Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(2); 2024 > Article
- Research Paper Influence of Illness Uncertainty on Health Behavior in Individuals with Coronary Artery Disease: A Path Analysis
- Hyesun Jeong, Yesul Lee, Jin Sup Park, Yoonju Lee
-
Journal of Korean Academy of Nursing 2024;54(2):162-177.
DOI: https://doi.org/10.4040/jkan.23136
Published online: May 31, 2024
2Department of Cardiology, Medical Research Institute, Pusan National University Hospital, Busan, Korea
3College of Nursing, Research Institute of Nursing Science, Pusan National University, Yangsan, Korea
-
Corresponding author:
Yoonju Lee,
Email: lyj@pusan.ac.kr
Abstract
Purpose
This study aimed to investigate the influence of uncertainty-related factors on the health behavior of individuals with coronary artery disease (CAD) based on Mishel’s uncertainty in illness theory (UIT).
Methods
We conducted a cross-sectional study and path analysis to investigate uncertainty and factors related to health behavior. The study participants were 228 CAD patients who visited the outpatient cardiology department between September 2020 and June 2021. We used SPSS 25.0 and AMOS 25.0 software to analyze the data.
Results
The final model demonstrated a good fit with the data. Eleven of the twelve paths were significant. Uncertainty positively affected danger and negatively affected self-efficacy and opportunity. Danger had a positive effect on perceived risk. Opportunity positively affected social support, self-efficacy, perceived benefit and intention, whereas it negatively affected perceived risk. Social support, self-efficacy, perceived benefit and intention had a positive effect on health behavior. We found that perceived benefit and intention had the most significant direct effects, whereas self-efficacy indirectly affected the relationship between uncertainty and health behavior.
Conclusion
The path model is suitable for predicting the health behavior of CAD patients who experience uncertainty. When patients experience uncertainty, interventions to increase their self-efficacy are required first. Additionally, we need to develop programs that quickly shift to appraisal uncertainty as an opportunity, increase perceived benefits of health behavior, and improve intentions.
Published online May 24, 2024.
https://doi.org/10.4040/jkan.23136
Influence of Illness Uncertainty on Health Behavior in Individuals with Coronary Artery Disease: A Path Analysis
Abstract
Purpose
This study aimed to investigate the influence of uncertainty-related factors on the health behavior of individuals with coronary artery disease (CAD) based on Mishel’s uncertainty in illness theory (UIT).
Methods
We conducted a cross-sectional study and path analysis to investigate uncertainty and factors related to health behavior. The study participants were 228 CAD patients who visited the outpatient cardiology department between September 2020 and June 2021. We used SPSS 25.0 and AMOS 25.0 software to analyze the data.
Results
The final model demonstrated a good fit with the data. Eleven of the twelve paths were significant. Uncertainty positively affected danger and negatively affected self-efficacy and opportunity. Danger had a positive effect on perceived risk. Opportunity positively affected social support, self-efficacy, perceived benefit and intention, whereas it negatively affected perceived risk. Social support, self-efficacy, perceived benefit and intention had a positive effect on health behavior. We found that perceived benefit and intention had the most significant direct effects, whereas self-efficacy indirectly affected the relationship between uncertainty and health behavior.
Conclusion
The path model is suitable for predicting the health behavior of CAD patients who experience uncertainty. When patients experience uncertainty, interventions to increase their self-efficacy are required first. Additionally, we need to develop programs that quickly shift to appraisal uncertainty as an opportunity, increase perceived benefits of health behavior, and improve intentions.
INTRODUCTION
1. Background
Cardiovascular diseases (CVDs) include coronary artery disease (CAD) and cerebrovascular disease [1]. The incidence of CVD is rapidly increasing worldwide, with approximately 17.9 million people having died from CVD in 2019, accounting for 32% of the global death toll [1]. The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 announced that the prevalence of CVD from 1990 to 2019 had approximately doubled from 271 million to 523 million, and mortalities due to CVD had also increased steadily from 12.1 million to 18.6 million [2]. In Korea, the mortality rate from CVD reached 61.5 per 100,000 people in 2021 [3]. The increase in the mortality rate from CVD among the population aged 25~64 years in the United States [4] has necessitated the implementation of health management programs to reduce the mortality rate.
CAD, which is the most rapidly increasing CVD, is caused by an inability to provide oxygen to the heart muscles due to the development of cortical sclerosis in the coronary arteries and is a typical condition of angina and myocardial infarction [5]. Percutaneous coronary intervention (PCI) is a typical treatment method used to prevent the progression of ischemia and infarction in CAD [6]. The number of PCIs conducted in Korean medical institutions in 2019 has steadily increased with the prevalence of CAD [7]. Patients who underwent PCI had a 31% reduction in CVD mortality and fewer cardiovascular events than those who underwent drug treatment [6]. Despite successful PCI intervention, restenosis and heart disease occur in 15%~50% of patients [8]; therefore, active and consistent healthy behavior involving lifestyle correction is important, even after patients with CAD receive PCI [9].
Patients with CAD may be uncertain about symptoms or post-treatment outcomes for the diagnosis of myocardial infarction or angina and the implementation of PCI [10]. Mishel [11] discussed the ongoing uncertainty among those with chronic diseases that are likely to recur and require continuous care. Mishel’s uncertainty in illness theory (UIT) [12] suggests that uncertainty is a meaningful factor in life. Mishel [11] argued that uncertainty management is important for disease adaptation, and that the primary purpose is to manage uncertainty in chronic diseases through providing a new perspective on life in which uncertainty is normalized.
For patients with CAD who face threats to their lives, uncertainty concerning their survival or prognosis acts as a serious psychosocial stressor. Over 30% of CAD patients experience anxiety and depression [13], which further exacerbates uncertainty [14]. Therefore, it is crucial to address the significant psychological issues caused by uncertainty. The latest tests or treatments for events occurring in the course of transdermal coronary interventions and medications can all be perceived as threats [10]. Moreover, uncertainly negatively affect the performance of health-related activities, such as physical activity and treatment instruction implementation [15]. Therefore, an intervention program should be developed to effectively maintain health through identifying the level of uncertainty in patients with CAD, thereby providing a theoretical basis for reducing or resolving uncertainty and promoting healthy behaviors.
UIT has been applied to patients with chronic diseases such as CAD [10], systemic lupus erythematosus [16], and cancer [17], as well as those undergoing hemodialysis [18]. Most studies have shown a relationship between uncertainty and several factors, such as social support and quality of life. Studies concerning the application of UIT to patients with CAD include a comparative study of psychological factors such as uncertainty levels, depression, and anxiety in patients undergoing PCI and coronary artery bypass graft surgery (CABG) [19] and a correlation study of uncertainty and coping [20].
