Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 52(6); 2022 > Article
- Research Paper Factors Influencing Preventive Behaviors for COVID-19 in Undergraduate Nursing Students: A Cross-Sectional Descriptive Study
- Jeong Sil Choi, Kyung Mi Kim
-
Journal of Korean Academy of Nursing 2022;52(6):554-563.
DOI: https://doi.org/10.4040/jkan.22047
Published online: December 31, 2022
2Department of Nursing Science, Medical College, Chungbuk National University, Cheongju, Korea
Abstract
Purpose
This study aimed to determine how undergraduate nursing students’ knowledge and health beliefs affected their COVID-19-related infection-prevention behaviors.
Methods
This study used a descriptive survey. A total of 188 undergraduate nursing students from two universities in South Korea participated in this study. The data were collected from June 2020 to August 2020. Factors influencing infection-prevention behaviors were identified using multiple regression analysis.
Results
The participants’ mean knowledge level regarding COVID-19 was 84.05 ± 11.78 out of 100. The average health belief score was 2.80 ± 0.32 points out of 5. COVID-19-related preventive health behaviors were correlated with experiences of searching for COVID-19 information (r = .22, p < .01), perceived severity (r = .24, p < .01), perceived benefits (r = .29, p < .01), cues to action (r = .30, p < .01), knowledge (r = .27, p < .01), and perceived barriers (r = - .19, p < .05). Factors that significantly affected COVID-19-related preventive health behaviors were the participants’ years of study, experiences regarding COVID-19 prevention education, perceived severity, perceived barriers, and cues to action.
Conclusion
COVID-19-related preventive health behaviors are promoted by increasing awareness about the disease and promoting COVID-19 education in nursing curriculums.
Published online Dec 31, 2022.
https://doi.org/10.4040/jkan.22047
Factors Influencing Preventive Behaviors for COVID-19 in Undergraduate Nursing Students: A Cross-Sectional Descriptive Study
Abstract
Purpose
This study aimed to determine how undergraduate nursing students’ knowledge and health beliefs affected their COVID-19-related infection-prevention behaviors.
Methods
This study used a descriptive survey. A total of 188 undergraduate nursing students from two universities in South Korea participated in this study. The data were collected from June 2020 to August 2020. Factors influencing infection-prevention behaviors were identified using multiple regression analysis.
Results
The participants’ mean knowledge level regarding COVID-19 was 84.05 ± 11.78 out of 100. The average health belief score was 2.80 ± 0.32 points out of 5. COVID-19-related preventive health behaviors were correlated with experiences of searching for COVID-19 information (r = .22, p < .01), perceived severity (r = .24, p < .01), perceived benefits (r = .29, p < .01), cues to action (r = .30, p < .01), knowledge (r = .27, p < .01), and perceived barriers (r = -.19, p < .05). Factors that significantly affected COVID-19-related preventive health behaviors were the participants’ years of study, experiences regarding COVID-19 prevention education, perceived severity, perceived barriers, and cues to action.
Conclusion
COVID-19-related preventive health behaviors are promoted by increasing awareness about the disease and promoting COVID-19 education in nursing curriculums.
INTRODUCTION
The infectious coronavirus disease (COVID-19) was first reported in December 2019 in the Chinese city of Wuhan [1] and later spread worldwide [2]. It is caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). SARS-CoV-2 is genetically distinguishable from coronavirus, which causes severe acute respiratory syndrome or Middle East Respiratory Syndrome (MERS) [3]. However, similar to other types of coronaviruses, SARS-CoV 2 is spread between humans [2]. Hence, the World Health Organization (WHO) has recommended that people should avoid direct contact with those infected with COVID-19 and comply with hand hygiene and respiratory/cough etiquette [2].
In South Korea, the first confirmed COVID-19 cases were identified in January 2020 among individuals who had arrived from Wuhan, and the number of confirmed cases accelerated owing to its spread in local communities [4]. The Korea Disease Control and Prevention Agency (KDCA) raised a disease alert of the highest level on February 23, 2020. It emphasized prevention against the infection [4], infection-prevention principles, and high-intensity social distancing. Implementing proper precaution principles is paramount to preventing the spread of COVID-19. The success of such measures often depends on compliance with preventive actions, which, in turn, is affected by factors such as knowledge and perceptions regarding COVID-19 [5].
