Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 53(2); 2023 > Article
- Research Paper Factors Related to Clinical Competence among Graduating Nursing Students during the COVID-19 Pandemic: A Cross-Sectional Study
- Su Kyoung Chung, Jinsook Kim, Pratibha Bhandari
-
Journal of Korean Academy of Nursing 2023;53(2):145-154.
DOI: https://doi.org/10.4040/jkan.22087
Published online: April 30, 2023
-
Corresponding author:
Pratibha Bhandari,
Email: pratibha.bhandari@uts.edu.au
Abstract
Purpose
This study investigated clinical competency, COVID-19-related anxiety, coping strategies, self-efficacy, and perceived stress among graduating nursing students during the COVID-19 pandemic.
Methods
We conducted a cross-sectional survey. Participants were recruited from universities located in four major cities in South Korea. General demographic information, clinical competency, self-efficacy, perceived stress, COVID-19-related anxiety, and coping strategies were assessed using reliable questionnaires. Descriptive statistics, correlations, and multiple regression tests were used to analyze the data.
Results
The mean clinical competency, self-efficacy, perceived stress, adaptive coping, and maladaptive coping were 138.16 ± 18.34, 83.85 ±14.02, 21.37 ± 5.79, 53.15 ± 4.64, and 30.98 ± 6.73, respectively. COVID-19-related anxiety was reported by 4.3% of participants. Clinical competency was significantly positively correlated with self-efficacy (r = .44, p < .001) and adaptive coping (r = .20, p = .035) and was significantly negatively correlated with maladaptive coping (r = .20, p = .035). The predictors of clinical competency were self-efficacy (β = .434, p < .001) and adaptive coping (β = .173, p < .039), which explained 23% of the variance in clinical competency.
Conclusion
Self-efficacy and adaptive coping strategies are significant predictors of clinical competence during the pandemic. Planning and implementing various curricular and non-curricular activities to increase senior students' self-efficacy and adaptive coping strategies will help prepare competent nursing graduates for the pandemic when they enter the nursing workforce.
Published online Apr 30, 2023.
https://doi.org/10.4040/jkan.22087
Factors Related to Clinical Competence among Graduating Nursing Students during the COVID-19 Pandemic: A Cross-Sectional Study
Abstract
Purpose
This study investigated clinical competency, COVID-19-related anxiety, coping strategies, self-efficacy, and perceived stress among graduating nursing students during the COVID-19 pandemic.
Methods
We conducted a cross-sectional survey. Participants were recruited from universities located in four major cities in South Korea. General demographic information, clinical competency, self-efficacy, perceived stress, COVID-19-related anxiety, and coping strategies were assessed using reliable questionnaires. Descriptive statistics, correlations, and multiple regression tests were used to analyze the data.
Results
The mean clinical competency, self-efficacy, perceived stress, adaptive coping, and maladaptive coping were 138.16 ± 18.34, 83.85 ±14.02, 21.37 ± 5.79, 53.15 ± 4.64, and 30.98 ± 6.73, respectively. COVID-19-related anxiety was reported by 4.3% of participants. Clinical competency was significantly positively correlated with self-efficacy (r = .44, p < .001) and adaptive coping (r = .20, p = .035) and was significantly negatively correlated with maladaptive coping (r = .20, p = .035). The predictors of clinical competency were self-efficacy (β = .434, p < .001) and adaptive coping (β = .173, p < .039), which explained 23% of the variance in clinical competency.
Conclusion
Self-efficacy and adaptive coping strategies are significant predictors of clinical competence during the pandemic. Planning and implementing various curricular and non-curricular activities to increase senior students' self-efficacy and adaptive coping strategies will help prepare competent nursing graduates for the pandemic when they enter the nursing workforce.
