Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 41(1); 2011 > Article
-
Original Article
- Verification of Validity of MPM II for Neurological Patients in Intensive Care Units
- Heejeong Kim, Kyunghee Kim
-
Journal of Korean Academy of Nursing 2011;41(1):92-100.
DOI: https://doi.org/10.4040/jkan.2011.41.1.92
Published online: February 28, 2011
1Full-time Lecturer, Department of Nursing, Namseoul University, Cheonan, Korea.
2Professor, Department of Nursing, Chung-Ang University, Seoul, Korea.
- Address reprint requests to: Kim, Kyunghee. Department of Nursing, Chung-Ang University, 29 Heukseong-no, Dongjak-gu, Seoul 155-756, Korea. Tel: +82-2-820-5670, Fax: +82-2-824-7961, kyung@cau.ac.kr
© 2011 Korean Society of Nursing Science
Abstract
-
Purpose
- Mortality Provability Model (MPM) II is a model for predicting mortality probability of patients admitted to ICU. This study was done to test the validity of MPM II for critically ill neurological patients and to determine applicability of MPM II in predicting mortality of neurological ICU patients.
-
Methods
- Data were collected from medical records of 187 neurological patients over 18 yr of age who were admitted to the ICU of C University Hospital during the period from January 2008 to May 2009. Collected data were analyzed through χ2 test, t-test, Mann-Whiteny test, goodness of fit test, and ROC curve.
-
Results
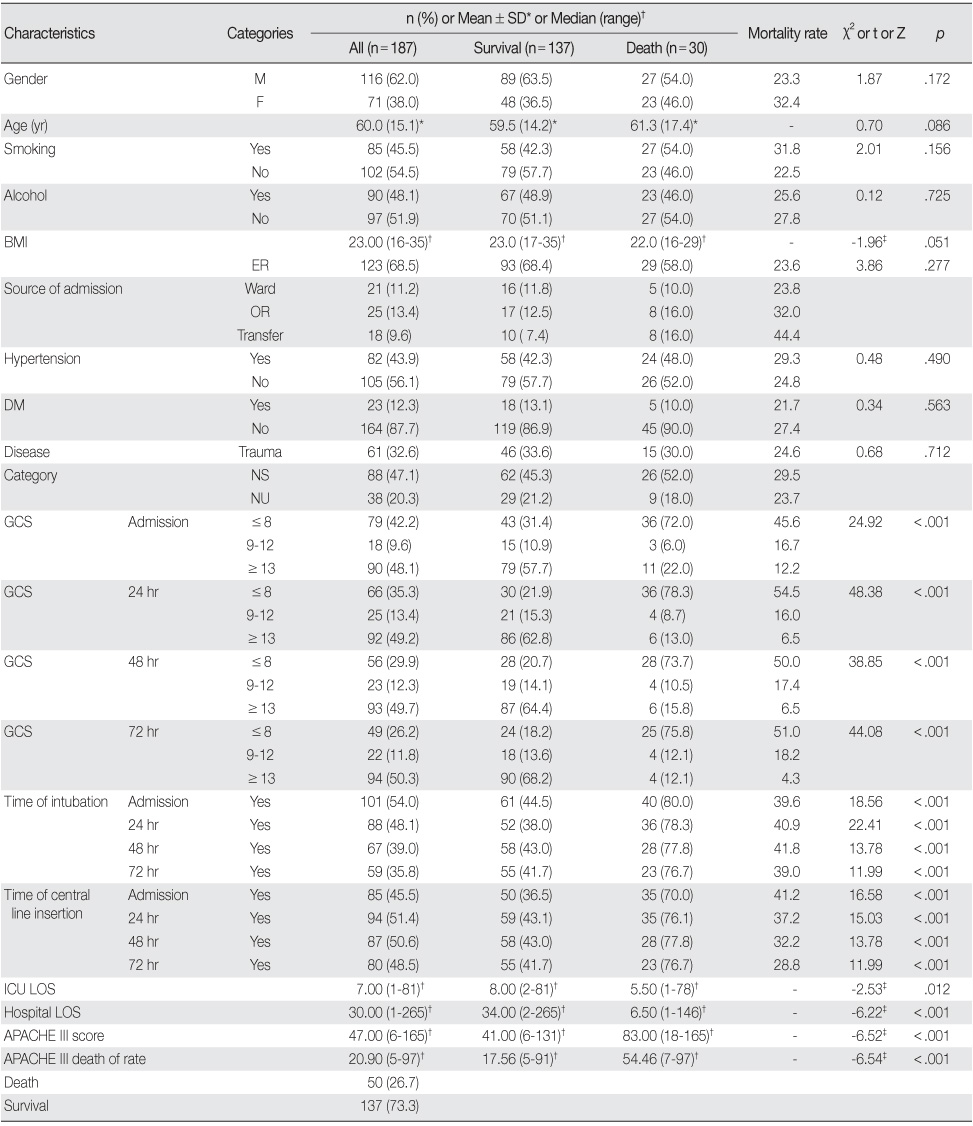
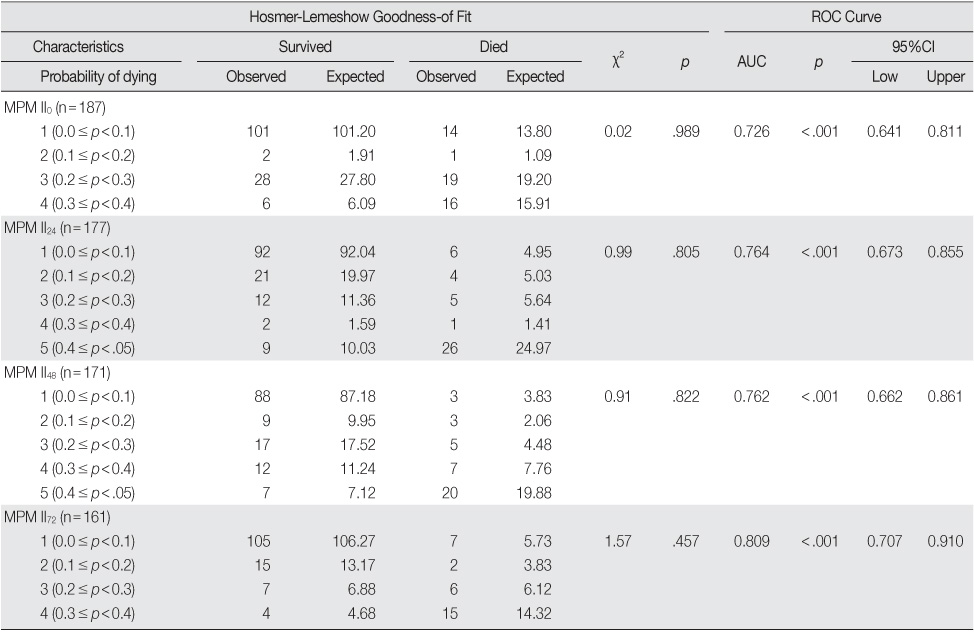
