Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 44(4); 2014 > Article
-
Original Article
- Pain Perception of Nurses and Pain Expression of Patients in Critical Care Units
- Kyung Hee Bae, Ihn Sook Jeong
-
Journal of Korean Academy of Nursing 2014;44(4):437-445.
DOI: https://doi.org/10.4040/jkan.2014.44.4.437
Published online: August 29, 2014
1Department of Nursing, Pusan National University Hospital, Busan, Korea.
2College of Nursing, Pusan National University, Yangsan, Korea.
- Address reprint requests to: Jeong, Ihn Sook. College of Nursing, Pusan National University, 49 BusanDaehak-ro, Mulgeum-eup, Yangsan 626-870, Korea. Tel: +82-51-510-8342, Fax: +82-51-510-8308, jeongis@pusan.ac.kr
© 2014 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- This study was done to identify pain perception (P-PER) by nurses and pain expression (P-EXP) by patients in critical care units (ICUs) and degree of agreement between nurses' P-PER and patients' P-EXP.
-
Methods
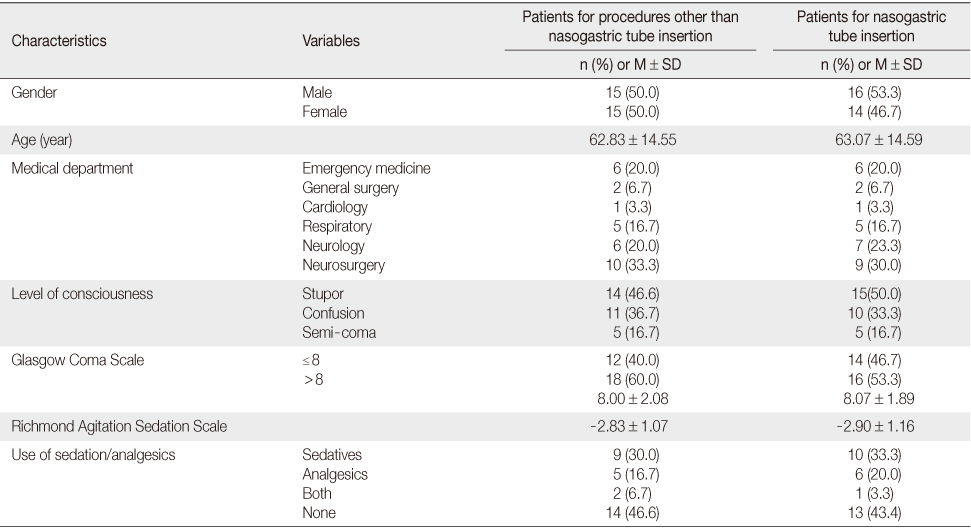
- Nurses' P-PER was measured with a self-administered questionnaire completed by 99 nurses working in ICUs during May, 2013. Patients' P-EXP was measured with the Critical Care Non-Verbal Pain Scale through observations of 31 ICU patients during nine nursing procedures (NPs) performed between May and July, 2013.
-
Results
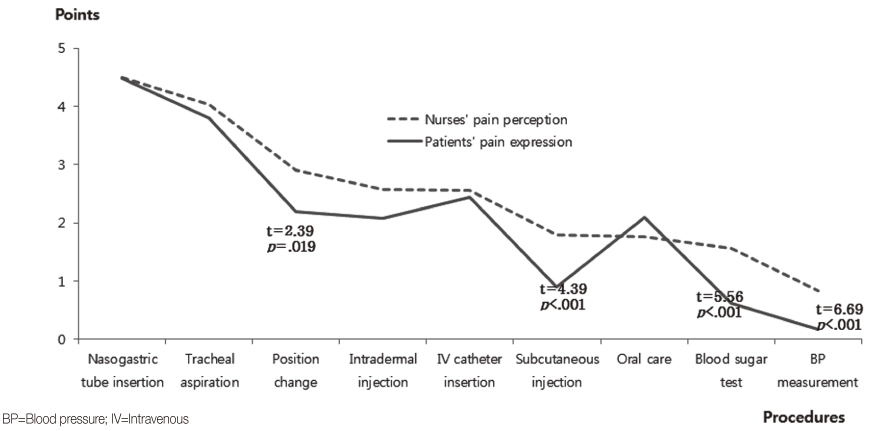
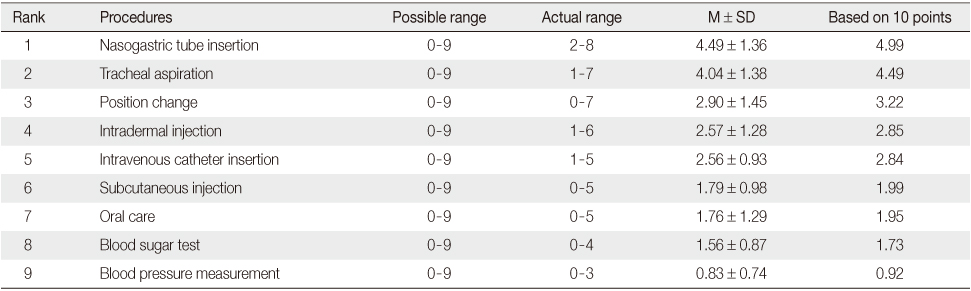
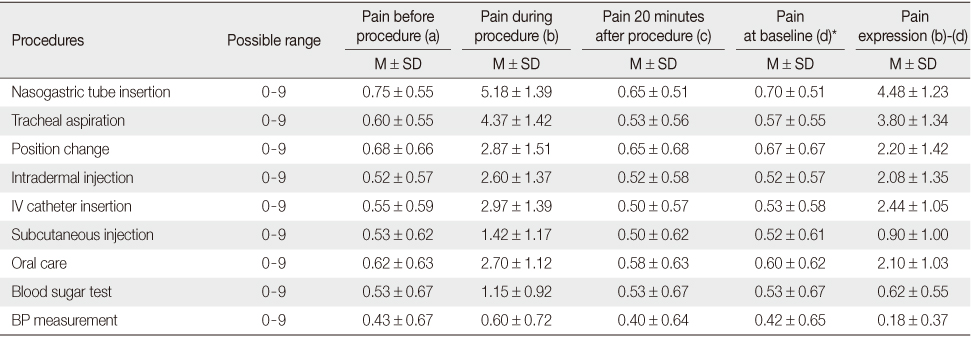
- Nurses' P-PER was from 4.49 points for nasogastric tube (NGT) insertion to 0.83 for blood pressure (BP) measurement based on a 9-point scale, Patients' P-EXP was 4.48 points for NGT to 0.18 for BP measurement based on a 10-point scale. Eight NPs except oral care showed higher scores for nurses' P-PER than for patients' P-EXP. Position change (p=.019), subcutaneous injection (p<.001), blood sugar test (p<.001), and BP measurement (p<.001) showed significant differences between nurses' P-PER and patients' P-EXP.
-
Conclusion
