Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(2); 2024 > Article
- Research Paper Sleep Deprivation and Fatigue among Nurses Working Consecutive Night Shifts: A Prospective Observational Study
- Ari Min, Jisu Seo, Minkyung Kang, Hye Chong Hong
-
Journal of Korean Academy of Nursing 2024;54(2):139-150.
DOI: https://doi.org/10.4040/jkan.23164
Published online: May 31, 2024
2Department of Nursing, The Graduate School, Chung-Ang University, Seoul, Korea
3College of Nursing, Ajou University, Suwon, Korea
-
Corresponding author:
Hye Chong Hong,
Email: julieh@cau.ac.kr
Abstract
Purpose
This study aimed to identify changes in sleep patterns and fatigue levels during consecutive night shifts among shift nurses and to determine the association between sleep parameters and increased fatigue levels during work.
Methods
This prospective observational study employing ecological momentary assessments was conducted using data collected from 98 shift nurses working in Korean hospitals between June 2019 and February 2021. The sleep patterns were recorded using actigraphy. The participants reported their fatigue levels at the beginning and end of each night shift in real time via a mobile link. Linear mixed models were used for the analysis.
Results
Nurses spent significantly less time in bed and had shorter sleep durations during consecutive night shifts than on off-duty days, whereas their wake times after sleep onset were much longer on off-duty days than on on-duty days. Fatigue levels were higher on the second and third night-shift days than on the first night-shift days. A shorter time spent in bed and asleep was associated with a greater increase in fatigue levels at the end of the shift than at the beginning.
Conclusion
Nurses experience significant sleep deprivation during consecutive night shifts compared with off-duty days, and this sleep shortage is associated with a considerable increase in fatigue levels at the end of shifts. Nurse managers and administrators must ensure sufficient intershift recovery time during consecutive night shifts to increase the time spent in bed and sleeping.
Published online May 16, 2024.
https://doi.org/10.4040/jkan.23164
Sleep Deprivation and Fatigue among Nurses Working Consecutive Night Shifts: A Prospective Observational Study
Abstract
Purpose
This study aimed to identify changes in sleep patterns and fatigue levels during consecutive night shifts among shift nurses and to determine the association between sleep parameters and increased fatigue levels during work.
Methods
This prospective observational study employing ecological momentary assessments was conducted using data collected from 98 shift nurses working in Korean hospitals between June 2019 and February 2021. The sleep patterns were recorded using actigraphy. The participants reported their fatigue levels at the beginning and end of each night shift in real time via a mobile link. Linear mixed models were used for the analysis.
Results
Nurses spent significantly less time in bed and had shorter sleep durations during consecutive night shifts than on off-duty days, whereas their wake times after sleep onset were much longer on off-duty days than on on-duty days. Fatigue levels were higher on the second and third night-shift days than on the first night-shift days. A shorter time spent in bed and asleep was associated with a greater increase in fatigue levels at the end of the shift than at the beginning.
Conclusion
Nurses experience significant sleep deprivation during consecutive night shifts compared with off-duty days, and this sleep shortage is associated with a considerable increase in fatigue levels at the end of shifts. Nurse managers and administrators must ensure sufficient intershift recovery time during consecutive night shifts to increase the time spent in bed and sleeping.
INTRODUCTION
Nurses are an essential part of healthcare organizations and must be available for any shift within a 24-hour service schedule and perform vital responsibilities that involve constant monitoring and care for unwell patients [1, 2]. Hence, night-shift work is inevitable for hospital nurses worldwide [3]. Most nurses in South Korea are engaged in rapid rotations of eight-hour shifts [4]. A recent study reported that Korean hospital nurses work approximately seven days of night shifts per month, with more than two-thirds working three consecutive night shifts [5].
Disruptions in sleep and alertness are frequently noted in shift workers, especially in those who work night shifts [6]. Moreover, a wealth of evidence supports the fact that the disruption of circadian rhythms and sleep patterns accounts for the substantial impact of night-shift work on the health and performance of healthcare providers [7, 8, 9]. Consequently, the safety of both patients and healthcare providers can be negatively affected by decreased alertness, increased fatigue, and an increased risk of errors and accidents in the workplace [10, 11, 12].
Most nurses working night shifts experience sleep disruptions due to alterations in their circadian rhythms [13]. Interference with regular circadian rhythms can lead to shortened sleep duration and poor sleep quality in shift nurses, particularly among night-shift nurses [14, 15, 16, 17]. Excessive sleepiness and drowsiness during night shifts in the period immediately following the shift and lack of adequate sleep during the day following the night shift are frequently reported by night-shift workers, including nurses [12, 18]. Sleep is more restricted among healthcare providers working consecutive night shifts than those working consecutive day shifts [8]. Constant sleep deprivation increases the risk of various chronic diseases, including cardiovascular disease, diabetes, metabolic syndrome, cancer, and mental illness [19, 20, 21, 22].
