Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(2); 2024 > Article
- Research Paper Examination of Predicting Factors for COVID-19 Vaccination Behaviors of University Students Utilizing the Theory of Planned Behavior
- Yeon Jeong Heo, Hye-Jin Hyun
-
Journal of Korean Academy of Nursing 2024;54(2):178-192.
DOI: https://doi.org/10.4040/jkan.24020
Published online: May 31, 2024
-
Corresponding author:
Hye-Jin Hyun,
Email: hjhyun@kangwon.ac.kr
- 1,465 Views
- 41 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
This study aimed to examine the predictive factors of COVID-19 vaccination behavior by evaluating the moderating effect of perceived behavioral control on the theory of planned behavior.
Methods
Data were collected from August 6 to August 31, 2022 from 235 college students (aged 20~29 years) across 12 universities using a structured web-based survey. Statistical analyses were conducted using the SPSS and AMOS software.
Results
Attitudes toward COVID-19 vaccination, subjective norms, and intention to be vaccinated significantly influenced COVID-19 vaccination behavior. Attitudes and subjective norms indirectly affected COVID-19 vaccination behavior through intention to vaccinate, whereas intention to vaccinate had a direct effect. The moderating effect of perceived behavioral control on the relationship between subjective norms and intention to vaccinate was significant.
Conclusion
Interventions that foster a positive attitude toward COVID-19 vaccination and bolster subjective norms and perceived behavioral control can boost the intention to be vaccinated and facilitate the uptake of COVID-19 vaccination.
Published online May 31, 2024.
https://doi.org/10.4040/jkan.24020
Examination of Predicting Factors for COVID-19 Vaccination Behaviors of University Students Utilizing the Theory of Planned Behavior
Abstract
Purpose
This study aimed to examine the predictive factors of COVID-19 vaccination behavior by evaluating the moderating effect of perceived behavioral control on the theory of planned behavior.
Methods
Data were collected from August 6 to August 31, 2022 from 235 college students (aged 20~29 years) across 12 universities using a structured web-based survey. Statistical analyses were conducted using the SPSS and AMOS software.
Results
Attitudes toward COVID-19 vaccination, subjective norms, and intention to be vaccinated significantly influenced COVID-19 vaccination behavior. Attitudes and subjective norms indirectly affected COVID-19 vaccination behavior through intention to vaccinate, whereas intention to vaccinate had a direct effect. The moderating effect of perceived behavioral control on the relationship between subjective norms and intention to vaccinate was significant.
Conclusion
Interventions that foster a positive attitude toward COVID-19 vaccination and bolster subjective norms and perceived behavioral control can boost the intention to be vaccinated and facilitate the uptake of COVID-19 vaccination.
INTRODUCTION
Vaccines play a pivotal role in preventing and ameliorating infectious diseases [1]. The global spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of coronavirus disease 2019 (COVID-19), has led to the emergence of new variants with increased transmissibility and pathogenicity, emphasizing the importance of acquiring herd immunity through vaccination [2]. Despite the availability of vaccines in over 90% of countries since 2014, vaccine hesitancy has steadily increased, influenced by factors such as trustworthiness, convenience, and contextual influences [3]. Studies have demonstrated that COVID-19 vaccine hesitancy is associated with cultural factors, attitudes, motivations, and social norms. Therefore, understanding various factors influencing individuals’ intentions and behaviors regarding COVID-19 vaccination is imperative [4].
The theory of planned behavior (TPB), introduced by Ajzen [5] in 1991, provides a conceptual framework for understanding the complexity of human social behavior and predicting context-specific behaviors. TPB posits that intentions directly influence behavior through attitudes, subjective norms, and perceived behavioral control factors, collectively determining behavior, with intentions as the direct determinants.
The TPB serves as a theoretical foundation for understanding individuals’ underlying motivations for vaccination and aids in identifying specific aspects of individual differences that induce intentional behavior [5]. Previous studies investigating COVID-19 vaccination intentions have reported a positive association of attitude, perceived behavioral control (PBC) toward the COVID-19 vaccination behavior, and subjective norms with the intention to receive vaccination [6, 7, 8]. However, in the TPB, PBC toward the COVID-19 vaccination behavior is not conceptualized as a direct determinant of intention [9], and recent studies have explored its regulatory effects in interaction with attitudes and subjective norms [10, 11, 12].
Previous studies applying TPB to various health behaviors have shown inconsistent measurement of PBC toward the COVID-19 vaccination behavior as a moderating variable affecting the influence of attitudes and subjective norms on intention or as a determinant of intention [13, 14, 15, 16, 17, 18, 19]. There is a paucity of studies exploring the moderating effects of PBC toward the COVID-19 vaccination behavior in the context of COVID-19 vaccination intentions using the TPB [6, 7, 8, 20] and other vaccination intentions [21, 22].
Studies by Wolff [7] and Yahaghi et al. [8] applying TPB to COVID-19 vaccination behavior suggested lower predictive validity of PBC toward the COVID-19 vaccination behavior compared to attitudes and subjective norms. Additionally, Seddig et al. [6] found no significant influence of PBC toward the COVID-19 vaccination behavior on COVID-19 vaccination intentions. These findings highlight the need for further research applying PBC toward the COVID-19 vaccination behavior as a moderating variable rather than a direct determinant of intention when predicting future COVID-19 vaccination intentions [10, 23].
According to the Disease Management Agency of the Ministry of Health and Welfare (MOHW), the proportion of individuals in the 20~29 years age group who received the third dose of the COVID-19 vaccine (approximately 50%) is much lower than that in other age groups [24]. The incidence of COVID-19 is also higher in this age group which primarily consists of university students engaged in communal living arrangements, posing a potential risk for virus transmission [25]. Therefore, this study aimed to examine the predicting factors for COVID-19 vaccination behaviors among university students by evaluating the moderating effect of PBC toward the COVID-19 vaccination behavior of the TPB.