A recent study investigated the predictive variables related to uncertainty in patients with CABG [10]; another employed a structural equation model to examine the mediating role of uncertainty in illness and depressive symptoms between symptom distress and health-related quality of life in patients with heart failure [14]. However, few studies have been conducted in relation to factors required to develop an intervention strategy to manage the uncertainty experienced by patients undergoing PCI following a diagnosis of CAD. Factors involved in well-performing health behaviors to reduce mortality and complications, and ultimately to improve quality of life in the presence of uncertainty, particularly when evaluating uncertainty as an opportunity or danger, need to be examined. Specifically, the health behavior of patients with CAD is directly related to their prognosis, and these health behaviors significantly impact the quality of life of patients [9, 15]. Therefore, it is important to investigate predictive variables that influence the health behaviors of patients experiencing uncertainty and to identify a simple yet optimal path through which uncertainty indirectly affects health behavior via path analysis. This will provide evidence for enhancing health behaviors among CAD patients experiencing uncertainty.
This study aimed to examine the optimal paths from uncertainty to health behavior based on reconceptualized Mishel’s UIT [11] through verifying the effects of perceived benefit and intention, perceived risk, social support, and self-efficacy on the path among patients with CAD who underwent PCI.
2. Theoretical foundation and hypothetical model
This study’s theoretical foundation and hypothetical model were derived from Mishel’s [11] reconceptualized UIT (Figure 1). uncertainty arises from the inability to accurately define disease-related events and situations and the lack of sufficient information to predict treatment outcomes [12]. The UIT explains how patients perceive uncertainty and structure meaning about disease-related events [21]. The original model of UIT focuses on the uncertainty experienced by acutely ill patients, while the reconceptualized UIT addresses the processes and outcomes experienced by patients living with uncertainty in chronic diseases or with the potential for recurrence. Therefore, this study emphasized the process and outcomes following uncertainty in patients with CAD based on the reconceptualized UIT.
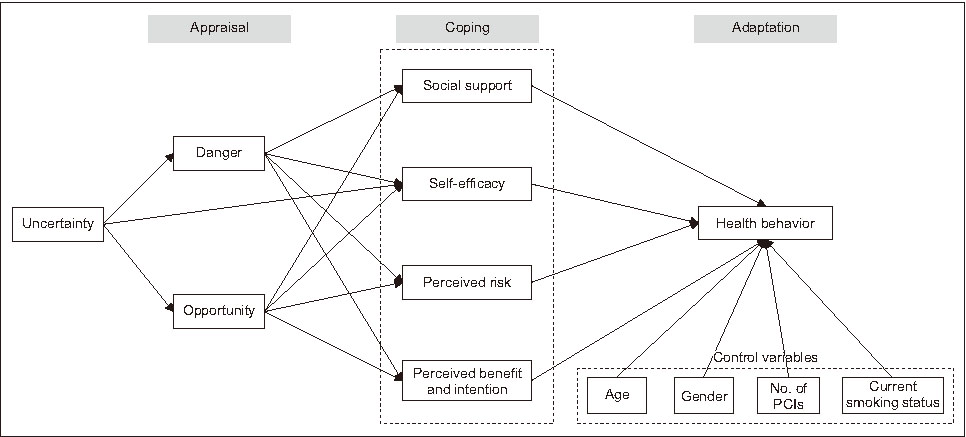
Figure 1
Hypothesized model.
No. = Number; PCI = Percutaneous coronary intervention.
The appraisal of uncertainty involves evaluating uncertainty as an opportunity or a threat [12]. After evaluating uncertainty, the next step is coping strategies, which were categorized into affect-control and buffering strategies [22]. While this study did not explicitly differentiate affect-control and buffering strategies, affect-control involves recognizing one’s emotions and selecting and regulating thoughts or actions that emphasize positive emotions or alleviate negative emotions, so variables such as self-efficacy [15, 23], perceived risk [24], perceived intention, and benefit [10] were set. Buffering strategy involves utilizing external support systems and social support systems, hence social support [10] was set as a variable. These coping strategy-related variables are crucial for coping with uncertainty and positively impacting health behaviors [10, 15, 23, 24].
Patients living with chronic uncertainty due to CAD require careful self-management, and health behavior is the core of self-management [9]. Therefore, in this study, the adaptation state of CAD patients was set as performing health behaviors. Even if uncertainty is initially evaluated as a threat rather than an opportunity in the reconceptualized model, over time, the evaluation of uncertainty may shift from risk to opportunity, leading to a reconstruction of perspectives on life and adaptation [11]. Therefore, it is deemed essential to identify the optimal path through which uncertainty affects adaptation (health behavior) through coping strategies, regardless of whether uncertainty is appraised as an opportunity or a threat [11]. Based on prior literature [25], this study attempted to explore the optimal path by adding a new path as uncertainty would be directly related to self-efficacy. This study aims to validate hypotheses related to this premise. Therefore, the hypothetical model of this study is as follows:
(1) Uncertainty will directly influence uncertainty appraisal (danger and opportunity).
(2) Uncertainty appraisal (danger and opportunity) will directly influence coping with uncertainty (social support, self-efficacy, perceived risk, perceived benefit and intention).
(3) Coping with uncertainty (social support, self-efficacy, perceived risk, perceived benefit and intention) will directly influence health behavior.
(4) Uncertainty will indirectly influence health behavior through uncertainty appraisal (danger, opportunity) and coping with uncertainty (social support, self-efficacy, perceived risk, perceived benefit and intention).
(5) We will identify the most effective path (Uncertainty → Self-efficacy) among the indirect pathways from uncertainty to health behavior (Figure 1).
METHODS
1. Study design
In this study, based on Mishel’s reconceptualization of the UIT model [11], we established a hypothetical model that included influencing factors explaining the adaptation process of patients with CAD. Cross-sectional data were collected from patients with CAD. This study presents a path model construction to verify the suitability and hypotheses of the path model.
2. Setting and sample
This study comprised patients with CAD, such as angina pectoris or myocardial infarction, who had been diagnosed by an internal medicine specialist, who then received follow-up care from the outpatient department of Cardiology Medicine at Pusan National University Hospital in Busan Metropolitan City. The inclusion criteria were as follows: (1) patients aged ≥ 18 years who had been diagnosed with CAD at a medical institution and (2) those who had undergone PCI within the past five years. The exclusion criteria were as follows: (1) patients with dementia or a history of cognitive impairment or mental illness; (2) patients with serious diseases (e.g., end-stage renal disease, cancer, stroke) that would affect their quality of life within one year; and (3) patients who had difficulty understanding and answering the questionnaire owing to cognitive issues. All participants provided informed consent prior to participation.