More importantly, sleep disturbance was significantly associated with fatigue among nurses [23]. Nurse fatigue refers to work-related states associated with an overwhelming sense of tiredness, exhaustion, and a lack of energy that may impair both physical and cognitive performance [23, 24]. Nurse fatigue is associated with negative nurse outcomes, such as decreased alertness and vigilance levels, concentration deficits, and increased risk of errors, all of which are more pronounced in nurses working night shifts [9, 15, 25, 26]. Fatigue is the main cause of medication errors and can affect the quality of care and safety of patients and staff [1, 9, 27]. Fatigue symptoms are also more prevalent and severe among night-shift nurses than day-shift nurses [23, 28].
The number of night shifts was also associated with nurse fatigue [29]. A national survey of nurses in New Zealand revealed that the risk of fatigue-related outcomes, such as clinical errors, drowsy driving, and excessive sleepiness, increased with the number of night shifts [30]. Moreover, fatigue can be exacerbated by consecutive workdays, which may increase accident rates [31].
Studies have indicated that working night shifts is associated with sleep problems and increased fatigue [30, 32]; however, to the best of our knowledge, no previous studies have investigated sleep pattern changes during consecutive days of night-shift work or the effects of potential sleep-pattern changes related to nurse fatigue during night shifts. Examining these relationships is important because nurses’ fatigue can influence both patients’ and nurses’ health. Therefore, the specific aim and purpose of this study were to identify the changes in sleep patterns and fatigue levels during consecutive night shifts among night-shift nurses and to clarify the association between sleep parameters and the increase in fatigue levels at work using ecological momentary assessments (EMA) and actigraphy.
METHODS
1. Study design
The current study conducted a secondary analysis using data from a project Scheduling to Avoid Fatigue and Exhaustion (SAFE) to examine changes in sleep patterns and levels of alertness and fatigue among shift nurses working in acute-care hospitals in South Korea [33, 34]. This project employed a prospective observational study design and an EMA.
2. Participants
The participants were recruited using convenience sampling. In total, 148 shift nurses who provided direct care in acute care hospitals in Korea participated in the SAFE project. Six participants were excluded (two because of discomfort while wearing the device and four because of incomplete data). To be included in this secondary data analysis, participants had to have had two or three consecutive night shifts, with one day off before and two days off after the night shift: off/night/night/night (optional)/off/off. This is the most common scheduling pattern used for night shifts in South Korea. After excluding ineligible participants, complete data from 98 participants (i.e., without any period of not wearing the actigraph) was included in this study. Among the participants, 62.2% of nurses worked fixed night shifts (n = 61), and others worked rotating shifts (37.8%, n = 37). The number of study participants was sufficiently larger than the required sample size, which was at least 40 samples for linear mixed models to detect a medium effect at 0.50 (power of at least 0.80, alpha = 0.05) over six days for each participant [35].
3. Data collection
Data were collected between June 2019 and February 2021 (none of the participants were involved in COVID-19-related patient care or working units). This study employed the EMA approach to obtain real-time data on sleep parameters and fatigue levels. Sleep parameter data were collected using a wrist actigraph ReadiBand (sample rate of 16 Hz; Fatigue Science). Participants wore the ReadiBand on their non-dominant hand, and the device objectively measured sleep parameters (i.e., minutes in bed, minutes asleep, latency, efficiency, wake time after sleep onset [WASO], and sleep quality) using the sleep-wake patterns of the participants by tracking the frequency of wrist movement. Additionally, the participants reported their subjective fatigue levels in real time before and after every shift via a mobile link. All participants provided demographic information on the first day of their participation in the online survey.
4. Measures
1) Sleep parameters
Sleep parameters included minutes spent in bed, minutes asleep, latency, efficiency, WASO, and sleep quality. Minutes in bed, minutes asleep, and latency (the time taken for sleep onset) were measured in minutes. Efficacy was defined as the total number of minutes spent in bed divided by the total number of minutes spent asleep. This is expressed as a percentage, with a higher percentage indicating better sleep efficacy. WASO refers to the time spent awake after sleep onset per night and is also measured in minutes. Sleep quality was calculated based on sleep parameters, with scores ranging from 0 to 10, with higher scores indicating better sleep quality.
The ReadiBand has been validated against laboratory-controlled assessments and demonstrates an accuracy rate of 93% while measuring sleep parameters, compared with the gold standard of polysomnography [36, 37], and is used in nurse populations [38]. Additionally, it demonstrates excellent inter-device reliability, as established in previous studies [38].