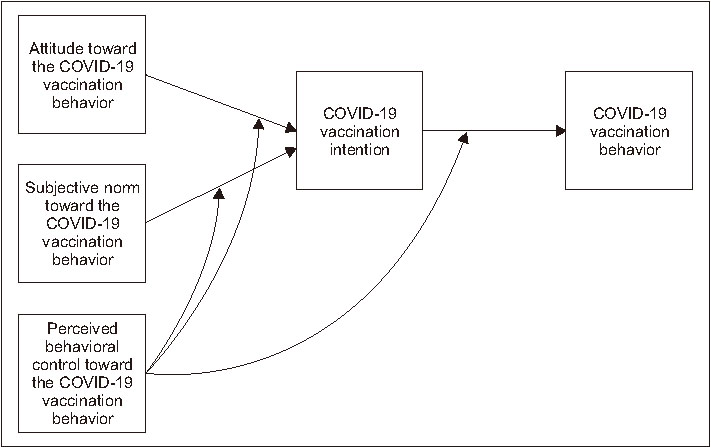
This study derived the following hypotheses from the TPB (Figure 1):
Figure 1
Conceptual framework of this study.
1) Hypothesis 1: Attitude toward the COVID-19 vaccination behavior influences the intention to receive COVID-19 vaccination.
2) Hypothesis 2: Subjective norm toward COVID-19 vaccination behavior influences the COVID-19 vaccination intention.
3) Hypothesis 3: PBC toward the COVID-19 vaccination behavior toward the COVID-19 vaccination behavior moderates the impact of attitude toward the COVID-19 vaccination behavior on the COVID-19 vaccination intention.
4) Hypothesis 4: PBC toward the COVID-19 vaccination behavior toward the COVID-19 vaccination behavior moderates the impact of subjective norm toward the COVID-19 vaccination behavior on the COVID-19 vaccination intention.
5) Hypothesis 5: PBC toward the COVID-19 vaccination behavior toward the COVID-19 vaccination behavior moderates the impact of the COVID-19 vaccination intention on the COVID-19 vaccination behavior.
6) Hypothesis 6: The COVID-19 vaccination intention influences the COVID-19 vaccination behavior.
METHODS
1. Study design
This study is an attempt at theoretical validation through the application of the TPB [10] with the inclusion of the moderating effect of PBC toward the COVID-19 vaccination behavior. This was a theory-validation study aimed at finding factors influencing COVID-19 vaccination behavior, integrating PBC toward the COVID-19 vaccination behavior as a moderating variable into the TPB, and assessing its utility in explaining specific behaviors such as COVID-19 vaccination behavior in particular situations.
2. Setting and study participants
In pursuit of study objectives, participants were chosen based on COVID-19 vaccination status using MOHW data [24]. As of May 31, 2022, the percentage of individuals in various age groups who had received the third dose of COVID-19 vaccine were as follows: 20~29 years (59.3%); 30~39 years (58.5%); 40~49 years (67.5%); 50~59 years (81.9%); 60~69 years (90.1%); 70~79 years (92.0%); and ≥ 80 years (84.9%) [24]. The study focused on adults aged 20~29 years, constituting a group with an approximately 50% rate of receiving the 3rd dose of COVID-19 vaccine, mainly comprising university students. This study covered four regions in Seoul, South Korea: Gyeonggi-do, Chungcheong-do, Gyeongsang-do, and Busan. Seoul, the capital, is a hub for politics, economy, and culture. Gyeonggi-do is neighboring Seoul. It has the highest population density in the metropolitan area. Chungcheong-do is in central South Korea. It mainly has agriculture and small to medium-sized businesses. Gyeongsang-do is in the southeast of South Korea. It is recognized for its developed agriculture and fisheries. Busan Metropolitan City is a significant coastal city that thrives on shipping, trade, and fishing industries. The target population comprised university students aged 20 to 29 years who were actively enrolled in 12 universities across Seoul (The University of Seoul, Kyung Hee University, Chung-Ang University), Gyeonggi province (Kyonggi University, Dankook University, Gachon University), Chungcheong province (Chungbuk National University, Cheongju National University, Semyung University), and Gyeongsang province (Kyungnam University, Changwon National University, Pusan National University).
University students aged 20~29 years who had received the third dose voluntarily, those who did not receive the third dose, and those who were unvaccinated were eligible for inclusion. Students who had received the fourth dose, those in the medical field (nursing and medical students), those on leave, and those resuming studies after a gap were not eligible for inclusion. Approval was secured from each department, and the survey URL was posted on department boards. Access to the online survey was provided from August 1 to August 31, 2022.
For structural equation modeling, 5~20 participants per variable are recommended, with a minimum sample size of 200 for robust conclusions [26]. Factoring a dropout rate of 20%, ≥ 250 participants were targeted. A total of 280 individuals accessed the URL during the study period. Of these, only 253 (90%) responded. After excluding 18 participants due to unreliable answers, data from 235 individuals were included in the analysis.
3. Measurements/instruments
1) Demographic characteristics
Demographic characteristics were assessed in a total of 8 items: gender, age, grade, major, university location, residence type, religion, and income. These variables align with the individual and social background factors outlined in Ajzen’s [27] TPB and were examined in relation the COVID-19 vaccination intention, drawing insights from previous studies [6, 7, 8, 20].
2) Attitude toward the COVID-19 vaccination behavior
This study utilized a tool modified by Hu [28] to assess attitudes toward COVID-19 vaccination behavior. The tool, based on Ajzen’s [29] questionnaire development method and adapted by Lee [30] for COVID-19 vaccination, employed an 8-paired adjective scale using a 7-point Likert scale, structured as a semantic differential scale. Respondents expressed their positive or negative thoughts regarding COVID-19 vaccination behavior through eight pairs of adjectives, such as Good-Bad and Pleasant-Unpleasant. The scale consisted of eight items, with higher scores indicating a more positive attitude. The instrument demonstrated high internal consistency in this study (Cronbach’s α = .94). Previous studies by Lee [30] and Hu [28] reported Cronbach’s α scores of .98 and .97 for attitudes toward AstraZeneca and Pfizer vaccines, respectively.
3) Subjective norm toward COVID-19 vaccination behavior
In this study, subjective norms toward COVID-19 vaccination behavior was assessed using a tool modified by Hu [28], based on Ajzen’s [5] instrument and adapted by Park et al. [31] and Park & Han [32], with approval from the original author. The tool consisted of six items each of which was rated using a 7-point scale, ranging from ‘Strongly Disagree’ (1 point) to ‘Strongly Agree’ (7 points). Higher scores indicate stronger societal pressure related to COVID-19 vaccination behavior. The instrument showed a high internal consistency in this study (Cronbach’s α = .92). A previous study by Park et al. [31] reported a Cronbach’s α of .80, while Park & Han [32] reported a Cronbach’s α of .74. In the study of Hu [28], the tool showed good reliability in assessing attitudes toward the AstraZeneca vaccine (Cronbach’s α = .98) and Pfizer vaccine (Cronbach’s α = .97).
