Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(2); 2024 > Article
- Research Paper Psychometric Properties of the Fall Risk Perception Questionnaire-Short Version for Inpatients in Acute Care Hospitals
- Jeeeun Choi, Sujin Lee, Eunjin Park, Sangha Ku, Sunhwa Kim, Wonhye Yu, Eunmi Jeong, Sukhee Park, Yusun Park, Hye Young Kim, Sung Reul Kim
-
Journal of Korean Academy of Nursing 2024;54(2):151-161.
DOI: https://doi.org/10.4040/jkan.23127
Published online: May 31, 2024
2College of Nursing, Korea University, Seoul, Korea
3College of Nursing, Research Institute of Nursing Science, Jeonbuk National University, Jeonju, Korea
4College of Nursing, Korea University Nursing Research Institute, Korea University, Seoul, Korea
-
Corresponding author:
Sung Reul Kim,
Email: srkim74@korea.ac.kr
- 3,346 Views
- 137 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
Patients’ perception of fall risk is a promising new indicator for fall prevention. Therefore, a fall risk perception questionnaire that can be used rapidly and repeatedly in acute care settings is required. This study aimed to develop a short version of the fall risk perception questionnaire (Short-FRPQ) for inpatients.
Methods
For the psychometric measurements, 246 inpatients were recruited from an acute care hospital. The construct (using confirmatory factor analysis and discriminant validity of each item), convergent, and known-group validities were tested to determine the validity of the Short-FRPQ. McDonald’s omega coefficient was used to examine the internal consistency of reliability.
Results
In the confirmatory factor analysis, the fit indices of the Short-FRPQ, comprising 14 items and three factors, appeared to be satisfactory. The Short-FRPQ had a significantly positive correlation with the original scale, the Korean Falls Efficacy Scale-International, and the Morse Fall Scale. The risk of falls group, assessed using the Morse Fall Scale, had a higher score on the Short-FRPQ. McDonald’s omega coefficient was .90.
Conclusion
The Short-FRPQ presents good reliability and validity. As patient participation is essential in fall interventions, evaluating the fall risk perception of inpatients quickly and repeatedly using scales of acceptable validity and reliability is necessary.
Published online May 07, 2024.
https://doi.org/10.4040/jkan.23127
Psychometric Properties of the Fall Risk Perception Questionnaire-Short Version for Inpatients in Acute Care Hospitals
Abstract
Purpose
Patients’ perception of fall risk is a promising new indicator for fall prevention. Therefore, a fall risk perception questionnaire that can be used rapidly and repeatedly in acute care settings is required. This study aimed to develop a short version of the fall risk perception questionnaire (Short-FRPQ) for inpatients.
Methods
For the psychometric measurements, 246 inpatients were recruited from an acute care hospital. The construct (using confirmatory factor analysis and discriminant validity of each item), convergent, and known-group validities were tested to determine the validity of the Short-FRPQ. McDonald’s omega coefficient was used to examine the internal consistency of reliability.
Results
In the confirmatory factor analysis, the fit indices of the Short-FRPQ, comprising 14 items and three factors, appeared to be satisfactory. The Short-FRPQ had a significantly positive correlation with the original scale, the Korean Falls Efficacy Scale-International, and the Morse Fall Scale. The risk of falls group, assessed using the Morse Fall Scale, had a higher score on the Short-FRPQ. McDonald’s omega coefficient was .90.
Conclusion
The Short-FRPQ presents good reliability and validity. As patient participation is essential in fall interventions, evaluating the fall risk perception of inpatients quickly and repeatedly using scales of acceptable validity and reliability is necessary.
INTRODUCTION
Falls are a high-priority safety problem in hospitals because of the resulting poor health outcomes and costs [1]. Unlike community-dwelling subjects, inpatients in acute care hospitals are likely to be at a high risk of falls because their disease status changes continuously and rapidly, and various medications and treatment modalities can cause falls [2, 3]. Therefore, falls in acute care hospitals are a major challenge for healthcare providers who prioritize patient safety and require considerable care and attention from healthcare providers [3, 4].
To prevent falls in hospitals, clinicians and researchers are continuing their efforts to identify factors related to falls while managing the known risk factors. Based on systematic reviews and current observational studies, recent clinical practice guidelines have reported that fall history (within the last 6 months), old age (> 70 years), gender (man), disease-related changes such as movement restriction and an increase in gait problems, dementia- and cancer-specific factors, medications such as anticonvulsants, antipsychotics, and sedatives, and external risk factors are significant risk factors for falls [5]. In a previous study comparing 447 fallers and 3,667 non-fallers admitted to an acute care hospital in South Korea, gender (man), low body mass index, defecation problems, gait problems, vision and hearing disturbances, and medications were reported as influencing factors for falls [6]. A systematic review of the risk factors associated with falls in non-ambulatory adults reported that the use of wheelchairs, changes in wheelchair setup and selection, performance of transfers, and impaired seated balance are risk factors for falls [7]. As described above, falls occurring in hospitals are characterized by the contribution of an individual patient’s underlying disease, factors related to changes in the current disease, and risk factors related to the hospital environment.