2) Fatigue
To capture real-time data, the participants were asked to report their subjective fatigue levels on a 10-point scale at the beginning and end of each shift via a mobile link. Higher scores indicated greater fatigue levels.
3) Demographic characteristics
The demographic characteristics of the study participants included age, gender (all participants were woman), marital and parental details, educational level (associate’s degree, bachelor’s degree, and master’s degree or higher), work experience, number of assigned patients nature of the working unit (medical/surgical unit, intensive care unit, or emergency room), nursing care model (functional method, team nursing, total patient care, or mixed type), hospital type (tertiary or general hospital), hospital size (number of beds), and teaching status (yes or no). All characteristics are included in the Supplementary Table 1.
5. Data analysis
Data were analyzed using STATA 15.1 (StataCorp.). The sleep parameters on each study day were defined as follows: off-duty day 0 (D0) stands for “the day before the first night shift,” and the sleep parameters of D0 include all sleep data that occurred before the first night shift, including naps. For example, if a nurse sleeps through the night and takes an additional nap just before the start of the first night shift, these two sleep records are defined as sleep parameters for the off-duty (D0). Each night shift was labeled first night shift (N1), second night shift (N2), or third night shift (N3). The sleep parameters for each night shift were measured using sleep data collected after each night shift, including naps. That is, the sleep parameters of N1 represent the sleep records between N1 and N2 and typically represent daytime sleep after the night shift is completed. Additionally, D1 and D2 refer to the first and second off-duty days after consecutive night shifts, respectively. As defined above, if sleep occurred during the daytime after completing the previous (second or third) night shift, the sleep data were defined as the sleep parameters of N2 and N3, respectively. In contrast, if sleep occurred again (or for the first time) at night after the previous (second or third) night shift, the sleep data were defined as the sleep parameters of the first off-duty day after consecutive night shifts (D1).
Descriptive statistics (mean, standard deviations [SD], frequencies, and percentages) were used to describe the characteristics of the study participants. Differences in sleep parameters and fatigue levels by shift were analyzed using linear mixed models with the Bonferroni correction, which is a multiple comparison correction. A paired t-test was also performed to determine differences in fatigue levels at the beginning and end of night shifts. Additionally, the association between sleep parameters and differences in fatigue levels at the beginning and end of each shift was examined using a linear mixed model. A p < .050 indicated statistical significance, and a 95% confidence interval (CI) was used.