INTRODUCTION
Clinical competence in nursing education refers to the ability to provide desirable nursing skills by synthesizing knowledge, skills, attitudes, and judgments to respond to the needs of nursing recipients in specific nursing practice [1]. Nursing students’ clinical competence is demonstrated by the direct observation and management of health problems exhibited by various patients, along with the performance of nursing tasks in the clinical field [2]. However, the nursing education system is experiencing unprecedented difficulties due to the coronavirus disease 2019 (COVID-19) pandemic, and various restrictions have been imposed on the progress of nursing students’ clinical practice due to fear of infection. Nursing colleges have had to operate simulations in classrooms or virtual spaces, rather than in hospital environments, to avoid infection risk and comply with hospital infection control policies. In this new practice education system, nursing students experience non-face-to-face online practice and meet patients and caregivers virtually to apply the nursing process. Virtual practicum has emerged as a new clinical practice approach for overcoming the difficulties of the pandemic [3]. The teaching methods included a simulation class, virtual simulation, and an online nursing skills program intended to overcome the limitations of clinical practice during the COVID-19 pandemic [3]. However, the ability of nursing students who have experienced online clinical practice to adapt to the clinical environment after graduation remains questionable. Nursing students experience more stress in unfamiliar clinical settings where they encounter chronically and terminally ill patients [4]. During a pandemic, nursing students are exposed to additional stressful factors, such as fear of infection [5].
COVID-19 is a large-scale infectious disease first reported in December 2019 and is a risk factor for the general public and medical personnel. Medical staff experienced COVID-19-related anxiety, depression, and high-intensity work fatigue [6]. Graduating nursing students are the key personnel responsible for important tasks as future healthcare professionals. The transition from student nurse to a graduate nurse is a stressful experience. New graduates undergo a reactionary phase of transition shock that encompasses emotional, physical, socio-developmental, cultural, and emotional changes [7, 8]. These feelings may make new graduates perceive themselves as professionally incompetent, affecting their work performance, adaptation, and employment intention [9, 10]. Graduate nurses’ entry into work life may have been more stressful because of the COVID-19 pandemic. In addition to the usual work-life transition shock, frontline workers may experience profound stress, anxiety, and depression about being a frontline worker [8, 11, 12]. In addition, anxiety and stress may cause negative experiences, such as frustration, tension, and a lack of self-confidence. Anxiety in nursing students can increase stress and reduce clinical competence. Higher instability is reportedly associated with lower clinical competence [9]. During the COVID-19 pandemic, there is a need to help graduate nursing students successfully settle into their jobs as clinical healthcare workers, despite COVID-19-related anxiety [12].
The degree of stress perception varies according to the coping strategy used by an individual [13], and newly graduating nursing students must identify positive coping strategies for use during a pandemic. However, few studies have been conducted on the relationship between COVID-19-related anxiety levels and the clinical competence of nursing students graduating during the pandemic. The extent of perceived clinical stress depends on how nurses think about their abilities. Self-efficacy refers to a personal belief that one can do something well [14]. If self-efficacy is high, a nurse feels motivated and clinically competent and will perform well in difficult situations [15, 16]. If self-efficacy improves during the COVID-19 pandemic, clinical adaptation is expected to improve, and clinical performance is expected to improve.
Nursing students’ clinical competency may be influenced by anxiety [16], stress [17, 18, 19], stress coping [20, 21], and self-efficacy [22, 23]. Greater anxiety and stress related to clinical tasks and occupational hazards can impair nursing students’ clinical performance [24], which, in turn, can compromise patient safety and care [25]. Hence, it would be meaningful to determine the correlations between these variables among nursing students who are about to graduate during the COVID-19 pandemic. In the current context, graduating nursing students constitute a new generation of individuals who have experienced discontinuation of their clinical practice due to COVID-19. There is a need to understand the ability of this new generation of nurses to perform tasks based on their experiences in new educational programs and virtual practice, which differ from the experiences of existing nurses. Therefore, this study attempted to investigate the relationship between COVID-19-related anxiety, coping strategies, self-efficacy, perceived stress, and clinical competency of graduating nursing students during the COVID-19 pandemic and to identify factors affecting nursing students’ clinical competency.
The objectives of this study were:
(1) To assess the levels of self-reported clinical competence, COVID-19 anxiety, perceived stress, coping strategies, and self-efficacy among graduate nursing students.