Recently, patients’ fall risk perception has become a promising new indicator for preventing falls [8]. Fall prevention and clinical management guidelines recommend incorporating patient perspectives as stakeholders in fall prevention and management [9]. Assessing patients’ perceptions of their fall risk can help healthcare professionals provide fall interventions and understand their fall-related behaviors [10]. Thus, fall prevention and management interventions need to be consistently performed, focusing on helping patients actively participate in fall interventions as they adjust to their condition [8]. Falls are accidents that can mostly be prevented, and managing falls with only the effort and attention of healthcare professionals has its limitations [9]. Therefore, patient participation is emphasized because patients are the subjects of fall prevention interventions aimed at decreasing falls in medical institutions [11, 12, 13].
From this perspective, scales for assessing patients’ fall risk perception, such as the falls risk perception questionnaire [14] and the fall risk self-assessment [15], are being developed and implemented. However, the falls risk perception questionnaire was developed for older community-dwelling adults with type 2 diabetes [14], and the fall risk self-assessment was developed for community-dwelling seniors [15]. Therefore, they do not reflect the characteristics of inpatients in acute care hospitals or their environmental characteristics.
Accordingly, we developed a fall risk perception questionnaire (FRPQ) comprising 27 questions regarding patients’ fall risk perceptions in acute care hospitals [16]. However, this questionnaire has limitations in terms of quickly identifying patient perceptions of fall risk in clinical practice. The questionnaire took approximately 7~10 minutes to complete, and only exploratory factor analysis was performed when developing the scale. In an acute care hospital, various treatments are rapidly provided, and the patient’s condition is unpredictable; therefore, the patient’s fall risk can easily change. Therefore, evaluating fall risk repeatedly and rapidly, as assessed by healthcare professionals and perceived by patients, is necessary in acute care hospitals. This study aimed to develop a short version of the fall risk perception questionnaire (Short-FRPQ) to quickly evaluate fall risk perception in patients hospitalized for acute treatments that are easy to repeat.
METHODS
1. Study design
This was a methodological study to develop the Short-FRPQ using a cross-sectional design.
2. Study subject
The participants were inpatients in a tertiary acute care setting in Seoul, South Korea. This hospital is large, with approximately 2,700 beds where many patients with acute diseases are hospitalized and treated. The inclusion criteria were as follows: (1) age > 18 years, (2) no diagnosis of cognitive impairment, and (3) no history of falls during hospital stay. Falls were related to the hospitalization period; therefore, patients whose hospitalization period was less than two days were excluded.
To identify construct validity using confirmatory factor analysis (CFA), the number of study samples had to exceed 200 [17]. Considering the dropout rate, the required sample size was estimated to be 250. A total of 250 structured questionnaires were distributed, and four were excluded because of a large amount of missing data (response rate: 98.4%). A total of 246 questionnaires were analyzed.
3. Measurements
The scales used in this study were used after approval from the scale developers.
1) Fall risk perception questionnaire
The FRPQ was developed by Choi et al. [16] to measure fall risk perception among inpatients in an acute hospital. This scale comprises 27 items across three subdomains. Subdomain I included eight items and risk attributes related to individual mobility, such as general weakness and leg strength. Subdomain II included six items and risk attributes related to individual chronic conditions, such as vision and hearing difficulties. Finally, Subdomain III included 13 items and risk attributes related to the environment, such as disorganized surroundings and poor lighting in the room. Each item was rated on a 4-point Likert scale (0 = absolutely not true, 1 = not true, 2 = true, and 3 = absolutely true), with a total score ranging from 0 to 81. Higher scores indicated a higher fall risk perception. Cronbach’s α was .95 in the original study [16] and .94 in this study.
2) Short version of the fall risk perception questionnaire
For the Short-FRPQ development, item generation was first performed through two content validity rounds based on the original scale (FRPQ). Through content validity rounding, attempts were made to group similar items or delete redundant items. Eight experts (two professors, two head nurses, two nurses with more than five years of clinical experience, one clinical nurse specialist, and one nursing team leader) participated in the content validity rounds. The experts had experience using or participating in the development of the original scale. In the first round, the item-level content validity index (I-CVI) coefficients were .50~1.00. Ten items of the FRPQ with I-CVI coefficients of less than .78 were deleted. The second round consisted of 17 items. After the 2nd CVI, the preliminary questions were presented with fourteen items, excluding three items with less than .78, I-CVI = .63~1.00, and scale-level content validity index (S-CVI) = .94. A pilot test was conducted with 20 inpatients for the preliminary questions of the Short-FRPQ to determine whether items that were not understood or words with difficult vocabulary had been included. None of the items, including sentences or phrases, were difficult to understand. Therefore, we confirmed the preliminary questions consisting of 14 items as the final questionnaire (Appendix 1, 2).
