care Unit Patients
- Jaeyeon Jung, Sujin Jang, Seonmi Jo, Sunhee Lee
- J Korean Acad Nurs 2022;52(2):134-143. Published online April 30, 2022
- DOI: https://doi.org/10.4040/jkan.21240
-
 Abstract
Abstract
 PDF
PDF - Purpose
The study aimed to understand the delirium experience of intensive care unit (ICU) patients.
Methods
We performed a qualitative study using Colaizzi’s phenomenological method. Eleven patients, who experienced delirium according to the Confusion Assessment Method for ICU, participated after transferring to general wards from the ICU. Individual in-depth semi-structured interviews ranging from 30 minutes to 2 hours in length were conducted between November 2018 and August 2019.
Results
Nine themes and four theme clusters emerged. The four theme clusters were: 1) “Overwhelmed by fear,” which describes the experience of a patient close to death and the feeling of difficulty in understanding disorganized thinking; 2) “Anxious about not understanding the situation,” which means that patients’ sense of time and space were disordered in the ICU; 3) “Being deserted,” which indicates the feeling of being separated from others and yourself; and 4) “Resistance to protect my dignity,” which indicates that the dignity and autonomy of an individual in the patient’s position at the ICU, are ignored.
Conclusion
Nursing interventions are needed that would enable patients to maintain orientation and self-esteem in the ICU. In addition, healthcare providers need to provide information about the unfamiliar environment in the ICU in advance. -
Citations
Citations to this article as recorded by- Patients' and family members' dyadic experience of post‐operative delirium in the intensive care unit: A qualitative study
Jing Dong, Weijing Sui, Yiyu Zhuang
Nursing in Critical Care.2025;[Epub] CrossRef - Association Between Person-centered Care, Intensive Care Experience, and Post-intensive Care Syndrome in Critical Care Survivors: A Multi-center Prospective Cohort Study
Jiyeon Kang, Seonyoung Yun
Asian Nursing Research.2025; 19(3): 274. CrossRef - Factors Influencing Intensive Care Unit Nurses’ Competency in Delirium Care in A Tertiary General Hospital
Mi Ran Lim, Gyoo Yeong Cho
Journal of Korean Critical Care Nursing.2024; 17(3): 37. CrossRef - Exploring patients’ and families’ preferences for auditory stimulation in ICU delirium prevention: A qualitative study
Yajun Ma, Nianqi Cui, Zhiting Guo, Yuping Zhang, Jingfen Jin
Intensive and Critical Care Nursing.2024; 82: 103629. CrossRef - The Influence of Ethical Nursing Competence and Positive Nursing Organizational Culture on Person-Centered Care in Intensive Care Unit Nurses: A Cross-Sectional Survey
Jae Eun Lee, Hye-Young Jang
Journal of Korean Academy of Fundamentals of Nursing.2024; 31(3): 304. CrossRef - A Study on Nurses' Communication Experiences with Intubation Patients
Ye Rim Kim, Hye Ree Park, Mee Kyung Shin
The Korean Journal of Rehabilitation Nursing.2023; 26(1): 28. CrossRef - Intensive Care Experience of Critical Care Patients and Its Related Factors : A Secondary Analysis Study
Jiyeon Kang, Hyojeong Woo
Journal of Korean Critical Care Nursing.2023; 16(3): 11. CrossRef - Item analysis of the Korean version of the Intensive Care Experience Questionnaire: Using the Rasch Model based on Item Response Theory
Jiyeon Kang, Minhui Kim
Journal of Korean Critical Care Nursing.2022; 15(3): 37. CrossRef
- Patients' and family members' dyadic experience of post‐operative delirium in the intensive care unit: A qualitative study
- 2,788 View
- 175 Download
- 3 Web of Science
- 8 Crossref

- Untact Visit Service Development Based on an Application Reflecting the Circumstances during COVID-19: Focusing on Utilization in the Pediatric Intensive Care Units
- Dahae Woo, Hanui Yu, Hyo Jin Kim, Minyoung Choi, Dong Hee Kim
- J Korean Acad Nurs 2021;51(5):573-584. Published online October 31, 2021
- DOI: https://doi.org/10.4040/jkan.21143
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to develop an untact visit service based on an application that can be utilized in the pediatric intensive care unit (PICU) during COVID-19.
Methods
This study adopted the double diamond process of service design comprising the discovery, defining, and development stages.
Results
We developed an untact visit service based on an application that considered the child’s status, schedule, photo, and video messages, and so on. Moreover, we derived a service flow regarding the required roles and the type of flow shown between each stakeholder.
Conclusion
Considering the ongoing pandemic, the untact visit service is designed to increase rapport and participation of parents, share the child’s information in real-time, and provide one-stop service without increasing healthcare providers’ work. It will be a useful visit service that can be applied and evaluated in various hospital settings and the PICU. -
Citations
Citations to this article as recorded by- Factors affecting pediatric nurses’ development of partnerships with parents of hospitalized children: An evaluation based on the stress-coping adaptation model
In Young Cho, So Hyoung Hong, Ji Yeong Yun
Journal of Child Health Care.2025; 29(1): 53. CrossRef - Correlation between oral health knowledge, demand for remote education tools, and self-efficacy among parents of children and adolescents
Min-Ji Park, Herry Novrinda, Jae-Young Lee
Journal of Korean Society of Dental Hygiene.2025; 25(1): 69. CrossRef - Development and Effects of a Family-centered Care Application for Intensive Care Unit Families Based on the Facilitated Sensemaking Model : Focusing on Family Satisfaction, Family Stress, and Self-Efficacy
Yun Ha Oak, Eun Ha Kim
Journal of Korean Critical Care Nursing.2025; 18(2): 1. CrossRef - Experiences of Family Members With Visitation Prohibition for Critically Ill Patients
Sunjung Kim, Sunghee H. Tak
Western Journal of Nursing Research.2024; 46(11): 854. CrossRef - Factors influencing neonatal intensive care unit nurses' parent partnership development
Eun Kyoung Kim, In Young Cho, Ji Yeong Yun, Bobae Park
Journal of Pediatric Nursing.2023; 68: e27. CrossRef - National Petition Analysis Related to Nursing: Text Network Analysis and Topic Modeling
HyunJung Ko, Seok Hee Jeong, Eun Jee Lee, Hee Sun Kim
Journal of Korean Academy of Nursing.2023; 53(6): 635. CrossRef - Relationship between parental stress and post‐traumatic stress disorder: The moderating effect of visitation restrictions in paediatric intensive care units during COVID‐19
Young Il Cho, Hyo Jin Kim, Dong Hee Kim
Nursing in Critical Care.2023; 28(5): 808. CrossRef - Need for Information and Communication Technology during COVID-19: An Exploratory Study Using Nurses’ Activity Diaries
Hyeongsuk Lee, Dongmin Lee, Seungmin Lee
Healthcare Informatics Research.2023; 29(3): 256. CrossRef - Effects of a Noncontact Visit Program in the NICU for the Prevention of COVID-19
Hye Young Ahn, Hee Jee Jo, Hyun Jeong Ko
Healthcare.2023; 11(15): 2152. CrossRef - The Development of Automated Personalized Self-Care (APSC) Program for Patients with Type 2 Diabetes Mellitus
Gaeun Park, Haejung Lee, Ah Reum Khang
Journal of Korean Academy of Nursing.2022; 52(5): 535. CrossRef
- Factors affecting pediatric nurses’ development of partnerships with parents of hospitalized children: An evaluation based on the stress-coping adaptation model
- 1,629 View
- 28 Download
- 8 Web of Science
- 10 Crossref

- Effect of Direct Breastfeeding Program for Premature Infants in Neonatal Intensive Care Unit
- Ji Hyun Kang, Hyunmi Son, Shin Yun Byun, Gyumin Han
- J Korean Acad Nurs 2021;51(1):119-132. Published online February 28, 2021
- DOI: https://doi.org/10.4040/jkan.20240
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to identify the effects of a direct breastfeeding program for premature infants in neonatal intensive care units (NICUs).
Methods
This quasi-experimental study was conducted during August 2016 to April 2017. Sixty mothers of premature infants were assigned to the experimental (n = 31) or control groups (n = 29). The program was comprised of breastfeeding education and direct breastfeeding support. The experimental and control groups were provided with education and counseling on breastfeeding at the time of admission and discharge. In the experimental group, the mothers initiated oral feeding with direct breastfeeding and engaged in breastfeeding at least seven times during the NICU stay. The collected data were analyzed by the χ2 -test and repeated measures ANOVA using an SPSS program.
Results
The experimental group showed a higher direct breastfeeding practice rate (χ2 = 19.29, p < .001), breastfeeding continuation rate (χ2 = 3.76, p < .001), and self-efficacy (F = 25.37, p < .001) than the control group except for maternal attachment.
Conclusion
The direct breastfeeding program in the NICU has significant effects on the practice and continuation rate of breastfeeding and breastfeeding self-efficacy. Therefore, this program can be applied in the NICU settings where direct breastfeeding is limited. -
Citations
Citations to this article as recorded by- Exploration of Family-Centered Care in NICUs: A Grounded Theory Methodology
Young Ah Park, YeoJin Im
Qualitative Health Research.2025; 35(10-11): 1231. CrossRef - Fresh Parent’s Own Milk for Preterm Infants: Barriers and Future Opportunities
Carrie-Ellen Briere, Jessica Gomez
Nutrients.2024; 16(3): 362. CrossRef - Development and Effectiveness Evaluation of Comprehensive Mobile-Based, Breastfeeding Promotion Program for Mothers with Gestational Diabetes
Eunju Kwak, Seungmi Park
Journal of Korean Academy of Nursing.2024; 54(2): 224. CrossRef
- Exploration of Family-Centered Care in NICUs: A Grounded Theory Methodology
- 3,167 View
- 168 Download
- 3 Web of Science
- 3 Crossref

- Cut-Off Values of the Post-Intensive Care Syndrome Questionnaire for the Screening of Unplanned Hospital Readmission within One Year
- Jiyeon Kang, Yeon Jin Jeong, Jiwon Hong
- J Korean Acad Nurs 2020;50(6):787-798. Published online December 31, 2020
- DOI: https://doi.org/10.4040/jkan.20233
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to assign weights for subscales and items of the Post-Intensive Care Syndrome questionnaire and suggest optimal cut-off values for screening unplanned hospital readmissions of critical care survivors.
Methods
Seventeen experts participated in an analytic hierarchy process for weight assignment. Participants for cut-off analysis were 240 survivors who had been admitted to intensive care units for more than 48 hours in three cities in Korea. We assessed participants using the 18-item Post-Intensive Care Syndrome questionnaire, generated receiver operating characteristic curves, and analysed cut-off values for unplanned readmission based on sensitivity, specificity, and positive likelihood ratios.
Results
Cognitive, physical, and mental subscale weights were 1.13, 0.95, and 0.92, respectively. Incidence of unplanned readmission was 25.4%. Optimal cut-off values were 23.00 for raw scores and 23.73 for weighted scores (total score 54.00), with an area of under the curve (AUC) of .933 and .929, respectively. There was no significant difference in accuracy for original and weighted scores.
Conclusion
The optimal cut-off value accuracy is excellent for screening of unplanned readmissions. We recommend that nurses use the Post-Intensive Care Syndrome Questionnaire to screen for readmission risk or evaluating relevant interventions for critical care survivors. -
Citations
Citations to this article as recorded by- Cutoff Values for Screening Post-Intensive Care Syndrome Using the Post-Intensive Care Syndrome Questionnaire
Jiwon Hong, Jiyeon Kang
Journal of Clinical Medicine.2025; 14(11): 3897. CrossRef - Translation and validation of the Chinese version of the post-intensive care syndrome questionnaire
Caidie Yang, Hongmei Wu, Chunmei Luo
BMC Nursing.2025;[Epub] CrossRef - Post‐Intensive Care Syndrome in Family: A Concept Analysis
Jiaqi Wen, Zhenjing Hu, Ziwei Li, Yu Liu, Liting Zhang, Chenchen Zhong
Scandinavian Journal of Caring Sciences.2025;[Epub] CrossRef - Post intensive care syndrome: A review of clinical symptoms, evaluation, intervention
Xiaofang He, Yuwei Song, Yuchun Cao, Liying Miao, Bin Zhu
Heliyon.2024; 10(10): e31278. CrossRef - Screening tools for post–intensive care syndrome and post-traumatic symptoms in intensive care unit survivors: A scoping review
Usha Pant, Krooti Vyas, Shaista Meghani, Tanya Park, Colleen M. Norris, Elizabeth Papathanassoglou
Australian Critical Care.2023; 36(5): 863. CrossRef
- Cutoff Values for Screening Post-Intensive Care Syndrome Using the Post-Intensive Care Syndrome Questionnaire
- 2,773 View
- 66 Download
- 5 Web of Science
- 5 Crossref

- Path Analysis for Delirium on Patient Prognosis in Intensive Care Units
- Sunhee Lee, Sun-Mi Lee
- J Korean Acad Nurs 2019;49(6):724-735. Published online December 30, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.6.724
-
 Abstract
Abstract
 PDF
PDF Purpose This study was conducted to investigate relationship between delirium, risk factors on delirium, and patient prognosis based on Donabedian's structure-process-outcome model.
Methods This study utilized a path analysis design. We extracted data from the electronic medical records containing delirium screening data. Each five hundred data in a delirium and a non-delirium group were randomly selected from electronic medical records of medical and surgical intensive care patients. Data were analyzed using SPSS 20 and AMOS 24.
Results In the final model, admission via emergency department (B=.06,
p =.019), age over 65 years (B=.11,p =.001), unconsciousness (B=.18,p =.001), dependent activities (B=.12,p =.001), abnormal vital signs (B=.12,p =.001), pressure ulcer risk (B=.12,p =.001), enteral nutrition (B=.12,p =.001), and use of restraint (B=.30,p =.001) directly affecting delirium accounted for 56.0% of delirium cases. Delirium had a direct effect on hospital mortality (B=.06,p =.038), hospital length of stay (B=5.06,p =.010), and discharge to another facility (not home) (B=.12,p =.001), also risk factors on delirium indirectly affected patient prognosis through delirium.Conclusion The use of interventions to reduce delirium may improve patient prognosis. To improve the dependency activities and risk of pressure ulcers that directly affect delirium, early ambulation is encouraged, and treatment and nursing interventions to remove the ventilator and drainage tube quickly must be provided to minimize the application of restraint. Further, delirium can be prevented and patient prognosis improved through continuous intervention to stimulate cognitive awareness and monitoring of the onset of delirium. This study also discussed the effects of delirium intervention on the prognosis of patients with delirium and future research in this area.
-
Citations
Citations to this article as recorded by- Does ICU admission dysphagia independently contribute to delirium risk in ischemic stroke patients? Results from a cohort study
Hongtao Cheng, Simeng Song, Yonglan Tang, Shiqi Yuan, Xiaxuan Huang, Yitong Ling, Zichen Wang, Xiaoying Tian, Jun Lyu
BMC Psychiatry.2024;[Epub] CrossRef - Preoperative Anxiety and Its Postoperative Associated Factors in Patients Receiving Post Anesthetic Recovery Care at Surgical Intensive Care Unit
Yul Ha Lee, Hye-Ja Park
Journal of Health Informatics and Statistics.2023; 48(3): 267. CrossRef - Delirium Experience of the Intensive Care Unit Patients
Jaeyeon Jung, Sujin Jang, Seonmi Jo, Sunhee Lee
Journal of Korean Academy of Nursing.2022; 52(2): 134. CrossRef - The training needs of Korean intensive care unit nurses regarding delirium
Young Sook Roh
Intensive and Critical Care Nursing.2021; 62: 102954. CrossRef - Effect on Quality of Care of a Delirium Prevention Campaign for Surgical Intensive Care Nurses
Heejeong Kim, Sun-Mi Lee
Journal of Nursing Care Quality.2021; 36(4): 361. CrossRef - A Systematic Review and Meta-analysis on the Effect of Delirium Prevention Intervention in Korean Intensive Care Units
Jiyeon Kang, Min Jeong Choi
Journal of Korean Critical Care Nursing.2021; 14(3): 141. CrossRef
- Does ICU admission dysphagia independently contribute to delirium risk in ischemic stroke patients? Results from a cohort study
- 2,511 View
- 53 Download
- 4 Web of Science
- 6 Crossref