- As to mortality according to patients' general and clinically related characteristics, mortality was statistically significantly different for ICU stay, hospital stay, APACHE III score, APACHE predicted death rate, GCS, endotracheal intubation, and central venous catheter. Results of Hosmer-Lemeshow goodness-of-fit test were MPM II0 (χ2=0.02, p=.989), MPM II24 (χ2=0.99 p=.805), MPM II48 (χ2=0.91, p=.822), and MPM II72 (χ2=1.57, p=.457), and results of the discrimination test using the ROC curve were MPM II0, .726 (p<.001), MPM II24, .764 (p<.001), MPM II48, .762 (p<.001), and MPM II72, .809 (p<.001).
-
Conclusion
- MPM II was found to be a valid mortality prediction model for neurological ICU patients.
- 1. Ahn ST, Kim AJ, Baek KJ, Lee JH, Han SB, Shin DW, et al. Mortality analysis of intensive care units patients using Mortality Probability Models (MPM II). Journal of the Korean Society of Traumatology. 2001;14:101–107.
- 2. Cazali I, Ramirez F, Mejia C, Ramirez C, Silvestre M, Gordillo R. Clinical correlates of Mortality Probability Models MPM II and the outcome of a Burkholderia cepacia bacteraemia outbreak in an intensive care unit in Guatemala, Central America. International Journal of Antimicrobial Agents. 2007;29:Suppl. 2. S658. Article
- 3. Glance LG, Osler TM, Dick AW. Identifying quality outliers in a large, multiple-institution database by using customized versions of the simplified acute physiology score II and the Mortality Probability Model II0. Critical Care Medicine. 2002;30:1995–2002.ArticlePubMed
- 4. Healthcare Policy Korean Medical Association Research Institute. Sources of analysis of the OECD health data 2007. 2007;12;(issue Brief No 3):Seoul, Research Institute for Healthcare Policy.