(2) To identify the correlations between clinical competence, COVID-19 anxiety, perceived stress, coping strategies, and self-efficacy among graduating nursing students.
(3) To identify factors associated with clinical competency among graduating nursing students during the COVID-19 pandemic.
METHODS
1. Study design
A cross-sectional online survey design was used for this study.
2. Sample
Convenience sampling was used to recruit participants from universities located in four major special and metropolitan cities in South Korea based on a similar curriculum. The required sample size was calculated using G-Power version 3.1 with a power of 0.80, an effect size of 0.15, and a level of significance of 0.05. Based on this calculation, the minimum required sample size was 92; thus, 116 participants were considered adequate. The inclusion criteria were students enrolled in a full-time four-year undergraduate nursing program and expected to graduate by the end of the current semester. Students enrolled in 3-year diploma programs were excluded from this study because it was thought that the difference in curriculum may affect the clinical competency of the two groups.
3. Data collection procedure
Data were collected online via surveys using Google Forms in February 2021. All participants were informed about the study aims and procedures in detail, and written consent for voluntary participation was obtained from all participants by asking them to type their full names on the online form. An online coupon for coffee was provided to all participants in appreciation of their time after the survey was completed.
4. Measurement
A general demographic questionnaire was designed.
Clinical competency was assessed using the nursing student clinical competency scale developed by Kim et al. [26]. The 5-point Likert scale included 34 items regarding nursing leadership (12 items), professional development (5 items), nursing skills (5 items), communication (7 items), and the nursing process (5 items). Higher scores indicated higher clinical competency. Cronbach’s alpha for this scale in the original and our study was 0.96.
Self-efficacy was assessed using the general self-efficacy Scale (GSES) developed by Sherer et al. (23 items) [27] and translated by Hong [28]. Responses to each item were provided using a 5-point Likert scale ranging from “never” (1) to “always” (5). Higher total scores indicated better self-efficacy. The Cronbach’s alpha for the Korean version was 0.89, whereas that for the current study was 0.91.
Perceived stress was assessed using the Korean version of the Perceived Stress Scale (10 items) [29, 30]. Each question is scored from 0 (never) to 4 (very often), and the total possible score ranges from 0 to 40. A higher score indicated a higher level of stress. The Cronbach’s alpha for the Korean scale was 0.74, while that for the current study was 0.76.
COVID-19-related anxiety was assessed using a five-item coronavirus anxiety scale (5 items) [31]. Responses were marked on a 5-point scale ranging from 0 (not at all) to 4 (nearly every day over the past two weeks). Scores ≥ 5 indicate clinical anxiety. Cronbach’s alpha for the original scale was 0.72, whereas that for the current study was 0.88.
Coping strategies were assessed using the Korean version of the brief Coping Orientation to Problems Experienced (COPE) scale (28 items) [32, 33]. The brief COPE scale measures coping mechanisms using 14 subscales: self-distraction, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. In accordance with previously published studies, the items from the brief COPE scale were grouped to compute the adaptive coping score (including active coping, planning, use of instrumental support, use of emotional support, positive reframing, acceptance, religion, and humor) and maladaptive coping score (including venting, denial, substance use, behavioral disengagement, self-distraction, and self-blame) [34, 35]. The scale had acceptable internal consistency. In our study, Cronbach’s alpha for the overall scale was 0.79; the internal consistency values for the adaptive and maladaptive subscales were 0.61 and 0.81, respectively.
5. Analysis
Participants’ general characteristics, clinical competency, self-efficacy, perceived stress, adaptive and maladaptive coping, and COVID-19-related anxiety were assessed using descriptive statistics. Differences in clinical competency, self-efficacy, perceived stress, coping (adaptive and maladaptive), and COVID-19-related anxiety were analyzed using an independent t-test, ANOVA, and a post-hoc Scheffé test, according to general demographic characteristics. Correlations were analyzed using Pearson’s correlation test. A stepwise linear multiple regression analysis was conducted to identify the factors affecting clinical competency. All analyses were performed using the IBM SPSS software (version 26.0; IBM Corp., Armonk, NY, USA). p-values < 0.05 were considered statistically significant. The data were checked for normality before analysis using the Kolmogorov-Smirnov and Shapiro-Wilk tests. The significance value for the tests was > 0.05, indicating normal distribution.
