Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 53(1); 2023 > Article
- Research Paper Factors Affecting the Quality of Life in Low-Income Older Adults with Sarcopenia: A Cross-Sectional Study
- Ju-Hee Nho, Eun Jin Kim
-
Journal of Korean Academy of Nursing 2023;53(1):1-11.
DOI: https://doi.org/10.4040/jkan.22126
Published online: February 28, 2023
2Research Institute of Nursing Science, Jeonbuk National University, Jeonju, Korea
-
Corresponding author:
Eun Jin Kim,
Email: jhnho@jbnu.ac.kr
Abstract
Purpose
This study aimed to identify the factors influencing quality of life (QoL) of low-income older adults (LOAs) with sarcopenia.
Methods
A convenience sample of 125 older adults was recruited from Jeonbuk Province, South Korea. Data were collected using a self-report questionnaire that included nutritional status, the Depression Anxiety Stress Scale-21, and the World Health Organization Quality of Life Instrument-Older Adults Module. Additionally, grip strength and appendicular skeletal muscle mass, were evaluated, along with the short physical performance battery.
Results
Sarcopenia and severe sarcopenia were observed in 43.2% and 56.8% of participants, respectively. Using multiple regression analysis, depression (β = - .40, p < .001), nutritional status (β = .24, p = .003), and anxiety (β = - .15, p = .042) were identified as factors affecting the QoL of the older adults in low-income groups with sarcopenia, the explanatory power of these variables was 44%.
Conclusion
The results of this study can be used to develop a nursing intervention program and establish policies to improve depression, anxiety, and nutritional status to enhance QoL of LOAs with sarcopenia.
Published online Feb 28, 2023.
https://doi.org/10.4040/jkan.22126
Factors Affecting the Quality of Life in Low-Income Older Adults with Sarcopenia: A Cross-Sectional Study
Abstract
Purpose
This study aimed to identify the factors influencing quality of life (QoL) of low-income older adults (LOAs) with sarcopenia.
Methods
A convenience sample of 125 older adults was recruited from Jeonbuk Province, South Korea. Data were collected using a self-report questionnaire that included nutritional status, the Depression Anxiety Stress Scale-21, and the World Health Organization Quality of Life Instrument-Older Adults Module. Additionally, grip strength and appendicular skeletal muscle mass, were evaluated, along with the short physical performance battery.
Results
Sarcopenia and severe sarcopenia were observed in 43.2% and 56.8% of participants, respectively. Using multiple regression analysis, depression (β = -.40, p < .001), nutritional status (β = .24, p = .003), and anxiety (β = -.15, p = .042) were identified as factors affecting the QoL of the older adults in low-income groups with sarcopenia, the explanatory power of these variables was 44%.
Conclusion
The results of this study can be used to develop a nursing intervention program and establish policies to improve depression, anxiety, and nutritional status to enhance QoL of LOAs with sarcopenia.
INTRODUCTION
The proportion of older adults in Korea has increased from 15.7% in 2020 to 16.5% in 2021 and is expected to rise to 20.3% by 2025 [1]. Sarcopenia progresses with age, wherein grip strength and muscle mass decrease due to physiological changes in the body [2, 3]. With an increasingly aging population, it is estimated that approximately 700,000~1 million older adults in Korea will suffer from sarcopenia [4]. The global prevalence of sarcopenia is 10%~27% and the prevalence of severe sarcopenia is 2%~9% [4]. The prevalence of sarcopenia among the older population living in local communities in Korea is 15%~23.7% [5, 6], while the prevalence of severe sarcopenia is 3.2%~6.4% [7]. This is aligned with the global trends in sarcopenia prevalence. Sarcopenia is a major geriatric problem that is closely related to other diseases (e.g., diabetes, cancer, hip fracture); it affects the quality of life (QoL) and survival rate and dramatically increases medical and long-term care costs [4]. Therefore, sarcopenia in older adults requires greater attention and should be carefully assessed.
Sarcopenia affects the performance of activities of daily living owing to physiological problems and physical disabilities [8]. An examination of the relationship between sarcopenia and cognitive impairment in older women revealed that the prevalence of cognitive impairment in older women with sarcopenia was 5.4 times higher than that in women without sarcopenia. Moreover, sarcopenia severity was found to be a determinant of cognitive impairment [9]. Compared to the control group without sarcopenia, older adults with sarcopenia had a 2.5 times higher risk of falling due to lower muscle strength, aerobic endurance, lower extremity flexibility, agility, and dynamic balance [6]; they were also significantly associated with the incidence of mortality [5].
The QoL of older adults with sarcopenia is much lower than that of older adults without sarcopenia [10]. Moreover, older adults with symptoms of sarcopenia have lower QoL in the areas of physical and mental health, exercise, body composition, activities of daily living, and decreased strength and muscle mass [2]. Older women who have had a fall and have been diagnosed with sarcopenia tend to have reduced QoL [11].