6. Ethical consideration
Ethical review and approval for this study were waived by the institutional review board of the Chung-Ang University because this study was a secondary analysis of existing data (No. 1041078-202108-HRSB-241-01).
RESULTS
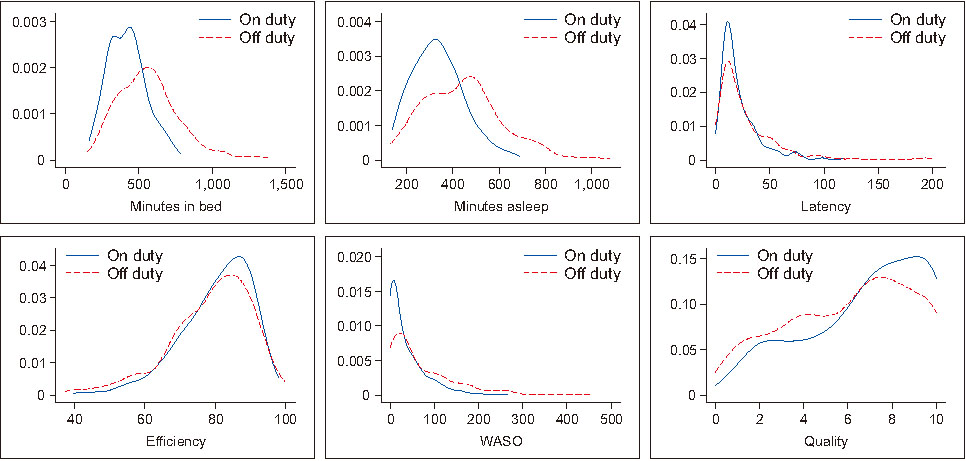
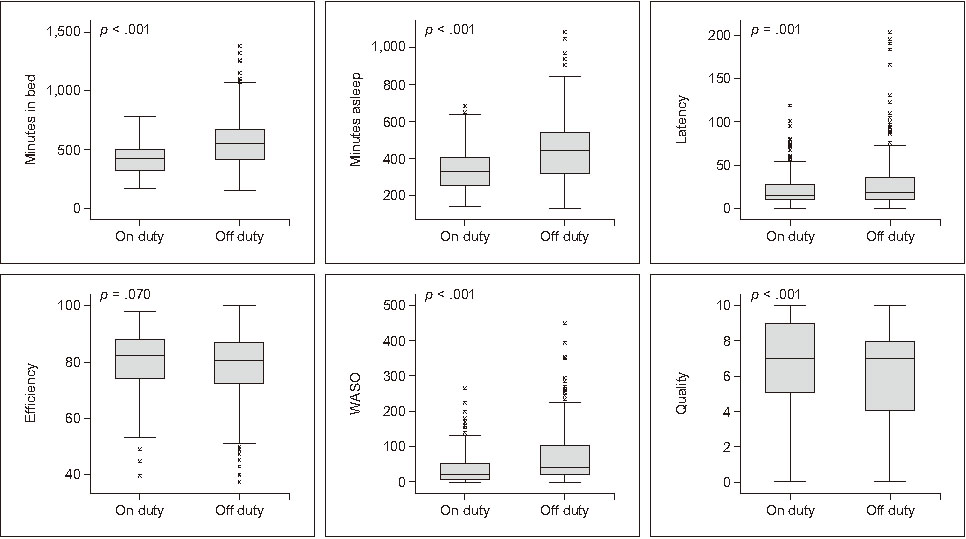
The demographic characteristics of the participants are presented in Supplementary Table 1. Figure 1 depicts the distribution of sleep parameters on both the on- and off-duty days. A linear mixed model with each participant as the random intercept was used to evaluate the differences in sleep parameters on on- and off-duty days (Figure 2; see also Supplementary Table 2 for detailed results). The minutes spent in bed (β = -148.07, p < .001), minutes asleep (β = -108.78, p < .001), latency (β = -7.17, p = .001), and WASO (β = -34.53, p < .001) were significantly lower on on-duty days than on off-duty days. Further, the sleep quality score was significantly higher on on-duty days than on off-duty days (β = 0.76, p < .001), whereas efficiency did not significantly differ (β = 1.61, p = .070).
Figure 1
Distribution of sleep parameters by on-duty and off-duty days.
WASO = Wake time after sleep onset.
Figure 2
WASO = Wake time after sleep onset; CI = Confidence interval.
Box and whisker plots showing median, intraquartile range, 95% CIs, and outliers of sleep characteristics between on-duty and off-duty days (N = 515 shifts, 98 nurses).
p-values were derived from the linear mixed model.
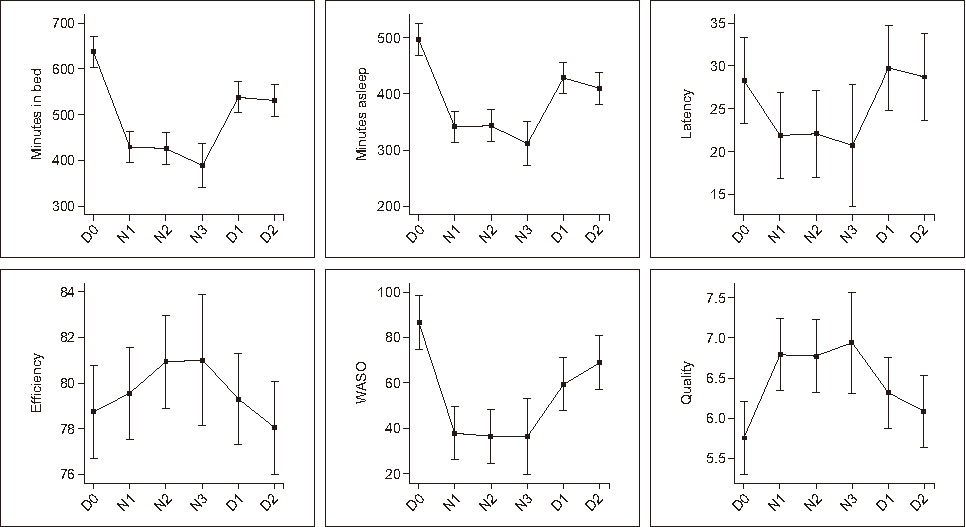
Figure 3 presents the results of the linear mixed model for differences in sleep parameters according to the days on which the study was conducted (see Supplementary Table 3 for detailed results). The time spent in bed was the longest on the day before the first night shift (mean [M] = 636.79), followed by two off-duty days after consecutive night shifts (D1: M = 539.18, D2: M = 530.54) and during consecutive night shifts (N1: M = 427.58, N2 = 425.67, N3 = 395.25). The minutes asleep were significantly longer on the day before the first night shift (D0: M = 497.35), followed by the two off-duty days after consecutive night shifts (D1: M = 430.08, D2: M = 409.92), and during consecutive night shifts (N1: M = 340.65, N2: M = 342.97, N3: M = 316.70). No significant differences were observed in terms of latency or efficiency. However, the WASO was significantly longer on the day before the first night shift (D0: M = 86.31), followed by the first off-duty day after consecutive night shifts (D1: M = 59.67), and during consecutive night shifts (N1: M = 37.46, N2: M = 36.63, N3: M = 35.94). Furthermore, the WASO was longer on the second off-duty day after consecutive night shifts (D2: M = 68.42) than during consecutive night shifts. Sleep quality scores were significantly higher on night-shift days (N1: M = 6.79, N2: M = 6.74, N3: M = 7.11) than on the day before the first night shift (D0: M = 5.77).