This study required a sample size of five times the free parameters, including all error variables and path coefficients [26]. We used maximum likelihood estimation, which is the most common estimation method in structural equation model analysis, and the number of samples was calculated based on a sample size of 100~150 [27]. A total of 44 free parameters were included in the hypothetical model. A questionnaire was administered to 242 individuals accordingly, an increase of 10% from the minimum 220 individuals required. Questionnaires with more than 10% missing values for each measurement tool were excluded from the analysis, and missing values were replaced with the mean. As a result, a total of 228 questionnaires were included in the analysis.
3. Measurements
1) Socio-demographic and disease-related characteristics
Socio-demographic characteristics of the participants were investigated using a self-report questionnaire based on gender, age, educational level, occupation, and smoking status. Disease-related characteristics; diagnosis, body mass index (BMI), CAD-related medical history; family history of CVDs, left ventricular ejection fraction (LVEF), number of diseased vessels, duration of disease, and number of PCI were investigated through examining hospital medical records.
2) Uncertainty in illness
In this study, the Korean version of Mishel’s Uncertainty in Illness Scale (MUIS) [28] was used [29]. The MUIS consists of 33 items in four domains of uncertainty: 13 items on ambiguity, seven on complexity, seven on inconsistency, five on unpredictability, and one not included in the four domains. The total score used for the analysis was calculated through summing the scores of each sub-item, with a higher score indicating higher uncertainty. Confirmatory factor analysis (CFA) of the measurement revealed four items with low regression weights that were deleted because of a low fit, leaving 29 measurable items. After adjustment, CFA showed that the measurement model fit the data better than the original model (χ2 = 516.40, χ2 / df [degree of freedom] = 1.70, standard root mean square residual [SRMR] = .07, goodness of fit index [GFI] = .86, comparative fit index [CFI] = .91, and root mean square error of approximation [RMSEA] = .06). Cronbach’s α was .91 in the original study [28] and .90 in the present study.
3) Uncertainty appraisal
The uncertainty appraisal scale consists of 15 items derived through item analysis by Mishel & Sorenson [30]; in this study, the Korean version of the scale was used [31]. This measure consists of two domains, with seven items measuring uncertainty appraisal as an opportunity and eight items measuring uncertainty appraisal as a danger. Responses were recorded on a self-reporting six-point Likert scale. The average score of the items in each domain was used for the analysis, and a higher score in each domain indicated that uncertainty was evaluated as an opportunity or danger. CFA showed that the measurement model fit the data (χ2 = 187.47, χ2 / df = 2.80, SRMR = .08, GFI = .90, CFI = .96, and RMSEA = .08). Cronbach’s α of opportunity appraisal was .82 and that of danger appraisal was .87 in a previous study [30]. In this study, Cronbach’s α of danger appraisal was .94 and that of opportunity appraisal was .92.
4) Social support
This study used the Korean version of the measurement developed by the RAND Medical Outcomes Study (MOS) team [32] and adapted by Lim et al. [33]. This comprises of 19 items, each consisting of four domains: eight items measuring emotional/informational support, four items measuring explicit support, three items measuring affectionate support, three items measuring positive interactions, and one additional item.
Responses to the items were rated on a five-point Likert scale. The scores for each subscale range from 0 to 100, and the total social support score ranges from 0 to 100. The higher the total social support score, the greater the social support. CFA showed that the measurement model fit the data (χ2 = 322.33, χ2 / df = 2.50, SRMR = .03, GFI = .90, CFI = .97, and RMSEA = .08). Cronbach’s α was .97 in a previous study [32] and .98 for the present study.
5) Self-efficacy
In this study, we used the Patient-Reported Outcomes Measurement Information System (PROMIS®) Item Bank v1.0 (FACIT) - Self-Efficacy for Managing Chronic Conditions - Managing Symptoms-Short Form 4a and PROMIS® Item Bank v1.0 - Self-Efficacy for Managing Chronic Conditions Managing Medications and Treatment-Short Form 4a. The Korean versions of the two item banks were provided and used by the PROMIS® translation department team following a license agreement process. The scale comprises four items measuring medication and treatment management, and four items measuring symptom management. Responses are recorded on a five-point Likert scale. The total score ranges from 1 to 20 points for each subscale, and the higher the total score, the higher the self-efficacy for drug and treatment management and symptom management. CFA showed that the measurement model fit the data (χ2 = 50.53, χ2 / df = 3.40, SRMR = .03, GFI = .95, CFI = .98 and RMSEA = .08). Cronbach’s α was .96~.97 in a previous study [34]; in the present study, Cronbach’s α for symptom management self-efficacy was .94, and Cronbach’s α for medication and treatment management was .90.
6) Perception of risk, benefit, and intention
The Attitudes and Beliefs about Cardiovascular Disease Risk Questionnaire is a tool used to measure a patient’s perspective on CVD risk and includes four scales: knowledge of CVD risk and prevention, perceived risk of heart attack/stroke, perceived benefit and intention to change, and healthy eating intention [35]. As the purpose of the present study was to measure patients’ perceptions and intentions to change to healthy behaviors, knowledge of CVD risk and prevention was excluded.
The researcher translated the questionnaire into Korean and a professional translator corrected and back-translated it. After translation, based on the results of exploratory factor analysis and expert panel review comments, it was revised into two scales: perceived risk of heart attack/stroke (eight items) and perceived health behavior benefits and intentions (ten items). Responses were recorded on a four-point Likert scale. A higher score indicates a higher perception of the risk of having a heart attack or stroke, and a higher perceived benefit and readiness for change with regard to exercise and diet behavior. Based on the CFA results for the two scales, ‘I do not intend to exercise for about 2.5 hours a week’ was deleted from the perceived benefit and intention of health behavior scales because the factor loading, the value of the item, and the overall model fit were low. CFA showed that the measurement model fit the data (χ2 = 180.19, χ2/df = 1.80, SRMR = .08, GFI = .93, CFI = .97, and RMSEA= .06). Cronbach’s α for perceived risk, perceived benefit and intention to change behavior, and healthy eating intentions were .85, 82, and .56 prospectively in Woringer et al.’s study [35]. In this study, Cronbach’s α was .80 for perceived risk of heart attack/stroke, and .73 for perceived benefit and intention to change health behavior.