6. Ethical consideration
Ethical clearance was obtained from the relevant Woosong University Institutional Review Board (IRB) prior to data collection on 21st January 2021 (IRB approval number 1041549-210105-SB-113). Informed consent was obtained from all participants (via the online method).
RESULTS
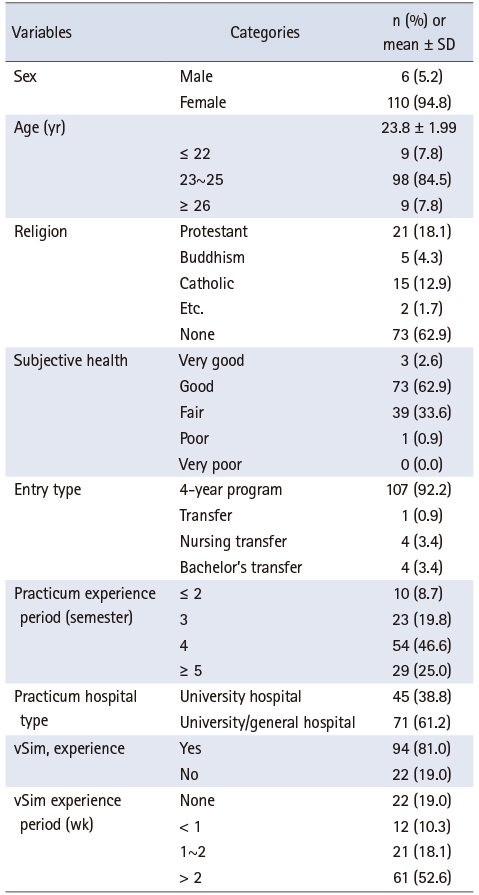
The general characteristics of the study participants are summarized in Table 1. Most respondents were women (94.8%), and the mean age of the participants was 23.8 years (range 22~34 yr). Most participants (92.2%) completed a 4-year bachelor’s degree program. Approximately 47% of the participants had four semesters of clinical experience, while approximately 81% had virtual simulation experience.
Table 1
General Demographic Characteristics
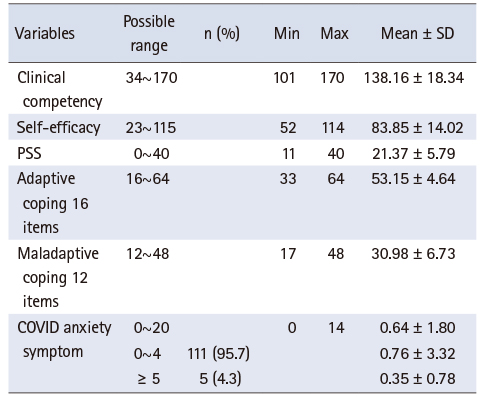
Mean clinical competency, self-efficacy, perceived stress, adaptive and maladaptive coping, and COVID-19-related anxiety scores are shown in Table 2. In our study, 4.3% of the participants reported experiencing COVID-19-related anxiety (cutoff score ≥ 5) (Table 2).