Figure 3
Predictive margins with 95% CIs of the linear mixed model results for the association between sleep characteristics and days on which the study was conducted.
D0 = The day before first night shift; D1 = The first off-duty day after consecutive night shifts; D2 = The second off-duty day after consecutive night shifts; N1 = The first nights shift; N2 = The second night shift; N3 = The third night shift; WASO = Wake time after sleep onset; CI = Confidence interval.
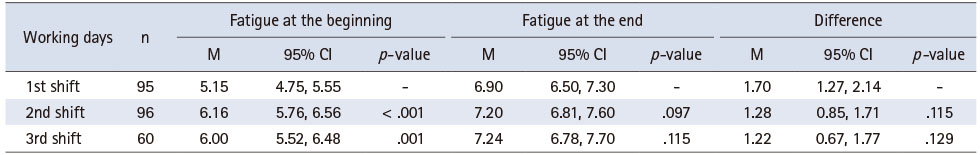
The difference in fatigue levels between the beginning and end of the night shift was evaluated using a paired t-test. The level of fatigue increased significantly at the end of the shift (M = 7.07, SD = 2.02) compared to the beginning (M = 5.72, SD = 2.04; t = -10.52, p < .001). Additionally, differences in fatigue levels at the beginning and end of each working day were investigated using linear mixed models with the Bonferroni correction (Table 1). Fatigue levels at the beginning of the night shift were significantly higher on the second (p < .001) and third days (p = .001) than on the first day. No significant differences were observed in fatigue levels at the end of or according to working days.
Table 1
Differences in the Level of Fatigue at the Beginning and End by Working Days
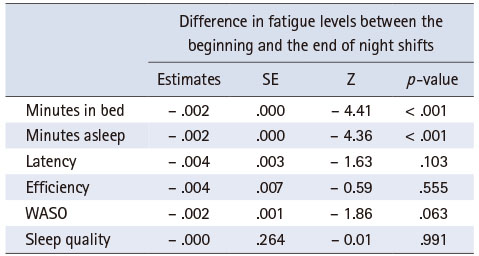
The effects of sleep parameters on differences in fatigue levels at the beginning and end of a night shift were investigated using linear mixed models (Table 2). Minutes in bed (β = -0.002, p < .001) and minutes asleep (β = -0.002, p < .001) were significantly negatively associated with the increase in fatigue levels at the end of night shifts compared with the beginning, whereas other sleep parameters did not contribute significantly.
Table 2
Association between Sleep Parameters and Differences in Fatigue Levels between the Beginning and End of Night Shifts among Hospital Nurses (N = 98)
DISCUSSION
This study aimed to identify changes in sleep patterns and fatigue levels during consecutive night shifts among shift nurses and to determine the association between sleep parameters and fatigue levels during work. Consistent with James et al. [38], we found that nurses spent more time in bed and asleep on off-duty days than on on-duty days. However, even when they were in bed for a longer time, the sleep latency and WASO were longer on off-duty days. Consequently, sleep quality was poorer on off-duty days than on on-duty days. Specifically, nurses were in bed and asleep during most of the daytime hours before their first scheduled night shift; this tendency was also observed in a study among nurses working 12-hour shifts [15]. However, the WASO durations were longer in our study than in nurses surveyed by Geiger-Brown et al. [15]. Remarkably, our findings revealed that nurses wake up less during sleep hours on on-duty days than on off-duty days. Thus, their sleep quality was better on on-duty days than on off-duty days. However, several factors, such as sleep environment, family obligations, and other personal factors, may have influenced the difference in the number of waking episodes and the time spent awake following such episodes between on- and off-duty days. Further studies are required to determine the underlying mechanisms of these relationships.