7) Health behavior
The Cardiac Health Behavior of Korean Adults was developed to evaluate the health behavior of Korean adults diagnosed with CVD or with a risk of CVD [36]. This measurement scale comprises 21 items on five subscales: health responsibility, exercise, diet behavior, stress management, and smoking cessation, with responses evaluated using a four-point Likert scale. The score of each subscale is summed and divided by the number of items in each subscale to calculate the final score. The higher the score on the subscale or the total health behavior score, the better the cardiac health behavior. CFA showed that the measurement model fit the Cronbach’s α was .83 in a previous study [36], and .88 in the present study.
4. Data collection
The data were collected between September 2020 and June 2021. The project investigator explained the purpose of the study to three cardiologists and obtained their cooperation in data collection. One researcher and one research assistant surveyed the patients, and another researcher collected the patients’ disease-related characteristic data from electronic medical records.
The researcher and research assistant explained the purpose of the study and the questionnaire response method to patients who visited the cardiology outpatient department and then distributed the questionnaire to the participants who provided written consent. The participants undertook the questionnaire in the outpatient clinic of the Department of Cardiology, which took approximately 25~30 minutes to complete.
5. Data analysis
Data were analyzed using SPSS win 25.0 and AMOS 25.0 software (IBM Co.). Descriptive statistics were used for participants’ characteristics and major variables, a t-test and ANOVA were used for differences in health behavior according to participants’ characteristics, and the Scheffé test was used for post-hoc testing. Covariate structural analysis was performed to test the hypothetical model. The normality of the measured variables and multicollinearity between variables were tested through calculating the correlation coefficients, skewness and kurtosis, variance expansion factors and tolerance limits, and state indices. The Durbin–Watson index was used for the autocorrelation of the dependent variables [37].
The reliability of each measurement tool was calculated using Cronbach’s α, and CFA was performed to verify its validity. To verify the model’s fit, χ2, normed χ2 (χ2 / df), GFI, SRMR, CFI, and RMSEA were used, as recommended by Kline [37]. The model was evaluated as acceptable when χ2 was small and p > .05, χ2 / df was ≤ 3, SRMR and RMSEA were ≤ .08, and GFI and CFI were > .90. The significance of the model path was confirmed using the regression coefficient, standard error, threshold, and a p-value. Statistical significance was set at a critical ratio (CR) of ≥ 1.965 and p < .05. Two-tailed significance was used, and the significance of the direct and total effects was verified at p < .05. For the indirect effect, a 95% confidence interval (CI) was obtained using the bootstrap method, and the number of bootstrap samples was set to 5,000. When there are multiple mediating variables in a multiple-mediator model, phantom variables are used to verify the differences between specific indirect effect paths. In this study, path analysis was conducted step by step for Model 1 and Model 2. Model 1, as suggested in the theory, tested a model consisting of a sequential path from uncertainty, uncertainty evaluation, various coping strategies, and health behavior. Model 2 tested the model that omitted the uncertainty assessment step in Model 1, establishing a direct path from uncertainty to self-efficacy [11, 25]. If control variables are used in structural equation models, the model better reflects reality in as far as possible and can be more readily applied in practice. Moreover, the influence of independent variables on dependent variables in a research model needs to be measured as accurately as possible [38]. In this study, therefore, based on a literature review, age, gender, smoking status, and the number of PCIs [2, 6, 10] were set as control variables that may affect the health behavior of patients with CAD. Gender and PCI frequency were changed to dummy variables and analyzed.
6. Ethical consideration
This study was approved by the Institutional Review Board of Pusan National University Hospital (approval no. H-2007-025-093). All aspects of the study were explained to potential participants. Those who agreed to participate signed a written consent form prior to data collection.
RESULTS
1. Study participant characteristics
Among the participants, 171 (75.0%) were men, the average age was 64.6 years (range, 36.0~88.0), and the average BMI was 25.34 kg/m2 (range, 16.0~49.6). Regarding medical history, 137 (60.1%) patients had hypertension, and 145 (63.6%) were diagnosed with myocardial infarction. The mean LVEF was 53.7% (range, 28.0~72.0), and 101 patients (44.3%) had one diseased vessel. Concerning disease duration, 124 (54.4%) patients had a disease duration > 1 year, and 189 (82.9%) participants had undergone PCI for the first time (Table 1).
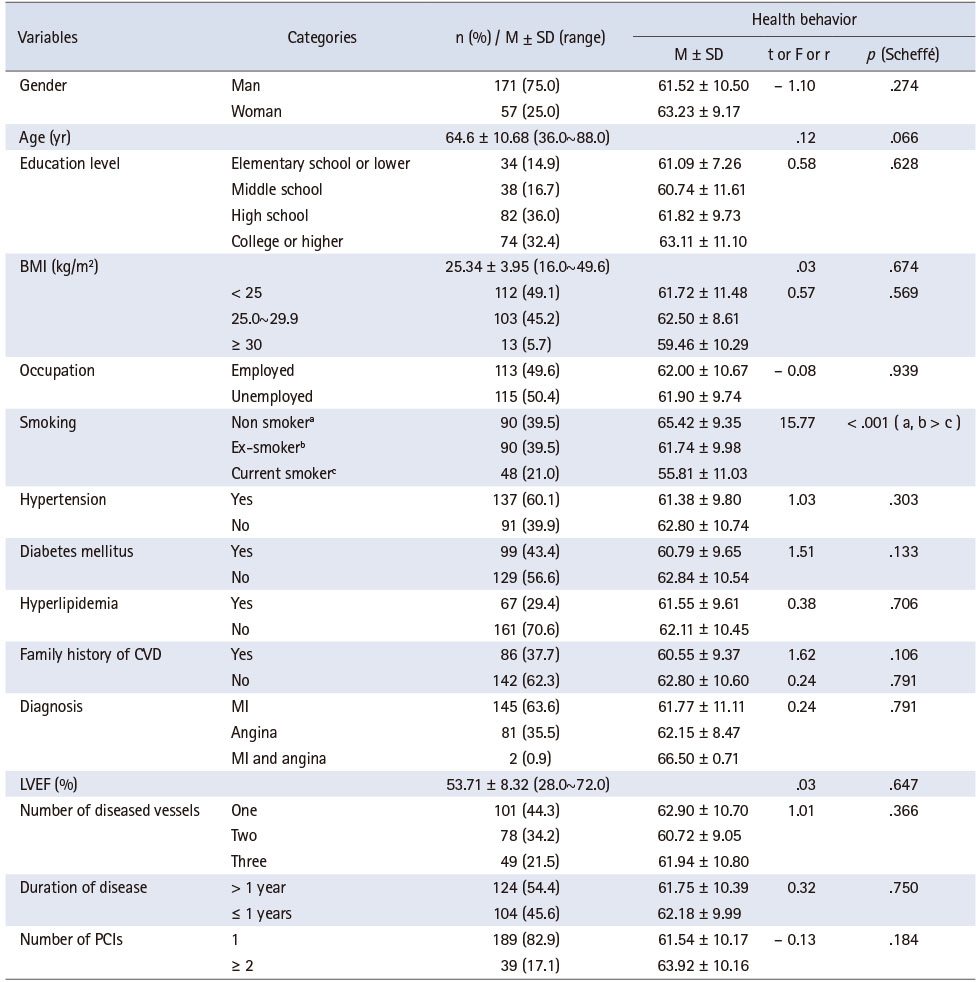
Table 1
Differences in Health Behavior in Relation to Patient Characteristics (N = 228)
As a result of examining the differences in participants’ characteristics according to health behavior, the only statistically significant difference in health behavior was current smoking status. The post-test results showed that the health behavior scores of former smokers and non-smokers were higher than those of current smokers.