4) Perceived behavioral control toward the COVID-19 vaccination behavior
In this study, PBC toward the COVID-19 vaccination behavior related to COVID-19 vaccination behavior was assessed using an instrument developed by Kim & Yeom [33] for measuring PBC in the context of influenza vaccination, following Ajzen’s [34, 35] suggested measurement method. The researcher adapted the tool, approved by the original author, to align with the specific objectives of the study. The content validity of the instrument was ensured through comparison with existing items by a nursing professor, and the appropriateness for the general adult population was verified. The preliminary item set was reviewed by six experts (two nursing professors and four infection control specialist nurses) for content appropriateness and refinement. Tool development employed the content validity index (CVI), and items with a CVI of .80 or above were considered as having content validity. The PBC construct comprised four items rated on a 7-point scale, ranging from ‘Strongly Disagree’ (1 point) to ‘Strongly Agree’ (7 points), with higher scores indicating a greater perceived level of behavioral control regarding COVID-19 vaccination. In Kim & Yeom’s [33] study, Cronbach’s α of the instrument was .76, while in the present study, Cronbach’s α of PBC was .76, indicating satisfactory internal consistency.
5) COVID-19 vaccination intention
In this study, COVID-19 vaccination intention was assessed based on the instrument developed by Ajzen [5]. The survey items were adapted from Park & Han [32], Lee & Kim [36], and Hwang & Cha [37], with modifications by Hu [28] to suit the context of COVID-19 vaccination. The tool, approved for use by the original author, comprises five items measured on a 7-point scale, ranging from ‘Strongly Disagree’ (1 point) to ‘Strongly Agree’ (7 points). Higher scores indicate a stronger intention to undergo COVID-19 vaccination. The reliability of the intentions for COVID-19 vaccination construct was assessed with Cronbach’s α, yielding satisfactory results. The reliability coefficients reported in previous studies include Park & Han [32] with Cronbach’s α = .92, Lee & Kim [36] with Cronbach’s α = .87, Hwang & Cha [37] with Cronbach’s α = .90, AstraZeneca vaccine intentions with Cronbach’s α = .97, and Pfizer vaccine intentions with Cronbach’s α = .96. Cronbach’s α in the current study was .95.
6) COVID-19 vaccination behavior
According to the Korea Disease Control and Prevention Agency (KDCA), the recommended number of vaccination doses and dosing intervals are as follows: Comirnaty/Pfizer and BioNTech - 2 doses (8 weeks apart), Spikevax/Moderna - 2 doses (8 weeks apart), Vaxzevria/AstraZeneca - 2 doses (8~12 weeks apart), Novavax Pre-Filled Syringe (Novavax) - 2 doses (3 weeks apart), and COVID-19 Vaccine Janssen/Janssen - 1 dose [38]. A third dose is recommended 3 months after the second dose, except for the COVID-19 Vaccine Janssen, for which a 2-month interval is recommended after the single dose [38].
In this study, COVID-19 vaccination behavior refers to adherence to the vaccination doses and intervals recommended by the KDCA, based on the specific COVID-19 vaccine type. Behavior was assessed by assigning points: 1 for the first dose, 2 for the second dose, and 3 for the third dose. Unvaccinated participants were awarded 0 points. For individuals receiving the COVID-19 Vaccine Janssen, completing the primary vaccination (1st and 2nd doses) counted as 2 doses, and an additional vaccine for the third dose was scored as 3 points. Higher scores indicate better adherence to COVID-19 vaccination.
4. Data collection
In this study, data were collected from August 6, 2022 to August 31, 2022. Following a detailed explanation of the study’s purpose and methods, approvals were obtained from each department, and recruitment notices were posted on the respective university department bulletin boards to solicit voluntary participation in the research. This study used an existing Internet platform to create survey questions and deliver the survey. The survey was conducted as an anonymous questionnaire study, where potential participants accessed a weblink to read the research description and consent form. The time required to complete the questionnaire was approximately 10~15 minutes, and to ensure the confidentiality of the collected data, a password was set during data storage, emphasizing that all information would be kept confidential. As a token of appreciation for participation, online gift vouchers were provided.
5. Data analysis
Data analyses were performed using the statistical software SPSS Statistics 25 and AMOS 25 (IBM Co.). The specific analysis methods are outlined as follows:
(1) Descriptive statistics, such as mean (standard deviation) and frequency (percentages) were computed for general demographical characteristics and measurement variables.
(2) The reliability of the measurement tools was assessed by computing Cronbach’s α.
(3) Normality of the sample was evaluated using the standardized values of skewness and kurtosis (critical ratio).
(4) Variance inflation factor (VIF) was employed to examine multicollinearity among measurement variables.
(5) Pearson correlation coefficients were used to analyze the relationships between measurement variables.
(6) Confirmatory factor analysis was conducted to evaluate the validity of latent variables in the research model.
(7) Model validation utilized the maximum likelihood method assuming multivariate normality.
(8) Model fit indices, including χ2 (chi-square), χ2/df, root mean squared residual (RMR), root mean square error of approximation (RMSEA), goodness of fit index (GFI), and adjusted goodness of fit index (AGFI), were calculated. Incremental fit measures included normed fit index (NFI), Tucker-Lewis index (TLI), and comparative fit index (CFI).
(9) Bootstrapping was employed to test the statistical significance of indirect and total effects in the model.
(10) Multigroup analysis, using measurement invariance testing through a chi-square difference test, was performed to examine the moderating effect of PBC. To address potential issues associated with hierarchical regression analysis, such as increased error due to interaction terms and potential underestimation of interaction effects [39], multigroup analysis was applied to verify the moderating effects [40].
6. Ethical considerations
This study was approved by the Kangwon National University’s Institutional Review Board (IRB approval number: KWNUIRB-2022-06-004-003). On accessing the survey URL, all participants were required to review the informed consent form and voluntarily opt to participate in the survey. The participants were made aware that there were no adverse repercussions of non-participation. Participants were also informed of their right to withdraw at any time and that their data would be discarded upon withdrawal. The online interface allowed the participants to proceed with the survey only after they had agreed to these terms. The study objectives, participation details, procedures, potential risks and benefits, compensation, voluntary participation, withdrawal, and privacy protection were outlined on the survey site.