The predictors of sarcopenia include age, disease characteristics (cancer, hypertension, and asthma), occupation [12], weight, body mass index, skeletal muscle mass [6], lack of activity [5], sedentary lifestyle [8], poor nutritional status, malnutrition risk, rural residence, and number of medications [13]. Nutritional status is often associated with health problems in older adults [14]. Older adults with sarcopenia often consume an unhealthy diet, such as one including insufficient protein [8]. Malnutrition in older people reduces QoL as their health deteriorates [15]. In particular, older adults with sarcopenia have remarkably low protein intake and QoL [16]. Therefore, it is necessary to evaluate the relationship between nutritional status and QoL in older adults with sarcopenia.
A previous study has identified an association between sarcopenia and psychological health, including issues such as depression, anxiety, and stress [10]. The severity of sarcopenia was found to be inversely proportional and significantly related to depression [9], with individuals with sarcopenia being highly vulnerable to anxiety and stress factors [17].
Low-income older adults (LOAs) are more likely to be exposed to factors that harm health; such exposure weakens their ability to cope with these risk factors in the future, which makes them susceptible to physical and mental health issues [18]. As they have a low socioeconomic status [19], they are affected by frequent malnutrition [20], depression as a result of prevalent physical health problems [18], and anxiety owing to concerns about social isolation and loneliness [21]. Stress is one of the main factors affecting the health of older adults. Elevated cortisol levels in stressful situations cause sarcopenia [22] and stress adversely affects metabolism, resulting in unhealthy behaviors and reduced QoL [23].
Recently, in Korea, interest in geriatric sarcopenia has increased, and research is being actively conducted [12]; however, there is no study on the factors affecting QoL of older adults with sarcopenia in the low-income category. Therefore, it is important to develop strategies to improve QoL by identifying factors that affect QoL of LOAs with sarcopenia.
The purpose of this study was to (1) identify the general characteristics, nutritional status, depression, anxiety, stress, and QoL of LOAs with sarcopenia; (2) reveal the nutritional status, depression, anxiety, stress, and QoL according to the general characteristics of LOAs with sarcopenia; (3) investigate the correlation between nutritional status, depression, anxiety, stress, and QoL of LOAs with sarcopenia; and (4) determine the factors influencing QoL in low-income groups with sarcopenia.
METHODS
1. Research design
Employing a cross-sectional design, this descriptive correlational study aimed to understand the general characteristics of LOAs with sarcopenia and the factors affecting their QoL.
2. Participants and data collection
The participants of this study were older adults (over 65 years of age) with sarcopenia in the low-income group living in rental apartments for low-income people in Jeonbuk Province. The inclusion criteria were: (1) adults older than 65 years; (2) those who satisfied the criteria for sarcopenia; (3) those who could measure grip strength and appendicular skeletal muscle mass (ASM) or perform strength training; and (4) those who could read and understand Korean. The exclusion criteria were as follows: (1) those who had been diagnosed with dementia or cognitive problems and (2) those who were bedridden or had difficulty moving due to physical problems. Regarding the sample size estimation for multiple regression analysis, G*Power 3.1.9.7 was used and a significance level of .05, power of .8. The effect size of .20 was based on a previous study that investigated the relationship between clinical variables and QoL in older adults with sarcopenia [11]. When 13 predictors (general characteristics, nutritional status, depression, anxiety, and stress) were entered, a minimum sample size of 101 was determined. Considering the non-response rate, data were collected from 150 participants. A total of 125 (response rate 83.3%) participants were included in the final analysis, excluding 25 owing to factors such as hemiplegia, prosthetic leg, need for a wheelchair assistant, and absence of sarcopenia.
Data were collected from November 11, 2021 to June 10, 2022 using convenience sampling. After obtaining consent from the participants and the director of the apartment manager, two trained research assistants administered a self-report questionnaire and evaluated their physical performance. To ensure readability, if a participant requested, the research assistants read the questionnaire verbatim and helped complete it, thereby ensuring reliability of data collection. Considering the participant’s safety (e.g., fall down), two research assistants measured the data for one older adult. Moreover, the research assistants helped or supported the participants in mobility to ensure that they could be evaluated in a safe environment during data collection. After completing the data collection, household goods were presented to the participants as compensation for participation.
3. Measurement
1) General characteristics
The general characteristics included age, sex, one-person household, education, religion, subjective health status, physical discomfort, disease, and sarcopenia severity (severe sarcopenia and sarcopenia).