2. Descriptive statistics, and correlation among the main variables
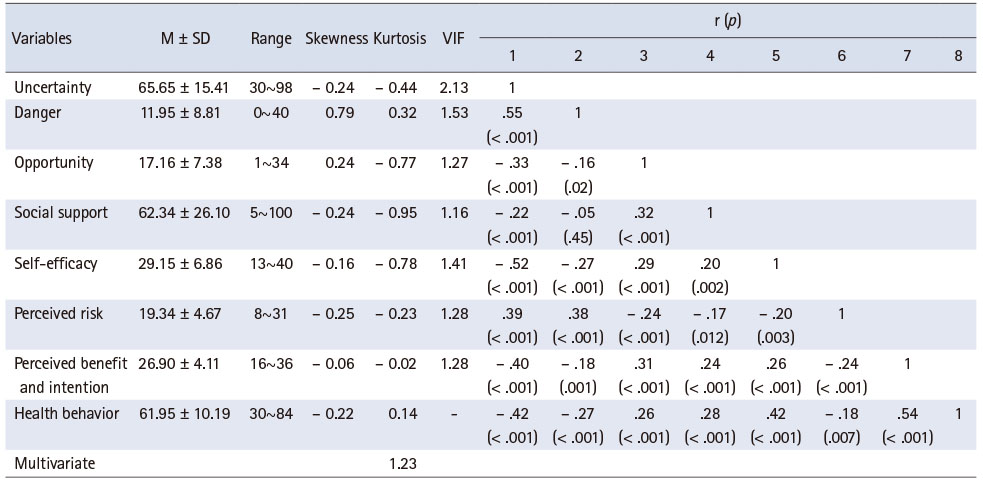
Table 2 presents the descriptive statistics and correlations among the variables. In this study, the multivariate kurtosis index was 1.23, which was less than the threshold of 23.69 at df = 14, and α = .05, and multivariate normality was satisfied. Furthermore, there was no issue with multicollinearity because all values of tolerance limits among the measurement variables were .47~.86 (> .10), and all variance inflation factors were 1.16~2.13 (< 10).
Table 2
Descriptive Statistics and Correlation among the Measurement Variables (N = 228)
The correlation coefficient between all variables was statistically significant, except for that between uncertainty opportunity appraisal and social support. The variables highly correlated with health behavior were uncertainty (r = -.42, p < .001), self-efficacy (r = .42, p < .001), and perceived benefit and intention (r = .54, p < .001).
3. Model fit of the hypothetical model
As a result of testing Model 1, all fit indices were found to be unacceptable, so the hypothesized model was modified (χ2 = 147.45, χ2 / df = 3.88, GFI = .89, SRMR = .09, CFI = .79, RMSEA = .11). The decision criteria for modifying the hypothetical model were based on the significance of fit indices, path coefficients, and modification indices. Sequentially deleting paths with low coefficients resulted in removing five paths: from danger to social support and self-efficacy, from perceived risk to health behavior, and from gender and number of PCIs to health behavior. Consequently, the fit indices indicated with some fit indices were not acceptable (χ2 = 162.55, χ2 / df = 3.78, GFI = .90, SRMR = .09, CFI = .77, RMSEA = .11).
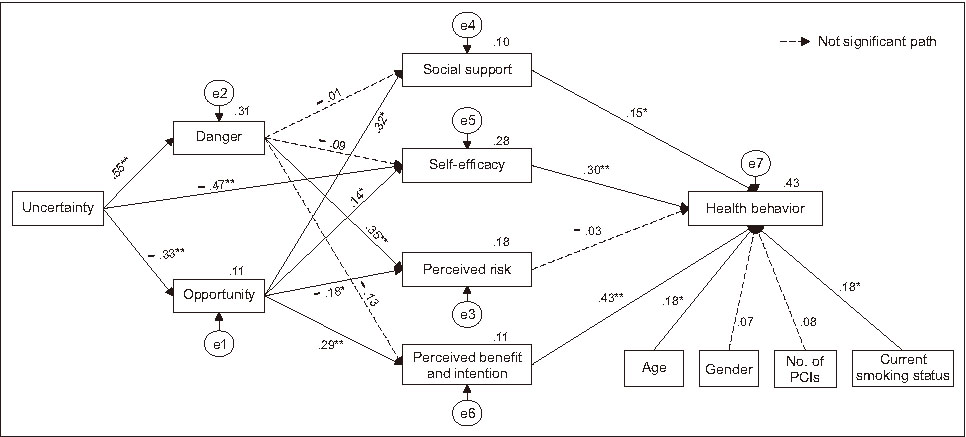
We tested Model 2 (Figure 2) to identify the optimal path and found that all goodness-of-fit indices were acceptable (χ2 = 79.19, χ2 / df = 2.83, SRMR = .07, GFI = .94, CFI = .90, RMSEA = .09). The χ2 difference test was performed to evaluate whether there was an improvement in the model fit [37], χ2 statistic decreased from 147.45 to 79.19, and df decreased by 10 (38~28), which was significant at α = .05 level. Additionally, the remaining fit indices generally satisfied the hypothesis model; therefore, Model 2 was selected as the optimal model.
Figure 2
*p < .01, **p < .001.
Standardized estimates of the final model.
e = Error term of each indicator; PCI = Percutaneous coronary intervention.