- Nasogastric tube (NGT) insertion was scored highest by both nurses and patients. Eight NPs except 'oral care' showed nurses' P-PER was higher or similar to patients' P-EXP, which indicates that nurses may overestimate procedural pain experienced by patients.
- 1. International Association for the Study of Pain Subcommittee on Taxonomy. Pain terms: A list with definitions and notes on usage. Recommended by the IASP subcommittee on taxonomy. Pain. 1979;6(3):249–252.PubMed
- 2. Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008;300(1):60–70. http://dx.doi.org/10.1001/jama.300.1.60ArticlePubMed
- 3. Puntillo KA, Max A, Timsit JF, Vignoud L, Chanques G, Robleda G, et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am J Respir Crit Care Med. 2014;189(1):39–47. http://dx.doi.org/10.1164/rccm.201306-1174OCArticlePubMed
- 4. Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, et al. Patients' perceptions and responses to procedural pain: Results from thunder project II. Am J Crit Care. 2001;10(4):238–251.ArticlePubMedPDF
- 5. de Jong A, Molinari N, de Lattre S, Gniadek C, Carr J, Conseil M, et al. Decreasing severe pain and serious adverse events while moving intensive care unit patients: A prospective interventional study (the NURSE-DO project). Crit Care. 2013;17(2):R74. http://dx.doi.org/10.1186/cc12683PubMedPMC
- 6. Greisen J, Juhl CB, Grøfte T, Vilstrup H, Jensen TS, Schmitz O. Acute pain induces insulin resistance in humans. Anesthesiology. 2001;95(3):578–584.ArticlePubMedPDF
- 7. Alsaadi SM, McAuley JH, Hush JM, Lo S, Lin CW, Williams CM, et al. Poor sleep quality is strongly associated with subsequent pain intensity in patients with acute low back pain. Arthritis Rheumatol. 2014;66(5):1388–1394. http://dx.doi.org/10.1002/art.38329ArticlePubMed
- 8. Courtenay M, Carey N. The impact and effectiveness of nurse-led care in the management of acute and chronic pain: A review of the literature. J Clin Nurs. 2008;17(15):2001–2013. http://dx.doi.org/10.1111/j.1365-2702.2008.02361.xArticlePubMed
- 9. Registered Nurses' Association of Ontario. Assessment and management of pain. 3rd ed. Toronto, CA: Author; 2013.