- Person-Centered Relational Care Experienced by Critical Care Nurses: An Interpretative Phenomenological Analysis Study
- Myoung Sun Jang, Sungjae Kim
- J Korean Acad Nurs 2019;49(4):423-436. Published online January 15, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.4.423
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The aim of the study was to explore nurses’ experience of person-centered relational care in the context of critical care.
Methods Key interview questions were developed based on the human-to-human relationship model suggested by Travelbee. Data were collected through in-depth interviews with a purposive sample of 11 nurses having more than 2 years of working experience in intensive care units. An interpretative phenomenological analysis was conducted to analyze the data.
Results Four super-ordinate and nine sub-ordinate themes were identified. Emerged super-ordinate themes were as follows: (1) encountering a live person via patient monitoring systems; (2) deep empathic connection; (3) humanistic and compassionate care, and (4) accompanying the journey to the end. Study findings revealed that nurses in intensive care units experienced ‘balancing emotions’ and ‘authenticity’ in caring when entering human-to-human relationships with dying patients. The phenomenon of person-centered relational care in intensive care units was found to subsume intrinsic attributes of empathy, compassion, and trust, similar to the central concepts of Travelbee's theory.
Conclusion The interpretative findings in this study provide deeper understanding of Travelbee's human-to-human relationship model. The technological environment in intensive care units did not hinder experienced nurses from forming human-to-human relationships. These themes need to be emphasized in critical care nursing education as well as in nursing management. The results of this study will contribute to understanding nurse-patient caring relationships in depth, and help improve the quality of nursing care in intensive care units.
-
Citations
Citations to this article as recorded by- Professional Identity Formation in Nursing: The Role of Travelbee's Human-to-Human Relationship Model
İnci İnceleme, Satı Demir
Journal of Gazi University Health Sciences Institute.2025; 7(1): 28. CrossRef - Concept Analysis of Warmth in Nursing
Jee-Won Kim, Mina Park
Journal of Korean Academy of Fundamentals of Nursing.2025; 32(2): 197. CrossRef - Workload, Teamwork, Compassion Competence, and Person-centered Critical Care Nursing among Critical Care Nurses
Hyun A Lee, Myung Sun Hyun, Jin-Hee Park, Eun Ji Seo
Journal of Korean Critical Care Nursing.2025; 18(2): 14. CrossRef - Listening to the voices of healthcare providers involved in the design of a new birthing room: an interpretative phenomenological analysis
Anwar Nader AlKhunaizi, Areej Ghalib Al-Otaibi
BMC Health Services Research.2025;[Epub] CrossRef - Framework of humanistic care for patients in theICU: A preliminary study
Yuchen Zhang, Li Zhao, Meng Zhang, Xiaojing Guo, Chen Xin, Yubiao Gai
Nursing in Critical Care.2024; 29(1): 125. CrossRef - Exploring Healthcare Providers’ and Women’s Perspectives of Labor Companionship during Childbirth: An Interpretative Phenomenological Analysis Study
Anwar Nader AlKhunaizi, Areej Ghalib Al-Otaibi, Manal F. Alharbi, Ghareeb Bahari
Healthcare.2024; 12(9): 869. CrossRef - Experience of Clinical Adaptation among Nurses in Intensive Care Unit
Jin Young Hong, Sue Kyung Sohn
Journal of Korean Critical Care Nursing.2024; 17(1): 1. CrossRef - Self-reflection of a General Ward Nurses on the Experience of End-of-Life Care for a Patient who Decided to Suspend Life-sustaining Treatment: van Manen's Hermeneutic Phenomenological Approach
Hee Jung Hong
Korean Journal of Adult Nursing.2023; 35(3): 273. CrossRef - The impact of family care visitation programme on patients and caregivers in the intensive care unit: A mixed methods study
Hye Jin Yoo, JaeLan Shim
Journal of Clinical Nursing.2023; 32(13-14): 3797. CrossRef - Effective Teaching Behaviors of Clinical Nursing Teachers: A Qualitative Meta-Synthesis
Jian Zhang, Fenhua Zhou, Jinxia Jiang, Xia Duan, Xin Yang
Frontiers in Public Health.2022;[Epub] CrossRef - Nurse Spiritual Care Therapeutics Scale
Kyung-Ah Kang, Elizabeth Johnston Taylor, Jiyoung Chun
Journal of Hospice & Palliative Nursing.2022; 24(6): E250. CrossRef - Person-centred care among intensive care unit nurses: A cross-sectional study
Hyuna Youn, Miyoung Lee, Sun Joo Jang
Intensive and Critical Care Nursing.2022; 73: 103293. CrossRef - The Effect of a Multifaceted Family Participation Program in an Adult Cardiovascular Surgery ICU*
Hye Jin Yoo, JaeLan Shim
Critical Care Medicine.2021; 49(1): 38. CrossRef - Conceptualization of Person-Centered Care in Korean Nursing Literature: A Scoping Review
Ji Yea Lee, Sewon Lee, Eui Geum Oh
Korean Journal of Adult Nursing.2020; 32(4): 354. CrossRef - Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study
Hye Jin Yoo, Oak Bun Lim, Jae Lan Shim, Liza Heslop
PLOS ONE.2020; 15(7): e0235694. CrossRef
- Professional Identity Formation in Nursing: The Role of Travelbee's Human-to-Human Relationship Model
- 2,847 View
- 91 Download
- 9 Web of Science
- 15 Crossref

- Risk Factors of Medical Device-Related Pressure Ulcer in Intensive Care Units
- MiJee Koo, YoungA Sim, InSoon Kang
- J Korean Acad Nurs 2019;49(1):36-45. Published online January 15, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.1.36
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to identify the characteristics of and risk factors for medical-device-related pressure ulcer (MDRPU) development in intensive care units.
Methods A prospective cohort study design was used, and the participants were 253 adult patients who had stayed in medical and surgical intensive care units. Data were collected regarding the application of medical devices and MDRPU-related characteristics over a period of six months from June to November, 2017. Data were analyzed using independent t-test, χ 2-test, Fisher's exact test, and binary logistic regression analysis with the SPSS 21.0 program.
Results Among the 253 participants, MDRPUs occurred in 51 (19.8%) participants. The results of the logistic regression analysis showed that the risk factors for MDRPUs were the use of endotracheal tubes (OR=5.79, 95% CI: 1.66~20.20), having had surgery (OR=2.95, 95% CI: 1.11~7.77), being in a semi-coma/coma (OR=5.79, 95% CI: 1.04~32.05), and sedation (OR=5.54, 95% CI: 1.39~22.19).
Conclusion On the basis of the study results, it is effectively facilitated by nurses when they care for patients with MDRPUs in intensive care units and the results are expected to be of help in preventive education for MDRPU development as well as preparing the base data for intervention studies.
-
Citations
Citations to this article as recorded by- Characteristics of and Risk Factors for Medical Device-Related Pressure Injuries in Trauma Patients in Intensive Care Units: A Retrospective Case–Control Study
Jong Eun Hyun, Seul Ki Park
Western Journal of Nursing Research.2026; 48(2): 131. CrossRef - Patient Safety and Quality Improvement in Nursing Practice: Associations Among Workload, Occupational Coping Self-Efficacy and Medical Device-Related Pressure Injury Prevention
Hyun Suk Gwag, Jin Ah Kim
Healthcare.2026; 14(2): 270. CrossRef - Risk Factors for Pressure Injury in ICU Patients
Yang Chaonan, Chaohui Ji, Pan Huibin, Li Shen, Luo Xiaohong
Nursing Open.2026;[Epub] CrossRef - Recommendations and Best Practices for the Risk Assessment of Pressure Injuries in Adults Admitted to Intensive Care Units: A Scoping Review
Ricardo Picoito, Tânia Manuel, Sofia Vieira, Rita Azevedo, Elisabete Nunes, Paulo Alves
Nursing Reports.2025; 15(4): 128. CrossRef - Association between nutrition risk and oral mucosal membrane pressure injury in critically ill adults requiring endotracheal tube placement: A prospective cohort study
Xiaohua Ai, Yuchun Deng, Bolan Wang, Hua Deng, Dongmei Tang, Linying Zeng, Yuping Jin, Yurong Liu, Lingli Jia
Journal of Parenteral and Enteral Nutrition.2025; 49(8): 983. CrossRef - Risk factors related to pressure injury after spinal surgery in the prone position in patients with diabetes mellitus: A prospective cohort study
Eren Hakki Isci, Ahmet Besir, Ersagun Tugcugil, Ali Riza Guvercin
Medicine.2025; 104(41): e45191. CrossRef - Risk Factors for Pressure Injury in Mechanically Ventilated Patients in Emergency Intensive Care Units: A Prospective Observational Study
Sun Woo Son, Mi Yu
Nursing in Critical Care.2025;[Epub] CrossRef - Fatores de risco para lesão por pressão relacionada a dispositivos médicos: revisão sistemática
Daniela Soldera, Nádia Chiodelli Salum, Mônica Stein, Juliana Balbinot Reis Girondi, Alacoque Lorenzini Erdmann, Maritza Regina Stuart
Revista Caribeña de Ciencias Sociales.2025; 14(11): e4911. CrossRef - Yoğun Bakım Hastalarında Tıbbi Cihazla İlişkili Basınç Yaralanması Gelişimi ve Etkileyen Faktörler: Nokta Prevalans Çalışması
Sevil Pamuk Cebeci, Asuman Çobanoğlu, Hatice Oğuzhan
Sağlık Bilimleri Üniversitesi Hemşirelik Dergisi.2024; 6(1): 57. CrossRef - Tıbbi Cihaza Bağlı Basınç Yarası Gelişme Riski
Handan Aydın Kahraman, Gülay İpekçoban
Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi.2024; 13(1): 486. CrossRef - Intensive care nurses' knowledge and practices regarding medical device‐related pressure injuries: A descriptive cross‐sectional study
Aslı Kurtgöz, Selin Keskin Kızıltepe, Hülya Keskin, Münevver Sönmez, İsmail Aşatır
International Wound Journal.2024;[Epub] CrossRef - Factors associated with facial pressure injury in patients receiving non‐invasive positive pressure ventilation mask: A retrospective case–control study
Pei‐Ling Wu, Yi‐Jou Li, Hsiang‐Chu Pai, Chien‐Chi Liu
Journal of Clinical Nursing.2024; 33(1): 149. CrossRef - Determination of Incidence and Risk Factors of Medical Device-Related Pressure Injury in the ICU: A Descriptive Study
Ezgi Dirgar, Neslihan Yağmur Gider, Betül Tosun
Advances in Skin & Wound Care.2024; 37(3): 1. CrossRef - Incidence, severity and characteristics of medical device-related pressure injuries in adult intensive care patients: A single-centre, cross-sectional study
Zeynep Temiz, Aylin Aydın Sayılan, Samet Sayılan, Esra Azum
Journal of Tissue Viability.2024; 33(2): 220. CrossRef - NGHIÊN CỨU TÌNH HÌNH CHẤN THƯƠNG ÁP LỰC DO THIẾT BỊ Y TẾ TẠI KHOA HỒI SỨC NGOẠI THẦN KINH BỆNH VIỆN CHỢ RẪY
Trang Nhung Nguyễn, Mai Anh Lợi Mai Anh Lợi, Nguyễn Thị Kim Bằng Nguyễn Thị Kim Bằng
Tạp Chí Khoa Học Trường Đại Học Quốc Tế Hồng Bàng.2024; : 134. CrossRef - Development and validation of a nomogram for oral mucosal membrane pressure injuries in ICU patients: A prospective cohort study
Lingli Jia, Yuchun Deng, Yu Xu, Xiaoli Wu, Dan Liu, Muying Li, Shijun Huang, Yaodan Zhang, Aiping Du, Huan Liu, Yongming Tian
Journal of Clinical Nursing.2024; 33(10): 4112. CrossRef - Factors affecting the occurrence of pressure injuries among patients receiving targeted temperature management after cardiac arrest
Shinhye Ahn, Minjeong An, Sung-Hee Yoo, Hyunyoung Park
Australian Critical Care.2023; 36(3): 313. CrossRef - Incidência de lesões por pressão relacionadas a dispositivos médicos em unidade de terapia intensiva adulto
Nara Reisdorfer, Eliane Regina Pereira do Nascimento, Daniele Delacanal Lazzari, Maria Elena Echevarría-Guanilo, Sabrina Guterres da Silva Galetto , Luciana Bihain Hagemann de Malfussi
Revista de Enfermagem da UFSM.2023; 13: e32. CrossRef - Characteristics and Risk Factors for Pressure Ulcers in Severe Trauma Patients Admitted to the Trauma Intensive Care Unit
Seung-yeon Lim, Young-min Jeong, So-young Jeong
Journal of Acute Care Surgery.2023; 13(2): 47. CrossRef - The Characteristics and Risk Factors of Medical Device Related Pressure Injury in Intensive Care Unit Patients
Mi Hyeon Jo, Hye-Ran Choi
Journal of Korean Critical Care Nursing.2023; 16(2): 28. CrossRef - Incidence, prevalence and risk factors of device‐related pressure injuries in adult intensive care unit: A meta‐analysis of 10,084 patients from 11 countries
Yi‐Jie Jia, Fei‐Hong Hu, Wan‐Qing Zhang, Wen Tang, Meng‐Wei Ge, Wang‐Qin Shen, Hong‐Lin Chen
Wound Repair and Regeneration.2023; 31(5): 713. CrossRef - Risk factors for device-related pressure injuries in general ward inpatients of a tertiary general hospital: A case-control study
Minkyung Kim, Yong Soon Shin
Journal of Tissue Viability.2023; 32(4): 601. CrossRef - Determining the incidence and risk factors of medical device-related pressure injury in intensive care patients
Kevser Karacabay, Ayşegül Savci, Mehmet Dalkılıç, Filiz Kabu Hergül
Journal of Tissue Viability.2023; 32(4): 596. CrossRef - Risk factors for medical device-related pressure injury in ICU patients: A systematic review and meta-analysis
Ling Gou, Zhiqin Zhang, Yongde A., Benjamin M. Liu
PLOS ONE.2023; 18(6): e0287326. CrossRef - Determining Optimal Cut-off Score for the Braden Scale on Assessment of Pressure Injury for Tertiary Hospital Inpatients
Sook Hyun Park, hyeyeon Choi, Youn-Jung Son
Journal of Korean Critical Care Nursing.2023; 16(3): 24. CrossRef - Risk factors of medical device‐related pressure injury in intensive care units
Wen Dang, Yuan Liu, Qing Zhou, Yuyu Duan, Huaxiu Gan, Lin Wang, Qiongli Zhu, Chunyan Xie, Ailing Hu
Journal of Clinical Nursing.2022; 31(9-10): 1174. CrossRef - Incidence, characteristics and risk factors of medical device-related pressure injuries: An observational cohort study
Öznur Erbay Dallı, İlkay Ceylan, Nermin Kelebek Girgin
Intensive and Critical Care Nursing.2022; 69: 103180. CrossRef - Incidence of and risk factors for self‐load‐related and medical device‐related pressure injuries in critically ill patients: A prospective observational cohort study
Tomoko Shimura, Gojiro Nakagami, Rei Ogawa, Shimpei Ono, Toshiaki Takahashi, Misako Nagata, Kosuke Kashiwabara, Junko Sugama, Hiromi Sanada, Makoto Oe
Wound Repair and Regeneration.2022; 30(4): 453. CrossRef - Device-related pressure ulcers: SECURE prevention. Second edition
Amit Gefen, Paulo Alves, Guido Ciprandi, Fiona Coyer, Catherine T Milne, Karen Ousey, Norihiko Ohura, Nicola Waters, Peter Worsley, Joyce Black, Michelle Barakat-Johnson, Dimitri Beeckman, Jacqui Fletcher, Holly Kirkland-Kyhn, Nils A. Lahmann, Zena Moore,
Journal of Wound Care.2022; 31(Sup3a): S1. CrossRef - Factors Associated with Pressure Injury Among Critically Ill Patients in a Coronary Care Unit
Eunji Ko, Seunghye Choi
Advances in Skin & Wound Care.2022; 35(10): 1. CrossRef - Incidence and risk factors of medical device-related pressure injuries among patients undergoing prone position spine surgery in the operating room
Mi Ae Choi, Myoung Soo Kim, Cheol Kim
Journal of Tissue Viability.2021; 30(3): 331. CrossRef - Incidence and Risk Factors Associated with Medical Device-Related Pressure Injuries in Neurosurgery Surgery Patients
Tae Yeong Yang, Joon Bum Kim, Hye Sung Kim, Jung Eun Park
Korean Journal of Adult Nursing.2021; 33(3): 226. CrossRef - Relationships Between Oral-Mucosal Pressure Ulcers, Mechanical Conditions, and Individual Susceptibility in Intubated Patients Under Intensive Care: A PCR-Based Observational Study
Soo Hyun Kim, Hee Sam Nah, Jin Bom Kim, Chul Hoon Kim, Myoung Soo Kim
Biological Research For Nursing.2021; 23(4): 557. CrossRef - Economic Evaluation of Hospital-based Home Care Services for the Breast Cancer Surgery Patients
Jeong Yeon Ko, Ju Young Yoon
Journal of Korean Academy of Community Health Nursing.2021; 32(3): 356. CrossRef - Differences in Associated Factors according to the Time of Occurrence of Pressure Ulcers in Intensive Care Unit Patients
Mijung Lee, Eunjeoung Seo, Miok Kim, Jeongok Park, Seonmi Lee, Hyunkyung Shin, Ilsim Yun, Mina Cho, Youngcha Cho, Bomi Kang, Hyunmi Seo, Misoon Lee, Sira Lee, Hyejoo Jang, Hyunsuk Jung, Jeong-Ah Ahn
Journal of Korean Critical Care Nursing.2021; 14(3): 26. CrossRef - Development and Testing of an Algorithm to Prevent Medical Device–Related Pressure Injuries
Yeong-Mi Seong, Hyejin Lee, Ji Min Seo
INQUIRY: The Journal of Health Care Organization, Provision, and Financing.2021;[Epub] CrossRef - Communication Competence, Nursing Professionalism and Job Performance among Home Healthcare Nurses
Eunha Jeong, Sujeong Han
Journal of Korean Academy of Nursing Administration.2020; 26(4): 409. CrossRef - Incidence and risk factors for medical device‐related pressure ulcers: The first report in this regard in Iran
Farnoosh Rashvand, Lida Shamekhi, Hossein Rafiei, Mohammad Nosrataghaei
International Wound Journal.2020; 17(2): 436. CrossRef - Risk prediction models for the development of oral-mucosal pressure injuries in intubated patients in intensive care units: A prospective observational study
Byung Kwan Choi, Myoung Soo Kim, Soo Hyun Kim
Journal of Tissue Viability.2020; 29(4): 252. CrossRef
- Characteristics of and Risk Factors for Medical Device-Related Pressure Injuries in Trauma Patients in Intensive Care Units: A Retrospective Case–Control Study
- 3,098 View
- 93 Download
- 28 Web of Science
- 39 Crossref