3) Korean Falls Efficacy Scale-International
The Korean version of the falls Efficacy Scale-International (KFES-I) was used to assess fall efficacy [18, 19]. The KFES-I includes 16 items, each rated on a 4-point Likert scale. A higher KFES-I score indicates greater concern about falls. Cronbach’s alpha for this scale was .96 in the original study [18] and .95 in the current study.
4) Morse Fall Scale
The Morse Fall Scale (MFS) was used to determine the risk of falling [20]. The MFS is commonly used to measure fall risk among inpatients in acute care hospitals [21, 22]. This scale comprises six items: history of falling, secondary diagnosis, ambulatory aid, IV/heparin lock, gait/transfer, and mental status. The total scores ranged from 0 to 125, and the optimal cut-off value of the MFS for predicting falls was 45 in acute care [23]. In a systematic review and meta-analysis, the pooled sensitivity and specificity of MFS were .73 (95% confidence interval [CI], .68~.78) and .75 (95% CI, .74~.76) [24].
4. Data collection
Data were collected from February 14 to August 4, 2022. Data were collected from six registered nurses in six wards. To ensure consistent data collection, the researcher held training sessions for the nurses. Participants completed the FRPQ, Short-FRPQ, and KFES-I using a questionnaire. The nurses then completed and scored the MFS. Each participant took approximately 15~30 minutes to complete the questionnaires. The patients’ demographic, clinical, and fall-related characteristics were also examined. Gender, and education level, and clinical were investigated. Fall-related characteristics, including fall occurrence, history of falls, sleep disturbance, urinary disturbance, and mobility problems, were examined. Comorbidities were assessed by allowing multiple responses.
5. Data analysis
The data were analyzed using SPSS 27.0 (IBM Co.) and AMOS 23.0 (IBM Co.). Demographic, clinical, and fall-related characteristics were analyzed using descriptive statistics. Construct, convergent, and known-group validities were evaluated to determine the validity of the Short-FRPQ. Construct validity was determined using CFA and the discriminant validity of each item. The normed χ2 (χ2/degrees of freedom, p), comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR) were used in the CFA to test the model. To test the goodness of fit, normed χ2 values ≤ 3.0 indicated acceptable fit, and CFI and TLI values ≥ .90 indicated good fit [25]. SRMR and RMSEA values between .05 and .08 indicated an acceptable fit [26]. A CFA model was then used to confirm the convergent and discriminant validity of the items. Standardized regression weights, average variance extracted (AVE), and composite reliability (CR) were used to establish the convergent validity of each item. The reference values were AVE of ≥ .50, CR of ≥ .70, and standardized regression weights of ≥ .50. To test the discriminant validity of each item, the AVE values were compared with the square values of the correlation coefficients for each subdomain of the Short-FRPQ [26]. The convergent validity of the Short-FRPQ was tested using Pearson’s correlation coefficients for associations among the FRPQ (I, II, III, and total), KFES-I, MFS, and Short-FRPQ subscales. Known-group validity was examined to test the differences in the Short-FRPQ scores between groups at risk and those not at risk of falling using the MFS. McDonald’s omega coefficient was used to examine internal consistency. Statistical significance was set at p = .050.
6. Ethical considerations
This study was approved by the Asan Medical Center’s Institutional Review Board (IRB No. 2022-0069). Written informed consent was obtained from all participants after explaining the aims and processes of the study. The participants were informed that they could stop participating at any time.