- 10. Hwang KH, Ryoo EN, Park KS. A study of the nurses' knowledge and attitude about pain management. J Korean Acad Soc Nurs Educ. 2007;13(1):41–51.
- 11. Song SS, Park CS. Pain management knowledge and attitude of internal medicine and surgery stream nurses. J Korean Acad Soc Home Care Nurs. 2010;17(1):55–62.
- 12. Bergeron DA, Leduc G, Marchand S, Bourgault P. Descriptive study of the postoperative pain assessment and documentation process in a university hospital. Pain Res Manag. 2011;16(2):81–86.PMC
- 13. Puntillo K, Neighbor M, O'Neil N, Nixon R. Accuracy of emergency nurses in assessment of patients' pain. Pain Manag Nurs. 2003;4(4):171–175.ArticlePubMed
- 14. Payen JF, Bru O, Bosson JL, Lagrasta A, Novel E, Deschaux I, et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med. 2001;29(12):2258–2263.ArticlePubMed
- 15. Gélinas C, Fillion L, Puntillo KA, Viens C, Fortier M. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care. 2006;15(4):420–427.ArticlePDF
- 16. Choi EH, Kim JH, Choi KO, Yoo JS, Kim MS, Kim PJ, et al. Development of a pain assessment tool for critically ill patients. J Korean Clin Nurs Res. 2012;18(1):136–148.
- 17. Choi EH, Kim JH, Ko MS, Kim JY, Kwon EO, Jang IS. Validation of critical care non-verbal pain scale for critically ill patients. J Korean Clin Nurs Res. 2013;19(2):245–254.
- 18. Gélinas C, Fortier M, Viens C, Fillion L, Puntillo K. Pain assessment and management in critically ill intubated patients: A retrospective study. Am J Crit Care. 2004;13(2):126–135.ArticlePubMedPDF
- 19. Rose L, Haslam L, Dale C, Knechtel L, Fraser M, Pinto R, et al. Survey of assessment and management of pain for critically ill adults. Intensive Crit Care Nurs. 2011;27(3):121–128. http://dx.doi.org/10.1016/j.iccn.2011.02.001Article
- 20. Chanques G, Jaber S, Barbotte E, Violet S, Sebbane M, Perrigault PF, et al. Impact of systematic evaluation of pain and agitation in an intensive care unit. Crit Care Med. 2006;34(6):1691–1699. http://dx.doi.org/10.1097/01.ccm.0000218416.62457.56ArticlePubMed
- 21. Chanques G, Sebbane M, Barbotte E, Viel E, Eledjam JJ, Jaber S. A prospective study of pain at rest: Incidence and characteristics of an unrecognized symptom in surgical and trauma versus medical intensive care unit patients. Anesthesiology. 2007;107(5):858–860. http://dx.doi.org/10.1097/01.anes.0000287211.98642.51ArticlePubMedPDF
- 22. Payen JF, Chanques G, Mantz J, Hercule C, Auriant I, Leguillou JL, et al. Current practices in sedation and analgesia for mechanically ventilated critically ill patients: A prospective multicenter patient-based study. Anesthesiology. 2007;106(4):687–695. http://dx.doi.org/10.1097/01.anes.0000264747.09017.daArticlePubMedPDF
- 23. Gélinas C. Management of pain in cardiac surgery ICU patients: Have we improved over time? Intensive Crit Care Nurs. 2007;23(5):298–303. http://dx.doi.org/10.1016/j.iccn.2007.03.002ArticlePubMed
- 24. Kim DH, Kim C, Sohn KT, Jeong KM, Chung Y, Choi YS, et al. Statistics: Theory and application. Paju: Freeacademy; 2003.
- 25. Siffleet J, Young J, Nikoletti S, Shaw T. Patients' self-report of procedural pain in the intensive care unit. J Clin Nurs. 2007;16(11):2142–2148. http://dx.doi.org/10.1111/j.1365-2702.2006.01840.xArticlePubMed
- 26. Resnick S, Morrison RS. Physicians' perceptions of procedural pain and discomfort. J Palliat Med. 2004;7(5):646–651.ArticlePubMed
- 27. Koeppen BM, Stanton BA. Berne & Levy physiology. 6th ed. Philadelphia, PA: Mosby; 2009.
- 28. Korea Institute for Healthcare Accreditation. KOIHA evaluation criteria for healthcare accreditation: Tertiary general hospital (Ver 2.0). Seoul: Ministry of Health & Welfare, Korea Institute for Healthcare Accreditation; 2014.