- A Relation Study on Burden, Health promotion Behavior and Health Status of the Family Caregiver of Intensive Care Unit Patient
- Eun Sil Kim, Jeong Sook Park, Chung Ja Park
- Journal of Korean Academy of Nursing 2002;32(5):654-664. Published online March 29, 2017
- DOI: https://doi.org/10.4040/jkan.2002.32.5.654
-
 Abstract
Abstract
 PDF
PDF PURPOSE: The purpose of this study was to identify the burden, health promotion behavior and health status and to describe the relationship of the burden, health promotion behavior and health status of the family caregivers of intensive care unit patients. METHOD: The subjects were 48 family caregivers of ICU patients in a University Hospital. Data were collected between June, 1 and July, 31, 2000 using structured questionnaires. Research tools used were Suh and Oh's Burden Scale, Revised Walker, Sechrist, and Pender's HPLP(1987) ; Revised Nam's Health State Scale(1965). RESULT: The mean score of burden of family caregiver was 3.01(full score was 5). The mean score of health promotion behavior of family caregiver was 2.52 (full score was 4). And the mean score of health status of family caregiver was 0.68(full score was 1.00). The score of psychological health state was a little higher than the physiological one. In correlational analysis, the burden and the health status of caregivers were reversely correlated . The correlation between the burden and the health promotion behavior, and the health behavior and health status were not significant. CONCLUSION: The more burden caregivers of ICU patients felt, the worse their health status. So nurses need to understand the family caregiver's burden and apply nursing care that can reduce burden, in order to improve the health status of family caregivers.
-
Citations
Citations to this article as recorded by- Experiences of Family Members With Visitation Prohibition for Critically Ill Patients
Sunjung Kim, Sunghee H. Tak
Western Journal of Nursing Research.2024; 46(11): 854. CrossRef - The Lived Experiences of Patient’s Families with the Intensive Care Unit Diary
Yu Jin Jeong, Sung Suk Ryoo, Hyun Jeong Shin, Young Hee Yi
Journal of Korean Critical Care Nursing.2023; 16(1): 28. CrossRef - Challenges Experienced by Family Caregivers of the Adult Intensive Care Unit Patients in Korea: An Integrative Review
JiYeon Choi, Judith A. Tate, Youn-Jung Son
Clinical Nursing Research.2021; 30(4): 423. CrossRef - Factors Affecting Caregivers' Burnout Caring for a Family Member in an Intensive Care Unit
Min-Jeong Park, So-Hee Park, Mi Young Chung
Korean Journal of Adult Nursing.2017; 29(5): 517. CrossRef - Nursing Needs of the Parents of Infants in Neonatal Intensive Care Unit
Ji-Sun Park, Kyung-Sook Bang
Journal of East-West Nursing Research.2014; 20(2): 136. CrossRef
- Experiences of Family Members With Visitation Prohibition for Critically Ill Patients
- 890 View
- 3 Download
- 5 Crossref

- Confirmatory Analysis of Perception and Preference Scales for Work Characteristics among Korean Nurses
- Yeon Ok Suh, Rha Yun Song, Daily Barbara
- Journal of Korean Academy of Nursing 1999;29(2):215-224. Published online March 29, 2017
- DOI: https://doi.org/10.4040/jkan.1999.29.2.215
-
 Abstract
Abstract
 PDF
PDF The study was conducted to confirm the construct of individual perception and preference for work characteristics as personal factors influencing Korean nurses' job satisfaction. The subjects of the study were 231 nurses who are currently working in intensive care units and have been for a minimum of 6 months. The study used the Staff Perception and Preference Scale(Song et al., 1997) to measure the individual's perception and preference on the technical, practice, and management components of the ideal work environment. The Korean version of the Staff Perception and Preference Scale consists of 16 items on perception and 13 on preference with each item related on a scale from 1 (not at all) to 4 (a great deal). Psychometric testing revealed that the preference and perception scale is internally consistent with Chronbach's alphas of .83 for perception scale and .80 for preference scale. The subscales of the perception and preference scale also showed acceptable reliability for the early stage of the development of the instruments with Chronbach alphas of .62-.76 and .69-.83 respectively. Criterion0related validity of the scale was tested by examining correlations with individual growth need that is conceptually close to individual preference, but not to individual perception. Individual growth need was significantly related to individual preference(r=.63, p<.05), but the correlation with the perception scale was not significant. A separate factor analysis for the each of perception and preference scales was performed with a three-factor loading solution based on a previous study. The results on the staff perception scale confirmed with varimax rotation that the items were cleanly and strongly loaded on technique, practice and management components, which together explained 50.7% of the variance. The factor analysis on the staff preference scale also yielded a three factor solution that explained 56.7% of the variance, but items on technique and management components were loaded together. This phenomena may due to the current nursing delivery system in Korea where nurses never experience either shared governance nor case management, and as a results they may not be able to consider management roles as their potential extended roles. Therefore, more efforts should be given to enhance nurses' autonomy and decision making in the technique, practice and management components of their work environment. Meanwhile, there is a need for continuously confirming and developing tools for individual perception and preferences to effectively enhance job satisfaction among Korea nurses through innovative work environments.
- 444 View
- 0 Download

- The Experiences of Patients in Intensive Care Units(ICU)
- Young Hae Kim, Mi Jee Koo, So Hee Kim, Young Mi Kim, Nae Young Lee, Koung Oh Chang
- Journal of Korean Academy of Nursing 2007;37(6):924-931. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2007.37.6.924
-
 Abstract
Abstract
 PDF
PDF PURPOSE: The purpose of this study was to describe the essence of the experiences of patients in an ICU, and to understand them from the patients' point of view. METHODS: Participants in this study were six patients in P hospital. Data collection consisted of in-depth interviews and an observation method done from January to April in 2005. The method was analysis using the phenomenological method proposed by Colaizzi(1978). RESULTS: The themes were classified into eight theme clusters. The eight theme clusters were finally grouped into four categories, 'shock', 'pain', 'gratefulness' and 'pleasure of revival'. CONCLUSION: The ICU patients had negative experiences in physical.mental critical situations, but also positive experiences in consolation and nurses and families' encouragement. Therefore, ICU nurses must support patients and their families to minimize the negative experiences and maximize the positive experiences.
-
Citations
Citations to this article as recorded by- A Study on Nurses' Communication Experiences with Intubation Patients
Ye Rim Kim, Hye Ree Park, Mee Kyung Shin
The Korean Journal of Rehabilitation Nursing.2023; 26(1): 28. CrossRef - Item analysis of the Korean version of the Intensive Care Experience Questionnaire: Using the Rasch Model based on Item Response Theory
Jiyeon Kang, Minhui Kim
Journal of Korean Critical Care Nursing.2022; 15(3): 37. CrossRef - Delirium Experience of the Intensive Care Unit Patients
Jaeyeon Jung, Sujin Jang, Seonmi Jo, Sunhee Lee
Journal of Korean Academy of Nursing.2022; 52(2): 134. CrossRef - Validation of a Korean Translated Version of the Critical Care Pain Observation Tool (CPOT) for ICU Patients
Eun-Mi Kwak, Heeyoung Oh
Journal of Korean Academy of Nursing.2012; 42(1): 76. CrossRef - Factors Predicting Patient Discomfort after Coronary Angiography
Ae Ran Park, Ja Yun Choi
Journal of Korean Academy of Nursing.2009; 39(6): 860. CrossRef - Concept Analysis of Relocation Stress - Focusing on Patients Transferred from Intensive Care Unit to General Ward -
Youn-Jung Son, Sung-Kyung Hong, Eun Young Jun
Journal of Korean Academy of Nursing.2008; 38(3): 353. CrossRef
- A Study on Nurses' Communication Experiences with Intubation Patients
- 994 View
- 3 Download
- 6 Crossref

- Analysis of the Nursing Practice in a Medical ICU Based on an Electronic Nursing Record
- Kyung Ja Song
- Journal of Korean Academy of Nursing 2007;37(6):883-890. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2007.37.6.883
-
 Abstract
Abstract
 PDF
PDF PURPOSE: The purpose of this study was to identify the entity of critical care nursing practices through analyzing nursing statements described by electronic nursing records in a MICU. METHODS: 176,459 nursing statements of 188 patients during a 6 month-stay were analyzed statement by statement according to the nursing process(nursing phenomena, nursing diagnosis, & nursing activity) and 21 nursing components of Saba's Clinical Care Classification. RESULTS: Among 176,459 single statements, the statements of nursing activity ranked first in number. The contents of the statements were analyzed and categorized by main themes. Among 489 categorized themes, the number of themes of nursing phenomena statements was the highest. When analyzed by Saba's clinical Care Classification, the nursing statements mainly included a physiological component. Among 21 components, the respiratory component ranked in the first position in nursing phenomena, nursing diagnosis and nursing activity. The extra statements not included in the 21 components were 9,294(15.1%) in nursing phenomena and 21,949(22.7%) in nursing activity. Most are statements related to tests and the doctor. CONCLUSION: The entity of MICU nursing practice expressed by electronic nursing records was mainly focused on physiological components and more precisely on respiratory components.
-
Citations
Citations to this article as recorded by- An Analysis of Tasks of Nurses Caring for Patients with COVID-19 in a Nationally-Designated Inpatient Treatment Unit
Minho Jung, Moon-Sook Kim, Joo-Yeon Lee, Kyung Yi Lee, Yeon-Hwan Park
Journal of Korean Academy of Nursing.2022; 52(4): 391. CrossRef - Emergency Department Nursing Activities: Retrospective Study on Data from Electronic Nursing Records
Seung Yeon Baik, Eunhee Cho, Young Ah Kim, Mona Choi
Korean Journal of Adult Nursing.2019; 31(5): 496. CrossRef - The Knowledge, Need, and Usage of Medical Terminology in Clinical Nursing Practice
Gisoo Shin, Mi-Kyoung Cho
Journal of Korean Biological Nursing Science.2014; 16(4): 276. CrossRef - Nurse Characteristics related to Level of Use of Essential Oriental Nursing Terms in Oriental Medicine Hospitals
Jee-In Hwang, Won-Ock Kim, Myoung-Ja Wang
Journal of Korean Academy of Nursing Administration.2011; 17(2): 209. CrossRef
- An Analysis of Tasks of Nurses Caring for Patients with COVID-19 in a Nationally-Designated Inpatient Treatment Unit
- 854 View
- 5 Download
- 4 Crossref