People’s health beliefs inform their preventive health practices [6]. The perceptions that constitute health beliefs are perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action, and self-efficacy. The health belief model is used for detecting the infection risk level in order to induce positive changes in one’s health. Additionally, the health belief model is a helpful tool for predicting preventive health behaviors in individuals [7]. Thus, health beliefs can be considered to predict health behaviors and prevent the spread of new infectious diseases [7]. For example, Lee’s [8] study on nursing college students revealed that participants’ health beliefs about MERS were related to their preventive health practices.
Generally, in the first and second years of nursing college, students are educated about basic nursing principles and the basic stages of integrated education; later, they participate in the practicum of third- and fourth-year students. Throughout the COVID-19 pandemic, nursing students completed their clinical practicum in hospitals that had a relatively high infection risk. Albaqawi et al. [5] reported that, because of their high level of learning and the COVID-19-related information in nursing students’ theoretical courses and hospital exposure, their knowledge increased as they climbed higher on the academic ladder. However, nursing education must ensure that students in all grades have equal access to COVID-19 resources (e.g., course information, lectures, practice training, and e-learning) in order to prevent knowledge gaps among students in different grades [5]. Nursing students are future healthcare professionals who will have to address emerging infectious diseases in the future [9]; therefore, it is necessary to investigate the health beliefs, knowledge levels, and infection-prevention performances of nursing students in all grades.
The researchers investigated the impact of health beliefs and knowledge on nursing students’ COVID-19 infection-prevention behavior throughout this study. Furthermore, the researchers intended to (1) provide nursing students with basic data in order to establish an educational program for efficient and implementable infection prevention and (2) help nursing students comply with infection-prevention guidelines and consequently promote good health.
METHODS
1. Design and setting
This cross-sectional descriptive study aimed to determine how nursing students’ health beliefs and knowledge can affect their infection-prevention behaviors. Convenience sampling was used for selecting the study participants, all of whom were undergraduate nursing students enrolled in two universities in two cities (Incheon and Cheongju) in South Korea.
2. Sampling
One hundred and eighty-eight undergraduate nursing students participated in the study. The study participation eligibility criterion was as follows: must be nursing students enrolled in any year of nursing college for more than one semester after the onset of the COVID-19 outbreak. One class (containing approximately 60 students) from each grade was convenience sampled at each university. Due to the COVID-19 pandemic, recruitment posts and information about the study background and purpose were distributed via the KakaoTalk online messenger application. One representative student from each class received a questionnaire in word document format or as a Google questionnaire through an online messenger application; these materials were sent to students who expressed their consent to participate in the study. Two hundred students (40 freshmen, 50 sophomores, 40 juniors, and 70 seniors) from both universities expressed their interest in participating in the study, and questionnaires were therefore distributed to them. Completed questionnaires were submitted to the department’s mailbox or collected via email by representative students.
The sample size was calculated using the G* power 3.1 program [10]. Based on a medium effect size of .15 [9], a significance level of .05, a power of .90, and 18 predictors used for multiple linear regression analysis, the minimum number of participants required for this study was 183. Among the 200 chosen participants, 195 responded to the survey (97.5%); 188 out of these 195 surveys were analyzed, as seven questionnaires were incomplete.
3. Measurements
1) Health beliefs
Health beliefs are defined as people’s ideas, convictions, and attitudes regarding disease [6]. The researchers developed a questionnaire based on previous studies [11, 12] in order to assess study participants’ health beliefs. The content validity of the developed tool was verified by two infection-control preventionists, one infectious disease specialist, and one nursing professor. The developed questionnaire had a Content Validity Index (CVI) of .95.