2) Sarcopenia
Based on the criteria of the Asian Working Group for Sarcopenia (AWGS), the algorithm for sarcopenia and severe sarcopenia comprises handgrip strength (HGS), short physical performance battery (SPPB), and ASM [3, 24]. The cutoff values for HGS were < 28 kg and < 18 kg for male and female, respectively. The cutoff scores for SPPB were ≤ 9 points for both male and female. The cut-off values for ASM were < 7.0 kg/m2 for male and < 5.7 kg/m2 for female. Sarcopenia was determined by low ASM along with either low HGS or low SPPB; moreover, severe sarcopenia was characterized by low ASM along with both low HGS and low SPPB [3, 24].
HGS was measured using a grip dynamometer (TKK5401®; Takei, Niigata, Japan), with proven reliability and validity [25]. A trained research assistant seated the participant in a chair without raising their arm on the handle of the chair. When holding the dynamometer, the elbow was flexed at 90° so that the second joint of the finger was held at a right angle. Providing a gap of 60 seconds between flexing the right and left hand, HGS was measured twice in this manner, and the maximum value among the measured values was used.
ASM was measured using a body composition analyzer (Inbody 270®; Biospace, Seoul, Korea) that uses bioelectrical impedance analysis of touch-type electrical stimulation. The accuracy of this device was 93%~96% for the measurement of muscle, fat, and body water [26]. After urination with an ASM body composition analyzer, the participant was required to wear light clothes, take off socks, and measure while standing. ASM is calculated as the skeletal muscle mass divided by the square of the height.
The SPPB consists of a balance test (side-by-side stand, semi-tandem stand, and tandem stand), gait speed test of 4 m, and five repeated chair stands [3]. For both the side-by-side stand and the semi-tandem stand, 1 point was recorded if held for 10 seconds and 0 points if not held for 10 seconds or not attempted. The tandem stand was scored as 2 points if held for 10 seconds, 1 point for 3~9.99 seconds, and 0 points for < 3 seconds or no attempts [3]. The gait speed test of 4 m was scored as 4 points if the duration was < 4.82 seconds, 3 points for 4.8~6.2 seconds, 2 points for 6.2~8.7 seconds, 1 point for more than 8.7 seconds, and 0 points if the participant was unable to do the walk [3]. The five repeated chair stands were scored as 4 points if the chair stand time was less than 11.2 seconds, 3 points for 11.2~13.69 seconds, 2 points for 13.7~16.7 seconds, 1 point for > 16.7 seconds, and 0 points for > 60 seconds. Therefore, the total SPPB score ranged from 0 to 12 points, and the cutoff was 9 points [3].
3) Nutritional status
The nutritional status of older adults was measured using the 17-item nutritional survey for older adults. It was developed for older adults and includes factors such as protein/fruit/milk food intake, eating behavior, age, household type, pocket money, education, age, and related diseases. Of the 17 questions, 6 were out of 2 points and 11 were out of 1 point, with a total score ranging from 0 to 23. Higher scores indicate a lower nutritional risk. At the time of development, the sensitivity, specificity, and positive predictive value were 75.6%, 100%, and 100%, respectively [14]. Scores were classified as follows: 0~11, 12~16, and 17~23 for high, moderate, and low risk of malnutrition, respectively [14].
4) Depression, anxiety, and stress
Depression, anxiety, and stress were measured using the Depression Anxiety Stress Scale (DASS-21) [27]. DASS-21 was developed by Henry and Crawford [27], and its Korean version [28] was used in this study. DASS-21 is a simplified form of the 42 items from the DASS tools. Depression is characterized by low positivity, low self-esteem and motivation, and feelings of hopelessness. Anxiety is assessed by questions about automatic arousal and fear, such as dry mouth, rapid heartbeat, and stress, which represent constant tension, irritability, and negative emotions, respectively. Each domain consists of seven items measured on a 4-point Likert scale; the higher the score, the more severe the degree of depression, anxiety, and stress [27]. The cut-off scores for depression, anxiety, and stress were ≥ 10 points, ≥ 8 points, and ≥ 15 points, respectively [27]. In this study, depression, anxiety, and stress were used separately [29]. At the time of development of this tool, the total Cronbach’s α was .95 [27]. In this study, Cronbach’s α for depression, anxiety, and stress were .83, .71, and .82, respectively.
5) Quality of life
QoL was measured using the Korean version of the World Health Organization Quality of Life Instrument-Older Adults Module (WHOQOL-OLD) [30]. This multidimensional tool measures the QoL of older adults in the WHOQOL group and consists of 24 items divided into six sub-domains (sensory abilities, autonomy, death and dying, past and present and future activities, social participation, and intimacy). It uses a 5-point Likert scale, with higher scores indicating a higher QoL. In the study by Kim et al. [30], the reliability coefficient was Cronbach’s α = .90, and the reliability coefficients of each sub-domain were as follows: .89 for sensory abilities, .80 for autonomy, .89 for death and dying, .77 for past and present and future activities, .81 for social participation, and. 86 for intimacy [30]. In this study, Cronbach’s α was .89, and Cronbach’s α for the sub-domains were as follows: .95 for sensory abilities, .76 for autonomy, .95 for death and dying,.73 for past and present and future activities, .79 for social participation, and .93 for intimacy.