- 5. Janssens U, Graf J, Dujardin R, Kersten A, Ortlepp J, Merx M, Koch KC, et al. Mortality Probability Model II (MPM0-72) in 1667 patients with acute cardiovascular disorders. Critical Care. 2002;6:Suppl. 1. 239.
- 6. Jo Y. Clinical analysis of the prognosis in the spontaneous potine hemorrhage. 2001;Seoul, Chung-Ang University. Unpublished master's thesis.
- 7. Kim EK, Kwon YD, Hwang JH. Comparing the performance of three severity scoring system for ICU patients: APACHE III, SAPS II, MPM II. Journal of Preventive Medicine and Public Health. 2005;38:276–282.PubMed
- 8. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–1636.ArticlePubMed
- 9. Knaus WA, Wagner DP, Zimmerman JE, Draper EA. Variation in mortality and length of stay in intensive care unit. Annals of Internal Medicine. 1993;118:753–761.PubMed
- 10. Lee DG, Chun HS, Yim DS, Choi SM, Choi JH, Yoo JH, et al. Efficacy of Vancomycin, Arbekacin, and Gentamicin alone or in combination against Methicillin-Resistant Staphylococcus aureus in an in Vitro Infective Endocarditis Model. Infection and Chemotherapy. 2003;35:145–153.
- 11. Lemeshow S, Klar J, Teres D, Avrunin JS, Gehlbach SH, Rapoport J, et al. Mortality Probability Models for patients in the intensive care unit for 48 or 72 hrs: A prospective multicenter study. Critical Care Medicine. 1994;22:1351–1358.ArticlePubMed
- 12. Lemeshow S, Teres D, Avrunin JS, Gage RW. Refining intensive care unit outcome prediction by using changing probabilities of mortality. Critical Care Medicine. 1988;16:470–477.ArticlePubMed
- 13. Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J. Mortality Probability Models(MPM II) based on an international cohort of intensive care unit patients. JAMA. 1993;270:2478–2486.ArticlePubMed
- 14. Murray JA, Demetriades D, Berne TV, Strattion SJ, Cryer HG, Bongard F, et al. Prehospital intubation in patients with severe head injury. The Journal of Trauma. 2000;49:1065–1070.ArticlePubMed
- 15. Patel PA, Grant BJ. Application of mortality prediction systems to individual intensive care units. Intensive Care Medicine. 1999;25:977–982.ArticlePubMedPDF
- 16. Rovlias A, Kotsou S. Classification and regression tree for prediction of outcome after severe head injury using simple clinical and laboratory variables. Journal of Neurotrauma. 2004;21:886–893.ArticlePubMed
- 17. Rue M. Interobserver variability of the measurement of the mortality probability models (MPM II) in the assessment of severity of illness. Intensive Care Medicine. 2000;26:286–291.ArticlePubMedPDF
- 18. Ruė M, Artigas A, Alvarez M, Quintana S., Valero C. Performance of the Mortality Probability Models in assessing severity of illness during the first week in the intensive care unit. Critical Care Medicine. 2000;28:2819–2824.ArticlePubMed
- 19. Ruė M, Quintana S, Alvarez M, Artigas A. Daily assessment of severity of illness and mortality prediction for individual patients. Critical Care Medicine. 2001;29:45–50.ArticlePubMed
- 20. Sicignano A, Carozzi C, Giudici D, Merli G, Arlati S, Pulici M. The influence of length of stay in the ICU on power of discrimination of a multipurpose severity score (SAPS). ARCHIDIA. Intensive Care Medicine. 1996;22:1048–1051.ArticlePubMed
- 21. Siempos II, Kopterides P, Tsangaris I, Dimopoulou I, Armaganidis AE. Impact of catheter-related bloodstream infection on the mortality of critically ill patients: A-meta analysis. Critical Care Medicine. 2009;37:2283–2289.ArticlePubMed
- 22. Suarez JI. Outcome in neurocritical care: Advances in monitoring and treatment and effect of a specialized neurocritical care team. Critical Care Medicine. 2006;34:9 Suppl. S232–S238.ArticlePubMed
- 23. Suistomaa M, Niskanen N, Kari A, Hynynen M, Takala J. Customized prediction models based on APACHE II and SAPS II scores in patients with prolonged length of stay in the ICU. Intensive Care Medicine. 2002;28:479–485.PubMed
- 24. Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–1293.ArticlePubMed
- 25. Teasdale G, Jennet B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84.PubMed
- 26. Wagner DP, Knaus WA, Harrell FE, Zimmerman J.E., Watts C. Daily prognostic estimates for critically ill adults in intensive care units: Results from a prospective, multicenter, inception cohort analysis. Critical Care Medicine. 1994;22:1359–1372.ArticlePubMed
- 27. Yeon BH. Comparison of predict mortality scoring system for spontaneous intracerebral hemorrhage patients. 2005;Daejeon, Eulji University. Unpublished master's thesis.