The COVID-19 Health Belief Questionnaire contains 18 questions: three questions on perceived susceptibility (the degree to which one perceives a risk of developing a disease), three questions on perceived severity (the degree to which one perceives the seriousness of contracting a disease), two questions on perceived benefits (the degree to which one perceives the benefits of taking preventive actions), eight questions on perceived barriers (the degree to which one perceives difficulties in performing a particular health action), and two questions on cues to action (the degree to which one perceives a cue or trigger that can stimulate one to participate in a specific action). The questionnaire used a 5-point Likert-type scale (1: strongly disagree; 5: strongly agree). Higher scores indicated higher perceived susceptibility, severity, benefits, and cues to action. In the case of perceived barriers, higher scores indicated more severe perceived difficulties in taking particular health actions. The preliminary survey confidence level of the 18 nursing students showed a Cronbach’s α of .73, and the confidence level of the final survey showed a Cronbach’s α of .77.
2) Knowledge regarding COVID-19
The researchers developed a measurement tool for assessing COVID-19-related knowledge by using the response guidelines provided by the Centers for Disease Control and Prevention [13] and the KDCA [14, 15] along with the COVID-19 knowledge questions used in Albaqawai et al.’s [5] study involving Saudi Arabian student nurses. Two infection-control preventionists, one physician in the division of infectious diseases, and one nursing professor reviewed the questions for assessing content validity. The researchers then deleted the questions that received ratings of 1 or 2 points for CVI and reorganized the survey into 17 questions: three questions on the disease cause; five questions on the spread mechanism; two questions on the symptom and incubation period; six questions on the diagnostic test, treatment, and prevention; and one question on patient nursing guidelines. A higher score indicated a higher level of knowledge. Next, the researchers conducted a preliminary survey involving 18 nursing students in order to confirm the final version of the tool. Correct answers received 1 point, and responses of “wrong” or “don’t know” received 0 points. The points were calculated based on a perfect score of 100. The final expert validity showed a CVI of .95; furthermore, the Kuder–Richardson 20 score was .65 in the preliminary survey involving 18 nursing students and .72 in the final survey.
3) COVID-19-related preventive health behaviors
COVID-19-related preventive health behaviors refer to the degree to which actions are taken to avoid the infection. The researchers developed a tool for assessing preventive health behaviors by using the KDCA’s COVID-19 response guidelines [15]. The developed questionnaire had a CVI of .95 after being reviewed for validity by one infection-control professor, two infection-control preventionists, and one physician in the infectious disease division. The final tool contained 20 questions: five questions on reducing the use of public places in daily life, six questions on hand hygiene, six questions on mask-wearing, two questions on respiratory/cough etiquette, and one question on cleaning and disinfection reinforcement. A 5-point Likert-type scale (never [never performed at all]: 1 point; always [always performed]: 5 points) was deployed. Higher scores indicated a higher level of health behavior. The scores were converted based on a total score of 100. The preliminary survey confidence level of the 18 nursing students showed a Cronbach’s α of .80, and the confidence level for the final survey showed a Cronbach’s α of .85.
4. Data analysis
The collected data were analyzed using SPSS/WIN 23.0 (IBM Corp., Armonk, NY, USA), which verified that the main variables were normally distributed (Kolmogorov–Smirnov test). The participants’ general characteristics, COVID-19-related health beliefs, and knowledge and infection-prevention performance were calculated using frequency, percentage, average, and standard deviation values. The reliability of the relevant variables was calculated using the Cronbach’s α. The differences in the students’ infection-prevention behaviors based on general characteristics were analyzed using an independent t-test, ANOVA, and post-hoc Scheffe test. Correlations were analyzed using the Pearson’s correlation test. Multiple regression analysis was conducted using an “enter” method to identify the factors affecting infection-prevention behavior by introducing variables that showed statistical significance in the difference test and correlation tests.
5. Ethical considerations
The data collection period lasted from June to August 2020. This study was approved by the Gachon University Institutional Review Board (no. 1044396-202004-HR-081-01). All participants provided informed consent and completed the questionnaires.