- A Study on Job Stress and the Coping of ICU Nurses
- Hyoung Sook Park, Eun Hee Gang
- Journal of Korean Academy of Nursing 2007;37(5):810-821. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2007.37.5.810
-
 Abstract
Abstract
 PDF
PDF Purpose This study investigated job stress and coping of ICU Nurses.
Method Data was accumulated from 206 ICU nurses serving at least more than one year in 500 bed order hospitals during the period of three months from June1, to August 30, 2006.
Results The average job stress was 2.96± .95 points, which was relatively high. The average coping was 2.55± .23 points.
Conclusion The extent of the job stress of ICU nurses was relatively high, and they received the heaviest stress from job circumstances. For the prevention of job stress, every effort is required to analyze the causes of stress caused by job circumstances and to pose an appropriate solution. Meanwhile, job stress, needs to be controlled using a solution for the central problem, and search for social support.
-
Citations
Citations to this article as recorded by- Occupational Stress, Coping, and Outcomes among Korean Nurses: An Integrative Review Based on the Transactional Model of Stress and Coping
Myungji Kim, Hyunkyung Choi
STRESS.2025; 33(3): 127. CrossRef - Analyzing employee attrition of research and development firms using mixed methods
Govind Nath Srivastava, Himanshu Sharma, Richa N. Agarwal, Ajay K. Jain
Cogent Business & Management.2025;[Epub] CrossRef - Priority analysis of educational needs for new nurses in the intensive care unit: A cross‐sectional study
Sung Ok Chang, Seung‐Kyo Chaung, Kyeong‐Yae Sohng, Kyunghee Kim, Jongsoon Won, Min‐Jung Choi
Nursing in Critical Care.2024; 29(5): 1162. CrossRef - Factors Related to Post-traumatic Stress Disorder Symptoms Among Intensive Care Unit Nurses
SuHee Kim, YeoJin Im
Asian Nursing Research.2024; 18(2): 159. CrossRef - The Effects of Communication Ability, Job Satisfaction, and Organizational Commitment on Nursing Performance of Intensive Care Unit Nurses
Nu Ri Kim, Sung Eun Kim, So Eun Jang
Journal of Korean Critical Care Nursing.2022; 15(1): 58. CrossRef - Factors Influencing Patient Safety Nursing Activities of Intensive Care Unit Nurses
Jae Eun Kim, Ju Eun Song, Jeong Ah Ahn, Sunjoo Boo
Journal of Korean Critical Care Nursing.2021; 14(2): 12. CrossRef - Factors Influencing Post-Traumatic Stress Disorder in Critical Care Nurses based on Lazarus & Folkman's Stress, Appraisal-Coping Model
Hye Gyeong Kim, Ja Yun Choi
Korean Journal of Adult Nursing.2020; 32(1): 88. CrossRef - Effects of Work Environment on the Job Satisfaction of Occupational Therapists: Mediating Effect of Empowerment
Bo-Young Son, Yo-Soon Bang, Jae-Hyeon Lee
Journal of Korean Society of Occupational Therapy.2020; 28(3): 15. CrossRef - Oral health care provided by nurses for hospitalized patients in Korea
Ye‐Ji Lee, Hie‐Jin Noh, Sun‐Young Han, Hyun‐Sun Jeon, Won‐Gyun Chung, So‐Jung Mun
International Journal of Dental Hygiene.2019; 17(4): 336. CrossRef - Factors Influencing Resilience in Long-term Care Hospital Nurses
Ju Hui Moon, Sook Hee Yoon
Journal of Korean Academy of Nursing Administration.2019; 25(5): 373. CrossRef - Experience of Violence from the Clients and Coping Methods Among Intensive Care Unit Nurses Working in a Hospital in South Korea
Hye Jin Yoo, Eunyoung E. Suh, Soon Haeng Lee, Jin Hee Hwang, Ji Hye Kwon
Asian Nursing Research.2018; 12(2): 77. CrossRef - Effects of Music Therapy on Subjective Stress Response, Salivary Cortisol, and Fatigue for Intensive Care Nurses
Hyun Hee Ji, Hyun Sook Jo
Korean Journal of Health Promotion.2017; 17(2): 119. CrossRef - Influence of the Emotional Intelligence, Communication Competence and Stress coping on Turnover Intention in Psychiatric Nurses
Hye-Seung Kang, Yoon-Young Kim
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(1): 141. CrossRef - Factors Affecting on Turnover Intentions among Operating Room Nurses
Yeo-Jin Kim, Keum-Sook Park, Eun-Ja Yang
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(12): 352. CrossRef - Structural Equation Model for Job Stress in Intensive Care Unit Nurses
Su Jin Jin, Ji Hyun Lee
Korean Journal of Occupational Health Nursing.2015; 24(2): 103. CrossRef - The Inter-Rater Reliability of Simplified Acute Physiology Score 3 (SAPS3) among Intensive Care Unit Nurses
Jun Hyun Kim, Ji Yeon Kim, Wonil Kim, Kyung Woo Kim, Sang-il Lee, Kyung-Tae Kim, Jang Su Park, Won Joo Choe, Jung Won Kim
The Korean Journal of Critical Care Medicine.2015; 30(1): 8. CrossRef - The Relationship between Metabolic Syndrome Risk Factors and Health Promotion Behavior in General Hospital Nurses
Hyun-Hee Park, Kwang-Ok Lee
The Journal of the Korea Contents Association.2015; 15(6): 314. CrossRef - The Convergence Study on the Relationship between the Job Stress and Mental Health of Nurses
Mi-Jin Kim, Gyun-Young Kang
Journal of the Korea Convergence Society.2015; 6(5): 39. CrossRef - Influence of Job Stress and Professional Self-concept on Job Satisfaction among Nurses in Rehabilitation Units
Jung Ok Ko, Eun Ko
The Korean Journal of Rehabilitation Nursing.2014; 17(2): 81. CrossRef - The Relationship between Emotional Intelligence and Stress Coping of Nurses
Hyoung-Sook Park, Jae-Hyun Ha, Mee-Hun Lee, Hyun-Ju Lee
Journal of Korean Academy of Fundamentals of Nursing.2014; 21(4): 466. CrossRef - Influences of Job Stress, Coping, Self-efficacy on Burnout of Clinical Nurses
Ji-Won Lee
Journal of Fisheries and Marine Sciences Education.2014; 26(5): 1003. CrossRef - Effect of the Occupational Stress and Self Esteem on Mental Health among Nurses
Hea-Shoon Lee
The Journal of the Korea Contents Association.2013; 13(3): 251. CrossRef - Job Stress, Job Satisfaction, and Organizational Commitment of Customized Home Health Care Nurse
Chan Gyeong Park, Ki Soo Park, Young Sil Kang
Journal of agricultural medicine and community health.2013; 38(1): 39. CrossRef - An Analysis of Factors Influencing Job Satisfaction among Nurses Working in College Health Centers
Kyu Jung Cha, Mi Ryeong Song
Journal of Korean Academy of Fundamentals of Nursing.2013; 20(3): 259. CrossRef - Relationships among Burnout, Job Satisfaction, Organizational Commitment and Turnover Intention to Resign in Hospital Nurses
Mi Ran Kim, GyeongAe Seomun
Korean Journal of Occupational Health Nursing.2013; 22(2): 93. CrossRef - Effect of Environmental Intervention on Sleep, Emotions and Job Satisfaction of Rotating Shift Nurses in Intensive Care Unit
Hee-Ja Kim
Korean Journal of Adult Nursing.2012; 24(1): 11. CrossRef - Occupational Stress and Coping Styles as Factors Affecting the Burnout of Clinical Nurses
Kyoung Ja Kwon, Seung-Hee Lee
Journal of Korean Academy of Nursing Administration.2012; 18(4): 383. CrossRef - The Relation Between the Occupational Stress and Fatigue Level of Neonatal Nurses
Eun-A Park, Jeong-Eon Park
Korean Journal of Occupational Health Nursing.2011; 20(3): 261. CrossRef - Role of internal marketing, organizational commitment, and job stress in discerning the turnover intention of Korean nurses
Haejung LEE, Myoung‐Soo KIM, Jung‐A YOON
Japan Journal of Nursing Science.2011; 8(1): 87. CrossRef - Exposure to Workplace Violence and Coping in Intensive Care Unit Nurses
Hyun-Jung Park, Hee-Sun Kang, Kyung-Hee Kim, Hye-Jin Kwon
Journal of Korean Academy of Psychiatric and Mental Health Nursing.2011; 20(3): 291. CrossRef - Effects of Perception of Job Stress and Stress Coping Style on Mental Health of Firefighters
Ho Jin Lee, Hee Sook Kim, Sang Yeon Park
Journal of Korean Academy of Psychiatric and Mental Health Nursing.2011; 20(3): 315. CrossRef
- Occupational Stress, Coping, and Outcomes among Korean Nurses: An Integrative Review Based on the Transactional Model of Stress and Coping
- 1,333 View
- 15 Download
- 31 Crossref

- Patients' Anxiety in Intensive Care Units and Its Related Factors
- Chin Kang Koh
- Journal of Korean Academy of Nursing 2007;37(4):586-593. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2007.37.4.586
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to describe patients' anxiety in the ICU and to investigate related factors on the anxiety level.
Methods An exploratory cross-sectional survey design was used. Forty-eight patients participated in the study. Questionnaires were asked to patients who had been cared in the ICUs.
Results Related to the anxiety level, the mean of the total anxiety score was 5.47, and 60% of the patients had moderate or severe level of anxiety. Patients from the coronary care unit had a significantly higher level of anxiety than those from surgical intensive care unit or pulmonary surgery care unit. Moreover, significantly different levels of anxiety were found among patients who had been stayed for 2, 3, or 4 days.
Conclusion Patients who were from the coronary care unit or had been stayed longer (up to 4 days) in the ICU were significantly associated with higher anxiety level.
-
Citations
Citations to this article as recorded by- Effects of Anxiety Focused Nursing Interventions on Anxiety, Cognitive Function and Delirium in Neurocritical Patients: A Non‐Randomized Controlled Design
Seo‐young Jang, Myung Kyung Lee
Nursing in Critical Care.2025;[Epub] CrossRef - Effect of audiovisual media-based nursing information on environmental stress, anxiety, and uncertainty in patients undergoing open-heart surgery
Jeong-Yeong Jeon, Dong-Hee Kim, Kyoungrim Kang
Medicine.2023; 102(8): e33001. CrossRef - Effects of Prior Information About Intensive Care Unit Environment on Anxiety and Environmental Stress in Patients Undergoing Open Heart Surgery
Kyong Mi Shin, Hye Ran Choi
The Journal of Korean Academic Society of Nursing Education.2015; 21(1): 28. CrossRef - The Effect of Back Pain Prevention Intervention Program on Back Pain Relief in Patients Following Percutaneous Coronary Intervention
Hyea Kyung Lee, Yeon Suk Park
The Korean Journal of Rehabilitation Nursing.2013; 16(2): 100. CrossRef - Factors Influencing Relocation Stress Syndrome in Patients Following Transfer from Intensive Care Units
Jin-Hee Park, Moon-Sook Yoo, Youn-Jung Son, Sun Hyoung Bae
Journal of Korean Academy of Nursing.2010; 40(3): 307. CrossRef - Concept Analysis of Relocation Stress - Focusing on Patients Transferred from Intensive Care Unit to General Ward -
Youn-Jung Son, Sung-Kyung Hong, Eun Young Jun
Journal of Korean Academy of Nursing.2008; 38(3): 353. CrossRef
- Effects of Anxiety Focused Nursing Interventions on Anxiety, Cognitive Function and Delirium in Neurocritical Patients: A Non‐Randomized Controlled Design
- 937 View
- 14 Download
- 6 Crossref

- Pain Assessment using CRIES, FLACC and PIPP in High-Risk Infants
- Youngmee Ahn, Heeok Kang, Eunjin Shin
- Journal of Korean Academy of Nursing 2005;35(7):1401-1409. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.7.1401
-
 Abstract
Abstract
 PDF
PDF Purpose Infants at neonatal intensive care units (NICU) are invariably exposed to various procedural and environmental stimuli. The study was performed to compare the pain responses in three NICU stimulants and to examine the clinical feasibility for NICU infants using CRIES, FLACC and PIPP.
Method In a correlational study, a total of 94 NICU stimulants including angio-catheter insertions, trunk-rubbings and loud noises, was observed for pain responses among 64 infants using CRIES, FLACC and PIPP.
Results A significant difference was identified among the mean scores in CRIES(F(2, 91)=47.847, p=.000), FLACC(F(2, 91)=41.249, p=.000) and PIPP(F(2, 91)=16.272, p=.000) to three stimulants. In a Post-hoc Scheff test, an angio-catheter insertion showed the highest scores in CRIES, FLACC and PIPP compared to the other two stimulations. A strong correlation was identified between CRIES and FLACC in all three stimulations(.817 < r < .945) while inconsistent findings were identified between PIPP and CRIES or FLACC.
Conclusions The results of the study support that CRIES and FLACC are reliable and clinically suitable pain measurements for NICU infants. Further studies are needed in data collection time-point as well as clinical feasibility on PIPP administration to assess pain response in infants, including premature infants.
-
Citations
Citations to this article as recorded by- Evaluation of Pain in the Pediatric Patient Admitted to Sub-Intensive Care: What Is the Evidence? A Scoping Review
Antonio Bonacaro, Carlotta Granata, Chiara Canini, Lucrezia Anderle, Federica Ambrosi, Maria Chiara Bassi, Giacomo Biasucci, Andrea Contini, Giovanna Artioli, Elisa La Malfa, Massimo Guasconi
Epidemiologia.2025; 6(1): 9. CrossRef - Clinical rating scales for assessing pain in newborn infants
Kenneth Färnqvist, Emma Olsson, Andrew Garratt, Themistoklis Paraskevas, Roger F Soll, Matteo Bruschettini, Emma Persad
Cochrane Database of Systematic Reviews.2025;[Epub] CrossRef - Using AI to Detect Pain through Facial Expressions: A Review
Gioacchino D. De Sario, Clifton R. Haider, Karla C. Maita, Ricardo A. Torres-Guzman, Omar S. Emam, Francisco R. Avila, John P. Garcia, Sahar Borna, Christopher J. McLeod, Charles J. Bruce, Rickey E. Carter, Antonio J. Forte
Bioengineering.2023; 10(5): 548. CrossRef - Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty
Paul F. Chisolm, Nikhi P. Singh, Ian Cummins, Robert A. Oster, Damon Cox, Pankaj P. Dangle
Surgeries.2021; 2(3): 278. CrossRef - Defining and distinguishing infant behavioral states using acoustic cry analysis: is colic painful?
Joanna J. Parga, Sharon Lewin, Juanita Lewis, Diana Montoya-Williams, Abeer Alwan, Brianna Shaul, Carol Han, Susan Y. Bookheimer, Sherry Eyer, Mirella Dapretto, Lonnie Zeltzer, Lauren Dunlap, Usha Nookala, Daniel Sun, Bianca H. Dang, Ariana E. Anderson
Pediatric Research.2020; 87(3): 576. CrossRef - Prevention and treatment of pain in the neonatal intensive care unit
Hanna Popowicz, Wioletta Mędrzycka-Dąbrowska, Katarzyna Kwiecień-Jaguś
BÓL.2018; 19(2): 21. CrossRef - Effect of vapocoolant spray and EMLA cream upon DPT vaccination pain in infants
Gunja Jang, Eunyoung Jeon, Eunsil Lee
Journal of the Korean Data and Information Science Society.2014; 25(4): 705. CrossRef - Evaluation of Mental Status in High-Risk Neonates using Infants Coma Scale
Young-Mee Ahn, Min Sohn, Sang-Mi Lee
Journal of Korean Academy of Nursing.2010; 40(4): 561. CrossRef - Pain Response to Procedural Pain in Premature Infants
Jung Sook Kim, Eun Jung Lee, Eun Ha Ham, Ji Hyun Kim, Young Hee Yi
Journal of Korean Academy of Child Health Nursing.2010; 16(4): 352. CrossRef
- Evaluation of Pain in the Pediatric Patient Admitted to Sub-Intensive Care: What Is the Evidence? A Scoping Review
- 1,072 View
- 19 Download
- 9 Crossref