- 29. Li KK, Harris K, Hadi S, Chow E. What should be the optimal cut points for mild, moderate, and severe pain? J Palliat Med. 2007;10(6):1338–1346. http://dx.doi.org/10.1089/jpm.2007.0087ArticlePubMed
- 30. World Health Organization. Pain relief ladder for cancer pain relief [Internet]. Geneva, World Health Organization. 2012;cited 2014 July 28. Available from: http://www.who.int/cancer/palliative/painladder/en/
REFERENCES
Figure & Data
REFERENCES
Citations

- Understanding oral care in the intensive care unit: A qualitative study of nurse experiences and practices with mechanically ventilated patients
Li SuWen, Huang YuYang, Bu Wei
Nursing in Critical Care.2025;[Epub] CrossRef - A Systematic Review on Pain Assessment Tools for Intensive Care Unit Patients
Eun-Jeong Kim, Jiwon Hong, Jiyeon Kang, Na geong Kim, NaRi Kim, Su-Youn Maeng, Hye-Ryeon Park, Min Kyung Ban, Gun Young Yang, Kyung Suk Lee, Eun Hye Jang
Journal of Korean Critical Care Nursing.2020; 13(1): 44. CrossRef - Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU
John W. Devlin, Yoanna Skrobik, Céline Gélinas, Dale M. Needham, Arjen J. C. Slooter, Pratik P. Pandharipande, Paula L. Watson, Gerald L. Weinhouse, Mark E. Nunnally, Bram Rochwerg, Michele C. Balas, Mark van den Boogaard, Karen J. Bosma, Nathaniel E. Bru
Critical Care Medicine.2018; 46(9): e825. CrossRef
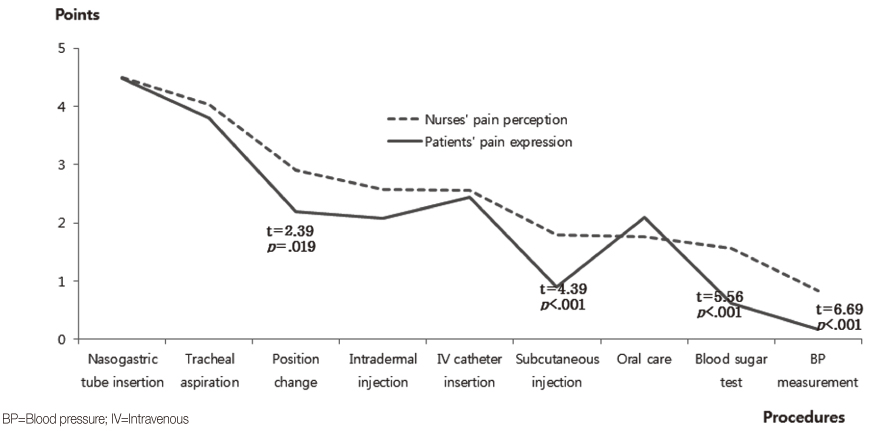
Figure 1
General Characteristics of Study Participants: Patients
Pain Perception of Intensive Care Units' Nurses for Nursing Procedures (N=99)
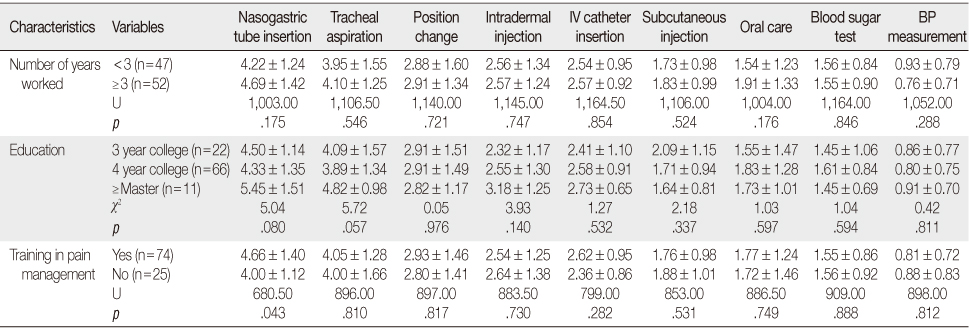
Pain Perception of Intensive Care Units' Nurses by General Characteristics (N=99)
IV=Intravenous; BP=Blood pressure.
Pain Expression of Intensive Care Unit Patients for Nursing Procedures (N=30)
*Pain at baseline (d) is the mean of pain before procedure and pain 20 min after procedure; IV=Intravenous; BP=Blood pressure.
IV=Intravenous; BP=Blood pressure.
*Pain at baseline (d) is the mean of pain before procedure and pain 20 min after procedure; IV=Intravenous; BP=Blood pressure.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