4. Path analysis of the model
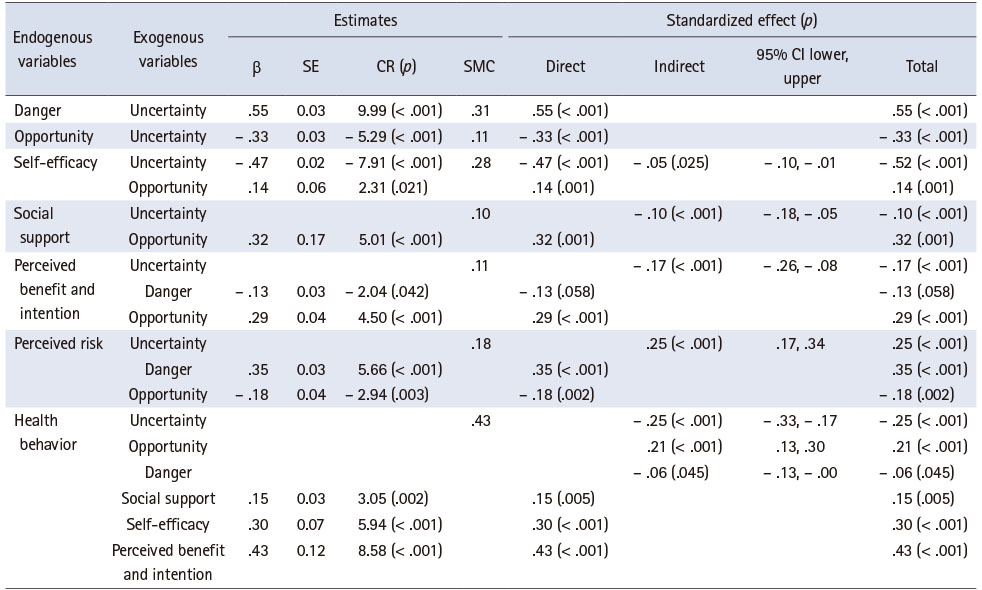
In Model 2, the analysis of individual paths between variables, excluding covariance, showed that 11 of the 12 paths were significant (Figure 2, Table 3). Uncertainty had a negative direct effect on opportunity (β = -.33, p < .001) and a positive direct effect on danger (β = .55, p < .001). Unlike the hypothetical path, uncertainty had a negative direct effect on self-efficacy (β = -.47, p < .001). Opportunity appraisal had a direct effect on social support (β = .32, p = .001), perceived risk (β = -.18, p = .002), self-efficacy (β = .14, p = .001), and perceived benefit and intention (β = .29, p < .001). Danger appraisal had a direct effect on perceived risk (β = .35, p < .001). Social support (β = .15, p = .005), self-efficacy (β = .30, p < .001), and perceived benefit and intention (β = .43, p < .001) had direct effects on health behavior.
Table 3
Estimates, Direct, Indirect, and Total Effects of the Modified Model (N = 228)
As a result of analyzing the indirect effects, the largest indirect effects on health behavior were in relation to perceived benefit and intention (β = .43, p < .001), self-efficacy (β = .30, p < .001), and uncertainty (β = -.25, p < .001).
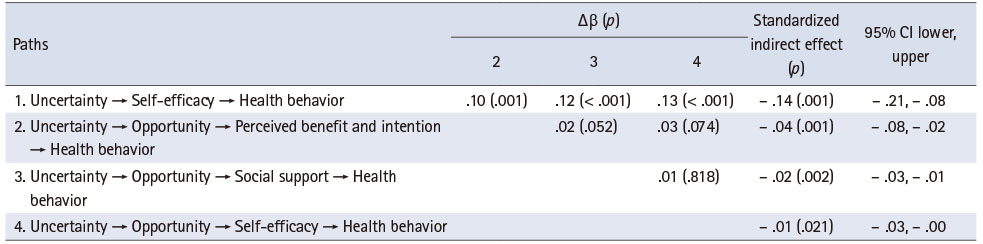
In the path model of this study, the relationship between uncertainty and health behavior can be explained by several indirect paths. The total indirect effect of uncertainty on health behavior was significant (β = -.25, 95% CI = -.33~-.17). Statistical differences in the four specific indirect effect paths were significant (Table 3). According to the results, the simple mediating effect through self-efficacy (β = -.14, 95% CI = .21~-.08) was most effective.
The results of validating the hypotheses of this study are as follows:
(1) It was confirmed that uncertainty directly influences uncertainty appraisal, thus confirming the hypothesis.
(2) The danger was found to influence perceived risk directly, while the opportunity was found to influence social support, self-efficacy, perceived risk, perceived benefit, and intention directly, partially confirming the hypothesis.
(3) Social support, self-efficacy, perceived benefit and intention were found to influence health behavior, partially confirming the hypothesis directly.
(4) Three indirect paths in the hypothetical model of this study were validated.
(5) We identified that the indirect effect of uncertainty on health behavior through self-efficacy is the most effective and straightforward optimal path (Table 4).
Table 4
Specific Indirect Effects of Uncertainty in Relation to Health Behavior
DISCUSSION
The primary purpose of this study was to examine factors that predict the health behavior of patients with CAD who experience uncertainty, based on Mishel’s UIT [11]. After constructing a hypothetical model to predict health behavior according to uncertainty appraisal (opportunity or danger), the statistical causal relationship between the factors was examined. The results revealed that the health behavior of patients with CAD were directly and indirectly related to uncertainty, uncertainty appraisal, social support, self-efficacy, perceived benefit and intention. These results were statistically confirmed as suitable as a path model for predicting the health behavior of patients with CAD.
Mishel [12] suggested that when individuals experience uncertainty, they cognitively evaluate it as an opportunity or a danger. The study findings indicate that the two paths in relation to uncertainty and uncertainty appraisal in terms of opportunity and danger, were statistically significant. This supports the results of a previous study that examined the correlation between uncertainty and uncertainty appraisal [18]. Evaluating uncertainty as an opportunity has positive implications for an event or situation, based on beliefs or purposeful misinterpretations, whereas evaluating it as a danger generally occurs when considering the possibility of a negative outcome [12].
The study patients had marginally higher opportunity appraisal scores than danger appraisal scores, similar to the reported uncertainty evaluation scores of patients with chronic diseases such as cancer [31] and those undergoing hemodialysis [18]. Considering that an average of 26 months had passed since the initial diagnosis, it can be assumed that the participants in this study had developed a new perspective on life in which uncertainty was accepted as a natural part of life. For patients with colorectal cancer who evaluated uncertainty as a danger, a mobile navigation program was structured around the enhancement of nursing continuity and empowerment, and was effective for growth through uncertainty [39]. Long-term exposure to uncertainty can lead to intrusive thinking, avoidance, and severe emotional distress [11]. Therefore, it is necessary to identify those who evaluate uncertainty as a danger immediately after receiving a diagnosis of CAD and to apply nursing interventions that help them experience a successful life transition more rapidly. Therefore, studies should explore the process by which patients with CAD evaluate uncertainty as an opportunity and identify strategies that are effective for growth.