- 28. You SM. Effectiveness of the surveillance of central venous catheter-related bloodstream infection in an ICU. 2001;Seoul, Seoul National University. Unpublished doctoral dissertation.
REFERENCES
Figure & Data
REFERENCES
Citations

- Development of a patient classification system for critical care nursing based on nursing intensity
Yukyung Ko, Bohyun Park, Hanju Lee, Donghwan Kim
International Journal of Nursing Practice.2023;[Epub] CrossRef - Validation Study of the Estimated Glycemic Load Model Using Commercially Available Fast Foods
Miran Lee, Haejin Kang, Sang-Jin Chung, Kisun Nam, Yoo Kyoung Park
Frontiers in Nutrition.2022;[Epub] CrossRef - Comparison of acute physiology and chronic health evaluation II and Glasgow Coma Score in predicting the outcomes of Post Anesthesia Care Unit's patients
Mohammad Hosseini, Jamileh Ramazani
Saudi Journal of Anaesthesia.2015; 9(2): 136. CrossRef - Evaluation of Critical Patient Severity Classification System(CPSCS) for neurocritical patients in intensive unit
Hee-Jeonh Kim
Journal of the Korea Academia-Industrial cooperation Society.2012; 13(11): 5238. CrossRef
General and Clinical Characteristics and Difference of Mortality according to General and Clinical Characteristics (N=187)
*Mean±SD; †Median (range); ‡Z value of Mann-Whitney test.
BMI=Body Mass Index; ER=Emergency Room; OR=Operating Room; DM=Diabetes Mellitus; NS=Neurosurgery; NU=Neurology; GCS=Glasgow Coma Scale; ICU= Intensive Care Unit; LOS=Length of Stay.
Hosmer-Lemeshow Goodness-of Fit Test and ROC Curve for MPM II
ROC=Receiver operating characteristic; AUC=Area under the curve; CI =Confidence Interval.
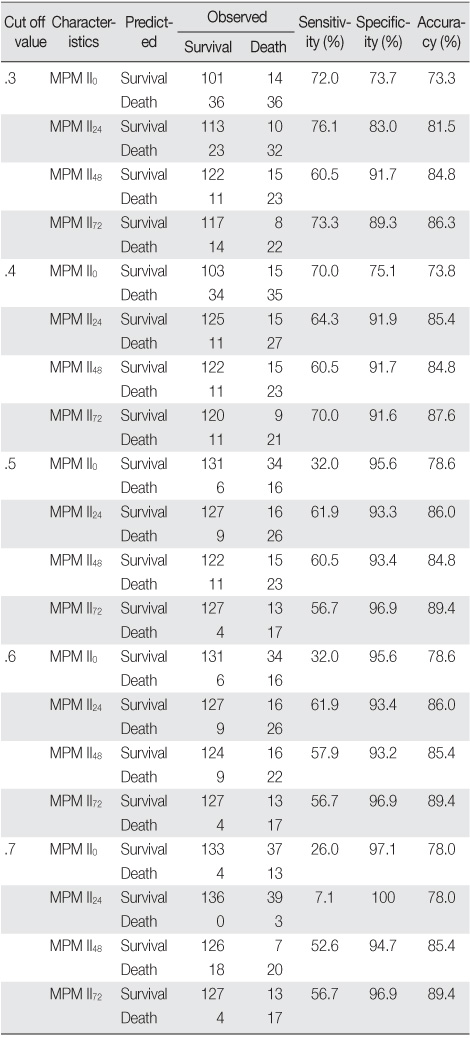
Comparison of Sensitivity, Specificity, and Accuracy of the MPM II0, 24, 48, 72. at Decision Thresholds of 0.3, 0.4, 0.5, 0.6 and 0.7
*Mean±SD; †Median (range); ‡Z value of Mann-Whitney test. BMI=Body Mass Index; ER=Emergency Room; OR=Operating Room; DM=Diabetes Mellitus; NS=Neurosurgery; NU=Neurology; GCS=Glasgow Coma Scale; ICU= Intensive Care Unit; LOS=Length of Stay.
ROC=Receiver operating characteristic; AUC=Area under the curve; CI =Confidence Interval.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