RESULTS
1. Sociodemographic characteristics and differences in COVID-19-related preventive health behaviors
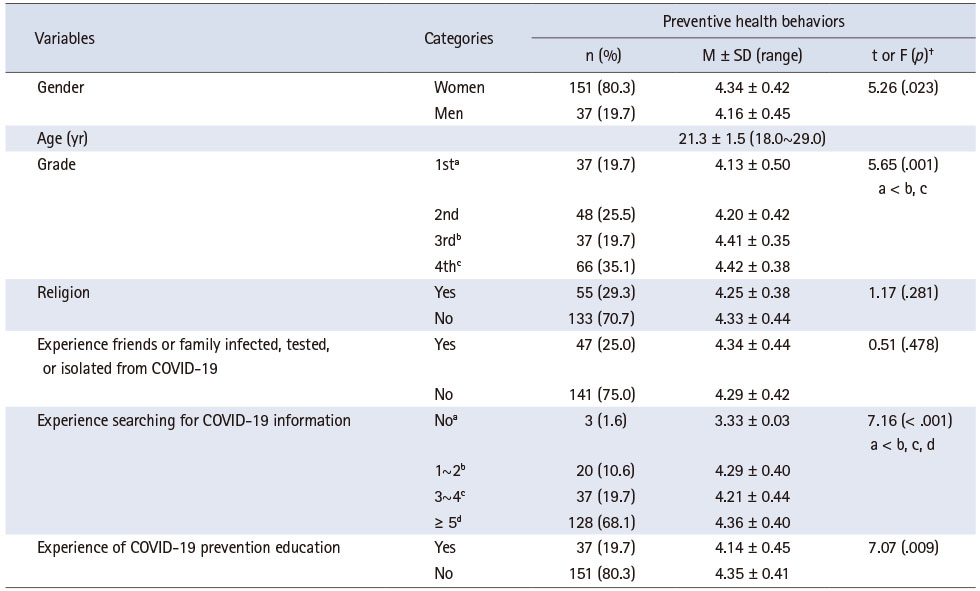
The subjects’ average age was 21.3 years, and 151 (80.3%) were women. Sixty-six students (35.1%) were seniors. Forty-seven (25.0%) participants had had experiences related to infected, tested, and isolated friends or family members, and 128 (68.1%) had conducted information searches for COVID-19 more than five times, which was the most frequent response. One hundred and fifty-one nursing students (80.3%) had no educational experience regarding COVID-19. In terms of general characteristics, participants’ COVID-19-related preventive health behaviors significantly differed depending on their gender, grade, number of information searches for COVID-19, and educational experiences regarding COVID-19 (p < .05) (Table 1).
Table 1
Socio-Demographic Characteristics and Differences in the COVID-19-Related Preventive Health Behaviors (N = 188)
2. Level of health belief, knowledge, and preventive health behaviors
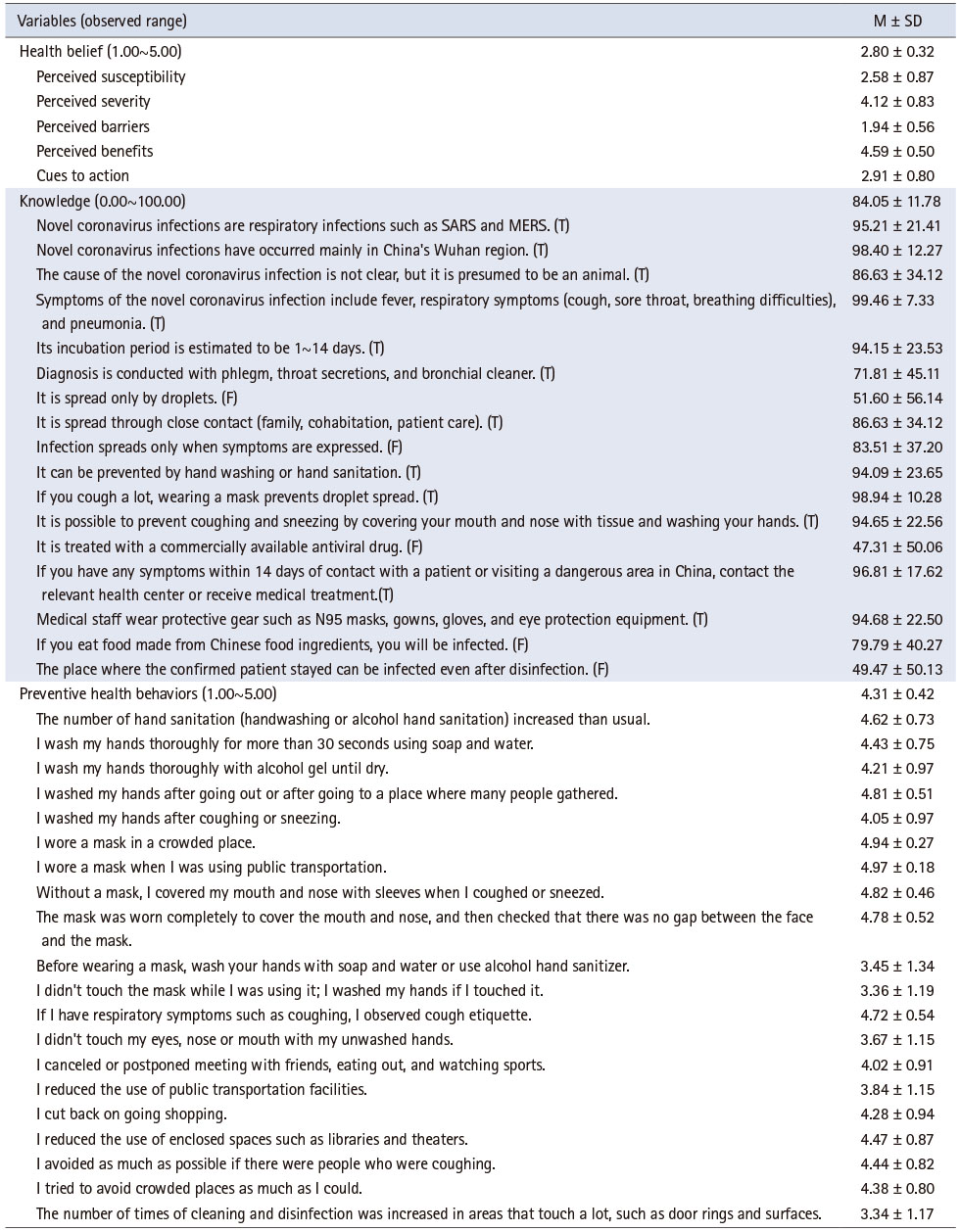