RESULTS
1. Participants’ demographic, clinical, and fall-related characteristics
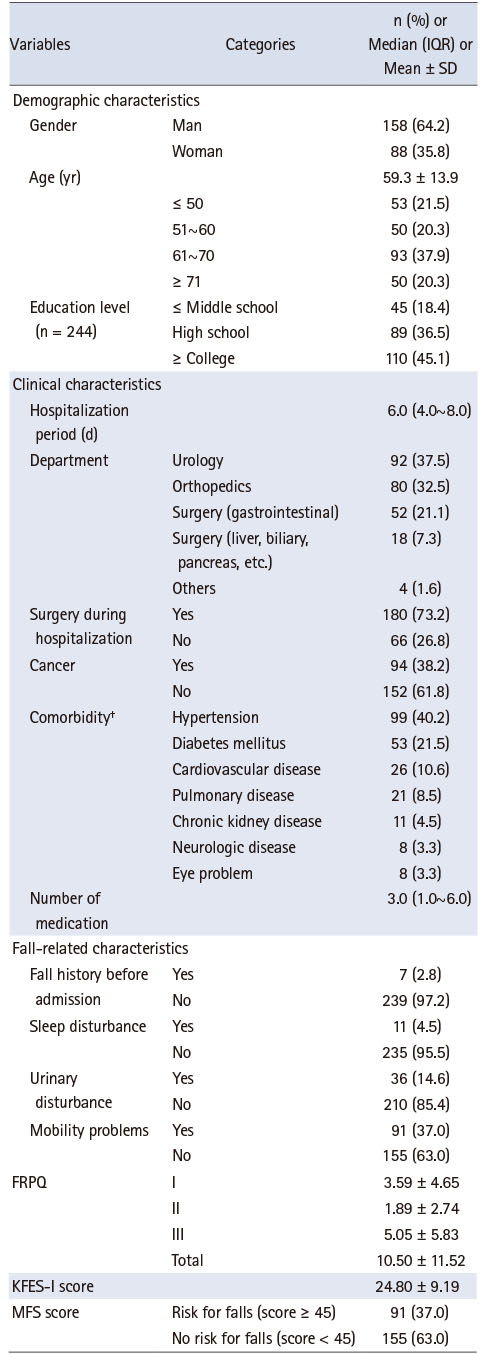
Demographic, clinical, and fall-related characteristics of the participants are presented in Table 1. The mean age was 59.3 ± 13.9, and 158 participants (64.2%) were men. The median hospitalized period was 6.0 days (interquartile range, 4.0~8.0), and hypertension (40.2%) was the most common comorbidity. Two falls occurred among the participants during the study period. When classified based on the MFS, 37.0% were classified into the fall-risk group (Table 1).
Table 1
Participants’ Demographic, Clinical, and Fall-Related Characteristics (N = 246)
2. Validity of the Short-FRPQ
1) Construct validity
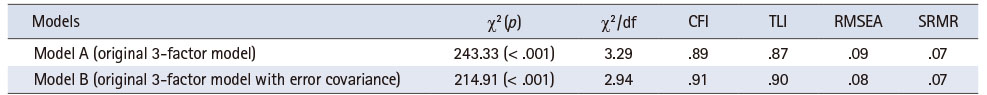
The data were fitted to a CFA measurement model. Unsatisfactory model fit indices (χ2/df = 3.29, CFI = .89, TLI = .87, RMSEA = .09, and SRMR = .07) were observed in the initial 3-factor model. After allowing for error covariance between items 12 and 13, which had the highest modification indices (MI) score of 25.17, the fit indices presented generally acceptable model fit indices (χ2/df = 2.94, CFI = .91, TLI = .90, RMSEA = .08, and SRMR = .07) (Table 2). The Short-FRPQ subscales had moderately strong intercorrelations, ranging from .51 to .70. The 14 items in the three subdomains had standardized regression weights that varied from .62 to .78. The AVE varied from .67 to .74. The CRs of the subdomains varied from .86 to .95. Consequently, the convergent validity of each item was verified. The discriminant validity of each item confirmed that the AVE values were higher than the squares of the correlation coefficients for each subdomain.
Table 2
Model Fit Test Results for the Short-FRPQ
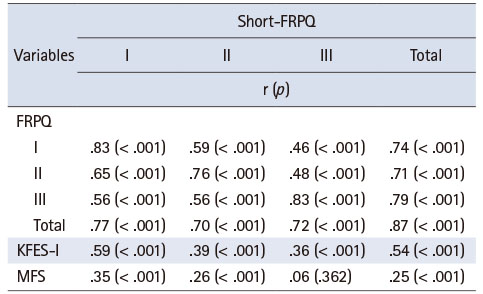
2) Convergent validity
The Short-FRPQ was significantly and positively correlated with the FRPQ, KFES-I, and MFS (Table 3). The total Short-FRPQ score was correlated with the total, I, II, and III scores of the FRPQ (r = .87, p < .001; r = .74, p < .001; r = .71, p < .001; and r = .79, p < .001, respectively), the KFES-I (r = .54, p < .001), and the MFS (r = .25, p < .001), thereby establishing convergent validity. By subdomain of the Short-FRPQ, the Short-FRPQ I was correlated with the total, I, II, and III of the FRPQ, KFES-I, and MFS, and the Short-FRPQ II was correlated with the total, I, II, and III of the FRPQ, KFES-I, and MFS. Additionally, the Short-FRPQ III score correlated with the total, I, II, and III scores of the FRPQ and KFES-I.
Table 3
Correlation of Short-FRPQ with the FRPQ, KFES-I, and MFS (N = 246)
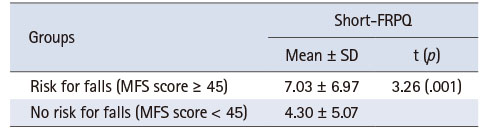
3) Known-group validity
The total MFS scores were divided into two groups based on a previous study stating that the optimal cutoff value of the MFS for predicting falls was 45 in acute care hospitals [23]. The fall risk group had a significantly higher perceived fall risk according to the Short-FRPQ than the non-fall risk group (t = 3.26, p = .001). Therefore, the known-group validity of the Short-FRPQ was confirmed (Table 4).