Data pertaining to personal information included gender, age, academic year, major, university location, residence type, religion, income, and phone number. Phone numbers were solely used to send a ₩5,000 mobile gift voucher to participants who completed the survey and opted for compensation. Strict confidentiality measures were applied to handle personal information, ensuring anonymity by utilizing clinical data only as needed and not directly incorporating personal details into the research. Personal information and research data were anonymized before analysis to preserve confidentiality.
RESULTS
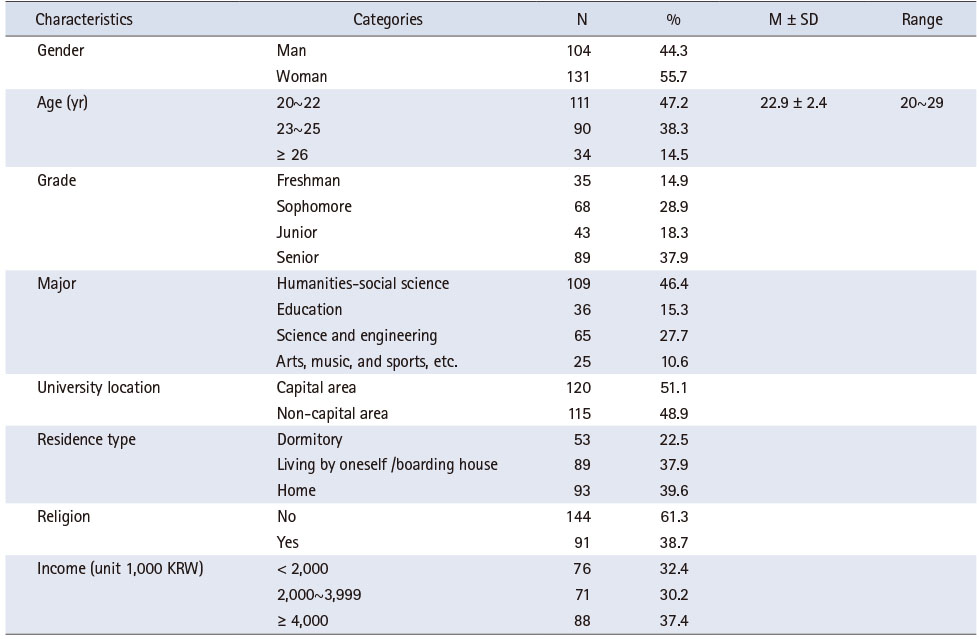
1. General characteristics of the study participants
The study participants comprised 235 students (104 man [44.3%] and 131 woman [55.7%]. The average age was 22.9 ± 2.4 years, with 111 participants (47.2%) aged between 20 and 22 years, 90 participants (38.3%) aged between 23 and 25 years, and 34 participants (14.5%) aged ≥ 26 years. The other general characteristics are summarized in Table 1.
Table 1
General Characteristics of the Study Participants (N = 235)
2. Measurement variables
Descriptive statistical analyses were conducted to examine the distribution of scores for attitudes toward COVID-19 vaccination behavior, subjective norms, PBC, intention for COVID-19 vaccination, and actual vaccination behavior. The normality of distribution of scores was assessed by calculating skewness and kurtosis (Supplementary Table 1). Attitudes toward COVID-19 vaccination behavior, subjective norms, PBC, and intention for COVID-19 vaccination were measured using a 7-point scale, with higher scores indicating more positive attitudes. The scores for the variables were as follows: attitudes toward COVID-19 vaccination behavior 4.62 ± 1.26 points; subjective norms 4.88 ± 1.40 points; PBC 4.50 ± 1.33 points; intention for COVID-19 vaccination 4.41 ± 1.60 points; and COVID-19 vaccination behavior 2.46 ± 0.59 points. Skewness ranged from -0.85 to -0.07, indicating values near ‘0’. Kurtosis ranged from -0.82 to 1.06, all presenting values near ‘0’, suggesting that the score distributions of the variables could be assumed to follow a normal distribution skewness and kurtosis (Supplementary Table 1).
3. Multicollinearity assessment
To assess the presence of multicollinearity among attitudes, subjective norms, and vaccination intentions input into the model, tolerance and VIF were calculated (Supplementary Table 1). The tolerance ranged from .45 to .68, which was above .10, and the VIF ranged from 1.46 to 2.21, all below 10. Thus, there was no evidence of multicollinearity among the variables tolerance and VIF were calculated (Supplementary Table 1).
4. Correlations among key variables
The relationship among attitudes toward COVID-19 vaccination, subjective norms, PBC, intention for COVID-19 vaccination, and actual vaccination behavior, were assessed by calculating Pearson correlation coefficients. The correlation analysis revealed significant positive correlations (r = .17~.70) among the variables.
5. Hypothesis testing
1) Confirmatory factor analysis
CFA was conducted to assess the appropriateness of the items used to assess attitude, norms, PBC, and intention (Supplementary Table 1). The construct reliability (CR) value, typically considered meaningful if above .70 and acceptable if between .60 and .70 [41], was examined. Additionally, the average variance extracted (AVE) value, generally deemed meaningful if above .50, could be acceptable if slightly below .50 when the CR value is above .60 [41]. The results of the CFA revealed standardized coefficient values above .50. The CR value was above .70, and the AVE values for the attitude, subjective norm, and intention variables were above .50, indicating good CR. However, the AVE for PBC was .48, slightly below .50 (Supplementary Table 1). However, the CR value was high at .70, indicating acceptable reliability and suggesting no issues with measurement [41].
2) Evaluation of model fit
The assessment of model fit, conducted using the maximum likelihood method under the assumption of normality of distribution of observed variables, yielded the following outcomes. The results of the model fit evaluation indicated a satisfactory chi-square value (χ2 = .94, p = .625). Absolute fit indices, including RMR (.01), RMSEA (.00), GFI (1.00), and AGFI (.99), met the criteria for a well-fitting model. Incremental fit indices, such as NFI (1.00), TLI (1.00), and CFI (1.00), also demonstrated a good fit. This implies that the model exhibits a robust fit, and its evaluation is considered reliable [26].
3) Path analysis
We verified the significance of the paths influencing COVID-19 vaccination behavior, a variable in the TPB. The results showed that the intention for COVID-19 vaccination was significantly influenced by the attitude toward COVID-19 vaccination (β = .52, p < .001) and subjective norms (β = .44, p < .001), with these variables explaining 54.8% of the variance. Furthermore, COVID-19 vaccination behavior was significantly influenced by the intention for vaccination (β = .41, p < .001), which explained 17.0% of the variance (Supplementary Table 2).