Nurses should attempt to adjust to working night shifts by compensating for possible sleep loss before the start of the first night shift. This is especially true for those working consecutive night shifts. Moreover, nurses attempt to compensate for the loss of sleep at night on off-duty days after consecutive night shifts [38], indicating an accumulation of sleep debt on duty days. Researchers recommend that nurses need at least three off-days after working two consecutive night shifts to adequately recover from fatigue [39]. The Korean Ministry of Health and Welfare [40] provided guidelines recommending that employees be given at least 48 hour of rest after working two consecutive night shifts. However, approximately two-thirds of nurses in Korea reported not being provided with this rest time [41]. Offering adequate time for full restoration and recovery before returning to work is of paramount importance for nurses in enhancing their work performance and keeping patients safe. Based on the findings of previous studies and our results, policy development at the organizational and unit levels, guaranteeing adequate consecutive days off after night shifts, is crucial for enhancing adequate intershift recovery among shift nurses.
In our study, nurses needed a shorter time to fall asleep with shorter sleep hours on on-duty days than on off-duty days, which supports the presumption that sleep deficiency occurs during consecutive night shifts; consequently, nurses may be sleepier during on-duty days than during off-duty days. Studies have reported that sleep deficiency among nurses could increase the risk of a decline in alertness at work, impair performance [15], and increase errors in patient care [42]. Nurses sleep fewer hours than recommended before work, and such a short sleep duration affects the quality of care and patient safety [33]. Sleep deprivation in nurses is linked to slow reaction times and frequent attention lapses while providing patient care [43], which could threaten patient safety. Moreover, overall sleep quality predicted medication administration errors among nurses [44].
Given that our participants had considerably short sleep durations (less than six hours) during on-duty days, nurses may be at a greater risk of injury, impaired performance, and committing errors that could affect patient safety. Therefore, effective strategies for enhancing sleep quantity and quality on on-duty days are urgently required for shift nurses, especially those engaged in night shifts.
In addition, the longer duration spent in bed with poor sleep quality before and after consecutive night shifts indicated that our participants may have experienced circadian rhythm disruption. Studies have indicated that disruptions in circadian rhythms, sleep homeostasis, and insomnia symptoms are common in nurses working night shifts [17, 45]. James et al. [38] reported that night-shift nurses can experience difficulty switching back and forth between the day and night shifts. Chronic sleep disruptions can affect the physical and mental health of nurses [19, 20, 21, 22], and lead to fatigue [23]. Moreover, circadian disruptions may be more evident when working with rotating shifts.
The provision of 24-hour services is inevitable in nursing, and some nurses must work night shifts. However, solutions for sleep deprivation and fatigue need to be identified. Fixed night shifts can be a solution for improving sleep quality among nurses who work night shifts. Although fixed-night shifts are uncommon in Korea, only a few hospitals have implemented them. However, the effect of working fixed night shifts on the quantity and quality of sleep in an 8-hour shift system is currently unknown and needs to be studied in the future.
Previous studies have reported that work-related sleep loss leads to nurse fatigue, which can cause nurses to make errors in vital care; for example, they may make critical mistakes in administering medication or falter while making clinical decisions [11, 46]. Nurses with short sleep durations (< 7 hour) experienced more fatigue and excessive daytime sleepiness than their counterparts, and occupational errors commonly occurred among nurses with short sleep durations [47]. Moreover, fatigued nurses are more likely to make errors [48] because they are less likely to be alert or concentrate on providing patient care [9]. In our study, as expected, nurses experienced greater fatigue at the end of each shift than at the beginning, and fatigue levels were significantly higher in the second and third consecutive night shifts than in the initial shift. Our findings are consistent with those of a study of 12-hour shift nurses [15], in which nurses’ neurobehavioral functions decreased from the beginning to the end of their shifts, and night-shift nurses were more prone to sleepiness at the end of their shifts than day-shift nurses. The nurses were also sleepier during each consecutive work shift. These findings suggest that nurses may experience accumulated sleep debt during consecutive night shifts.
Similarly, nurses working more consecutive night shifts had significantly lower sleep quantity, lower sleep efficiency, and longer sleep latency than those working 0~2 consecutive night shifts [49], indicating that an increased number of consecutive night shifts may lead to the accumulation of sleep debt and accelerate fatigue among nurses. The Korean Ministry of Health and Welfare [43] provides guidelines that limit the number of consecutive night shifts to three. Nevertheless, some nurses in Korea continue to work four or five consecutive night shifts [41]. Thus, the development of regulations and monitoring systems that restrict the number of consecutive night shifts is required for nurses in the country. Furthermore, nurse managers should consider shift arrangements prior to assigning consecutive night shifts because nurse fatigue can accumulate if a day or evening shift is arranged before consecutive night-shift work.
The impact of shift arrangements on sleep and fatigue may be more important among nurses working eight-hour rotating shifts, as they may switch shifts faster and have less time to adjust to their circadian rhythm, with less recovery time. However, the effects of shift arrangements before consecutive night shifts could not be examined because our study focused only on a set of shifts that included one day off before night shifts. Future research is needed to examine how the arrangement of shifts affects nurse fatigue and sleep deficiency and to provide evidence for nurse managers to develop healthy schedules for nurses.