Table 2
Clinical Competency, Self-Efficacy, PSS, Adaptive Coping, Maladaptive Coping, and COVID Symptom
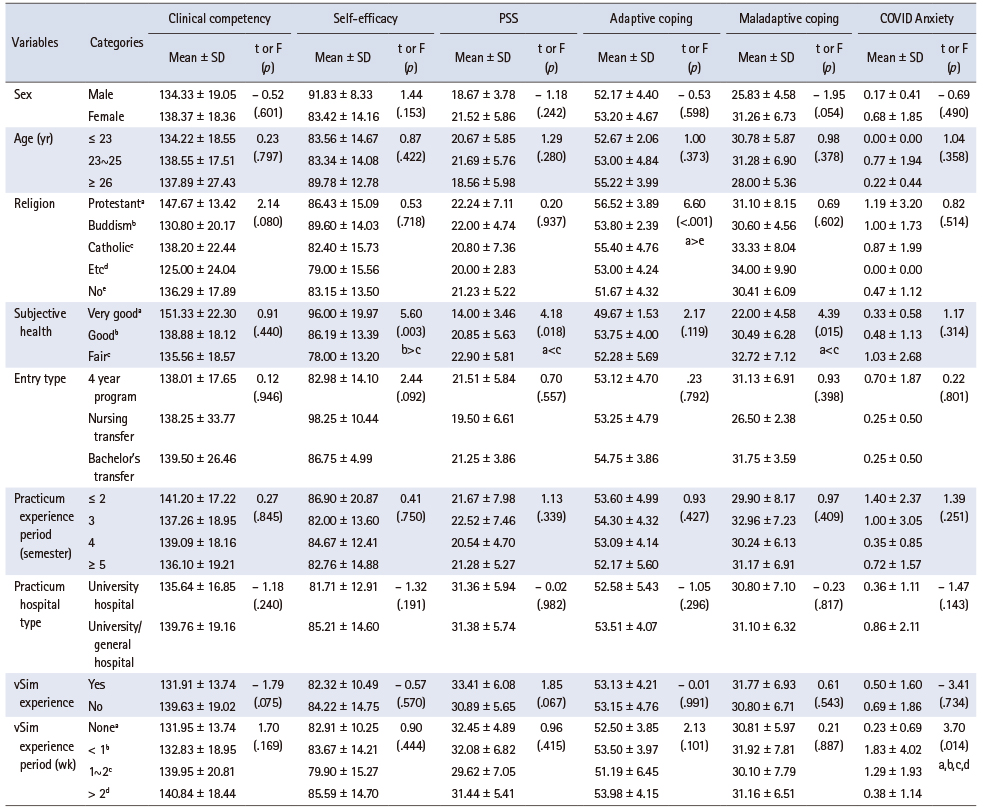
Table 3 shows the differences in clinical competency, self-efficacy, perceived stress, coping (adaptive and maladaptive), and COVID-19-related anxiety according to the general demographic characteristics.
Table 3
Difference of Clinical Competency, Self-Efficacy, PSS, Adaptive Coping, Maladaptive Coping and COVID Symptom according to General Characteristics (N = 116)
No significant differences were observed in the study variables concerning sex, age, type of nursing program completed, clinical experience, or hospital type. Adaptive coping was significantly higher in Christians than non-religious participants (F = 6.60, p < .001).
Significant differences in self-efficacy, perceived stress, maladaptive coping, and COVID-19-related anxiety were observed based on the perceived health status. Participants with “good” perceived health status reported higher self-efficacy than did participants with “fair” perceived health status (F = 5.60, p = .003). Similarly, participants with “very good” perceived health status had significantly less perceived stress (F = 4.18, p = .018) and a lower maladaptive coping score (F = 4.39, p = .015) than did participants with “fair” perceived health status (Table 3). Significant differences in COVID-19 related anxiety were also observed based on the vSim experience period (F = 3.70, p = 0.01). However, the post hoc analysis was not significant (Table 3).
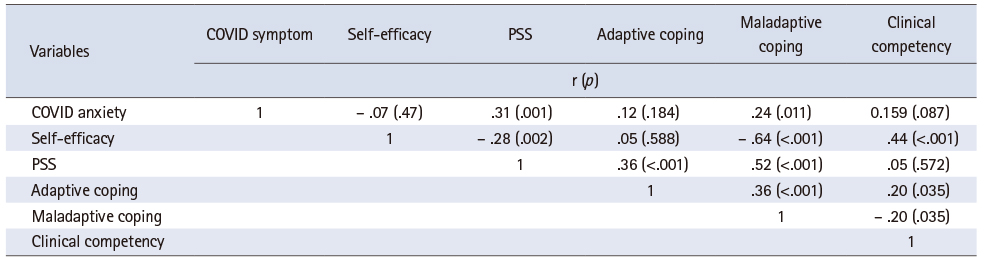
The bivariate correlations among clinical competency, self-efficacy, perceived stress, adaptive coping, maladaptive coping, and COVID-19-related anxiety are shown in Table 4. Clinical competency was significantly positively correlated with self-efficacy (r = .44, p < 0.001) and adaptive coping (r = .20, p = .035); it was significantly negatively correlated with maladaptive coping (r = -.20, p = .035). Self-efficacy and maladaptive coping were also significantly and negatively correlated (r = -.64, p < 0.001). COVID-19-related anxiety significantly correlated with perceived stress (r = .31, p = .011) and maladaptive coping (r = .24, p = .011) (Table 4).