4. Ethical consideration
This study was conducted after obtaining approval (IRB no. 2021-07-012-002) from the Institutional Review Board of Jeonbuk National University, and confidentiality and anonymity were ensured as personal information of the participants was not collected. All participants provided informed consent for participation in the study.
5. Statistical analysis
The participants with sarcopenia were selected according to the AWGS algorithm, and the data were analyzed. The collected data were analyzed using SPSS WIN 25.0 (IBM Corp., Armonk, NY, USA). Participants’ general characteristics and the variables were analyzed using descriptive statistics. An independent test and one-way analysis of variance were conducted to compare differences in depression, anxiety, stress, and QoL according to participants' general characteristics. Pearson’s correlation analysis was performed to investigate the correlations between nutritional status, depression, anxiety, stress, and QoL. Hierarchical multiple regression analysis was used to identify the factors affecting QoL of LOAs with sarcopenia.
RESULTS
1. Participants’ general characteristics
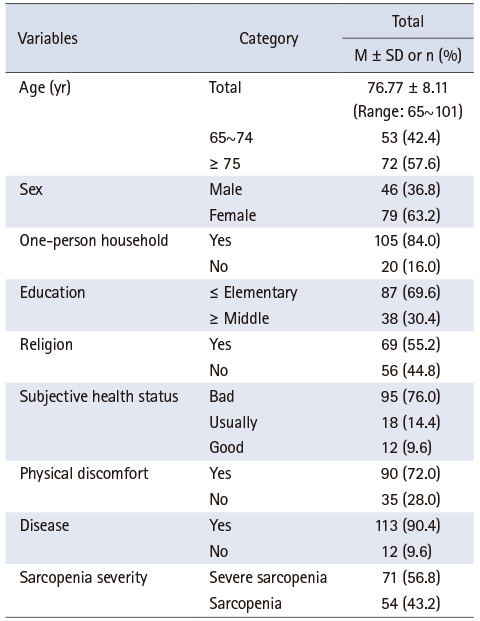
Table 1 presents the participants’ general characteristics. The mean age of the participants was 76.8 years old, and 57.6% were 75 years or older. Among them, 63.2% were female, and 84.0% were one-person households. A total of 76.0% of participants reported that their subjective health status was ‘bad.’ Of the participants, 72.0% had physical discomfort, and 90.4% had a diagnosed disease. When classified according to the AWGS sarcopenia criteria [8], 56.8% had severe sarcopenia and 43.2% had sarcopenia (Table 1).
Table 1
General Characteristics of Participants (N = 125)
2. Participants’ nutritional status, depression, anxiety, stress, and QoL
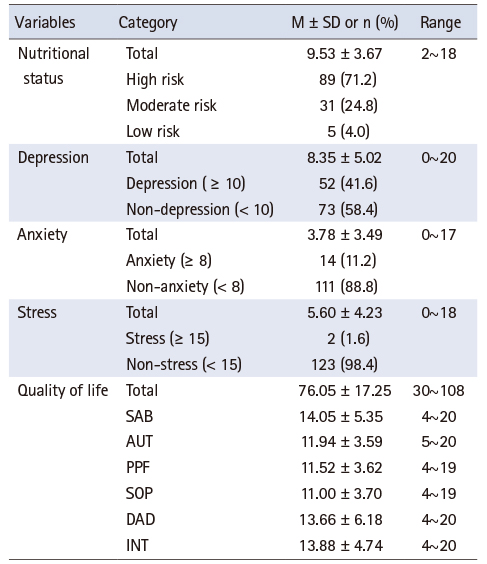
Table 2 presents the levels of the participants’ nutritional status, depression, anxiety, stress, and QoL. The average nutritional status score of these participants was 9.53 ± 3.67, and in terms of the risk of nutritional status, 71.2% were at high risk, 24.8% were at moderate risk, and 4.0% were at low risk. The scores for depression, anxiety, and stress were 8.35 ± 5.02, 3.78 ± 3.49, and 5.60 ± 4.23, respectively. The prevalence rates of depression, anxiety, and stress were 41.6%, 11.2%, and 1.6%, respectively. The mean score for QoL was 76.05 ± 17.25, and the scores for the subdomains were as follows: sensory ability, 14.05 ± 5.35; autonomy, 11.94 ± 3.59; death and dying, 13.66 ± 6.18; past, present, and future activity, 11.52 ± 3.62; social participation, 11.00 ± 3.70; and intimacy, 13.88 ± 4.74 (Table 2). In this study, the major variables of nutritional status, depression, anxiety, stress, and QoL were all normally distributed, as skewness and kurtosis were within the absolute value of 2.