For health belief, the average score was 2.80 ± 0.32 points out of 5. Perceived susceptibility had an average score of 2.58 ± 0.87 points, perceived severity had an average score of 4.12 ± 0.83 points, perceived barriers had an average score of 1.94 ± 0.56 points, perceived benefits had an average score of 4.59 ± 0.50 points, and cues to action had an average score of 2.91 ± 0.80 points. Knowledge level had an average score of 84.05 ± 11.78 points out of 100, and preventive health behaviors had an average score of 4.31 ± 0.42 points out of 5 (Table 2).
Table 2
Level of Main Variables (N = 188)
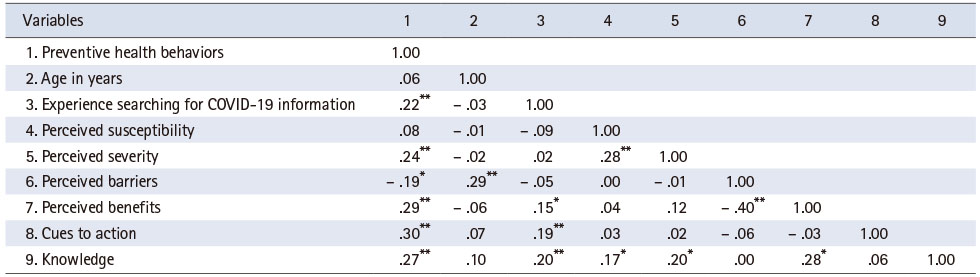
3. COVID-19-related preventive health behaviors and correlation between the main study variables
The study showed some significant positive correlations between COVID-19-related preventive health behaviors and searches for COVID-19 information (r = .22, p < .01), perceived severity (r = .24, p < .01), perceived benefits (r = .29, p < .01), cues to action (r = .30, p < .01), and knowledge (r = .27, p < .01). A significant negative correlation emerged between COVID-19-related preventive health behaviors and perceived barriers (r = -.19, p < .05) (Table 3).