Table 4
Known-Group Comparison of the Short-FRPQ Scores between the MFS Risk for Falls Group and the No-Risk for Falls Group (N = 246)
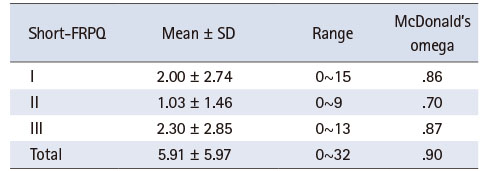
3. Reliability and descriptive statistics of the Short-FRPQ
McDonald’s omega coefficients for Short-FRPQ was .90 and ranged from .70 to .87 for the three subdomains (Table 5). The Short-FRPQ scores were 5.91 ± 5.97; 2.00 ± 2.74 for I of the Short-FRPQ, 1.03 ± 1.46 for II of the Short-FRPQ, and 2.30 ± 2.85 for III of the Short-FRPQ.
Table 5
Descriptive Statistics and Reliability of the Short-FRPQ
DISCUSSION
Falls are considered preventable safety problems, and the first step in their management is to assess the patient’s fall risk. Therefore, an individualized, continuous, and repeatable strategy is required to assess fall risk under changing conditions [27]. In previous studies, nurses’ fall risk assessment was primarily included as a first step in fall prevention [28, 29]. Recently, studies on patient perceptions of fall risk have increased, and it is recommended that such recognition be performed together with nurses’ fall risk assessments [9, 10, 30]. Furthermore, the patient’s condition may change rapidly depending on the treatment administered after admission to an acute care setting, and patients should adapt to the hospital environment. Therefore, we aimed to develop a scale to evaluate patient perceptions of fall risk rapidly and repetitively in acute care hospitals.
In this study, the reliability-measured internal consistency was calculated using McDonald’s omega coefficient. McDonald’s omega coefficients can be used for both unidimensional and multidimensional scales, whereas Cronbach’s alpha has been reported to be suitable for unidimensional scales [31, 32, 33]. As the difference between McDonald’s omega coefficients and Cronbach’s alpha has been reported [32], studies reporting reliability using McDonald’s omega coefficients have increased [34, 35]. Additionally, McDonald’s omega coefficients can help with brief form construction by removing items from a longer scale [31]. Therefore, we decided it would be more appropriate to use McDonald’s omega coefficients for internal consistency in this study.
In this study, McDonald’s omega coefficients of the Short-FRPQ were .90, .86, .70, and .87 for the total, I, II, and III, respectively. Although the interpretation criteria of McDonald’s omega vary depending on the study, the values were mentioned as excellent (.93~.94), strong (.91~.93), and reliable (.84~.90), and a value of .70 or greater is considered acceptable [31]. In this study, McDonald’s omega values for the Short-FRPQ were greater than .70, indicating good reliability. In future research on the development of scales with multidimensional properties, it would be desirable to calculate the internal consistency using McDonald’s omega coefficients.
This study confirmed the construct, convergent, and known-group validity of the Short-FRPQ. In this study, the construct validity of the two models—the original three-factor model and the three-factor model with error correlation—was tested by calculating the goodness-of-fit indices of the measurement models using CFA. The three-factor model with error correlation demonstrated reasonable goodness-of-fit and was selected as the final model for this investigation. The MI offered by AMOS suggested that when fitting the models, one should permit error covariance between the two environmental-related items, “I am at risk of falling because the lighting in the patient room is too low (item 12)” and “I am at risk of falling because the hospital environment is unfamiliar (item 13)”. Justifying the error correlation between pairs of items is acceptable because it frequently denotes perceived repetition in item content or nonrandom errors because of technique impacts [26, 36]. The inclusion of an error correlation between the two items was justified because they reflected the similarities evoked by the hospital’s physical environment in the fall risk set. Therefore, further investigation should be conducted to assess the environmental subdomain, which revealed an error correlation between items 12 and 13.
For convergent validity, we analyzed the correlations among the Short-FRPQ, FRPQ, KFES-I, and MFS. The Short-FRPQ displayed a strong correlation with the FRPQ, and the scale was significantly correlated with the KFES-I and MFS scores. These findings are consistent with the fact that the FRPQ scores correlated with the KFES-I and MFS scores in the original scale development study [16]. Furthermore, the Short-FRPQ I, Short-FRPQ II, and Short-FRPQ III had the highest correlations with FRPQ I, FRPQ II, and FRPQ III, respectively. Therefore, we confirmed the convergent validity of the Short-FRPQ.
For known-group validity using the MFS, a statistically significant difference was observed in the Short-FRPQ scores between the fall and non-fall risk groups. This finding is consistent with the statistically significant difference in FRPQ scores between the fall and non-fall-risk groups in the original scale development study [16]. Therefore, we confirmed the known-group validity of the Short-FRPQ.