More importantly, our findings demonstrated that nurses who spent more time in bed displayed a smaller increase in fatigue levels before and after night shifts. In other words, fatigue levels may have been reduced if the nurses had adequate recovery with longer sleep hours between consecutive night shifts. Therefore, adequate sleep duration should be guaranteed between shifts, and optimal strategies should be implemented to promote sleep quantity in nurses working night shifts. At the individual level, nurses should educate themselves about the risks of sleep deficiency as it pertains to their health as well as the health of their patients [50]. Nurses can use personal strategies to improve sleep quality, such as avoiding caffeinated drinks toward the end of a night shift, participating in regular aerobic exercise, restricting electronic media use in bed before sleeping, or taking melatonin after a night shift [13]. Additionally, for nurses to fully recover between shifts, managers and administrators should promote sleep health and alertness by avoiding extended working hours (or overtime) and too many consecutive night shifts that could interfere with adequate sleep [45, 47].
1. Limitations
This study also outlines some limitations. We employed convenience sampling to recruit participants; therefore, caution should be exercised when generalizing the study results. Individual characteristics such as marriage, number of children, and chronic illness may have contributed to sleep quantity, quality, and fatigue. Moreover, stress levels related to work, relationships between coworkers, and the work environment may differ between units and departments, which may contribute to nurse fatigue. For a more accurate interpretation of the results, individual and organizational factors should be considered and controlled in future studies. Despite these limitations, our results add important knowledge to previous research by interpreting 515 on- and off-duty days among shift nurses using objective measures such as ReadiBand and ecological momentary assessment.
CONCLUSION
Consecutive night shifts lead to poor sleep quality and quantity among hospital nurses and increased fatigue near the end of their shifts. As nurse fatigue is associated with various adverse patient and nurse outcomes, effective strategies to enhance sleep quantity and quality during on-duty days are crucial for shift nurses, especially those involved in night shifts. These strategies should be considered at policy development, national, and organizational levels. This evidence supports limiting consecutive night shifts and guaranteeing consecutive days off after night shifts to enhance inter-shift recovery. Nurse managers should consider shift arrangements and limit extended working hours. Individual nurses should be aware of the risks associated with sleep deprivation to ensure patients’ and their own well-being.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online at https://doi.org/10.4040/jkan.23164.
Demographic Characteristics of Study Population (N = 98)Supplementary Table 1
Differences in Sleep Parameters between On-Duty and Off-Duty Days (N = 515 days, 98 nurses)Supplementary Table 2
Differences in Sleep Parameters according to the Days On Which the Study was Conducted (N = 515 days, 98 nurses)Supplementary Table 3
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
FUNDING:This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (no. 2018R1D1A1B07042018) and Chung-Ang University Research Scholarship Grants in 2022.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Min A & Seo J & Kang M & Hong H.
Data curation or/and Analysis: Min A & Seo J.
Funding acquisition: Min A.
Investigation: Min A & Kang M & Hong H.
Project administration or/and Supervision: Min A.
Resources or/and Software: Min A & Seo J.
Validation: Min A & Kang M.
Visualization: Min A & Seo J.
Writing original draft or/and Review & Editing: Min A & Seo J & Kang M & Hong H.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
Pélissier C, Cavelier C, Vercherin P, Roche F, Patural H, Fontana L. Vigilance and sleepiness in nurses working 12-hr shifts and their coping strategies. Journal of Nursing Management 2021;29(5):962–970. [doi: 10.1111/jonm.13233]
-
-
Shiffer D, Minonzio M, Dipaola F, Bertola M, Zamuner AR, Dalla Vecchia LA, et al. Effects of clockwise and counterclockwise job shift work rotation on sleep and work-life balance on hospital nurses. International Journal of Environmental Research and Public Health 2018;15(9):2038 [doi: 10.3390/ijerph15092038]
-
-
Dall’Ora C, Dahlgren A. Shift work in nursing: Closing the knowledge gaps and advancing innovation in practice. International Journal of Nursing Studies 2020;112:103743 [doi: 10.1016/j.ijnurstu.2020.103743]
-
-
Park SK, Jo KM, Jwa YK, Kang DW, Lee YJ. Survey on the current status of nurse activity [Internet]. Korea Health Industry Development Institute; c2014 [cited 2023 Dec 1].Available from: https://www.khidi.or.kr/board/view?linkId=158628&menuId=MENU00085 .
-
-
Reinberg A, Smolensky MH, Riedel M, Touitou Y, Le Floc’h N, Clarisse R, et al. Chronobiologic perspectives of black time--accident risk is greatest at night: An opinion paper. Chronobiology International 2015;32(7):1005–1018.