Table 4
Correlation between Study Variables (N = 116)
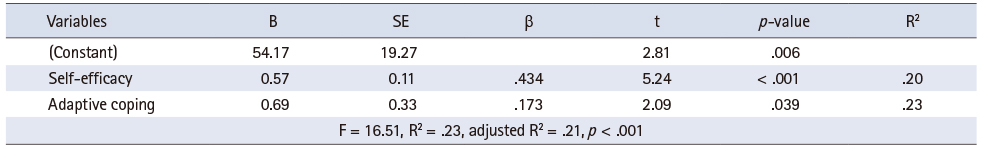
Stepwise multiple regression analysis was conducted to identify factors affecting clinical competency. Variables that were significantly correlated with clinical competency (i.e., self-efficacy and adaptive and maladaptive coping) were added to the regression model. The Durbin-Watson test was used to check for autocorrelation, which was close to 2 (2.097), indicating no autocorrelation. The tolerance limit was .99, and the variance inflation factor was 1.003, both within the cutoff points (tolerance < 1, variance inflation factor < 10), indicating no multicollinearity. The variables that had a significant effect on clinical competency were self-efficacy (β = .434, p < .001) and adaptive coping (β = .173, p < .039). The nursing students’ clinical competency increased with greater self-efficacy and adaptive coping. These variables explained 23.0% of the variance in clinical competency among nursing students, with self-efficacy explaining 20.0% of the variance and having the greatest influence on clinical competency (Table 5).
Table 5
Factors Affecting to Clinical Competency (Stepwise Regression) (N = 116)
DISCUSSION
This study aimed to assess the clinical competency of graduating student nurses during the COVID pandemic and identify factors associated with clinical competency. We found that 4.3% of the participants had COVID-related anxiety, which was lower than the proportion reported in previous studies [5]. This is potentially because our data were collected before the fourth wave of the pandemic, which was related to the delta variant in South Korea. Additionally, in contrast to previous studies that included nursing students at all levels, our study participants were senior graduate students; thus, they had almost completed the required education and clinical training (equivalent to 1,000 h) to become licensed registered nurses. High-proficiency students tended to experience less anxiety and stress [36].
Our results show that participants who perceived their health status as “good” or “very good” had higher self-efficacy, lower perceived stress, and a lower maladaptive coping score. This suggests that methods to improve perceived health status, such as providing adequate physical and psychological institutional support and promoting self-compassion, must be integral components when planning pandemic preparedness for nursing students [37]. Although there was no cutoff score for the brief COPE scale, the mean adaptive coping scores of the participants were generally high in our study. This finding is similar to the results reported by Baluwa et al. [38] and Nebhinani et al. [39]; however, their study included nursing students enrolled between years one and four. Although other factors may be involved, a high mean adaptive score was a positive finding in our study. This indicates the potential psychological strength that should be further enhanced by interventions such as problem-solving, self-care, and stress management workshops tailored to this group of students.
Self-efficacy and adaptive coping were significant predictors of clinical competency. Self-efficacy and coping strategies have been extensively reported in previous studies of nursing students [40, 41]. Our study further emphasizes self-efficacy and the use of adaptive coping strategies, such as planning, active coping, instrumental support, positive reframing, and humor, which benefit prospective graduates psychologically by neutralizing their anxiety and stress while helping them become more clinically competent and prepared to take on the healthcare provider role during a pandemic. Although the mode of instruction has changed to an online or hybrid method worldwide due to the pandemic, nurse educators should design a curriculum with opportunities for high-fidelity online simulations to enhance the self-efficacy of graduating students. Furthermore, educators must create more opportunities for open-guide discussions on self-reflection and debriefing sessions to help students identify their psychological reactions to the pandemic and promote healthy coping strategies [40, 41, 42]. Because specific coping strategies are often adopted habitually throughout life or during healthcare provision, it is important to plan methods to enhance adaptive coping strategies during the training period, which will facilitate the establishment of a healthy and competent workforce prepared for a pandemic.