Table 2
Nutritional Status, Depression, Anxiety, Stress, and Quality of Life (N = 125)
3. Nutritional status, depression, anxiety, stress, and QoL according to general characteristics
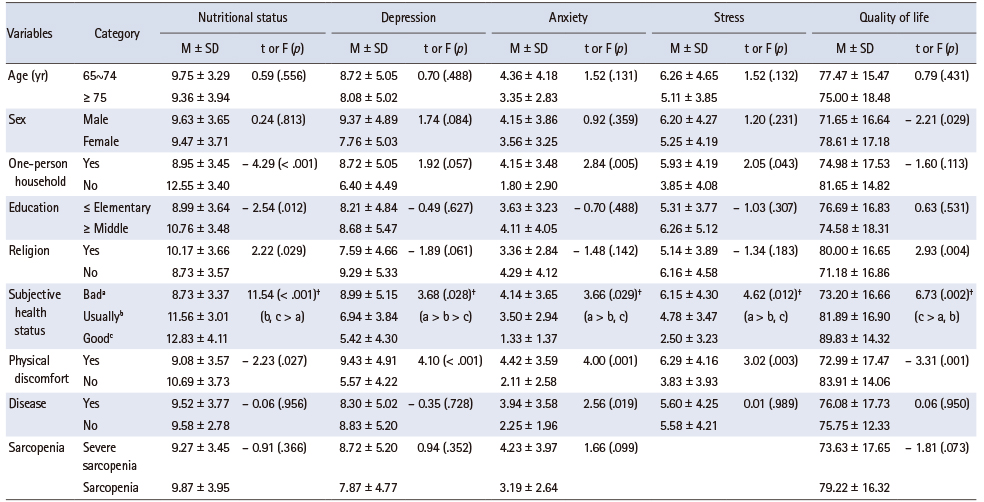
Table 3 shows nutritional status, depression, anxiety, stress, and QoL according to general characteristics. Nutritional status showed a difference according to one-person households (t = - 4.29, p < .001), education (t = - 2.54, p = .012), religion (t = 2.22, p = .029), subjective health status (F = 11.54, p < .001), and physical discomfort (t = - 2.23, p = .027). Depression showed a difference according to subjective health status (F = 3.68, p = .028) and physical discomfort (t = 4.10, p < .001). Anxiety showed a difference according to one-person households (t = 2.84, p = .005), subjective health status (F = 3.66, p = .029), and physical discomfort (t = 4.00, p = .001). Stress showed a difference according to one-person households (t = 2.05, p = .043), subjective health status (F = 4.62, p = .012), and physical discomfort (t = 3.02, p = .003). QoL showed a difference according to sex (t = - 2.21, p = .029), religion (t = 2.93, p = .004), subjective health status (F = 6.73, p = .002), and physical discomfort (t = - 3.31, p = .001) (Table 3).
Table 3
Nutritional Status, Depression, Anxiety, Stress, and Quality of Life according to General Characteristics (N = 125)
4. Correlation of variables
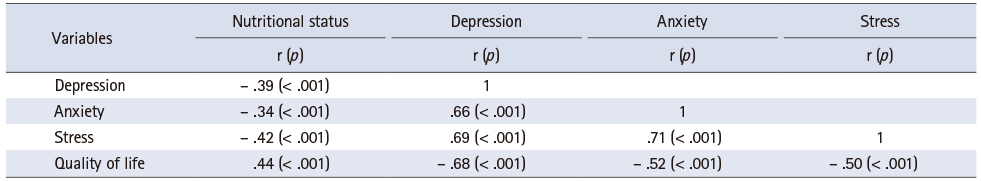
Table 4 shows the correlations between the variables. The higher the nutritional status score, the lower the scores for depression (r = -.39, p < .001), anxiety (r = -.34, p < .001), and stress (r = -.42, p < .001) and the higher the QoL score (r = .44, p < .001). The higher the depression score, the higher the scores for anxiety (r = .66, p < .001) and stress (r = .69, p < .001) and the lower the QoL score (r = -.68, p < .001). The higher the anxiety score, the higher the stress score (r = .71, p < .001) and the lower the QoL score (r = -.52, p < .001). Finally, the higher the stress score, the lower the QoL score (r = -.50, p < .001) (Table 4).