-
-
Sagherian K, Clinton ME, Abu-Saad Huijer H, Geiger-Brown J. Fatigue, work schedules, and perceived performance in bedside care nurses. Workplace Health & Safety 2017;65(7):304–312. [doi: 10.1177/2165079916665398]
-
-
Garde AH, Hansen AM, Hansen J. Sleep length and quality, sleepiness and urinary melatonin among healthy Danish nurses with shift work during work and leisure time. International Archives of Occupational and Environmental Health 2009;82(10):1219–1228. [doi: 10.1007/s00420-009-0419-4]Erratum in: International Archives of Occupational and Environmental Health. 2010;83(1):119.
-
-
Kaliyaperumal D, Elango Y, Alagesan M, Santhanakrishanan I. Effects of sleep deprivation on the cognitive performance of nurses working in shift. Journal of Clinical and Diagnostic Research 2017;11(8):CC01–CC03. [doi: 10.7860/JCDR/2017/26029.10324]
-
-
Hansen AB, Stayner L, Hansen J, Andersen ZJ. Night shift work and incidence of diabetes in the Danish Nurse Cohort. Occupational & Environmental Medicine 2016;73(4):262–268. [doi: 10.1136/oemed-2015-103342]
-
-
Mealer M, Jones J, Newman J, McFann KK, Rothbaum B, Moss M. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: Results of a national survey. International Journal of Nursing Studies 2012;49(3):292–299. [doi: 10.1016/j.ijnurstu.2011.09.015]
-
-
Vallières A, Azaiez A, Moreau V, LeBlanc M, Morin CM. Insomnia in shift work. Sleep Medicine 2014;15(12):1440–1448. [doi: 10.1016/j.sleep.2014.06.021]
-
-
Fang J, Kunaviktikul W, Olson K, Chontawan R, Kaewthummanukul T. Factors influencing fatigue in Chinese nurses. Nursing & Health Sciences 2008;10(4):291–299. [doi: 10.1111/j.1442-2018.2008.00407.x]
-
-
Øyane NM, Pallesen S, Moen BE, Akerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One 2013;8(8):e70228 [doi: 10.1371/journal.pone.0070228]
-
-
Scherbaum CA, Ferreter JM. Estimating statistical power and required sample sizes for organizational research using multilevel modeling. Organizational Research Methods 2009;12(2):347–367. [doi: 10.1177/1094428107308906]
-
-
Russell C, Caldwell J, Arand D, Myers L, Wubbels P, Downs H. Validation of the fatigue science ReadiBand actigraph and associated sleep/wake classification algorithms [Internet]. Archionetics; c2000 [cited 2021 Feb 15].Available from: https://www.fatiguescience.com/wp-
content/uploads/2016/09/Readiband- Validation- Accuracy.pdf .
-
-
Korean Ministry of Health and Welfare (MOHW). Nurse workers’ night shift guideline [Internet]. Korean Ministry of Health and Welfare; c2019 [cited 2023 Dec 1].Available from: https://www.mohw.go.kr/board.es?mid=a10501010400&bid=0003&tag=&act=view&list_
no=350963 .
-
-
Cho SH, Hong KJ, Jung EH. Analysis of the current status of nurses’ shift work and improvement plan based on the guidelines for night shift work by the Ministry of Health and Welfare [Internet]. Hospital Nurses Association; c2020 [cited 2023 Dec 1].Available from: https://khna.or.kr/home/pds/utilities.php .
-
-
Di Muzio M, Dionisi S, Di Simone E, Cianfrocca C, Di Muzio F, Fabbian F, et al. Can nurses’ shift work jeopardize the patient safety? A systematic review. European Review for Medical and Pharmacological Sciences 2019;23(10):4507–4519. [doi: 10.26355/eurrev_201905_17963]
-
-
Abdulah DM, Suleman SK. Interactive effects of sleep difficulty and time pressure on patient safety in nurses in public hospitals. Sleep and Vigilance 2021;5(2):299–307. [doi: 10.1007/s41782-021-00171-3]
-
-
Chaiard J, Deeluea J, Suksatit B, Songkham W, Inta N. Short sleep duration among Thai nurses: Influences on fatigue, daytime sleepiness, and occupational errors. Journal of Occupational Health 2018;60(5):348–355. [doi: 10.1539/joh.2017-0258-OA]Erratum in: Journal of Occupational Health. 2018;60(6):e2.
-
-
Morelock S. Sustained vigilance and errors in critical care. Nursing Critical Care 2016;11(6):38–47. [doi: 10.1097/01.CCN.0000503414.59852.16]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