Table 3
Pearson’s Correlation for the Main Study Variables (N = 188)
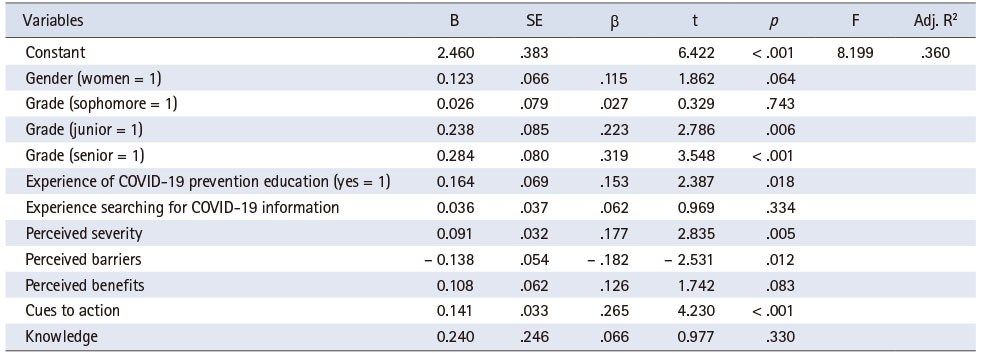
4. Factors predicting COVID-19-related preventive health behaviors
For COVID-19-related preventive health behaviors, the students’ university year (junior: β = .223, p < .05, and senior: β = .319, p < .001) was found to be a significant affecting factor. In the detailed category of health beliefs, COVID-19-related preventive health behaviors were significantly affected by higher perceived severity (β = .177, p < .05), lower perceived barriers (β = -.182, p < .05), and higher cues to action (β = .265, p < .001). These variables accounted for 36.0% of COVID-19-related health behaviors (Table 4).
Table 4
Linear Regression Analysis for Predicting the COVID-19-Related Preventive Health Behaviors (N = 188)
The study’s regression analysis satisfied the basic assumptions of the model. The Durbin–Watson statistic value was not autocorrelated (1.994), tolerance received a score of more than .1 (.450~.957), and the variation inflation factor was also less than 10 (1.045~2.222), thus indicating that there was no problem with multicollinearity.
DISCUSSION
Most of the participants of this study had no educational experience regarding COVID-19; however, their COVID-19-related knowledge level received a score of 84 points, indicating relatively high levels of knowledge. Over half of the participants were found to have gained knowledge about COVID-19 through more than five Internet searches. It is believed that the KCDA’s response guidelines, including the latest updates regarding COVID-19 and social distancing, may have affected the nursing students’ knowledge of COVID-19. For the students, the items with the lowest level of COVID-19 knowledge were “It is spread only through droplets” and “It is treated with a commercially available antiviral drug.” COVID-19 mainly spreads through droplets, but direct contact with infected people, contaminated materials, or contaminated surfaces can also transmit the virus. It is also possible for COVID-19 to spread during aerosol production or in enclosed spaces [14]. Kwok et al. [16] found that medical students touched their faces an average of 23 times per hour, with 44% touching mucous membrane areas (e.g., mouth, nose, and eyes), which are the main channels through which bacteria or viruses spread. The most frequent contact with mucous membranes was conducted through the mouth (36%), nose (31%), and eyes (6%). In a study by KDCA [17], facial contact accounted for 50% of all physical contact cases. Among them, mucosal contact between the eyes, nose, and mouth accounted for 46.3% of all physical contact cases. Average contact frequency between the mouth and nose was found to be high, and the mouth area was reported to have the longest contact time. Therefore, to prevent the spread of COVID-19 through contact, people must wear masks and comply with proper hand hygiene. Hand hygiene is the single most important measure for preventing the transmission of healthcare-associated infections [18]. Nursing students may be exposed to infectious agents and risk becoming disease carriers to others, including patients, during clinical practice in hospitals. Accordingly, nursing students should be able to perform adequate hand hygiene based on accurate knowledge [18]. Therefore, it is necessary to thoroughly educate nursing students on proper hand hygiene through fundamental nursing theory and practice classes and clinical practice in hospitals.