4) Effect analysis
For effect analysis in this study, bootstrapping was conducted with 200 bootstrap samples. Direct effects, indirect effects, and total effects of variables significantly influencing each path were examined. Variables significantly influencing COVID-19 vaccination behavior were attitude toward COVID-19 vaccination (β = .18, p = .005), subjective norm (β = .22, p = .010), and intention for COVID-19 vaccination (β = .41, p < .001). Attitude toward COVID-19 vaccination indirectly influenced COVID-19 vaccination behavior through the mediation of intention for COVID-19 vaccination. Subjective norms for COVID-19 vaccination indirectly influenced COVID-19 vaccination behavior through the mediation of intention for COVID-19 vaccination. Intention for COVID-19 vaccination had a direct impact on COVID-19 vaccination behavior (Supplementary Table 2).
5) Moderation analysis
(1) Measurement invariance test
To examine the moderating effect of PBC on COVID-19 vaccination behavior, a multiple-group path analysis was conducted, classifying participants into low and high groups based on the median score of PBC for COVID-19 vaccination. Those below the median of 4.25 were classified as the low group, and those above 4.25 were classified as the high group. Measurement invariance testing, a prerequisite for testing moderation effects, ensures that each group, the analysis target (moderator variable), perceives the measurement tool (survey items) similarly. This is determined by comparing the χ2 values of the unconstrained model and the measurement weights-constrained model, with a decrease in χ2 (Δχ2) indicating measurement invariance. The unconstrained model yielded χ2 = 2.63 with degree of freedom (df) = 4, while the measurement weights-constrained model yielded χ2 = 10.16 with df = 7. The Δχ2 increased by 7.52 with a Δdf of 3. For a significance level of 0.05 and df = 3, the critical χ2 value is 7.82 [42]. The observed Δχ2 value of 7.52 fell below the critical value, indicating no statistically significant difference between the two groups. Thus, measurement invariance was established.
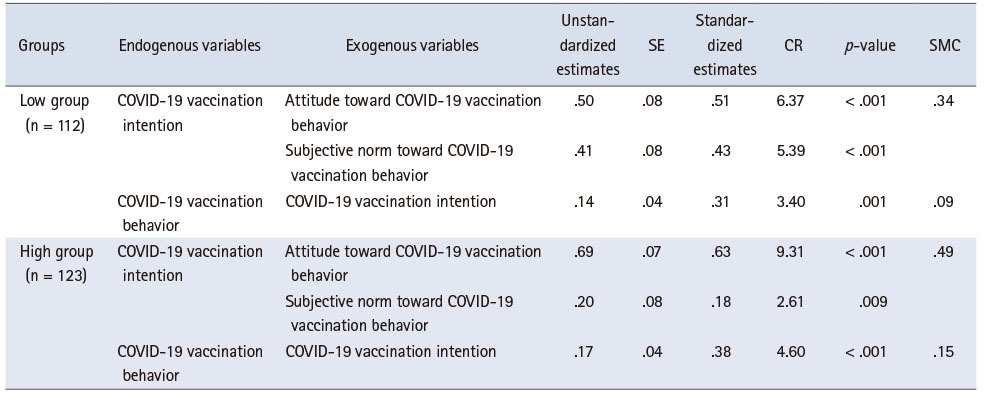
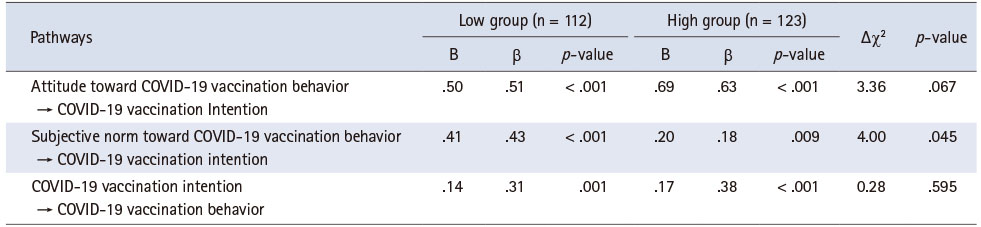
(2) Path coefficients for PBC toward the COVID-19 vaccination behavior on COVID-19 vaccination behavior across different groups
The path coefficients for groups with low and high levels of PBC on COVID-19 vaccination behavior were as follows. In the group with low PBC, the intention for COVID-19 vaccination was significantly influenced by the attitude (β = .51, p < .001) and subjective norms (β = .43, p < .001) toward COVID-19 vaccination, with these variables explaining 33.7% of the variance. COVID-19 vaccination behavior was significantly influenced by the intention (β = .31, p = .001), explaining 9.4% of the variance. In the group with high PBC, the intention for COVID-19 vaccination was significantly influenced by the attitude (β = .63, p < .001) and subjective norms (β = .18, p = .009) toward COVID-19 vaccination, with these variables explaining 48.6% of the variance. COVID-19 vaccination behavior was significantly influenced by the intention (β = .38, p < .001), explaining 14.8% of the variance (Table 2).
Table 2
Pathways in Groups with Low and High Perceived Behavioral Control toward the COVID-19 Vaccination Behavior (N = 235)
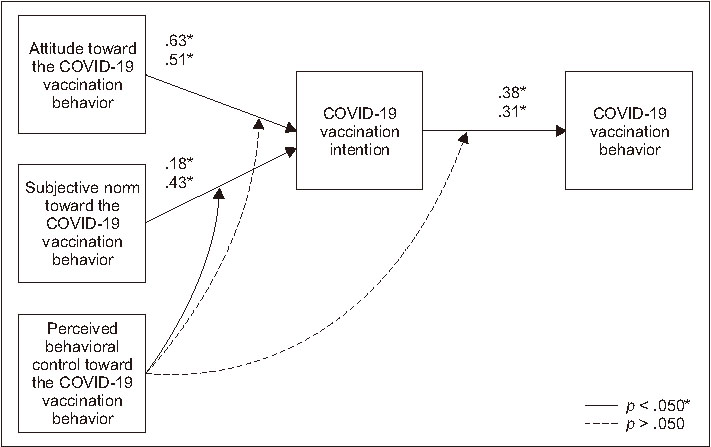
(3) Testing moderating effect of PBC toward the COVID-19 vaccination behavior on COVID-19 vaccination behavior
The results of testing the moderating effect of PBC on COVID-19 vaccination behavior revealed a significant difference in the path from subjective norms for COVID-19 vaccination behavior to the intention for COVID-19 vaccination between the group with high PBC and the group with low PBC (χ2 = 4.00, p = .045). In other words, the moderating effect of PBC on the relationship between subjective norms for COVID-19 vaccination behavior and the intention for COVID-19 vaccination was found to be significant (Figure 2) (Table 3).