The limitations of this study are as follows: First, the original study mainly included patients in the gastroenterology ward. Therefore, we attempted to include participants with a variety of diseases in this study, including orthopedic diseases, in which falls frequently occur [37]. Data were collected from six wards of an acute care hospital. Two-thirds of the participants underwent surgery, and the number of patients receiving medical treatment was relatively small. A previous study reported that a surgical specialty decreases the risk of falls [2]. Therefore, fewer individuals at a high risk of falling may have been included in the study. Further studies that include participants with various diseases and studies that equally include those who received surgical and medical treatment are needed for more well-rounded research. Second, the scale did not derive criterion validity based on fall occurrence because of the low number of falls.
When providing interventions for fall management and prevention, understanding patients’ perceptions and views of falls is important. In addition to the fall risk assessment by healthcare professionals using a scale with established validity, the assessment of a patient’s fall risk perception should be conducted systematically.
CONCLUSION
In conclusion, the Short-FRPQ presented good reliability and validity. Patient perceptions of fall risk should be assessed using a fall risk recognition scale that can be used rapidly and repeatedly in acute care hospitals. As the risk of falls in patients admitted to an acute care hospital is constantly changing because of rapid changes in their disease, medications, and treatment procedures, healthcare professionals should pay close attention to fall prevention in inpatients. The perception of fall risk is a promising new indicator for preventing falls, and the patients’ perceived fall risk should be considered along with the assessment of fall risk factors. As using a scale for the quick assessment of fall risk perception can potentially help prevent falls in hospital settings, it should be included in fall prevention interventions across all hospital setups. This proactive approach can significantly contribute to enhancing patient care and preventing falls.