- Evaluating the Validity of the Pediatric Index of Mortality II in the Intensive Care Units
- Jung Soon Kim, Sun Joo Boo
- Journal of Korean Academy of Nursing 2005;35(1):47-55. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.1.47
-
 Abstract
Abstract
 PDF
PDF Purpose This study was to evaluate the validity of the Pediatric Index of Mortality II(PIM II).
Method The first values on PIM II variables following ICU admission were collected from the patient's charts of 548 admissions retrospectively in three ICUs(medical, surgical, and neurosurgical) at P University Hospital and a cardiac ICU at D University Hospital in Busan from January 1, 2002 to December 31, 2003. Data was analyzed with the SPSSWIN 10.0 program for the descriptive statistics, correlation coefficient, standardized mortality ratio(SMR), validity index(sensitivity, specificity, positive predictive value, negative predictive value), and AUC of ROC curve.
Result The mortality rate was 10.9%(60 cases) and the predicted death rate was 9.5%. The correlation coefficient(r) between observed and expected death rates was .929(p<.01) and SMR was 1.15. Se, Sp, pPv, nPv, and the correct classification rate were .80, .96, .70, .98, and 94.0% respectively. In addition, areas under the curve(AUC) of the receiver operating characteristic(ROC) was 0.954(95% CI=0.919~0.989). According to demographic characteristics, mortality was underestimated in the medical group and overestimated in the surgical group. In addition, the AUCs of ROC curve were generally high in all subgroups.
Conclusion The PIM II showed a good, so it can be utilized for the subject hospital.
-
Citations
Citations to this article as recorded by- The Values of the Pediatric Logistic Organ Dysfunction (PELOD) Score and the Pediatric Index of Mortality (PIM) 2 Score in Emergency Department and Intensive Care Unit
Si Kyoung Jeong, Woon Jeong Lee, Yun Joo Moon, Seon Hee Woo, Yeon Young Kyong, Se Min Choi, Won Jung Jeong, Kyu Nam Park
The Korean Journal of Critical Care Medicine.2010; 25(3): 144. CrossRef - Outcome and risk factors of pediatric hemato-oncology patients admitted in pediatric intensive care unit
Bo Eun Kim, Eun Ju Ha, Keun Wook Bae, Seonguk Kim, Ho Joon Im, Jong Jin Seo, Seong Jong Park
Korean Journal of Pediatrics.2009; 52(10): 1153. CrossRef - Performance effectiveness of pediatric index of mortality 2 (PIM2) and pediatricrisk of mortality III (PRISM III) in pediatric patients with intensive care in single institution: Retrospective study
Hui Seung Hwang, Na Young Lee, Seung Beom Han, Ga Young Kwak, Soo Young Lee, Seung Yun Chung, Jin Han Kang, Dae Chul Jeong
Korean Journal of Pediatrics.2008; 51(11): 1158. CrossRef
- The Values of the Pediatric Logistic Organ Dysfunction (PELOD) Score and the Pediatric Index of Mortality (PIM) 2 Score in Emergency Department and Intensive Care Unit
- 681 View
- 0 Download
- 3 Crossref

- Factors Predicting the Interface Pressure Related to Pressure Injury in Intensive Care Unit Patients
- Ji Seon Shine, Soo Jin Kim, Ji Hyun Lee, Mi Yu
- J Korean Acad Nurs 2017;47(6):794-805. Published online January 15, 2017
- DOI: https://doi.org/10.4040/jkan.2017.47.6.794
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose Interface pressure is a factor that contributes to the occurrence of pressure injuries. This study aimed to investigate interface pressure at common sites of pressure injury (occipital, gluteal and peritrochanteric areas), to explore the relationships among risk factors, skin condition and interface pressure, and to identify risk factors influencing interface pressure.
Methods A total of 100 patients admitted to the intensive care unit were enrolled at a tertiary teaching hospital in Korea. Interface pressure was recorded by a scanning aid device (PalmQ). Patient data regarding age, pulmonary disease, Braden Scale score, body mass index, serum albumin, hemoglobin, mean blood pressure, body temperature, and oxygen saturation were included as risk factors. Data collected from July to September 2016 were analyzed using binary logistic regression.
Results The mean interface pressure of the occipital, gluteal, and right and left peritrochanteric areas were 37.96 (±14.90), 41.15 (±16.04), 53.44 (±24.67), and 54.33 (±22.80) mmHg, respectively. Predictive factors for pressure injuries in the occipital area were age ≥70 years (OR 3.45, 95% confidence interval [CI]: 1.19~9.98), serum albumin deficit (OR 2.88, 95% CI: 1.00~8.26) and body temperature ≥36.5oC (OR 3.12, 95% CI: 1.17~8.17); age ≥70 years (OR 2.81, 95% CI: 1.10~7.15) in the right peritrochanteric area; and body temperature ≥36.5oC (OR 2.86, 95% CI: 1.17~6.98) in the left peritrochanteric area.
Conclusion Our findings suggest that old age, hypoalbuminemia, and high body temperature may be contributory factors to increasing interface pressure; therefore, careful assessment and nursing care of these patients are needed to prevent pressure injury. Further studies are needed to establish cutoff values of interface pressure for patients with pressure ulcers.
-
Citations
Citations to this article as recorded by- Postoperative Mobility and its Relationship with Surgery-Related Pressure Injuries: Incidence and Risk Factors in Bariatric Surgery Patients
Yasemin Uslu, Rabia Tülübaş, Yakup Akyüz, Mustafa Atabey
Obesity Surgery.2026; 36(1): 128. CrossRef - Risk Factors for Pressure Injury in Mechanically Ventilated Patients in Emergency Intensive Care Units: A Prospective Observational Study
Sun Woo Son, Mi Yu
Nursing in Critical Care.2025;[Epub] CrossRef - Innovative air mattress for the prevention of pressure ulcers in neonates
Tino Adrian Jucker, Simon Annaheim, Elodie Morlec, Martin Camenzind, Anna-Barbara Schlüer, Barbara Brotschi, René Michel Rossi
Journal of Wound Care.2024; 33(9): 652. CrossRef - A Prospective, Randomized, Non-inferiority Trial to Compare the Efficacy of 3% Povidone-Iodine Foam Dressing and Silver Foam Dressing in the Treatment of Pressure Injuries
Kyung Hee Park, Kyuwon Baek, Minkyung Kim, Myoung Jean Ju, Won Hee Jung, Yong Soon Yoon
Journal of Wound Management and Research.2023; 19(1): 13. CrossRef - Characteristics and risk factors of nasal mucosal pressure injury in intensive care units
Ruiling Nan, Yujie Su, Juhong Pei, Haixia Chen, Li He, Xinman Dou, Shuling Nan
Journal of Clinical Nursing.2023; 32(1-2): 346. CrossRef - Risk Factors of Endotracheal Intubation-Related Pressure Injury among Patients Admitted to the ICU
Lili Qin, Wenjuan Yun, Cheng Hang
Advances in Skin & Wound Care.2021; 34(3): 144. CrossRef - Impact of Pressure Injuries on Patient Outcomes in a Korean Hospital
Yina Han, Yinji Jin, Taixian Jin, Sun-Mi Lee, Ju-Young Lee
Journal of Wound, Ostomy & Continence Nursing.2019; 46(3): 194. CrossRef - The relationship of subepidermal moisture and early stage pressure injury by visual skin assessment
Chul-Gyu Kim, Seungmi Park, Ji Woon Ko, Sungho Jo
Journal of Tissue Viability.2018; 27(3): 130. CrossRef
- Postoperative Mobility and its Relationship with Surgery-Related Pressure Injuries: Incidence and Risk Factors in Bariatric Surgery Patients
- 1,660 View
- 30 Download
- 8 Crossref

- Development and Evaluation of a Self-Reflection Program for Intensive Care Unit Nurses Who Have Experienced the Death of Pediatric Patients
- Hyun-Ju Kang, Kyung-Sook Bang
- J Korean Acad Nurs 2017;47(3):392-405. Published online January 15, 2017
- DOI: https://doi.org/10.4040/jkan.2017.47.3.392
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose This study aims to develop a self-reflection program for nurses who have experienced the death of pediatric patients in the intensive care unit and to evaluate its effectiveness.
Methods The self-reflection program was developed by means of the following four steps: establishment of the goal through investigation of an initial request, drawing up the program, preliminary research, and implementation and improvement of the program. The study employed a methodological triangulation to evaluate the effectiveness of the program. Participants were 38 nurses who had experienced the death of pediatric patients (experimental group=15, control group=23); they were recruited using convenience sampling. The self-reflection program was provided over 6 weeks (6 sessions). Data were collected from April to August, 2014 and analyzed using t-tests and content analysis.
Results The quantitative results showed that changes in personal growth (t=-6.33,
p <.001) and burnout scores (z=-2.76,p =.005) were better in the experimental group compared to the control group. The qualitative results exhibited two themes, namely “personal growth” and “professional growth”, and ten sub-themes.Conclusion The self-reflection program developed by this study was effective in helping nurses who had experienced the death of pediatric patients to achieve personal growth through self-reflection, and it was confirmed that the program can be applied in a realistic clinical nursing setting. Furthermore, it can be recommended as an intervention program for clinical nurses.
-
Citations
Citations to this article as recorded by- Impact of Work–Life Balance and Nursing Reflection on the Nursing Performance of Nurses in a Tertiary Hospital
Yoo Jin Hwang, Won Hee Jun
International Journal of Nursing Practice.2025;[Epub] CrossRef - Nurses’ perceptions of end-of-life care in neonatal and pediatric intensive care units in Korea: a qualitative descriptive study using thematic analysis
Hyo Jeong Lee, Hyejin Kim
Child Health Nursing Research.2025; 31(4): 272. CrossRef - Improving Intensive End-of-Life Care for Infants and Children: A Scoping Review of Intervention Elements
Elizabeth G. Broden Arciprete, Na Ouyang, Sarah E. Wawrzynski, Ijeoma J. Eche-Ugwu, Janene Batten, Deena K. Costa, Shelli L. Feder, Jennifer M. Snaman
Children.2025; 12(11): 1485. CrossRef - Interventions for Compassion Fatigue in Healthcare Providers—A Systematic Review of Randomised Controlled Trials
Sanjay Patole, Dinesh Pawale, Chandra Rath
Healthcare.2024; 12(2): 171. CrossRef - Effectiveness of End-of-Life Care Debriefing for Intensive Care Unit Nurses
Sook Hyun Park, Jung Eun Lee, Yu-Jin Jung, Ha Neul Yoo, Yeon Su Kim, Young Hee Yi
Journal of Korean Critical Care Nursing.2024; 17(3): 87. CrossRef - Interventions to reduce burnout among clinical nurses: systematic review and meta-analysis
Miran Lee, Chiyoung Cha
Scientific Reports.2023;[Epub] CrossRef - Effectiveness of a critical reflection competency program for clinical nurse educators: a pilot study
Sujin Shin, Inyoung Lee, Jeonghyun Kim, Eunyoung Oh, Eunmin Hong
BMC Nursing.2023;[Epub] CrossRef - Self-reflection of a General Ward Nurses on the Experience of End-of-Life Care for a Patient who Decided to Suspend Life-sustaining Treatment: van Manen's Hermeneutic Phenomenological Approach
Hee Jung Hong
Korean Journal of Adult Nursing.2023; 35(3): 273. CrossRef - Effects of psychological intervention on empathy fatigue in nurses: A meta-analysis
Xiaojuan Chen, Mingdi Chen, Huang Zheng, Chaoyu Wang, Huimin Chen, Qinglan Wu, Huizhao Liao, Jinru Zhu, Junyan Lin, Xudong Ou, Zhihong Zou, Zhiwei Wang, Zhenzhen Zheng, Xianrui Zhuang, Riken Chen
Frontiers in Public Health.2022;[Epub] CrossRef - Predictors of posttraumatic growth of intensive care unit nurses in Korea
Ae Kyung Chang, Hyejin Yoon, Ji Hyun Jang
Japan Journal of Nursing Science.2021;[Epub] CrossRef - Burnout and Resilience After a Decade in Palliative Care: What Survivors Have to Teach Us. A Qualitative Study of Palliative Care Clinicians With More Than 10 Years of Experience
Mervyn Y.H. Koh, Allyn Y.M. Hum, Hwee Sing Khoo, Andy H.Y. Ho, Poh Heng Chong, Wah Ying Ong, Joseph Ong, Patricia S.H. Neo, Woon Chai Yong
Journal of Pain and Symptom Management.2020; 59(1): 105. CrossRef - Neonatal ICU Nurses’ Coping with Death of High Risk Newborn
Yu Mi Kim, Hyu Yong Yoon, Yong-Jun Choi, Dong-Soo Shin
Journal of Health Informatics and Statistics.2019; 44(2): 103. CrossRef - Relationship between Job Stress and Compassion Satisfaction, Compassion Fatigue, Burnout for Nurses in Children’s Hospital
Heekang Choi, Jisun Park, Mijeong Park, Bobae Park, Yeseul Kim
Child Health Nursing Research.2017; 23(4): 459. CrossRef
- Impact of Work–Life Balance and Nursing Reflection on the Nursing Performance of Nurses in a Tertiary Hospital
- 1,857 View
- 29 Download
- 13 Crossref