Self-efficacy has a direct and mediating effect on nursing performance among clinical [16] and student nurses [43]. Self-efficacy is an important factor for student nurses to successfully translate their education and training into practice when they become registered nurses. Students often feel unprepared for practice [44, 45]. A practice-oriented educational experience is recommended to facilitate the smooth transition of students into practice [9]; however, the pandemic hindered this experience. Students have limited opportunities to practice and learn in a real clinical environment, which may make them unprepared for practice. Our findings emphasize that promoting self-efficacy through curricular and non-curricular activities is an integral part of nursing education. Because clinical competency is a multidimensional concept [46], nursing programs must include self-efficacy enhancement educational strategies for all components, such as academic education and nursing skills, leadership, critical thinking, clinical decision-making, and communication. This approach can best be accomplished by providing real practice and work opportunities early in the nursing career [47]. Similarly, various refresher courses, internships, and orientation programs that provide opportunities to develop self-efficacy and promote adaptive coping must be established as common practices, aiding in smooth transitions and reducing the intention to quit among new nurses.
Limitations
Our study has some limitations. First, it used a cross-sectional design, which hindered assessing causal relationships among the study variables. The internal consistency of the adaptive coping subscale was moderate (0.61). Future studies should be conducted using additional instruments to assess adaptive coping to confirm its reliability. Third, there may have been a survey response bias from the participants because the survey used a self-reported online format.
CONCLUSION
This study expands our knowledge of factors affecting the clinical competence of graduating nursing students. Our study showed that self-efficacy and adaptive coping strategies were significant predictors of clinical competence even during the COVID-19 pandemic. Because the methods of instruction delivery and clinical practice are affected by the pandemic, nurse educators should plan strategies to increase self-efficacy and adaptive coping strategies among senior students through various curricular and non-curricular activities so that competent nursing graduates will be “pandemic-ready” when they enter the workforce.
CONFLICTS OF INTEREST:The authors declared that no conflict of interest.
FUNDING:This study was supported by Woosong University Research Grant.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Chung SK & Kim JS & Bhandari P.
Data curation or/and Analysis: Chung SK & Kim JS & Bhandari P.
Funding acquisition: Chung SK.
Investigation: Chung SK & Kim JS & Bhandari P.
Project administration or/and Supervision: Chung SK & Kim JS & Bhandari P.
Resources or/and Software: Chung SK & Kim JS & Bhandari P.
Validation: Chung SK & Kim JS & Bhandari P.
Visualization: Chung SK & Kim JS & Bhandari P.
Writing original draft or/and review & editing: Chung SK & Kim JS & Bhandari P.
ACKNOWLEDGEMENTS
The authors are grateful to all the students who took the time to participate in this study.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: A comparison with the general population. International Journal of Environmental Research and Public Health 2020;17(18):6550 [doi: 10.3390/ijerph17186550]
-
-
Järvinen T, Eklöf N, Salminen L. Factors related to nursing students’ readiness to enter working life - a scoping literature review. Nurse Education in Practice 2018;29:191–199. [doi: 10.1016/j.nepr.2018.01.010]
-
-
Urban RW, Rogers MR, Eades TL, Allard PM, Porter MT, Cipher DJ. Resilience, stress, anxiety, and depression: Exploring the mental health of new graduate nurses transitioning to practice during COVID-19. The Journal of Continuing Education in Nursing 2022;53(12):533–543. [doi: 10.3928/00220124-20221107-05]
-
-
Jeong YJ, Koh CK. Effects of personality and coping behavior on clinical practice stress among one college nursing students. The Korean Journal of Stress Research 2016;24(4):296–302. [doi: 10.17547/kjsr.2016.24.4.296]
-
-
Bandura A. In: Social foundations of thought and action: A social cognitive theory. Englewood Cliffs (NJ): Prentice Hall; 1986. pp. 94.