Table 4
Correlation among Nutritional Status, Depression, Anxiety, Stress, and Quality of Life (N = 125)
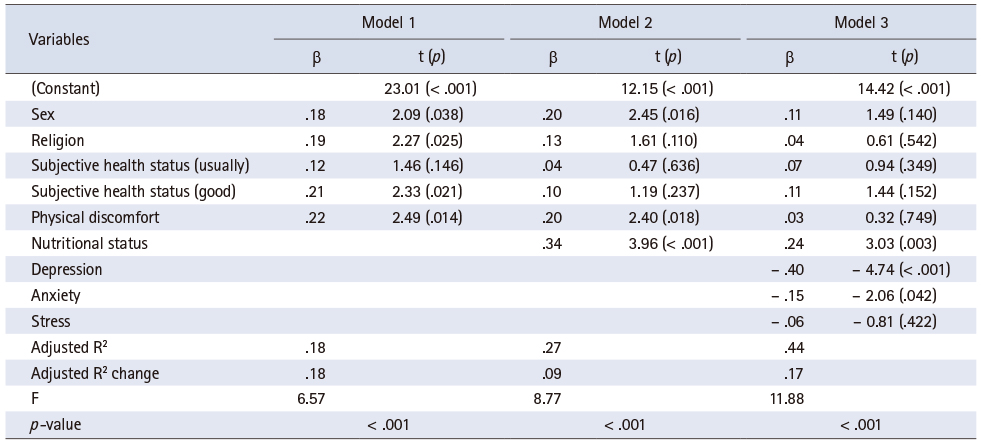
5. Factors influencing the QoL of vulnerable older adults with sarcopenia
Table 5 presents the factors influencing QoL of LOAs with sarcopenia. Previous studies have hierarchically input general characteristics, nutritional status, and psychological characteristics [26]. In this study, general characteristics (sex, religion, subjective health status, and physical discomfort) with significant differences in participants’ QoL were entered in the first model; nutritional status, in the second model; and depression, anxiety, and stress were treated as dummy variables in the third model. The result of confirming the assumptions of regression analysis for independent variables before performing hierarchical regression analysis to confirm the influence on the participants’ QoL, the Durbin–Watson index was 1.840, indicating that there was no autocorrelation. Tolerance was 0.64 to 0.95, which was more than 0.10, and the variance inflation factor (VIF) values were 1.05 to 1.55, which was less than 10, thereby confirming that there was no multicollinearity.
Table 5
Factors Affecting the Quality of Life (N = 125)
Model 1 showed that the general characteristics explained 18.0% of the variance in QoL in LOAs with sarcopenia. In Model 2, nutritional status (β = .34, p < .001) significantly influenced QoL, and explanatory power increased from 9.0% to 27.0%. In Model 3, depression (β = -.40, p < .001) and anxiety (β = -.15, p = .042) significantly influenced QoL, and the explanatory power increased from 17.0% to 44.0%. The total explanatory power of QoL of LOAs with sarcopenia was 44.0% in the hierarchical regression model (F = 11.88, p < .001). In this study, a low depression score (β = -.40, p < .001), high nutritional status score (β = .24, p = .003), and low anxiety score (β = -.15, p = .042) influenced the QoL of LOAs with sarcopenia (Table 5).
DISCUSSION
In this study, the QoL of LOAs with sarcopenia was significantly lower than that of healthy older adults [31, 32]. The QoL of LOAs with sarcopenia in this study was low, possibly due to low income, lack of surrounding resources, and lack of support systems. In a cohort study of older adults in Korea, muscle strength loss was highly correlated with physical function decline after five years [2], thereby reducing QoL and leading to mortality [4]. Thus, efforts are needed to improve the QoL of LOAs with sarcopenia.
In this study, the variables that significantly affected the QoL of LOAs with sarcopenia were sex, religion, subjective health status, and physical discomfort. These results are similar to those of a previous study [18], in which gender, subjective health status, body mass index, daily living performance, depression, and social support were identified as variables that significantly affected the QoL of LOAs. Therefore, national and policy efforts are needed to improve QoL in LOAs. In this study, depression, nutritional status, and anxiety were identified as factors influencing the QoL of LOAs with sarcopenia. These factors are discussed in descending order of influence as follows.
In this study, the depression score of LOAs with sarcopenia was 8.35, which was higher than the mean score of 5.12 [33] for older adults in general. Additionally, the variables affecting depression were subjective health status and physical discomfort, and depression was negatively correlated with QoL. This supports the results of a previous study [18] that the QoL of older adults living in rural areas was negatively correlated with depression and that the QoL of older adults with depression was lower than that of older adults without depression. Since sarcopenia in older adults is significantly associated with an increased risk of depression [9], to improve the QoL of the older adults with sarcopenia it is necessary to develop a social support system using small groups of the older adults living alone and a specific program for the management of older adults with depression [18].