In this study, participants were not very susceptible to developing COVID-19, and their perceived barriers to preventing COVID-19 were not very high. In contrast, their preventive health behaviors were very high. These findings echo that of Fathian-Dastgerdi et al. [19], who studied low sensitivity levels and preventive behavioral obstructions among adolescents. Similarly, in a study of adults aged 18 to 77 years, Shahnazi et al. [12] found that, although perceived barriers such as handwashing-related barriers (perceived barrier to independent preventive behaviors) were low, perceived barriers were still highly influenced by environmental barriers such as shortages of masks, alcohol sponges, and disinfectants. Although masks were not readily available in the early days of the COVID-19 pandemic, the Korean government actively intervened to provide the public with sufficient amounts of hand sanitizer and masks. Consequently, prevention barriers appeared to be lower at the time of this study. Furthermore, the Korean government raised the infectious disease alert level to “orange”–the third level in a four-tier alert system–in January 2020 and promoted COVID-19 prevention rules via mass media and government websites; therefore, the students’ perceived benefits of the guidelines were high, and their level of prevention was considered to have increased.
Additionally, COVID-19-related preventive health behaviors were significantly correlated with searches for COVID-19 information, perceived severity, perceived benefits, cues to action, and knowledge (r = .27, p < .01) and were significantly negatively correlated with perceived barriers. In the study by Fathian-Dastgerdi et al. [19], protective behavior, self-efficacy, perceived benefit, and perceived severity were positively correlated with each other, whereas perceived susceptibility and perceived barriers were negatively correlated; these findings were similar to those of the current study. As excessive obstacles can interfere with the creation of health behaviors [12], it is essential to increase disease prevention-related awareness and reduce environmental barriers to preventive behavior.
In this study, high levels of COVID-19-related preventive health behaviors, higher university years (junior and senior), and high educational experiences regarding COVID-19 resulted in lower perceived barriers and higher cues to action. In a study on COVID-19 repositories, symptoms, and prevention, Elgzar et al. [20] trained nursing students using presentations, group conversations, and problem-solving methods. The authors reported that overcoming their perceived barriers to implementing COVID-19-related preventive actions increased participants’ self-efficacy. In contrast, Shahnazi et al. [12] reported that inducing perceived benefits increased self-efficacy and led individuals to overcome their perceived barriers. Therefore, national efforts are necessary for reducing negative perceptions such as inconvenience, costs, and pain in carrying out COVID-19-related preventive actions. The results of this study also indicate that COVID-19-related knowledge is positively correlated with perceived susceptibility, severity, benefits, and preventive health behaviors. In South Korea, nursing students are educated about infection-control theory in basic nursing and learn core basic nursing skills in practice classes [21]. They then increase their infection control-related knowledge and proficiency through the third- and fourth-year curriculum and clinical practice [21]. However, the core basic nursing skills focus on the use of simple sterile gowns and waste management [21]. Furthermore, the clinical practice focuses only on the disease-related knowledge, nursing interventions, and primary infection-control performance necessary for preventing healthcare-associated infections [21]. Therefore, it is evident that it is insufficient for improving performance related to specialized patient care (e.g., the donning and doffing of personal protective equipment, the treatment and response procedures necessary for infectious disease patients, the preparation and application of practical infection-control guidelines in healthcare settings, patient screening, and so on), which is necessary during infectious disease pandemics, such as the COVID-19 situation [21]. Furthermore, WHO has warned that new infectious diseases are emerging at an unprecedented rate [22]. Therefore, it is necessary to educate nursing students about emerging infectious diseases, including COVID-19, in order to raise their awareness of the seriousness of such viruses, provide them with practical information, and promote their individual readiness for emerging infectious diseases.
The first limitation of this study was that the subjects were convenience sampled from two nursing universities in South Korea. The second limitation was that COVID-19-related preventive health behaviors were self-reported and not directly observed. Last, although this study was conducted relatively recently, its results must be compared with those of other studies examining the latest situation, as the COVID-19 pandemic situation has been changing dramatically since then. As more than two years have passed since the initial outbreak, changes in health beliefs should be considered along with the education and testing experiences of nursing students. Therefore, further studies are warranted in this regard.
CONCLUSION
This study aimed to determine the effect of health beliefs and COVID-19-related knowledge on infection-prevention behaviors among nursing students. The factors that significantly affected COVID-19-related preventive health behaviors were students’ university year of study, experience regarding COVID-19 prevention education, perceived severity, perceived barriers, and cues to action. Therefore, COVID-19-related preventive health behaviors should be promoted by increasing awareness of COVID-19 and imparting COVID-19 education in nursing courses.