- Psychological and Physical Health in Family Caregivers of Intensive Care Unit Survivors: Current Knowledge and Future Research Strategies
- JiYeon Choi, Michael P. Donahoe, Leslie A. Hoffman
- J Korean Acad Nurs 2016;46(2):159-167. Published online April 29, 2016
- DOI: https://doi.org/10.4040/jkan.2016.46.2.159
-
 Abstract
Abstract
 PDF
PDF Purpose This article provides an overview of current knowledge on the impact of caregiving on the psychological and physical health of family caregivers of intensive care unit (ICU) survivors and suggestions for future research.
Methods Review of selected papers published in English between January 2000 and October 2015 reporting psychological and physical health outcomes in family caregivers of ICU survivors.
Results In family caregivers of ICU survivors followed up to five years after patients' discharge from an ICU, psychological symptoms, manifested as depression, anxiety and post-traumatic stress disorder, were highly prevalent. Poor self-care, sleep disturbances and fatigue were identified as common physical health problems in family caregivers. Studies to date are mainly descriptive; few interventions have targeted family caregivers. Further, studies that elicit unique needs of families from diverse cultures are lacking.
Conclusion Studies to date have described the impact of caregiving on the psychological and physical health in family caregivers of ICU survivors. Few studies have tested interventions to support unique needs in this population. Therefore, evidence for best strategies is lacking. Future research is needed to identify ICU caregivers at greatest risk for distress, time points to target interventions with maximal efficacy, needs of those from diverse cultures and test interventions to mitigate family caregivers' burden.
-
Citations
Citations to this article as recorded by- Effect of diary intervention on sleep quality and risk of stress disorders among critically ill children in pediatric intensive care units and on their parents’ anxiety level: A randomized controlled trial
Yingshuang He, Yuhong Zhang, Huining Xin, Jinling Lin, Shuting Lin, Sijia Li, Xiao Cheng, Guihua Liu, Jinhua Liao
Intensive and Critical Care Nursing.2026; 93: 104315. CrossRef - The Caregiver Pathway Intervention Can Contribute to Reduced Post-Intensive Care Syndrome Among Family Caregivers of ICU Survivors: A Randomized Controlled Trial
Solbjørg Watland, Lise Solberg Nes, Øivind Ekeberg, Morten Rostrup, Elizabeth Hanson, Mirjam Ekstedt, Una Stenberg, Milada Hagen, Elin Børøsund
Critical Care Medicine.2025; 53(3): e555. CrossRef - Interventions for adult survivors discharged from the intensive care unit: a scoping review
Tong Wu, Fanghong Yan, Guoli Zhang, Rongrong Zhao, Guotian Peng, Ruiyi Sun, Yuxia Ma, Lin Han, Jinping Liu
BMJ Open.2025; 15(8): e096634. CrossRef - Mirror Emotions: A Cross‐Sectional Study of How Patients' Stress, Anxiety and Depression in Critical Care Settings Shape Family Caregivers' Emotional Distress
Asma Alhasani, Zainab Al Kindi, Omar Al Omari, Sulaiman Al Sabei, Hala Mohamed Sanad, Fawwaz Alaloul, Huda Al‐Noumani, Zakariya Al‐Naamani, Mohammad Al Qadire, Mohammed ALBashtawy, Abdullah Alkhawaldeh
Nursing in Critical Care.2025;[Epub] CrossRef - Families’ Experiences Making Decisions across Time and Settings in Chronic Critical Illness
Amanda C. Moale, Chareeni E. Kurukulasuriya, Mikhaila N. Layshock, Svea Cheng, Robert M. Arnold, Renee D. Boss, Bryan J. McVerry, Douglas B. White, Judy C. Chang
Annals of the American Thoracic Society.2025; 22(10): 1539. CrossRef - Family Satisfaction of Polytrauma Patients in Intensive Care Unit at a Tertiary Care Center
Vipin K Singh , Azin Ahmad, Vaibhav Jaiswal
Cureus.2024;[Epub] CrossRef - Does gender moderate resiliency variables and posttraumatic stress symptoms in informal caregivers of neurocritical care patients? An exploratory study
Melissa V. Gates, Ethan G. Lester, Mira Reichman, Ilyssa H. Silverman, Ann Lin, Ana-Maria Vranceanu
Psychology, Health & Medicine.2024; 29(1): 22. CrossRef - Novel Definitions of Wellness and Distress among Family Caregivers of Patients with Acute Cardiorespiratory Failure: A Qualitative Study
Blair Wendlandt, Torrie Edwards, Sherick Hughes, Bradley N. Gaynes, Shannon S. Carson, Laura C. Hanson, Mark Toles
Annals of the American Thoracic Society.2024; 21(5): 782. CrossRef - Integrating Perspectives on Family Caregiving After Critical Illness: A Qualitative Content Analysis
Amanda C. Moale, Erica M. Motter, Peter Eisenhauer, Nimit Gandhi, S. Peter Kim, Tim D. Girard, Charles F. Reynolds, Natalie E. Leland, Judy C. Chang, Leslie P. Scheunemann
American Journal of Critical Care.2024; 33(3): 180. CrossRef - Posttraumatic Stress Symptom Trajectories in Family Caregivers of Patients With Acute Cardiorespiratory Failure
Blair Wendlandt, Liam Pongracz, Feng-Chang Lin, Mark Toles, Bradley N. Gaynes, Laura C. Hanson, Shannon S. Carson
JAMA Network Open.2023; 6(4): e237448. CrossRef - The Caregiver Pathway, a Model for the Systematic and Individualized Follow-up of Family Caregivers at Intensive Care Units: Development Study
Solbjørg Watland, Lise Solberg Nes, Elizabeth Hanson, Mirjam Ekstedt, Una Stenberg, Elin Børøsund
JMIR Formative Research.2023; 7: e46299. CrossRef - Exploring Psychosocial Concerns and Needs of Ventilator and Nonventilator Caregivers in the Emergency and Trauma Care Setting
Tiruchengode R. Kanmani, Birudu Raju, Srikanth Pallerla, Pallavi Mech, Annmary Jacob, Suffi Makkar
Journal of Health and Allied Sciences NU.2023; 13(02): 212. CrossRef - Chronic illness and critical care—A qualitative exploration of family experience and need
Geraldine O'Gara, Theresa Wiseman, Anne‐Marie Doyle, Natalie Pattison
Nursing in Critical Care.2023; 28(4): 574. CrossRef - Sleep Disturbances among Caregivers of Home-Isolated and Hospitalized COVID-19 Patients: A Multi-National Cross-Sectional Study
Nafisa Turabi, Shashi Prabha Tomar, Onyekachi E. Anyagwa, Hanusha Durganaudu, V Ishwarya, Husam Kivan, Magdalena M. Kras, Paraskevi Samouti, Eman Khaled, N Nishitha Ramesh, Amruth S. Krishnegowda, Moshi Moshi Shabani, Miguel A. Palacios-Garay, Fernanda Am
Indian Journal of Community Medicine.2023; 48(5): 676. CrossRef - Relationships among Demographic, Clinical, and Psychological Factors Associated with Family Caregiver Readiness to Participate in Intensive Care Unit Care
Breanna D. Hetland, Natalie S. McAndrew, Kevin A. Kupzyk, Dustin C. Krutsinger, Alison E. Turnbull, Bunny J. Pozehl, Jennifer M. Heusinkvelt
Annals of the American Thoracic Society.2022; 19(11): 1881. CrossRef - Family Caregiver Preferences and Contributions Related to Patient Care in the ICU
Breanna D. Hetland, Natalie S. McAndrew, Kevin A. Kupzyk, Dustin C. Krutsinger, Bunny J. Pozehl, Jennifer M. Heusinkvelt, Courtney E. Camenzind
Western Journal of Nursing Research.2022; 44(3): 214. CrossRef - Psychological Attachment Orientation and Long-Term Posttraumatic Stress Symptoms Among Family Members of ICU Patients
Qiang Zhang, Andrea K. Knies, Jolanta Pach, Tara Kimbrough, Aida Martinez, Prerak Juthani, Stephanie Tu, Joan K. Monin, Ana-Maria Vranceanu, David Y. Hwang
Critical Care Explorations.2022; 4(9): e0753. CrossRef - The effect of short music videos on needs satisfaction and separation anxiety of children's family members during COVID-19: The example of TikTok
Ya-Li Huang, Yu-Kun Chen, Shi-Hao Lin, Hua Cao, Qiang Chen
Frontiers in Pediatrics.2022;[Epub] CrossRef - Interpreting the lived experiences of home caregivers in the families of patients with COVID-19 in Iran: a phenomenological study
Masumeh Akbarbegloo, Mahnaz Sanaeefar
International Journal for Quality in Health Care.2022;[Epub] CrossRef - Experiences of family caregivers of patients with COVID-19
Tahereh Rahimi, Neda Dastyar, Foozieh Rafati
BMC Family Practice.2021;[Epub] CrossRef - Music experience is associated with lower depression level and higher quality of life among family caregivers of critically ill patients
Ga Eul Yoo, Jeongmin Kim, Da In Choi, Myung Sun Yeo, Soo Ji Kim, Sungwon Na
Psychology of Music.2021; 49(4): 901. CrossRef - Posttraumatic Stress Disorder Symptom Trajectories in ICU Family Caregivers
Blair Wendlandt, Yi Tang Chen, Feng-Chang Lin, Mark Toles, Bradley Gaynes, Laura Hanson, Shannon Carson
Critical Care Explorations.2021; 3(4): e0409. CrossRef - Challenges Experienced by Family Caregivers of the Adult Intensive Care Unit Patients in Korea: An Integrative Review
JiYeon Choi, Judith A. Tate, Youn-Jung Son
Clinical Nursing Research.2021; 30(4): 423. CrossRef - Experiencias de pacientes con discapacidades funcionales posteriores al tratamiento en la Unidad de Cuidados Intensivos
Camila Zucato da Silva, Claudinei José Gomes Campos , Michelle Ferraz Martins Jamarim , Gerusa Marcondes Pimentel de Abreu Lima
Revista Cuidarte.2020;[Epub] CrossRef - Family intensive care unit syndrome: An integrative review
Yaser Saeid, MohammadMahdi Salaree, Abbas Ebadi, SeyedTayeb Moradian
Iranian Journal of Nursing and Midwifery Research.2020; 25(5): 361. CrossRef - Review: Post-Intensive Care Syndrome: Unique Challenges in the Neurointensive Care Unit
Jamie Nicole LaBuzetta, Jonathan Rosand, Ana-Maria Vranceanu
Neurocritical Care.2019; 31(3): 534. CrossRef - Family members' satisfaction with care and decision‐making in intensive care units and post‐stay follow‐up needs—a cross‐sectional survey study
Gro Frivold, Åshild Slettebø, Daren K Heyland, Bjørg Dale
Nursing Open.2018; 5(1): 6. CrossRef - The Post-ICU Clinic: Implications for Critical Care Medicine and the Health Care System
Karen A. Korzick, A. Joseph Layon
ASA Monitor.2017; 81(11): 10. CrossRef - Quality of Life and Related Factors Among Patients Discharged from Critical Care Units
Azita Zaheri, Zohre Sadat, Mohamad Abasian, Leila Ghanbari Afra, Mohamad Abdi, Koroosh Joodaki, Masoumeh Sadat Mousavi Sarcheshmeh
Journal of Critical Care Nursing .2017;[Epub] CrossRef
- Effect of diary intervention on sleep quality and risk of stress disorders among critically ill children in pediatric intensive care units and on their parents’ anxiety level: A randomized controlled trial
- 2,644 View
- 29 Download
- 29 Crossref

- Model for Unplanned Self Extubation of ICU Patients Using System Dynamics Approach
- Yu Gil Song, Eun Kyoung Yun
- J Korean Acad Nurs 2015;45(2):280-292. Published online April 30, 2015
- DOI: https://doi.org/10.4040/jkan.2015.45.2.280
-
 Abstract
Abstract
 PDF
PDF Purpose In this study a system dynamics methodology was used to identify correlation and nonlinear feedback structure among factors affecting unplanned extubation (UE) of ICU patients and to construct and verify a simulation model.
Methods Factors affecting UE were identified through a theoretical background established by reviewing literature and preceding studies and referencing various statistical data. Related variables were decided through verification of content validity by an expert group. A causal loop diagram (CLD) was made based on the variables. Stock & Flow modeling using Vensim PLE Plus Version 6.0b was performed to establish a model for UE.
Results Based on the literature review and expert verification, 18 variables associated with UE were identified and CLD was prepared. From the prepared CLD, a model was developed by converting to the Stock & Flow Diagram. Results of the simulation showed that patient stress, patient in an agitated state, restraint application, patient movability, and individual intensive nursing were variables giving the greatest effect to UE probability. To verify agreement of the UE model with real situations, simulation with 5 cases was performed. Equation check and sensitivity analysis on TIME STEP were executed to validate model integrity.
Conclusion Results show that identification of a proper model enables prediction of UE probability. This prediction allows for adjustment of related factors, and provides basic data do develop nursing interventions to decrease UE.
-
Citations
Citations to this article as recorded by- Prediction model for unplanned extubation of thoracoabdominal drainage tube in postoperative inpatients: a retrospective study
Yushu Sun, Xiuping Li, Jia Xu, Xiaojie Zhang, Fanglei Gu, Hongying Pan
European Journal of Medical Research.2025;[Epub] CrossRef - Clinical application and evaluation of a new type of tracheal catheter fixation belt
Fang Niu, Qinghua Liu, Xiaohui Li, Xiang Li
Nursing Open.2023; 10(4): 2593. CrossRef - Incidence of Unplanned Extubation and Related Factors of Reintubation in the Neonatal Intensive Care Unit
Hee Moon Lim, Hyejung Lee, Mi Jung Park, Jeong Eun Shin
Journal of The Korean Society of Maternal and Child Health.2022; 26(2): 72. CrossRef - Design of assessment tool for unplanned endotracheal extubation of artificial airway patients
Ping Zhang, Li‐Ping Liu
Nursing Open.2021; 8(4): 1696. CrossRef - Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study
Hye Jin Yoo, Oak Bun Lim, Jae Lan Shim, Liza Heslop
PLOS ONE.2020; 15(7): e0235694. CrossRef
- Prediction model for unplanned extubation of thoracoabdominal drainage tube in postoperative inpatients: a retrospective study
- 1,292 View
- 16 Download
- 5 Crossref