CONFLICTS OF INTEREST:Kim, Sung Reul and Kim, Hye Young have been the Editorial Board Members of JKAN between 2020 and 2023 but have no role in the review process. Except for that, no potential conflict of interest relevant to this article was reported.
FUNDING:This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Science and ICT) [NRF-2021R1F1A1048955]. The funding source was not involved in the study design, data collection, analysis, interpretation of results, preparation of the manuscript, or decision to publish.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Choi J & Lee S & Park E & Ku S & Kim SW & Yu W & Jeong E & Park S & Park Y & Kim H & Kim SR.
Data curation or/and Analysis: Choi J & Lee S & Park E & Ku S & Kim SW & Yu W & Jeong E & Park Y & Kim H & Kim SR.
Funding acquisition: Kim SR.
Investigation: Choi J & Lee S & Park E & Ku S & Kim SW & Yu W & Jeong E & Park S.
Project administration or/and Supervision: Choi J & Park S & Kim SR.
Resources or/and Software: Choi J & Park Y & Kim H & Kim SR.
Validation: Choi J & Lee S & Park E & Ku S & Kim SW & Yu W & Jeong E & Park S & Park Y & Kim H & Kim SR.
Visualization: Choi J & Park Y & Kim H & Kim SR.
Writing original draft or/and Review & Editing: Choi J & Lee S & Park E & Ku S & Kim SW & Yu W & Jeong E & Park S & Park Y & Kim H & Kim SR.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
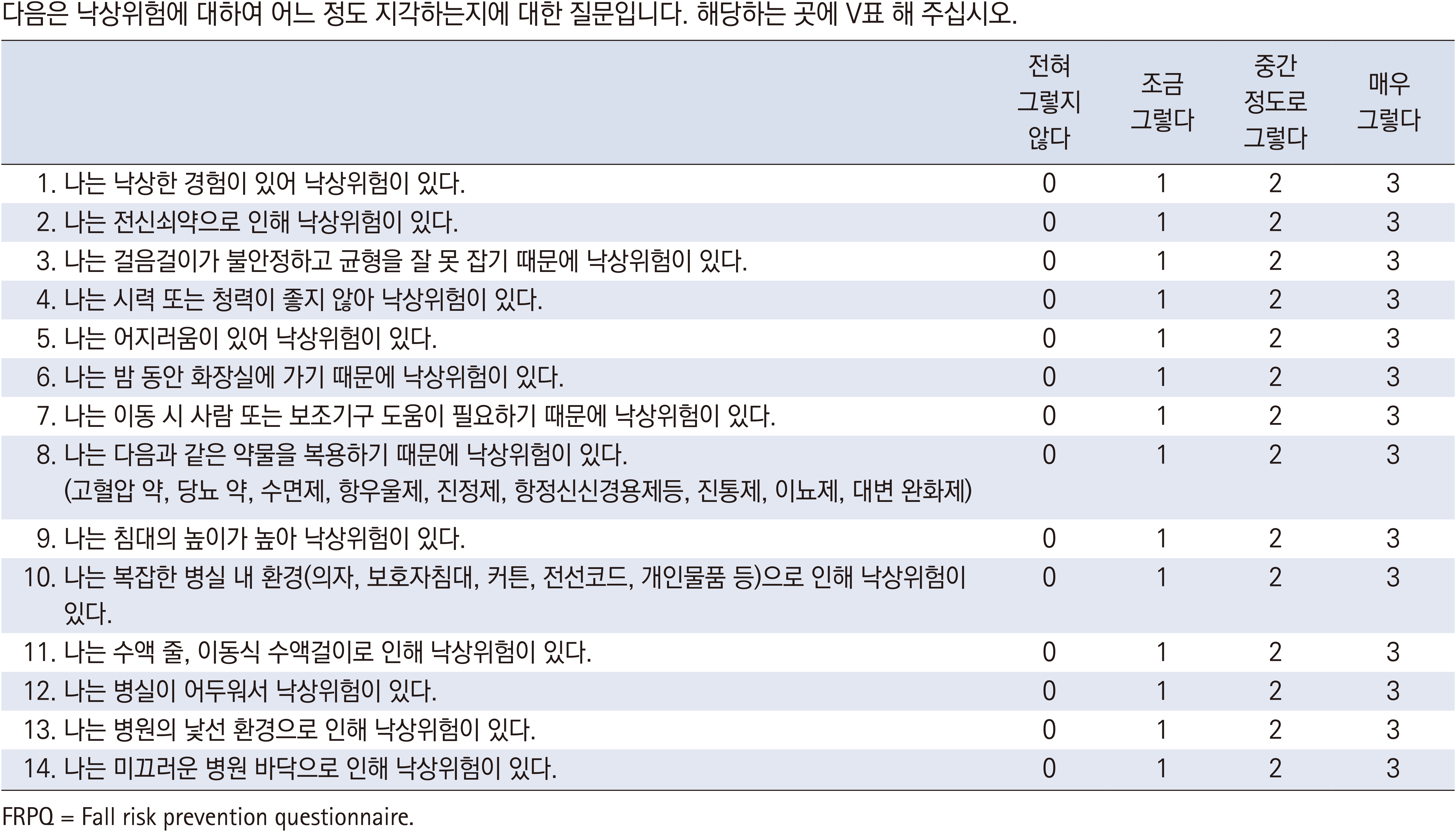
Appendix 1
The Final Version of the Korean Short-FRPQ
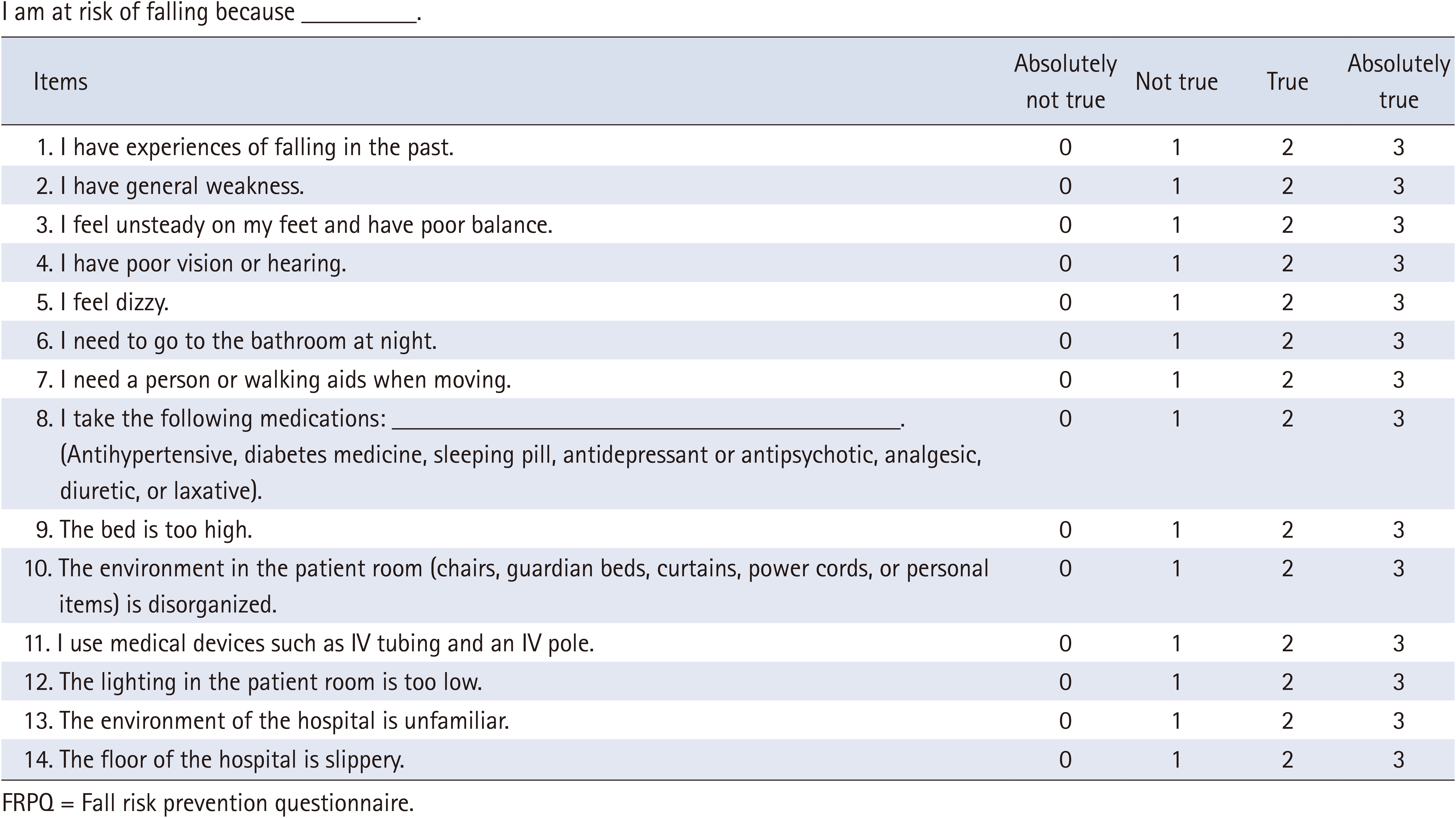
Appendix 2
The Final Version of the Short-FRPQ
References
-
Heikkilä A, Lehtonen L, Junttila K. Fall rates by specialties and risk factors for falls in acute hospital: A retrospective study. Journal of Clinical Nursing 2023;32(15-16):4868–4877. [doi: 10.1111/jocn.16594]
-
-
Reuben DB, Gazarian P, Alexander N, Araujo K, Baker D, Bean JF, et al. The strategies to reduce injuries and develop confidence in elders intervention: Falls risk factor assessment and management, patient engagement, and nurse co-management. Journal of the American Geriatrics Society 2017;65(12):2733–2739. [doi: 10.1111/jgs.15121]
-
-
Tzeng HM, Yin CY. Patient engagement in hospital fall prevention. Nursing Economics 2015;33(6):326–334.
-
-