-
-
Jo MJ, Sung MH. Impact of role conflict, self-efficacy, and resilience on nursing task performance of emergency department nurses. Korean Journal of Occupational Health Nursing 2018;27(1):59–66. [doi: 10.5807/kjohn.2018.27.1.59]
-
-
Kim EH. Relationship of anxiety, empathy, ego-resilience and clinical competency in nursing students. Journal of the Korea Contents Association 2018;18(8):326–337. [doi: 10.5392/JKCA.2018.18.08.326]
-
-
Song Y, Lee JY. Effects of clinical practice stress and moral sensitivity on clinical competency in nursing students. The Journal of Korean Academic Society of Nursing Education 2020;26(2):157–166. [doi: 10.5977/jkasne.2020.26.2.157]
-
-
Yu HS. Relationship among stress of clinical practice, practice satisfaction and clinical competence in nursing students. Journal of the Korean Data Analysis Society 2015;17(2):1129–1144.
-
-
Lee KE, Hong JY. Effects of empathy, caring efficacy and stress coping on clinical competence in nursing students. The Journal of Learner-Centered Curriculum and Instruction 2020;20(24):1251–1270. [doi: 10.22251/jlcci.2020.20.24.1251]
-
-
Kim SM, Hwang TY. Comparison of stress levels arising in clinical settings, stress coping mechanisms and clinical competency between male and female nursing students. The Journal of Korean Academic Society of Nursing Education 2014;20(4):606–616. [doi: 10.5977/jkasne.2014.20.4.606]
-
-
Yang SY. The effect of emotional intelligence and self-efficacy on clinical competence of the nursing students. Journal of the Korea Contents Association 2015;15(6):370–378. [doi: 10.5392/JKCA.2015.15.06.370]
-
-
Kim YS. The effects of clinical practice stress, grit and self-efficacy on clinical competency in nursing students. Journal of the Korea Contents Association 2022;22(9):451–460. [doi: 10.5392/JKCA.2022.22.09.451]
-
-
Apisarnthanarak A, Apisarnthanarak P, Siripraparat C, Saengaram P, Leeprechanon N, Weber DJ. Impact of anxiety and fear for COVID-19 toward infection control practices among Thai healthcare workers. Infection Control & Hospital Epidemiology 2020;41(9):1093–1094. [doi: 10.1017/ice.2020.280]
-
-
Kim BY, Chae MJ, Choi YO. Reliability and validity of the clinical competency scale for nursing students. Journal of Korean Academy of Community Health Nursing 2018;29(2):220–230. [doi: 10.12799/jkachn.2018.29.2.220]
-
-
Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self-efficacy scale: Construction and validation. Psychological Reports 1982;51(2):663–671. [doi: 10.2466/pr0.1982.51.2.663]
-
-
Hong H. In: The relationship of perfectionism, self-efficacy and depression [master’s thesis]. Seoul: Ewha Womans University; 1995. pp. 1-73.
-
-
Kim Y, Seidlitz L. Spirituality moderates the effect of stress on emotional and physical adjustment. Personality and Individual Differences 2002;32(8):1377–1390. [doi: 10.1016/S0191-8869(01)00128-3]
-
-
Meyer B. Coping with severe mental illness: Relations of the brief COPE with symptoms, functioning, and well-being. Journal of Psychopathology and Behavioral Assessment 2001;23(4):265–277. [doi: 10.1023/A:1012731520781]
-
-
Shahsavari H, Ghiyasvandian S, Houser ML, Zakerimoghadam M, Kermanshahi SSN, Torabi S. Effect of a clinical skills refresher course on the clinical performance, anxiety and self-efficacy of the final year undergraduate nursing students. Nurse Education in Practice 2017;27:151–156. [doi: 10.1016/j.nepr.2017.08.006]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