According to Mishel [11], the effect of uncertainty as an outcome of adaptation is ultimately related to the effect of coping to reduce uncertainty, evaluated as a danger, or to maintain uncertainty evaluated as an opportunity. The results of this study showed that, when uncertainty was evaluated as an opportunity, self-efficacy, social support, perceived benefit and intention were significant in attaining health behavior. However, when uncertainty was evaluated as a danger, only the factors of perceived benefit and intention significantly affected health behavior. In addition, the mediator variable, which had an indirect effect on health behavior, had more significant paths to opportunity than to danger. These results suggest that nursing interventions performed for patients who evaluate uncertainty as an opportunity may be effective in improving the health behavior of patients with CAD. Thus, it is pivotal to appraise a patient’s uncertainty before implementing nursing interventions aimed at promoting and improving their health behavior.
In terms of the relationship between uncertainty appraisal and health behavior we found, first, that perceived benefit and intention were the only effective parameters to promote the health behavior of participants who evaluated CAD as a danger and that these were the most effective parameters for participants who evaluated CAD as an opportunity. Therefore, nursing interventions aimed at increasing the perceived benefit and intention to enhance the health behavior of patients who experience uncertainty and evaluating uncertainty as either an opportunity or danger are the most effective. A systematic literature review indicated that disease awareness, such as methods for alleviating the symptoms of the disease, is important for promoting positive health behaviors [40]. Rather than simply educating patients on how to exercise and maintain a healthy diet, presenting in detail how exercise and eating habits benefit health promotion can improve their motivation to implement these habits [41]. In a prior study that applied an intervention program for patients with CAD based on the health promotion model, perceived exercise benefit was shown to increase in the experimental group; furthermore, perceived barriers decreased, and self-efficacy increased [42]. Therefore, it would appear that nurses need to focus on and provide support in terms of how health behaviors such as exercise, healthy diet, and smoking cessation affect symptom improvement, function improvement, complication prevention, and good prognosis when providing health-related information to patients with CAD.
In contrast, the path from perceived risk to health behavior was not significant. For participants who evaluated uncertainty as a danger, the effect of the path on danger recognition was considerable. However, for those who evaluated uncertainty as an opportunity, the relationship was negative and the size of the effect was smaller than that of danger appraisal. A comparison of patients with CVD with and without risk perception revealed that those with risk perception had significantly higher anxiety and depression scores [43]. Therefore, to promote the health behavior of patients with CVD experiencing uncertainty, we recommend educating such patients on the benefits of maintaining a healthy lifestyle and applying strategies that can continue to motivate them, rather than emphasizing the negative risk perception of the health outcome of their diagnosis.
Our study results showed that self-efficacy was the second most effective factor for promoting the health behavior of participants who evaluated uncertainty as an opportunity. In a previous study, self-efficacy was shown to directly affect the health behavior of Korean patients with CAD [9]. Regarding the relationship between social support and physical activity, self-efficacy has been reported to be a crucial factor in promoting physical activity in patients with CAD [44] and a leading factor in the implementation of health behaviors in many previous studies [15, 23].
In this study, paths sequentially linked to uncertainty, self-efficacy, and health behavior were also identified. Among the four specific indirect effects of uncertainty on health behavior, the ‘Uncertainty → Self-efficacy → Health behavior’ path had the largest specific indirect effect, and there were statistical differences between this path and the other paths. This finding indicates that self-efficacy is an important mediating factor for uncertainty and health behavior, even without any evaluation process for uncertainty. The more nursing interventions that can increase self-efficacy are implemented for patients experiencing uncertainty, the more effective and more quickly implemented their health behaviors are likely to be. In a previous study, healthcare providers applied goal-setting in relation to health behavior, feedback, and motivation-reinforcement strategies to improve self-efficacy [45]. However, given advances in technology, more recent prevention and personalized digital therapeutics, such as identifying an individual’s digital phenotype through machine learning and designing a customized nursing intervention model, should be attempted [46].
Social support indirectly affected the promotion of health behavior in patients with CAD who evaluated uncertainty as an opportunity, which is consistent with previous studies [10, 41, 47]. Mishel [11] emphasized in the reconceptualization of the UIT that social support could be a key coping strategy rather than a precursor to uncertainty, highlighting its essential role in managing uncertainty. Social support can manifest in various forms such as information provision, emotional support, and psychological stability [32], which helps enhance patients’ ability to cope with uncertainty [11]. In previous studies, institutional support and interventions providing information and skills education to enhance self-assessment and positive perception effectively reduced uncertainty [25]. Therefore, nursing programs promoting health behaviors in CAD patients should focus on enhancing various forms of social support.
However, this study had some limitations. As this study only collected data from patients with CAD who visited a single tertiary general hospital in one city, there may have been sampling bias; thus, caution is needed when interpreting the study results. Additionally, it was difficult to accurately analyze the uncertainty of early CAD given that patients were recruited with a progression period of less than five years. In future studies, it is recommended to evaluate patients’ uncertainty regarding early CAD using patient data within one year of such patients receiving PCI. Furthermore, this study did not include variables such as knowledge about CAD, educational level, levels of depression, and anxiety, which may influence uncertainty. Therefore, research incorporating a variety of variables, including the preceding factors in the original model, is needed to understand their impact on health behaviors. Further research is needed to develop an integrated intervention based on the predictive factors of health behavior identified in this study and to examine its effectiveness.
Despite these limitations, the present study is meaningful because it empirically examined the effective path of health behavior according to uncertainty evaluation among patients with CAD, based on Mishel’s UIT [11], through examining two hypothetical pathways to health behavior as a patient role adaptation according to uncertainty appraisal. Furthermore, it has practical implications in that it provides evidence-based findings in relation to developing nursing interventions to improve the health behaviors of patients with CAD experiencing uncertainty. For patients diagnosed with CAD to experience successful transition and to improve health behavior performance, education or support programs can be developed that recognize the benefits of self-efficacy and suitable health behavior and strengthen relationships that can help provide support from families and loved ones through accurate information provision and motivation reinforcement.