Among the nutritional status categories in this study, the high-risk group comprised 71.2% (89 patients), and the mean score for nutritional status was 9.5 points; thus, the nutritional status of older adults was poor. A previous study found that [33] the high-risk group for nutritional status was 39% and the mean nutritional status score was 12.9 in a study of general older adults; compared to these results, it can be seen that the nutritional status of older adults in this study was very poor and that the nutritional status evaluation of older adults is paramount. It is recommended that older adults consume more than 1.2 g/day of protein per 1 kg of body weight, which is higher than the daily recommended amount (0.9 g for the general public in Korea) [5]. Adequate nutritional support is recommended at an early stage to improve bodily function, thereby preventing the progression of sarcopenia in older adults [5]. Nutritional interventions tailored to LOAs increase nutrient intake and reduce malnutrition in all older adults [20]. Therefore, there is a need for public awareness of the importance of adequate daily protein intake and implementation of guidelines on daily protein intake in the older adult population in Korea, especially in clinical practice [5]. Additionally, depression had a mediating effect on the relationship between nutritional status and QoL in older adults [33]. Therefore, to improve the QoL of LOAs or alleviate the lack of social support, special evaluation and focus are needed to understand nutritional status and depression simultaneously.
In this study, the variables affecting the anxiety of the participants were one-person households, subjective health status, and physical discomfort. The higher the anxiety, the lower the participants’ QoL. This supports the results of a study by de Oliveira et al. [34] that found that active older adults had less anxiety and a higher QoL than sedentary older adults. Anxiety among high-vulnerability older adults is a concern for physical health related to social isolation and loneliness [21]. To improve the QoL of older adults living alone, active nursing intervention activities that can reduce anxiety in both public and private spaces, such as social welfare centers and senior citizen centers, should be prioritized.
Sarcopenia status was not identified as a factor influencing QoL in this study. However, the relationship between physical status and QoL has been confirmed through objective indicators of grip strength, muscle mass, and physical performance in older adults with sarcopenia. The results are significant in that they reveal the factors affecting the prevalence of severe sarcopenia and QoL of LOAs with sarcopenia. In the current study, 56.8% of participants had severe sarcopenia. Severe sarcopenia is influenced by a combination of several risk factors such as sex, diabetes, impairment in performing activities of daily living, and nutritional intake [8]. Therefore, it is necessary to comprehensively assess several risk factors, in addition to a wide range of health, social, and economicsupport, for LOAs. The results of this study demonstrate the importance of assessment and intervention for sarcopenia and psychological distress in LOAs. Sarcopenia in LOAs should be screened, and an integrated sarcopenia management service, including multidisciplinary nutritional and psychosocial interventions, should be developed and implemented.
This study has some limitations. First, the study participants were LOAs living in the community. In the future, it is necessary to conduct a study targeting older people in various environments. Second, the results of this study cannot be generalized because the data were collected from one region. Nevertheless, in the current study, an objective evaluation of sarcopenia was performed according to the AWGS algorithm, and nutritional status and psychological factors were identified as factors influencing the QoL of LOAs with sarcopenia. Therefore, it is meaningful to present an objective, evidence-based nursing perspective to improve the QoL of LOAs with sarcopenia.
CONCLUSION
In this study, depression, nutritional status, and anxiety were factors influencing QoL in LOAs with sarcopenia. This finding provides practical and useful evidence that nursing interventions, including strategies to reduce depression, improve nutritional status, and reduce anxiety, can potentially improve QoL in LOAs with sarcopenia.
This work was presented at 2022 Korean Society of Nursing Science Conference, October 2022, Seoul, Republic of Korea.
CONFLICTS OF INTEREST:The authors declared that no conflict of interest.
FUNDING:This research was supported by National University Development Project at Jeonbuk National University in 2021.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Nho JH & Kim EJ.
Data curation or/and Analysis: Nho JH & Kim EJ.
Funding acquisition: Nho JH.
Investigation: Nho JH.
Project administration or/and Supervision: Nho JH.
Resources or/and Software: Nho JH.
Validation: Nho JH & Kim EJ.
Visualization: Nho JH & Kim EJ.
Writing original draft or/and review & editing: Nho JH & Kim EJ.
ACKNOWLEDGEMENTS
None.
References
-
Statistics Korea. 2021 Senior statistics [Internet]. Daejeon: Statistics Korea; 2021 [cited 2022 Apr 20].Available from: http://www.kostat.go.kr/portal/korea/kor_
nw/1/1/index.board?bmode=read&aSeq=403253 .
-
-
Yoo JI, Ha YC, Kim M, Seo SH, Kim MJ, Lee GY, et al. Translation and validation of the Korean version of the Sarcopenia Quality of Life (SarQoL-K®) questionnaire and applicability with the SARC-F screening tool. Quality of Life Research 2021;30(2):603–611. [doi: 10.1007/s11136-020-02630-2]
-
-
Beom JW. Clinical significance of sarcopenia. Geriatric Rehabilitation 2020;10(2):46–49.