- Risk Factors for Deliberate Self-extubation
- Young Shin Cho, Jung Hee Yeo
- J Korean Acad Nurs 2014;44(5):573-580. Published online October 31, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.5.573
-
 Abstract
Abstract
 PDF
PDF Purpose This study was conducted to analyze intubation survival rates according to characteristics and to identify the risk factors affecting deliberate self-extubation.
Methods Data were collected from patients' electronic medical reports from one hospital in B city. Participants were 450 patients with endotracheal intubation being treated in intensive care units. The collected data were analyzed using Kaplan-Meier estimation, Log rank test, and Cox's proportional hazards model.
Results Over 15 months thirty-two (7.1%) of the 450 intubation patients intentionally extubated themselves. The patients who had experienced high level of consciousness, agitation. use of sedative, application of restraints, and day and night shift had significantly lower intubation survival rates. Risk factors for deliberate self-extubation were age (60 years and over), unit (neurological intensive care), level of consciousness (higher), agitation, application of restraints, shift (night), and nurse-to-patient ratio (one nurse caring for two or more patients).
Conclusion Appropriate use of sedative drugs, effective treatment to reduce agitation, sufficient nurse-to-patient ratio, and no restraints for patients should be the focus to diminish the number of deliberate self-extubations.
-
Citations
Citations to this article as recorded by- ICU Nurses’ Attitudes, Practices, and Perceived Ethical Dilemmas
Regarding the Application of Physical Restraint Algorithms
Ah-Young Cho, Min-Ji Lee, Hyo-Jung Ban, Eun-Jeong Jun, Min-Jung Choi
Korean Journal of Medical Ethics.2025; 28(3): 229. CrossRef - Results of Applying a Ventilator Weaning Protocol Led by an Advanced Practice Nurse for Cardiac Surgery Patients
YoungJu Eim, Su Jung Choi
Journal of Korean Critical Care Nursing.2024; 17(2): 42. CrossRef - Risk Factors associated with Unplanned Removal of Nasogastric Tubes in Neurocritical Patients
Jaejin Kang, Yang-Sook Yoo
Korean Journal of Adult Nursing.2022; 34(2): 158. CrossRef - Incidence of Unplanned Extubation and Related Factors of Reintubation in the Neonatal Intensive Care Unit
Hee Moon Lim, Hyejung Lee, Mi Jung Park, Jeong Eun Shin
Journal of The Korean Society of Maternal and Child Health.2022; 26(2): 72. CrossRef - Unplanned Extubation as a Prognostic Factor in Critically Ill Patients: A Systematic Review and Meta-analysis
Takeshi Unoki, Hideaki Sakuramoto, Shunsuke Taito, Yuki Kataoka
Annals of Clinical Epidemiology.2021; 3(3): 78. CrossRef - Nurses’ Experiences of Patients’ Safety Accidents
Yujin Hur, Miha Chung, Jinyoung Lee
The Korean Journal of Rehabilitation Nursing.2021; 24(2): 131. CrossRef - Self-extubation in patients with traumatic head injury: Determinants, complications, and outcomes
SaeedA Mahmood, OmaimaS Mahmood, AymanA El-Menyar, MohammadM Asim, AhmedAbdel-Aziz Abdelbari, TalatSaeed Chughtai, HassanA Al-Thani
Anesthesia: Essays and Researches.2019; 13(3): 589. CrossRef - Unplanned Extubation in Patients with Mechanical Ventilation: Experience in the Medical Intensive Care Unit of a Single Tertiary Hospital
Tae Won Lee, Jeong Woo Hong, Jung-Wan Yoo, Sunmi Ju, Seung Hun Lee, Seung Jun Lee, Yu Ji Cho, Yi Yeong Jeong, Jong Deog Lee, Ho Cheol Kim
Tuberculosis and Respiratory Diseases.2015; 78(4): 336. CrossRef
- ICU Nurses’ Attitudes, Practices, and Perceived Ethical Dilemmas
Regarding the Application of Physical Restraint Algorithms
- 1,535 View
- 10 Download
- 8 Crossref

- Pain Perception of Nurses and Pain Expression of Patients in Critical Care Units
- Kyung Hee Bae, Ihn Sook Jeong
- J Korean Acad Nurs 2014;44(4):437-445. Published online August 29, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.4.437
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to identify pain perception (P-PER) by nurses and pain expression (P-EXP) by patients in critical care units (ICUs) and degree of agreement between nurses' P-PER and patients' P-EXP.
Methods Nurses' P-PER was measured with a self-administered questionnaire completed by 99 nurses working in ICUs during May, 2013. Patients' P-EXP was measured with the Critical Care Non-Verbal Pain Scale through observations of 31 ICU patients during nine nursing procedures (NPs) performed between May and July, 2013.
Results Nurses' P-PER was from 4.49 points for nasogastric tube (NGT) insertion to 0.83 for blood pressure (BP) measurement based on a 9-point scale, Patients' P-EXP was 4.48 points for NGT to 0.18 for BP measurement based on a 10-point scale. Eight NPs except oral care showed higher scores for nurses' P-PER than for patients' P-EXP. Position change (
p =.019), subcutaneous injection (p <.001), blood sugar test (p <.001), and BP measurement (p <.001) showed significant differences between nurses' P-PER and patients' P-EXP.Conclusion Nasogastric tube (NGT) insertion was scored highest by both nurses and patients. Eight NPs except 'oral care' showed nurses' P-PER was higher or similar to patients' P-EXP, which indicates that nurses may overestimate procedural pain experienced by patients.
-
Citations
Citations to this article as recorded by- Understanding oral care in the intensive care unit: A qualitative study of nurse experiences and practices with mechanically ventilated patients
Li SuWen, Huang YuYang, Bu Wei
Nursing in Critical Care.2025;[Epub] CrossRef - A Systematic Review on Pain Assessment Tools for Intensive Care Unit Patients
Eun-Jeong Kim, Jiwon Hong, Jiyeon Kang, Na geong Kim, NaRi Kim, Su-Youn Maeng, Hye-Ryeon Park, Min Kyung Ban, Gun Young Yang, Kyung Suk Lee, Eun Hye Jang
Journal of Korean Critical Care Nursing.2020; 13(1): 44. CrossRef - Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU
John W. Devlin, Yoanna Skrobik, Céline Gélinas, Dale M. Needham, Arjen J. C. Slooter, Pratik P. Pandharipande, Paula L. Watson, Gerald L. Weinhouse, Mark E. Nunnally, Bram Rochwerg, Michele C. Balas, Mark van den Boogaard, Karen J. Bosma, Nathaniel E. Bru
Critical Care Medicine.2018; 46(9): e825. CrossRef
- Understanding oral care in the intensive care unit: A qualitative study of nurse experiences and practices with mechanically ventilated patients
- 1,114 View
- 9 Download
- 3 Crossref

- Validation of a Modified Early Warning Score to Predict ICU Transfer for Patients with Severe Sepsis or Septic Shock on General Wards
- Ju Ry Lee, Hye Ran Choi
- J Korean Acad Nurs 2014;44(2):219-227. Published online April 30, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.2.219
-
 Abstract
Abstract
 PDF
PDF Purpose To assess whether the Modified Early Warning Score (MEWS) predicts the need for intensive care unit (ICU) transfer for patients with severe sepsis or septic shock admitted to general wards.
Methods A retrospective chart review of 100 general ward patients with severe sepsis or septic shock was implemented. Clinical information and MEWS according to point of time between ICU group and general ward group were reviewed. Data were analyzed using multivariate logistic regression and the area under the receiver operating characteristic curves with SPSS/WIN 18.0 program.
Results Thirty-eight ICU patients and sixty-two general ward patients were included. In multivariate logistic regression, MEWS (odds ratio [OR] 2.02, 95% confidence interval [CI] 1.43-2.85), lactic acid (OR 1.83, 95% CI 1.22-2.73) and diastolic blood pressure (OR 0.89, 95% CI 0.80-1.00) were predictive of ICU transfer. The sensitivity and the specificity of MEWS used with cut-off value of six were 89.5% and 67.7% for ICU transfer.
Conclusion MEWS is an effective predictor of ICU transfer. A clinical algorithm could be created to respond to high MEWS and intervene with appropriate changes in clinical management.
-
Citations
Citations to this article as recorded by- Predictive performance of clinical scores and survival outcomes in critically ill patients with sepsis: a prospective longitudinal study at a tertiary medical centre in Ethiopia
Girum Tesfaye Kiya, Zeleke Mekonnen, Elsah Tegene Asefa, Edosa Kejela, Edosa Tadasa, Esayas Kebede Gudina, Tilahun Yemane, Gemeda Abebe
PeerJ.2025; 13: e20109. CrossRef - Modified Early Warning Score (MEWS) as a predictor of intensive care unit admission in cancer patient on chemotherapy with positive blood culture: A retrospective cohort study
Jawad Allarakia, Taher Felemban, Amer Alghamdi, Abdullah Ashi, Yousef M. Al Talhi, Ashraf Alsahafi, Abdulfatah Alamri, Mona Aldabbagh
Journal of Infection and Public Health.2023; 16(6): 865. CrossRef - Korean nurses’ perception and performance on communication with physicians in clinical deterioration
Bo-Gyeong Jin, Kyoungrim Kang, Hyun-Jin Cho
Medicine.2022; 101(38): e30570. CrossRef - Job Analysis for Nurse-led Rapid Response Teams in Korea
Ju-Ry Lee, Eui Geum Oh, Eun-Young Yoo
Journal of Korean Academy of Nursing Administration.2021; 27(1): 43. CrossRef - Implementing the National Early Warning Score 2 into pre-registration nurse education
Zoe Abigail Butler
Nursing Standard.2020; 35(3): 70. CrossRef - Derivation and validation of modified early warning score plus SpO2/FiO2 score for predicting acute deterioration of patients with hematological malignancies
Ju-Ry Lee, Youn-Kyoung Jung, Hwa Jung Kim, Younsuck Koh, Chae-Man Lim, Sang-Bum Hong, Jin Won Huh
The Korean Journal of Internal Medicine.2020; 35(6): 1477. CrossRef - Performance of Three Scoring Systems in Predicting Massive Transfusion in Patients with Unstable Upper Gastrointestinal Hemorrhage
Dong Hun Lee, Kyeung Mi Lee, Sung Min Lee, Byung Kook Lee, Yong Soo Cho, Goeun Choi, Seong Woo Yun
Yonsei Medical Journal.2019; 60(4): 368. CrossRef - Implementation of the Surviving Sepsis Campaign guidelines
Vikramjit Mukherjee, Laura Evans
Current Opinion in Critical Care.2017; 23(5): 412. CrossRef - Strengths and limitations of early warning scores: A systematic review and narrative synthesis
C.L. Downey, W. Tahir, R. Randell, J.M. Brown, D.G. Jayne
International Journal of Nursing Studies.2017; 76: 106. CrossRef - Senior Nursing Students' Perceived Competence of Intensive and Critical Care Nursing
Jin-il Kim, Doo Ree Kim, Hyo Nam Lim
The Journal of Korean Academic Society of Nursing Education.2016; 22(2): 115. CrossRef - Temporal changes in physiological parameters of systemic inflammatory response syndrome during the three days prior to a diagnosis of sepsis: a case–control study
HyunSoo Oh, EunKyoung Bae, SeonYoung Lim, JiHye Oh, SunYoung Han, WhaSook Seo
Journal of Clinical Nursing.2016; 25(21-22): 3176. CrossRef - Analysis of Risk Factors to Predict Intensive Care Unit Transfer in Medical in-Patients
Ju Ry Lee, Hye Ran Choi
Journal of Korean Biological Nursing Science.2014; 16(4): 259. CrossRef
- Predictive performance of clinical scores and survival outcomes in critically ill patients with sepsis: a prospective longitudinal study at a tertiary medical centre in Ethiopia
- 1,275 View
- 22 Download
- 12 Crossref

- Risk Factors and Clinical Outcomes for Vancomycin-Resistant Enterococcus Colonization on Intensive Care Unit Admission
- Sook-Jin Byun, Jiyeon Kang
- J Korean Acad Nurs 2013;43(2):287-295. Published online April 30, 2013
- DOI: https://doi.org/10.4040/jkan.2013.43.2.287
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to identify vancomycin-resistant enterococcus (VRE) colonization rate in patients admitted to the intensive care unit (ICU), associated risk factors and clinical outcomes for VRE colonization.
Methods Of the 7,703 patients admitted to the ICUs between January, 2008 and December, 2010, medical records of 554 VRE colonized and 503 uncolonized patients were reviewed retrospectively. To analyzed the impact of colonization on patients' clinical outcomes, 199 VRE colonized patients were matched with 199 uncolonized patients using a propensity score matching method.
Results During the study period, 567 (7.2%) of the 7,703 patients were colonized with VRE. Multivariate analysis identified the following independent risk factors for VRE colonization: use of antibiotics (odds ratio [OR]=3.33), having bedsores (OR=2.92), having invasive devices (OR=2.29), methicillin-resistant Staphylococcus aureus co-colonization (OR=1.84), and previous hospitalization (OR=1.74). VRE colonized patients were more likely to have infectious diseases than uncolonized patients. VRE colonization was associated with prolonged hospitalization and higher mortality.
Conclusion Strict infection control program including preemptive isolation for high-risk group may be helpful. Further research needs to be done to investigate the effects of active surveillance program on the incidence of colonization or infection with VRE in the ICU.
-
Citations
Citations to this article as recorded by- Vancomycin Resistant Enterococci Prevalence, Antibiotic Susceptibility Patterns and Colonization Risk Factors Among HIV-Positive Patients in Health-Care Facilities in Debre Berhan Town, Ethiopia
Mikiyas Zike, Abdurahaman Ahmed, Awraris Hailu, Bedru Hussien
Infection and Drug Resistance.2024; Volume 17: 17. CrossRef - Previous antibiotic therapy as independent risk factor for the presence of vancomycin-resistant enterococci in surgical inpatients. Results from a matched case-control study
Philip MacKenzie, Jacqueline Färber, Marius Post, Torben Esser, Lukas Bechmann, Siegfried Kropf, Roland Croner, Gernot Geginat
BMC Infectious Diseases.2023;[Epub] CrossRef - Steady Inflow of Vancomycin-Resistant Enterococci from Outside a Hospital
Hye-sun An, Sang-Won Park, Su-hui Ko, Ji Hwan Bang
Korean Journal of Healthcare-Associated Infection Control and Prevention.2017; 22(2): 63. CrossRef - Vancomycin-resistant Enterococcus colonization in the intensive care unit: Clinical outcomes and attributable costs of hospitalization
Euihan Jung, Sookjin Byun, Hojin Lee, Sang Yi Moon, Hyuck Lee
American Journal of Infection Control.2014; 42(10): 1062. CrossRef
- Vancomycin Resistant Enterococci Prevalence, Antibiotic Susceptibility Patterns and Colonization Risk Factors Among HIV-Positive Patients in Health-Care Facilities in Debre Berhan Town, Ethiopia
- 1,158 View
- 2 Download
- 4 Crossref

- Verification of Validity of MPM II for Neurological Patients in Intensive Care Units
- Heejeong Kim, Kyunghee Kim
- J Korean Acad Nurs 2011;41(1):92-100. Published online February 28, 2011
- DOI: https://doi.org/10.4040/jkan.2011.41.1.92
-
 Abstract
Abstract
 PDF
PDF Purpose Mortality Provability Model (MPM) II is a model for predicting mortality probability of patients admitted to ICU. This study was done to test the validity of MPM II for critically ill neurological patients and to determine applicability of MPM II in predicting mortality of neurological ICU patients.
Methods Data were collected from medical records of 187 neurological patients over 18 yr of age who were admitted to the ICU of C University Hospital during the period from January 2008 to May 2009. Collected data were analyzed through χ2 test, t-test, Mann-Whiteny test, goodness of fit test, and ROC curve.
Results As to mortality according to patients' general and clinically related characteristics, mortality was statistically significantly different for ICU stay, hospital stay, APACHE III score, APACHE predicted death rate, GCS, endotracheal intubation, and central venous catheter. Results of Hosmer-Lemeshow goodness-of-fit test were MPM II0 (χ2=0.02,
p =.989), MPM II24 (χ2=0.99p =.805), MPM II48 (χ2=0.91,p =.822), and MPM II72 (χ2=1.57,p =.457), and results of the discrimination test using the ROC curve were MPM II0, .726 (p <.001), MPM II24, .764 (p <.001), MPM II48, .762 (p <.001), and MPM II72, .809 (p <.001).Conclusion MPM II was found to be a valid mortality prediction model for neurological ICU patients.
-
Citations
Citations to this article as recorded by- Development of a patient classification system for critical care nursing based on nursing intensity
Yukyung Ko, Bohyun Park, Hanju Lee, Donghwan Kim
International Journal of Nursing Practice.2023;[Epub] CrossRef - Validation Study of the Estimated Glycemic Load Model Using Commercially Available Fast Foods
Miran Lee, Haejin Kang, Sang-Jin Chung, Kisun Nam, Yoo Kyoung Park
Frontiers in Nutrition.2022;[Epub] CrossRef - Comparison of acute physiology and chronic health evaluation II and Glasgow Coma Score in predicting the outcomes of Post Anesthesia Care Unit's patients
Mohammad Hosseini, Jamileh Ramazani
Saudi Journal of Anaesthesia.2015; 9(2): 136. CrossRef - Evaluation of Critical Patient Severity Classification System(CPSCS) for neurocritical patients in intensive unit
Hee-Jeonh Kim
Journal of the Korea Academia-Industrial cooperation Society.2012; 13(11): 5238. CrossRef
- Development of a patient classification system for critical care nursing based on nursing intensity
- 1,006 View
- 4 Download
- 4 Crossref