Gravesande J, Richardson J, Griffith L, Scott F. Test-retest reliability, internal consistency, construct validity and factor structure of a falls risk perception questionnaire in older adults with type 2 diabetes mellitus: A prospective cohort study. Archives of Physiotherapy 2019;9:14 [doi: 10.1186/s40945-019-0065-4]
-
-
Kyriazos TA. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018;9(8):2207–2230. [doi: 10.4236/psych.2018.98126]
-
-
Park GB, Cho BL, Kwon IS, Park BJ, Kim T, Cho KY, et al. Reliability and validity of Korean version of Falls Efficacy Scale-International (KFES-I). Journal of the Korean Academy of Rehabilitation Medicine 2010;34(5):554–559.
-
-
Morse JM, Morse RM, Tylko SJ. Development of a scale to identify the fall-prone patient. Canadian Journal on Aging 1989;8(4):366–377. [doi: 10.1017/S0714980800008576]
-
-
Bagui S, Long T, Bagui S. Selecting the optimal Morse Falls Scale cut-off point for patient fall risk. Health 2019;11(7):924–931. [doi: 10.4236/health.2019.117074]
-
-
Park SH, Kim EK. Systematic review and meta-analysis for usefulness of fall risk assessment tools in adult inpatients. Korean Journal of Health Promotion 2016;16(3):180–191. [doi: 10.15384/kjhp.2016.16.3.180]
-
-
Hair JF Jr, Black WC, Babin BJ, Anderson RE. In: Multivariate data analysis. 7th ed. Pearson; 2010. pp. 1-816.
-
-
Kim GS. In: Analysis structural equation modeling. Hannarae Publishing Co; 2010. pp. 1-663.
-
-
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J, et al. Evaluation of clinical practice guidelines on fall prevention and management for older adults: A systematic review. JAMA Network Open 2021;4(12):e2138911 [doi: 10.1001/jamanetworkopen.2021.38911]
-
-
Hayes AF, Coutts JJ. Use Omega rather than Cronbach’s alpha for estimating reliability. But…. Communication Methods and Measures 2020;14(1):1–24. [doi: 10.1080/19312458.2020.1718629]
-
-
McDonald RP. In: Test theory: A unified treatment. Psychology Press; 1999. pp. 1-498.
-
-
Byrne BM, Baron P, Campbell TL. Measuring adolescent depression: Factorial validity and invariance of the Beck Depression Inventory across gender. Journal of Research on Adolescence 1993;3(2):127–143.
-
-
Kobayashi K, Ando K, Inagaki Y, Suzuki Y, Nagao Y, Ishiguro N, et al. Characteristics of falls in orthopedic patients during hospitalization. Nagoya Journal of Medical Science 2018;80(3):341–349. [doi: 10.18999/nagjms.80.3.341]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