CONCLUSION
This study investigated the level of uncertainty in patients with CAD who had undergone PCI and identified several significant factors in the path between their uncertainty and health behavior. We found that the paths for uncertainty evaluation in terms of danger and opportunity were significant. However, when evaluating uncertainty as a danger, only the parameters of perceived benefit and intention were significant. When evaluating uncertainty as an opportunity, social support, self-efficacy, perceived benefit and intention were significant. Furthermore, through evaluating differences in specific indirect effect paths, the indirect effect size of the path leading to health behavior as mediated in terms of self-efficacy under uncertainty was found to be the largest. Therefore, when patients experience uncertainty, interventions that increase their self-efficacy are urgently required. Furthermore, developing programs that can help patients quickly transform viewing uncertainty as a danger into an opportunity is worthwhile. Finally, increasing social support and self-efficacy through focusing on the perceived benefit and intention of health behavior may benefit patients.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Lee YJ & Jeong H & Lee YS & Park J.
Data curation or/and Analysis: Jeong H & Lee YJ.
Funding acquisition: None.
Investigation: Jeong H & Lee YS.
Project administration or/and Supervision: Lee YJ.
Resources or/and Software: Jeong H & Lee YS & Park J.
Validation: Jeong H & Lee YS.
Visualization: Lee YJ & Jeong H.
Writing original draft or/and Review & Editing: Lee YJ & Jeong H & Lee YS & Park J.
ACKNOWLEDGEMENTS
The authors acknowledge the contributions of all the study participants.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
World Health Organization (WHO). Cardiovascular diseases (CVDs) [Internet]. WHO; c2021 [cited 2023 May 3].Available from: https://www.who.int/news-
room/fact- sheets/detail/cardiovascular- diseases- (cvds) .
-
-
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 Study. Journal of the American College of Cardiology 2020;76(25):2982–3021. [doi: 10.1016/j.jacc.2020.11.010]Erratum in: Journal of the American College of Cardiology. 2021;77(15):1958-1959.
-
-
Korea National Statistical Office. Statistics on causes of death [Internet]. Statistics Korea; c2019 [cited 2023 May 3].
-
-
Chacko L, Howard JP, Rajkumar C, Nowbar AN, Kane C, Mahdi D, et al. Effects of percutaneous coronary intervention on death and myocardial infarction stratified by stable and unstable coronary artery disease: A meta-analysis of randomized controlled trials. Circulation: Cardiovascular Quality and Outcomes 2020;13(2):e006363 [doi: 10.1161/CIRCOUTCOMES.119.006363]
-
-
Health Insurance Review & Assessment Service (HIRA). Results of the 6th adequacy evaluation for coronary artery bypass surgery [Internet]. Health Insurance Review & Assessment Service; c2020 [cited 2021 Aug 10].Available from: https://www.hira.or.kr/cms/open/04/04/12/2020_
3.pdf .
-
-
Ahn S, Song R, Choi SW. Effects of self-care health behaviors on quality of life mediated by cardiovascular risk factors among individuals with coronary artery disease: A structural equation modeling approach. Asian Nursing Research 2016;10(2):158–163. [doi: 10.1016/j.anr.2016.03.004]
-
-
White RE, Frasure-Smith N. Uncertainty and psychologic stress after coronary angioplasty and coronary bypass surgery. Heart & Lung 1995;24(1):19–27. [doi: 10.1016/s0147-9563(05)80091-3]
-
-
Budner S. Intolerance of ambiguity as a personality variable. Journal of Personality 1962;30(1):29–50. [doi: 10.1111/j.1467-6494.1962.tb02303.x]
-
-
Cho SH, Yun KS. Influence of uncertainty, physiologic risk factors, self-efficacy on self-management in stroke patients. Journal of Muscle and Joint Health 2016;23(2):114–124. [doi: 10.5953/JMJH.2016.23.2.114]
-
-
Thompson NM, Bevan JL, Sparks L. Healthcare reform information-seeking: Relationships with uncertainty, uncertainty discrepancy, and health self-efficacy. Journal of Communication in Healthcare 2012;5(1):56–66. [doi: 10.1179/1753807611Y.0000000016]
-
-
Bentler PM, Chou CP. Practical issues in structural modeling. Sociological Methods & Research 1987;16(1):78–117. [doi: 10.1177/0049124187016001004]
-
-
Hair JF. In: Multivariate data analysis: A global perspective. 7th ed. Prentice Hall; 2009. pp. 637.
-
-
Chung C, Kim MJ, Rhee MH, Do HG. Functional status and psychosocial adjustment in gynecologic cancer patients receiving chemotherapy. Korean Journal of Women Health Nursing 2005;11(1):58–66. [doi: 10.4069/kjwhn.2005.11.1.58]
-
-
Cha K, Kim K. Impact of uncertainty on resilience in cancer patients. Asian Oncology Nursing 2012;12(2):139–146. [doi: 10.5388/aon.2012.12.2.139]
-
-
Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine 1991;32(6):705–714. [doi: 10.1016/0277-9536(91)90150-b]
-
-
Lim MK, Kim MH, Shin YJ, Yoo WS, Yang BM. Social support and self-rated health status in a low income neighborhood of Seoul, Korea. Korean Journal of Preventive Medicine 2003;36(1):54–62.
-
-
Woringer M, Nielsen JJ, Zibarras L, Evason J, Kassianos AP, Harris M, et al. Development of a questionnaire to evaluate patients’ awareness of cardiovascular disease risk in England’s National Health Service Health Check preventive cardiovascular programme. BMJ Open 2017;7(9):e014413 [doi: 10.1136/bmjopen-2016-014413]
-
-
Kline RB. In: Principles and practice of structural equation modeling. 3rd ed. Guilford Press; 2011. pp. 60-214.
-
-
Becker TE. Potential problems in the statistical control of variables in organizational research: A qualitative analysis with recommendations. Organizational Research Methods 2005;8(3):274–289. [doi: 10.1177/1094428105278021]
-
-
Karataş T, Polat Ü. Effect of nurse-led program on the exercise behavior of coronary artery patients: Pender’s Health Promotion Model. Patient Education and Counseling 2021;104(5):1183–1192. [doi: 10.1016/j.pec.2020.10.003]
-
-
Komasi S, Saeidi M. A perceived risk factor may lead to increased anxiety and depression in cardiovascular patients. Jundishapur Journal of Chronic Disease Care 2016;5(4):e34159 [doi: 10.17795/jjcdc-34159]
-
-
Kim SY, Kim MY. Development and effectiveness of tailored education and counseling program for patients with coronary artery disease undergoing percutaneous coronary intervention. Korean Journal of Adult Nursing 2017;29(5):547–559. [doi: 10.7475/kjan.2017.29.5.547]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