-
-
Jung HW, Kim SW, Kim IY, Lim JY, Park HS, Song W, et al. Protein intake recommendation for Korean older adults to prevent sarcopenia: Expert consensus by the Korean Geriatric Society and the Korean Nutrition Society. Annals of Geriatric Medicine and Research 2018;22(4):167–175. [doi: 10.4235/agmr.18.0046]
-
-
Kim M, Won CW. Sarcopenia in Korean community-dwelling adults aged 70 years and older: Application of screening and diagnostic tools from the Asian Working Group for Sarcopenia 2019 update. Journal of the American Medical Directors Association 2020;21(6):752–758. [doi: 10.1016/j.jamda.2020.03.018]
-
-
Handajani YS, Widjaja NT, Turana Y, Tengkawan J. Diabetes mellitus, adl disability and nutrition intake: Determination factors of severe sarcopenia among elderly in urban nursing homes. Indian Journal of Public Health Research & Development 2018;9(3):69–75.
-
-
Lee I, Cho J, Hong H, Jin Y, Kim D, Kang H. Sarcopenia is associated with cognitive impairment and depression in elderly Korean women. Iranian Journal of Public Health 2018;47(3):327–334.
-
-
Kim HH, Kim JS, Yu JO. Factors contributing to sarcopenia among community-dwelling older Korean adults. Journal of Korean Gerontological Nursing 2014;16(2):170–179. [doi: 10.17079/jkgn.2014.16.2.170]
-
-
Gao L, Jiang J, Yang M, Hao Q, Luo L, Dong B. Prevalence of sarcopenia and associated factors in Chinese community-dwelling elderly: Comparison between rural and urban areas. Journal of the American Medical Directors Association 2015;16(11):1003.e1–1003.e6. [doi: 10.1016/j.jamda.2015.07.020]
-
-
Kim KN, Hyun T, Lee JW. Development of a simple screening test for identifying Korean elderly at risk of undernutrition. Korean Journal of Community Nutrition 2000;5(3):475–483.
-
-
Verlaan S, Aspray TJ, Bauer JM, Cederholm T, Hemsworth J, Hill TR, et al. Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: A case-control study. Clinical Nutrition 2017;36(1):267–274. [doi: 10.1016/j.clnu.2015.11.013]
-
-
Umegaki H. Sarcopenia and frailty in older patients with diabetes mellitus. Geriatrics & Gerontology International 2016;16(3):293–299. [doi: 10.1111/ggi.12688]
-
-
Kim JI. Levels of health-related quality of life (EQ-5D) and its related factors among vulnerable elders receiving home visiting health care services in some rural areas. Journal of Korean Academy of Community Health Nursing 2013;24(1):99–109. [doi: 10.12799/jkachn.2013.24.1.99]
-
-
Lee Y, Yang N, Shin M, Lee KE, Yoo CH, Kim K. The effects of a personalized nutrition intervention program on food security, health and nutritional status of low-income older adults in Seoul city. Journal of Nutrition and Health 2020;53(4):416–430. [doi: 10.4163/jnh.2020.53.4.416]
-
-
Kim YS, Tae YS, Nam GH. Distress and quality of life among elderly patients with gastric cancer: The mediating effect of social support. Korean Journal of Adult Nursing 2017;29(5):536–546. [doi: 10.7475/kjan.2017.29.5.536]
-
-
Won CW. Diagnosis of sarcopenia in primary health care. Journal of the Korean Medical Association 2020;63(10):633–641. [doi: 10.5124/jkma.2020.63.10.633]
-
-
Balogun JA, Onigbinde AT. Intratester reliability and validity of the Takei Kiki Kogo hand grip dynamometer. Journal of Physical Therapy Science 1991;3:55–60.
-
-
Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, et al. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clinical Nutrition 2011;30(5):610–615. [doi: 10.1016/j.clnu.2011.04.001]
-
-
Cha ES. Cha Korean translation of the DASS21 [Internet]. Sydney: Psychology Foundation of Australia; 2018 [cited 2022 Apr 10].Available from: http://www2.psy.unsw.edu.au/dass .
-
-
Lovibond SH, Lovibond PF. In: Manual for the depression anxiety stress scales. 2nd ed. Sydney: Psychology Foundation of Australia; 1995. pp. 4-42.
-
-
Nho JH, Kim EJ. Mediating effects of depression on relationships between nutritional status and quality of life among older adults: A cross-sectional study. Journal of Korean Gerontological Nursing 2022;24(1):47–54. [doi: 10.17079/jkgn.2022.24.1.47]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