- Factors Influencing Relocation Stress Syndrome in Patients Following Transfer from Intensive Care Units
- Jin-Hee Park, Moon-Sook Yoo, Youn-Jung Son, Sun Hyoung Bae
- J Korean Acad Nurs 2010;40(3):307-316. Published online June 30, 2010
- DOI: https://doi.org/10.4040/jkan.2010.40.3.307
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to identify the levels of relocation stress syndrome (RSS) and influencing the stress experienced by Intensive Care Unit (ICU) patients just after transfer to general wards.
Methods A cross-sectional study was conducted with 257 patients who transferred from the intensive care unit. Data were collected through self-report questionnaires from May to October, 2009. Data were analyzed using the Pearson correlation coefficient, t-test, one-way ANOVA, and stepwise multiple linear regression with SPSS/WIN 12.0.
Results The mean score for RSS was 17.80±9.16. The factors predicting relocation stress syndrome were symptom experience, differences in scope and quality of care provided by ICU and ward nursing staffs, satisfaction with transfer process, length of stay in ICU and economic status, and these factors explained 40% of relocation stress syndrome (F=31.61,
p <.001).Conclusion By understanding the stress experienced by ICU patients, nurses are better able to provide psychological support and thus more holistic care to critically ill patients. Further research is needed to consider the impact of relocation stress syndrome on patients' health outcomes in the recovery trajectory.
-
Citations
Citations to this article as recorded by- A phenomenological study on the experiences of patient transfer from the intensive care unit to general wards
Eun-Young Lee, Jin-Hee Park, Alvisa Palese
PLOS ONE.2021; 16(7): e0254316. CrossRef - Development and psychometric evaluation of the Relocation Stress Syndrome Scale-Short Form for patients transferred from adult intensive care units to general wards
Mi Hwa Won, Youn-Jung Son
Intensive and Critical Care Nursing.2020; 58: 102800. CrossRef - Development and Effects of a Transition Nursing Program for Patients and Family Caregivers at a Neurological ICU in Korea
Sun Hee Yun, Eui Geum Oh, Yang Sook Yoo, So Sun Kim, Yeon Soo Jang
Clinical Nursing Research.2017; 26(1): 27. CrossRef - The Effects of Aromatherapy on Intensive Care Unit Patients’ Stress and Sleep Quality: A Nonrandomised Controlled Trial
Eun Hee Cho, Mi-Young Lee, Myung-Haeng Hur, Nativ Dudai
Evidence-Based Complementary and Alternative Medicine.2017;[Epub] CrossRef - A tailored relocation stress intervention programme for family caregivers of patients transferred from a surgical intensive care unit to a general ward
Seul Lee, HyunSoo Oh, YeonOk Suh, WhaSook Seo
Journal of Clinical Nursing.2017; 26(5-6): 784. CrossRef - Clinical validity of a relocation stress scale for the families of patients transferred from intensive care units
HyunSoo Oh, Seul Lee, JiSun Kim, EunJu Lee, HyoNam Min, OkJa Cho, WhaSook Seo
Journal of Clinical Nursing.2015; 24(13-14): 1805. CrossRef
- A phenomenological study on the experiences of patient transfer from the intensive care unit to general wards
- 1,425 View
- 12 Download
- 6 Crossref

- Development of Nursing Key Performance Indicators for an Intensive Care Unit by using a Balanced Scorecard
- Yun Jeong Choi, Ji Young Lim, Young Whee Lee, Hwa Soon Kim
- J Korean Acad Nurs 2008;38(5):656-666. Published online October 12, 2008
- DOI: https://doi.org/10.4040/jkan.2008.38.5.656
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to develop visions of nursing service, nursing strategies and key performance indicators (KPIs) for an intensive care unit (ICU) based on a Balanced Scorecard (BSC).
Methods This study was undertaken by using methodological research. The development process consisted of four phases; the first phase was to develop the vision of nursing in ICUs. The second phase was to develop strategies according to 4 perspectives of a BSC. The third phase was to develop KPIs according to the 4 perspectives of BSC and the final phase was to combine the nursing visions, strategies and KPIs of ICUs.
Results Two main visions of nursing service for ICUs were established. These were ‘realization of harmonized professional nursing with human respect’ and ‘recovery of health through specialized nursing’ respectively. In order to reach the aim of developing nursing visions, thirteen practical strategies and nineteen KPIs were developed by four perspectives of the BSC.
Conclusion The results will be used as objective fundamental data to attain business outcomes for the achievement of nursing visions and strategies of ICUs.
-
Citations
Citations to this article as recorded by- Development of Performance Indicators for Clinical Research Coordinators Using the Balanced Scorecard in South Korea
Youn Sun Hwang, Tae Wha Lee
Therapeutic Innovation & Regulatory Science.2019; : 216847901987075. CrossRef - Augmenting Walkability, Visibility and Arrangement for Korean ICU
Javaria Manzoor Shaikh
Sir Syed University Research Journal of Engineering & Technology.2015; 5(1): 20. CrossRef - Development and Application of a Performance Prediction Model for Home Care Nursing Based on a Balanced Scorecard using the Bayesian Belief Network
Wonjung Noh, GyeongAe Seomun
Journal of Korean Academy of Nursing.2015; 45(3): 429. CrossRef - Testing The Healing Environment Conditions for Nurses with two Independent Variables: Visibility Enhancement along with Shortening the Walking Distance of the Nurses to Patient - Focused on LogWare stop sequence and space syntax for U-Shape, L- Shape and
Javaria Manzoor Shaikh, Jae Seung Park
KIEAE Journal.2015; 15(2): 19. CrossRef - Barrier free visibility for staff in ICU Focused on space syntax for circulation in Asian ICU
Javaria Manzoor Shaikh
Sir Syed University Research Journal of Engineering & Technology.2014; 4(1): 9. CrossRef
- Development of Performance Indicators for Clinical Research Coordinators Using the Balanced Scorecard in South Korea
- 1,548 View
- 17 Download
- 4 Web of Science
- 5 Crossref

- Concept Analysis of Relocation Stress - Focusing on Patients Transferred from Intensive Care Unit to General Ward -
- Youn-Jung Son, Sung-Kyung Hong, Eun Young Jun
- J Korean Acad Nurs 2008;38(3):353-362. Published online June 30, 2008
- DOI: https://doi.org/10.4040/jkan.2008.38.3.353
-
 Abstract
Abstract
 PDF
PDF Purpose This study was conducted to analyze and clarify the meaning of the concept for relocation stress-focusing on patients transferred from an intensive care unit to a general ward.
Methods This study used Walker and Avant's process of concept analysis.
Results Relocation stress can be defined by these attributes as follows: 1) involuntary decision about relocation, 2) moving from a familiar and safe environment to an unfamiliar one, 3) broken relationship of safety and familiarity, 4) physiological and psychosocial change after relocation. The antecedents of relocation stress consisted of these facts: 1) preparation degrees of transfer from the intensive care unit to a general ward, 2) pertinence of the information related to the transfer process, 3) change of major caregivers, 4) change in numbers of monitoring devices, 5) change in the level of self-care. There are consequences occurring as a result of relocation stress: 1) decrease in patients' quality of life, 2) decrease in coping capacity, 3) loss of control.
Conclusion Relocation stress is a core concept in intensive nursing care. Using this concept will contribute to continuity of intensive nursing care.
-
Citations
Citations to this article as recorded by- Suicidal ideation and self-destructive behavior in Vietnamese adolescents and young adults with psychiatric disorders
Thi To Uyen Duong, Nguyen Ngoc Tran, Thi Anh Thoa Nguyen, Van Hai Nguyen, Lam Vu Tran, Van Thich Pham, Thu Ha Nguyen, Thi Thu Cao, My Ha Tran, Thanh Tung Pham, Le Tuan Linh Hoang, Danh Khai Duong
Discover Psychology.2025;[Epub] CrossRef - Transfer anxiety in parents of children transferred from pediatric intensive care units to general wards in South Korea: a hybrid concept analysis
Jisu Park, Eun Kyoung Choi
Child Health Nursing Research.2022; 28(2): 154. CrossRef - Development and psychometric evaluation of the Relocation Stress Syndrome Scale-Short Form for patients transferred from adult intensive care units to general wards
Mi Hwa Won, Youn-Jung Son
Intensive and Critical Care Nursing.2020; 58: 102800. CrossRef - A tailored relocation stress intervention programme for family caregivers of patients transferred from a surgical intensive care unit to a general ward
Seul Lee, HyunSoo Oh, YeonOk Suh, WhaSook Seo
Journal of Clinical Nursing.2017; 26(5-6): 784. CrossRef - Clinical validity of a relocation stress scale for the families of patients transferred from intensive care units
HyunSoo Oh, Seul Lee, JiSun Kim, EunJu Lee, HyoNam Min, OkJa Cho, WhaSook Seo
Journal of Clinical Nursing.2015; 24(13-14): 1805. CrossRef
- Suicidal ideation and self-destructive behavior in Vietnamese adolescents and young adults with psychiatric disorders
- 1,102 View
- 10 Download
- 5 Crossref

- Risk Factors for Nosocomial Urinary Tract Infection in the Intensive Care Unit with a Positive Urine Culture and Foley Catheterization
- Seong Mi Yu, Kyung Yeon Park
- Journal of Korean Academy of Nursing 2007;37(7):1149-1158. Published online December 31, 2007
- DOI: https://doi.org/10.4040/jkan.2007.37.7.1149
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to identify the risk factors for a nosocomial urinary tract infection in intensive care units with a foley catheterization which showed a positive urine culture.
Method Three-hundred eighty-seven patients were included in the study. A retrospective review of the electrical medical record system's databases and medical record sheets in hospitalized patients from January 2003 to December 2003 was used. The collected data was analyzed by descriptive statistics, t-test, chi-square test and logistic regression analysis.
Result The frequency of the participants' nosocomial urinary tract infection was 72.9%. Significant risk factors for a nosocomial urinary tract infection were ‘age’, ‘place of catheter insertion’, ‘frequency of catheter change’, and ‘duration of catheterization’. These variables explained 18.4% of variance in the experience of nosocomial urinary tract infection in intensive care units with foley catheterization.
Conclusion Medical personnel can decrease the incidence of a nosocomial urinary tract infection by recognizing and paying attention to the duration of catheterization, frequency of catheter change, and place of catheter insertion. As a result, specific and scrupulous strategies should be developed to reflect these factors for decreasing nosocomial urinary tract infections.
-
Citations
Citations to this article as recorded by- Epidemiology and Resistance Patterns of Bacterial Pathogens in Urinary Tract Infections in the Northern Gyeonggi-do Area during 2007-2011
Eunyoung Oh, Hyukmin Lee, Hwan Sub Lim, Younhee Park
Laboratory Medicine Online.2013; 3(1): 34. CrossRef - Effects of perineal care in preventing catheter associated urinary tract infections (CAUTI) in intensive care units (ICU)
Jeong-Sil Choi, Jeong-Hwa Yeon
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(2): 223. CrossRef
- Epidemiology and Resistance Patterns of Bacterial Pathogens in Urinary Tract Infections in the Northern Gyeonggi-do Area during 2007-2011
- 813 View
- 5 Download
- 2 Crossref

- Variations in Nurse Staffing in Adult and Neonatal Intensive Care Units
- Sung Hyun Cho, Jeong Hae Hwang, Yun Mi Kim, Jae Sun Kim
- Journal of Korean Academy of Nursing 2006;36(5):691-700. Published online August 31, 2006
- DOI: https://doi.org/10.4040/jkan.2006.36.5.691
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to analyze variations in unit staffing and recommend policies to improve nursing staffing levels in intensive care units (ICUs).
Method A cross-sectional study design was used, employing survey data from the Health Insurance Review Agency conducted from June-July, 2003. Unitstaffing was measured using two indicators; bed-to-nurse (B/N) ratio (number of beds per nurse), and patient-to-nurse (P/N)ratio (number of average daily patients per nurse). Staffing levels were compared according to hospital and ICU characteristics.
Result A total of 414 institutions were operating 569 adult and 86 neonatal ICUs. Tertiary hospitals (n=42) had the lowest mean B/N (0.82) and P/N (0.76) ratios in adult ICUs, followed by general hospitals (B/N: 1.34, P/N: 0.97). Those ratios indicated that a nurse took care of 3 to 5 patients per shift. Neonatal ICUs had worse staffing and had greater variations in staffing ratios than adult ICUs. About 17% of adult and 26% of neonatal ICUs were staffed only by adjunct nurses who had responsibility for a general ward as well as the ICU.
Conclusion Stratification of nurse staffing levels and differentiation of ICU utilization fees based on staffing grades are recommended as a policy tool to improve nurse staffing in ICUs.
-
Citations
Citations to this article as recorded by- Development of a competency for professional oral hygiene care of endotracheally-intubated patients in the intensive care unit: development and validity evidence
Eun-Sil Choi, Hie-Jin Noh, Won-Gyun Chung, So-Jung Mun
BMC Health Services Research.2021;[Epub] CrossRef - Associated Factors with Performance of Infection Control for the Prevention of Ventilator-associated Pneumonia among Some Intensive Care Unit Nurses
Hyeon Hwa Lee, Mi Ah Han, Jong Park, Seong Woo Choi
Journal of Health Informatics and Statistics.2018; 43(1): 1. CrossRef - Influencing Factors on Nursing Practices for Healthcare-associated Infections Control in Intensive Care Unit
Soon Ok Kim, Jin Suk Ra
Korean Journal of Healthcare-Associated Infection Control and Prevention.2018; 23(2): 39. CrossRef - The Study of Preceptor Nurses’ Occupational Stress and Burden
Joohee Han, Eun Kwang Yoo
Korean Journal of Stress Research.2018; 26(1): 38. CrossRef - Financial Projection of the Nursing Fee Differentiation Policy Improvement Proposal in the National Health Insurance: Using a Break-even Analysis Model for the Optimal Nursing Fee
Sungjae Kim, Jinhyun Kim
Journal of Korean Academy of Nursing Administration.2013; 19(5): 565. CrossRef - Nurse Staffing and Patient Mortality in Intensive Care Units
Sung-Hyun Cho, Jeong Hae Hwang, Jaiyong Kim
Nursing Research.2008; 57(5): 322. CrossRef
- Development of a competency for professional oral hygiene care of endotracheally-intubated patients in the intensive care unit: development and validity evidence
- 1,018 View
- 6 Download
- 6 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