Figure 2
Moderating effects of perceived behavioral control in the theory of planned behavior.
Table 3
Verification of the Moderating Effect of Perceived Behavioral Control (N = 235)
DISCUSSION
This study aimed to examine whether the TPB [10], augmented with the moderating effect of PBC, is a useful framework for explaining COVID-19 vaccination behavior in specific situations, such as the COVID-19 pandemic. By applying Ajzen’s [10] TPB with PBC as a moderator, we aimed to validate its applicability to COVID-19 vaccination behavior, identify factors influencing such behavior, and elucidate the moderating effect of PBC on COVID-19 vaccination behavior.
In this study, COVID-19 vaccination intentions were significantly influenced by attitudes (β = .52, p < .001) and subjective norms (β = .44, p < .001) toward COVID-19 vaccination behavior, explaining 54.8% of the variance. Additionally, COVID-19 vaccination behavior was significantly influenced by vaccination intentions (β = .41, p < .001), explaining 17.0% of the variance. According to the TPB [5], stronger intentions to engage in specific behavior are associated with more favorable attitudes, subjective norms, and PBC. Positive attitudes and supportive subjective norms are assumed to motivate individuals to perform actions, shaping their intentions and ultimately influencing behavior [43].
The study results support the TPB, highlighting that changes in attitudes and subjective norms lead to changes in intentions, directly influencing behavior. This aligns with previous research validating the applicability of the TPB in explaining various health behaviors, such as breastfeeding [13], contraceptive use [16], helmet use [17], breast self-examination [18], smoking cessation [14], reproductive health promotion [19], and safe sexual practices [15]. These findings underscore the importance of applying the TPB as a strategic framework to enhance vaccination behavior, particularly in the context of the COVID-19 pandemic.
According to the TPB [10], PBC regulates attitudes toward intentions. However, this study found no significant moderating effect of PBC on the relationship between attitudes toward COVID-19 vaccination and the intention for COVID-19 vaccination. Similar to our findings, a study by Seddig et al. [6] also identified attitudes as the sole direct predictor of the intention for COVID-19 vaccination, with no observed interaction between attitudes and PBC. These results suggest that individual beliefs about the positive or negative outcomes of vaccination significantly influence the intention to receive or refuse vaccination [6].
While the moderating effects of PBC between attitudes and intentions were not significant in both the present study and the study by Seddig et al. [6] on COVID-19 vaccination, significant interactions between attitudes and intentions have been observed in previous studies related to smoking cessation intentions [44] and the intention of women to receive the human papillomavirus vaccine [11]. The differences in the moderating effect of PBC on intentions between COVID-19 vaccination and other health behaviors are likely attributable to a lack of trust in COVID-19 vaccines.
In the context of the COVID-19 pandemic, a lack of trust in the safety and efficacy of COVID-19 vaccines led to the formation of negative attitudes towards vaccination, leading to hesitancy. Conversely, the belief that COVID-19 vaccination protects against severe illness, death, and adverse long-term health-related outcomes reinforces the positive attitudes and increases the intention for vaccination. Recent studies have indicated a positive correlation between anxiety about COVID-19, fear of infection, and positive attitudes and intentions towards COVID-19 vaccination [45].
A meta-analysis by Hagger et al. [46] found no moderating effect of PBC on the relationship between attitudes and intentions across various health behaviors, including health protection and risk behaviors, physical activity, and dietary behaviors. However, there is a paucity of research exploring the moderating effect of PBC on the relationship between attitudes and intentions within the context of the TPB. Future studies should investigate the role of PBC as a moderating variable in the relationship between attitudes and intentions across diverse health behaviors.
This study revealed a significant moderating influence of PBC on the relationship between subjective norms related to COVID-19 vaccination behavior and intention to vaccinate. Specifically, in groups with lower PBC, subjective norms had a greater impact on the intention to vaccinate against COVID-19 compared to groups with higher PBC. This suggests that as the perceived difficulty or inconvenience of getting vaccinated for COVID-19 increases, individuals become more influenced by the opinions of groups important to them.
Similar to the results of this study, the moderating effect of PBC on the relationship between subjective norms and intentions in the study by La Barbera & Ajzen [47] had a negative sign, indicating that when individuals have high PBC, normative. This suggests a possibility of being less affected. In another study, Castanier et al. [12] found that the more control people felt over performing a behavior, the less likely their behavior, such as drunk driving or disobeying road signs, was influenced by peer pressure. We found a significant negative interaction between subjective norms and PBC, indicating that the subjective norm’s prediction of intention was weaker in conditions of high PBC than in low [12]. However, in a study by Seddig et al. [6], no interaction between subjective norms and perceived behavioral control was found, which was different from the results of this study.
The difference in these findings is that, in the study by La Barbera & Ajzen [47], voting for European integration, reducing household food waste, and reducing energy consumption were actions that the individuals intended to perform, whereas citizens’ votes in support of greater European integration were actions that the individuals intended to perform. Getting through and achieving the goals of reducing food waste and reducing energy consumption will depend on the actions of others. In contrast, a study by Yzer & van den Putte [48] found that the relative importance of subjective norms increased the intention to quit smoking as a function of the amount of PBC, meaning that this was not a characteristic of individualistic behavior. A significant moderating effect of PBC in the relationship between subjective norms and intention may be the difference between collectivistic and individualistic behavior [47]. This study found that the group with low PBC during the COVID-19 pandemic situation was more influenced by subjective norms in their COVID-19 vaccination intention. Feeling less in control means being more influenced by people around you to get vaccinated against COVID-19. COVID-19 vaccination behavior is not an obligation but an optional behavior. However, if people around you, such as friends and colleagues, have been vaccinated against COVID-19, you may feel unspoken pressure to get vaccinated. Felt. COVID-19 vaccination may reflect an individual’s health-related behavior. However, it may also be a collectivist behavior influenced by social pressure to prevent others from getting infected, so it is thought to be different from previous studies.