CONFLICTS OF INTEREST:The authors declared that no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Choi J.
Data curation or/and Analysis: Choi J.
Funding acquisition: None.
Investigation: Choi J & Kim K.
Project administration or/and Supervision: Kim K.
Resources or/and Software: Choi J.
Validation: None.
Visualization: None.
Writing original draft or/and review & editing: Choi J & Kim K.
ACKNOWLEDGEMENTS
None.
References
-
World Health Organization (WHO). Coronavirus disease 2019 (COVID-19): Situation report, 23 [Internet]. Geneva: WHO; 2020 [cited 2022 Jan 23].Available from: https://apps.who.int/iris/handle/10665/330992 .
-
-
Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology 2020;5(4):536–544. [doi: 10.1038/s41564-020-0695-z]
-
-
Rosenstock IM. The health belief model and preventive health behavior. Health Education Monographs 1974;2(4):354–386. [doi: 10.1177/109019817400200405]
-
-
Shin SH. Relationships between health promoting lifestyle, health belief about emerging infectious disease and hygiene behavior of college students. Journal of the Korea Convergence Society 2019;10(4):285–293. [doi: 10.15207/JKCS.2019.10.4.285]
-
-
Lee KH. In: Knowledge, health belief and preventive health behavior of nursing students on Middle East Respiratory Syndrome(MERS) [master’s thesis]. Seoul: Kyung Hee University; 2017. pp. 1-48.
-
-
Choi JS, Yang NY. Perceived knowledge, attitude, and compliance with preventive behavior on influenza A (H1N1) by university students. Journal of Korean Academy of Adult Nursing 2010;22(3):250–259.
-
-
Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID-19: A cross sectional study with health belief model in Golestan province, northern of Iran. Infectious Diseases of Poverty 2020;9(1):157 [doi: 10.1186/s40249-020-00776-2]
-
-
Centers for Disease Control and Prevention (CDC). COVID-19 [Internet]. Atlanta: CDC; 2020 [cited 2021 Sep 26].Available from: https://www.cdc.gov/coronavirus/2019-
ncov/index.html .
-
-
Korea Disease Control and Prevention Agency (KDCA). COVID-19 information [Internet]. Cheongju: KDCA; 2020 [cited 2022 Jan 25].Available from: http://ncov.mohw.go.kr/baroView.do?brdId=4&brdGubun=41 .
-
-
Korea Disease Control and Prevention Agency (KDCA). COVID-19 response guidelines [Internet]. Cheongju: KDCA; 2020 [cited 2022 Jan 25].Available from: http://ncov.mohw.go.kr/duBoardList.do .
-
-
Korea Disease Control and Prevention Agency (KDCA). Analysis of transmission patterns of infection according to contact behavior in daily life [Internet]. Cheongju: KDCA; 2018 [cited 2022 Jan 25].Available from: https://library.nih.go.kr/ncmiklib/archive/rom/reportView.do .
-
-
Elgzar WT, Al-Qahtani AM, Elfeki NK, Ibrahim HA. COVID-19 outbreak: Effect of an educational intervention based on health belief model on nursing students’ awareness and health beliefs at Najran university, Kingdom of Saudi Arabia. African Journal of Reproductive Health 2020;24(s1):78–86.
-
-
Park HY, Kim YJ. Infection control education programs for nursing students: A systematic review. Journal of Korean Academy of Fundamentals of Nursing 2021;28(2):237–248. [doi: 10.7739/jkafn.2021.28.2.237]
-
-
Shin NR, Baek SJ, Yoo HS, Shin IS. Global trends in preparation for future infectious diseases. Public Health Weekly Report 2019;12(5):120–126.
-
- Related articles
-
- Psychometric testing of the Korean version of the Undergraduate Nursing Student Academic Satisfaction Scale: a methodological study
- Factors influencing smartphone overdependence in university students: an ecological model: a descriptive study
- Factors Influencing the Intention for Continual Fertility Treatments by the Women Undergoing Assisted Reproductive Technology Procedures: A Cross-Sectional Study
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