A meta-analysis by Hagger et al. [46] suggested that PBC does not consistently moderate the relationship between subjective norms and intentions. Our study indicates that when PBC is low, subjective norms have a stronger impact on intention. This underscores the importance of considering the moderating role of PBC on the influence of subjective norms on intention in future research, emphasizing that PBC may not directly affect intention but moderates the impact of subjective norms on intention.
In this study, the moderating effect of PBC on the relationship between COVID-19 vaccination intention and vaccination behavior was not significant, which is consistent with the findings of Seddig et al. [6]. Seddig et al. [6] suggested that explicit instructions to assume quick access to a COVID-19 vaccination appointment might have led participants to overlook the perceived barriers, potentially diminishing the impact of PBC. Several studies within the TPB framework have also found no significant interaction effects of PBC on intention [44].
Contrary to our findings, the meta-analysis by Hagger et al. [46] suggested that the moderating effect of PBC on the relationship between intention and behavior is stronger when the PBC is high. Previous studies on different behaviors, such as weight loss and marijuana use, demonstrated significant moderating effects of PBC [49]. However, less than 30% of studies included in a meta-analysis by Armitage & Conner [50] investigated the moderating role of PBC, showing a lack of clear consensus.
Challenges in testing interactions include issues related to statistical power, distribution of predictor and moderator variables, and floor/ceiling effects in the data collected [48]. There is a paucity of empirical evidence supporting the moderating effects of PBC, which is attributed to methodological challenges and the need for sufficient variance in the measured variables [47]. The study suggests that incorporating PBC in the TPB may help enhance the theoretical explanation of behavior formation and change. Future research should explore variables elucidating the role of the moderating effects of PBC with studies verifying its impact on behavior formation.
This study was significant in that it validated the TPB by integrating PBC as a moderating variable in predicting COVID-19 vaccination behavior. Utilizing the TPB, a widely applicable theory in explaining health behavior, the research predicted COVID-19 vaccination behavior and confirmed the moderating effect of PBC in the relationship between subjective norms and intentions. The confirmation of the moderating effect may help advance the explanatory power of the TPB for behavior formation and change in specific circumstances, such as the COVID-19 pandemic. To enhance external validity, future research should include diverse study populations. While TPB theorists propose that PBC mitigates the influences on intentions, there is a paucity of empirical evidence. This confirmation may help advance the TPB’s explanatory framework for behavior formation and change. The results of this study make an important contribution to the theory by providing a basis for the key predictions of planned behavior, whose moderating effects have not been tested across multiple studies. In the future, a vaccination program should be developed and applied based on the direct and controlling factors affecting COVID-19 vaccination behavior identified in this study.
Some limitations of this study should be considered. Firstly, this study categorized the COVID-19 pandemic into three phases based on significant events in South Korea. This might have introduced potential variations in research outcomes depending on the temporal context of the ongoing third wave. Secondly, measuring both intention and behavior of COVID-19 vaccination concurrently might have introduced a bias. However, we took precautions in formulating questions to minimize bias and enhance mediation effects. Thirdly, the study’s participants were university students from specific regions, potentially limiting the generalizability of our findings to the broader population of 20 to 29-year-old adults. The convenience sampling methodology might have also introduced an element of bias. Fourthly, this study relied on self-reported measurements for COVID-19 vaccination behavior. This might have introduced measurement errors due to socially desirable responses and positive biases.
CONCLUSION
The study provides foundational evidence supporting the role of PBC in TPB, emphasizing its impact in groups with lower perceived behavioral control. Future research should focus on developing targeted vaccination programs based on identified factors and explore the moderating effects of perceived behavioral control in diverse health behaviors, populations, and contexts. Future studies should include a more diverse sample and use more reliable measurement tools to enhance generalizability and minimize measurement errors.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online at https://doi.org/10.4040/jkan.24020.
Descriptive Statistics, Variance Inflation Factor among the Observed Variables, and Confirmatory Factor Analysis (N = 235)Supplementary Table 1
Pathways Influencing Behaviors and Direct, Indirect, and Total Effects for the Model (N = 235)Supplementary Table 2
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Heo Y & Hyun H.
Data curation or/and Analysis: Heo Y.
Funding acquisition: None.
Investigation: Heo Y.
Project administration or/and Supervision: Hyun H.
Resources or/and Software: Heo Y.
Validation: Hyun H.
Visualization: Heo Y.
Writing original draft or/and Review & Editing: Heo Y & Hyun H.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
Ahn SH, Lee SH. Updates on coronavirus disease 19 vaccine and its clinical application. Korean Journal of Family Practice 2021;11(4):236–246. [doi: 10.21215/kjfp.2021.11.4.236]
-
-
World Health Organization (WHO). COVID-19: Variants [Internet]. World Health Organization; c2022 [cited 2022 Nov 25].Available from: https://www.who.int/westernpacific/emergencies/covid-
19/information/covid- 19- variants .
-
-
Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes 1991;50(2):179–211. [doi: 10.1016/0749-5978(91)90020-T]
-
-
Seddig D, Maskileyson D, Davidov E, Ajzen I, Schmidt P. Correlates of COVID-19 vaccination intentions: Attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Social Science & Medicine 2022;302:114981 [doi: 10.1016/j.socscimed.2022.114981]
-
-
Yahaghi R, Ahmadizade S, Fotuhi R, Taherkhani E, Ranjbaran M, Buchali Z, et al. Fear of COVID-19 and perceived COVID-19 infectability supplement theory of planned behavior to explain Iranians’ intention to get COVID-19 vaccinated. Vaccines (Basel) 2021;9(7):684 [doi: 10.3390/vaccines9070684]
-
-
Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action Control: From Cognition to Behavior. Springer; 1985. pp. 11-39.
-
-
Ajzen I. TPB questionnaire construction [Internet]. University of Massachusetts Amherst; c2019 [cited 2022 Apr 18].Available from: https://people.umass.edu/aizen/pdf/tpb.measurement.pdf .
-
-
Castanier C, Deroche T, Woodman T. Theory of planned behaviour and road violations: The moderating influence of perceived behavioural control. Transportation Research Part F: Traffic Psychology and Behaviour 2013;18:148–158. [doi: 10.1016/j.trf.2012.12.014]
-
-
Kim HS, Nam ES. Prediction of breastfeeding intentions and behavior: An application of the theory of planned behavior. The Journal of Nurses Academic Society 1997;27(4):796–806. [doi: 10.4040/jnas.1997.27.4.796]
-
-
Do ES, Seo YS. Predictors of intention to quit smoking in elderly smokers following a stroke. Journal of Korean Academy of Fundamentals of Nursing 2014;21(1):48–56. [doi: 10.7739/jkafn.2014.21.1.48]
-
-
Kim MH, Paek KS. Testing the theory of planned behavior in the prediction of contraceptive behavior among married women. Journal of Korean Academy of Nursing 1998;28(3):550–562. [doi: 10.4040/jkan.1998.28.3.550]
-
-
Ambak K, Ismail R, Abdullah RA, Borhan MN. Prediction of helmet use among Malaysian motorcyclist using structural equation modeling. Australian Journal of Basic and Applied Sciences 2010;4(10):5263–5270.
-
-
Bae PW, Suh SR. Predictive factors on breast self-examination intention and behavior in middle aged women: Based on the theory of planned behavior. Journal of the Korea Academia-Industrial Cooperation Society 2013;14(5):2349–2359. [doi: 10.5762/KAIS.2013.14.5.2349]
-
-
Kim LY. In: Factors associated with influenza vaccination intention among the airline cabin crew: An application of the theory of planned behavior [master’s thesis]. Seoul: Yonsei University; 2021. pp. 1-88.
-
-
Ajzen I. The theory of planned behavior: Frequently asked questions. Human Behavior and Emerging Technologies 2020;2(4):314–324. [doi: 10.1002/hbe2.195]
-
-
Korean Ministry of Health and Welfare. COVID-19 vaccination status [Internet]. Korean Ministry of Health and Welfare; c2022 [cited 2022 Jun 5].Available from: https://www.korea.kr/briefing/pressReleaseView.do?newsId=156509611&-
call_ from=nate_ news#pressRelease .
-
-
Korea Disease Control and Prevention Agency (KDCA). In the first week of August, the number of confirmed cases increased by 22.5% compared to the previous week (8.9. regular briefing) [Internet]. Korea Disease Control and Prevention Agency; c2022 [cited 2022 Nov 17].Available from: https://www.korea.kr/briefing/pressReleaseView.do?newsId=156520188&pageIndex=3&rep-
CodeType=&repCode=&startDate=2021- 08- 09&end- Date=2022- 08- 09&srchWord=&period= .
-
-
Bae BR. In: Structural equation modeling with Amos 27. Chungram; 2021. pp. 132-133.
-
-
Ajzen I. Theory of planned behavior with background factors [Internet]. University of Massachusetts Amherst; c2019 [cited 2022 Apr 18].Available from: https://people.umass.edu/aizen/tpb.background.html .
-
-
Hu HQ. In: Investigating factors affecting intention to take COVID-19 vaccine using theory of reasoned action: Focusing on uncertainty of vaccine safety, negative media exposure, knowledge, health involvement [master’s thesis]. Seoul: Kyung Hee University; 2021. pp. 1-100.
-
-
Ajzen I. Constructing a theory of planned behavior questionnaire [Internet]. Measurement Instrument Database for the Social Sciences Ireland; c2013 [cited 2022 May 2].Available from: https://people.umass.edu/aizen/pdf/tpb.questionnaire.pdf .
-
-
Lee KE. Factors associated with intention to receive human papillomavirus vaccine in undergraduate women: An application of the theory of planned behavior. Journal of Korean Academy of Fundamentals of Nursing 2014;21(4):457–465. [doi: 10.7739/jkafn.2014.21.4.457]
-
-
Park YJ, Xia R, Hwang HS. A study on factors that influence university students’ intention on continuous usage of instagram using the theory of planned behavior and SNS literacy: Focused on difference between user groups. Korean Journal of Broadcasting and Telecommunication Studies 2019;33(3):80–107. [doi: 10.22876/kab.2019.33.3.003]
-
-
Park SH, Han MJ. A survey on user attitudes and behavioral intention for identifying preventive campaign measures for illegal online downloading. Journal of Public Relations 2007;11(2):195–231. [doi: 10.15814/jpr.2007.11.2.195]
-
-
Kim SB, Yeom JS. Current advances in pharmacological treatments for patients with COVID-19. Journal of the Korean Medical Association 2021;64(5):375–385. [doi: 10.5124/jkma.2021.64.5.375]
-
-
Ajzen I. Theory of planned behavior diagram [Internet]. University of Massachusetts Amherst; c2019 [cited 2022 Apr 18].Available from: https://people.umass.edu/aizen/tpb.diag.html .
-
-
Ajzen I. Sample TPB questionnaire [Internet]. University of Massachusetts Amherst; c2019 [cited 2022 Apr 18].Available from: https://people.umass.edu/aizen/pdf/tpb.questionnaire.pdf .
-
-
Lee HY, Kim NJ. The impact of fine particular matter risk perception on the outdoor behavior of recreationists: An application of the extended theory of planned behavior. Journal of Tourism Sciences 2017;41(7):27–44. [doi: 10.17086/JTS.2017.41.7.27.44]
-
-
Hwang HH, Cha HW. The effect of non-market issue involvement and market issue involvement on the behavioral intention to visit South Korea: Based on the theory of planned behavior. The Korean Journal of Advertising 2018;29(2):97–130. [doi: 10.14377/KJA.2018.2.28.97]
-
-
Korea Disease Control and Prevention Agency (KDCA). Revision of COVID-19 vaccination practice standards and related FAQ information (as of February 14, 2022) [Internet]. Korea Disease Control and Prevention Agency; 2022 [cited 2022 May 3].
-
-
Aguinis H. Statistical power problems with moderated multiple regression in management research. Journal of Management 1995;21(6):1141–1158. [doi: 10.1016/0149-2063(95)90026-8]
-
-
Moulder BC, Algina J. Comparison of methods for estimating and testing latent variable interactions. Structural Equation Modeling 2002;9(1):1–19. [doi: 10.1207/S15328007SEM0901_1]
-
-
Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research 1981;18(1):39–50. [doi: 10.2307/3151312]
-
-
Woo JP. In: Structural equation model misconceptions and prejudice. Hannarae; 2014. pp. 284-285.
-
-
Fishbein M, Ajzen I. In: Predicting and changing behavior: The reasoned action approach. Psychology Press; 2010. pp. 65-148.
-
-
La Barbera F, Ajzen I. Control interactions in the theory of planned behavior: Rethinking the role of subjective norm. Europe’s Journal of Psychology 2020;16(3):401–417. [doi: 10.5964/ejop.v16i3.2056]
-
-
Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology 2001;40(4):471–499. [doi: 10.1348/014466601164939]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

