Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 53(2); 2023 > Article
- Research Paper Association between Visual Impairment and Nutritional Risk among Older Adults with Diabetes: A Population-Based Cross-Sectional Study
- Eunjin Yang, Kyung Hee Lee
-
Journal of Korean Academy of Nursing 2023;53(2):167-176.
DOI: https://doi.org/10.4040/jkan.22141
Published online: April 30, 2023
-
Corresponding author:
Kyung Hee Lee,
Email: kyungheelee@yuhs.ac
Abstract
Purpose
Despite the high prevalence of visual impairment caused by diabetic retinopathy and nutritional problems among older adults with diabetes, evidence regarding factors related to nutritional risk in this population is limited. Therefore, this study aimed to identify the correlates of nutritional risk among older adults with diabetes, focusing on visual impairment.
Methods
This study was a secondary data analysis of the 2020 National Survey of Older Koreans aged 65 years and above. The sample comprised 2,376 older adults with diabetes, and complex sample ANOVA and Rao–Scott chi-square tests were used to compare the groups according to visual impairment. Complex-sample logistic regression analyses were conducted to verify the association between visual impairment and nutritional risk.
Results
Older adults with diabetes, who also have severe visual impairment, are more likely to have nutritional risk status than those without impairment after controlling for covariates (odds ratio [OR] = 2.44, 95% confidence interval [CI] 1.16~5.13). Among the covariates, depression (OR = 3.58, 95% CI 2.60~4.94), dependent activities of daily living status (OR = 2.79, 95% CI 1.60~4.86), and experience of hospitalization during the past year (OR = 2.51, 95% CI 1.57~4.03) were strongly associated with nutritional risk.
Conclusion
Severe visual impairment increases the nutritional risk among older adults with diabetes. Therefore, it is essential to prevent visual impairment due to exacerbation of diabetes through appropriate management. Additionally, tailored nutritional interventions for visually impaired older adults with diabetes that consider visual characteristics are required.
Published online Apr 30, 2023.
https://doi.org/10.4040/jkan.22141
Association between Visual Impairment and Nutritional Risk among Older Adults with Diabetes: A Population-Based Cross-Sectional Study
Abstract
Purpose
Despite the high prevalence of visual impairment caused by diabetic retinopathy and nutritional problems among older adults with diabetes, evidence regarding factors related to nutritional risk in this population is limited. Therefore, this study aimed to identify the correlates of nutritional risk among older adults with diabetes, focusing on visual impairment.
Methods
This study was a secondary data analysis of the 2020 National Survey of Older Koreans aged 65 years and above. The sample comprised 2,376 older adults with diabetes, and complex sample ANOVA and Rao–Scott chi-square tests were used to compare the groups according to visual impairment. Complex-sample logistic regression analyses were conducted to verify the association between visual impairment and nutritional risk.
Results
Older adults with diabetes, who also have severe visual impairment, are more likely to have nutritional risk status than those without impairment after controlling for covariates (odds ratio [OR] = 2.44, 95% confidence interval [CI] 1.16~5.13). Among the covariates, depression (OR = 3.58, 95% CI 2.60~4.94), dependent activities of daily living status (OR = 2.79, 95% CI 1.60~4.86), and experience of hospitalization during the past year (OR = 2.51, 95% CI 1.57~4.03) were strongly associated with nutritional risk.
Conclusion
Severe visual impairment increases the nutritional risk among older adults with diabetes. Therefore, it is essential to prevent visual impairment due to exacerbation of diabetes through appropriate management. Additionally, tailored nutritional interventions for visually impaired older adults with diabetes that consider visual characteristics are required.
INTRODUCTION
The global prevalence of diabetes among people aged 20~79 is expected to increase from 10.5% in 2021 to 12.2% in 2045 [1]. Furthermore, approximately 13.6% of people aged 30 and above in South Korea have diabetes; the majority (56.6%) are older adults aged 60 and older [2]. Various health concerns related to older adults with diabetes have been raised, one of which is nutritional problems, which are highly prevalent among people with diabetes of all ages [3, 4, 5]. Previous studies found that 18.5% to 21.2% of hospitalized older adults with diabetes were malnourished, and 33.1% to 39.1% were at risk of malnutrition [6, 7]. Moreover, community-dwelling older adults with diabetes might have a higher nutritional risk than those without diabetes [8].
Nutrition is a crucial factor for healthy aging [9] and an integral part of self-care for older adults with diabetes [10]. Malnutrition can be defined as a condition in which an imbalance of energy and nutrients adversely affects bodily functions and clinical outcomes. It is associated with a decline in other muscle, cognitive, digestive, and homeostatic regulatory functions [11, 12]; this term encompasses undernourishment and overnutrition [13]. Unlike malnutrition, nutritional risk refers to the risk of inadequate nutritional status caused by an imbalance between intake and metabolic needs [14, 15]. Nutritional deficiencies in older adults with diabetes can cause adverse health outcomes such as sarcopenia [16], frailty [17], risk of falls [18], diabetes complications, and mortality [19]. Therefore, good nutritional status is essential to prevent adverse outcomes and maintain a healthy life for older adults.
Several factors could put older adults with diabetes at a higher nutritional risk, such as restrictive eating habits to control blood glucose levels and age-related changes, including difficulty swallowing, changing sense of appetite, delayed gastric emptying, and dental problems [10, 20]. Previous studies have revealed that hospitalization, eating dependency, poor appetite, health status, and decreased physical function are associated with malnutrition in older adults [21]. Additionally, dementia, impaired functioning, chewing difficulties, swallowing difficulties, and older age are associated with malnutrition among institutionalized older adults [22]. Longitudinal studies have revealed that age, frailty, excessive polypharmacy, decreased physical function, and Parkinson’s disease affect malnutrition in older adults [23]. However, these studies focused on the general population of older adults.
Although a few studies regarding nutritional concerns have been conducted on older adults with diabetes [6, 7], they were performed in hospital settings and faced limitations in terms of identifying factors related to nutritional risk. In particular, visual impairment (VI) resulting from aging and diabetes complications is a risk factor for nutritional problems and may affect nutritional status in this population. A systematic review revealed that VI is linked to abnormal body mass index, difficulty shopping for meals, challenging meal preparation and eating, and visiting restaurants [24]. This implies that poor vision could be a barrier to adequate food intake. However, most of the included studies did not focus on individuals with diabetes. Older adults with diabetes have a higher prevalence of VI than the non-diabetic population [25]; however, empirical evidence regarding the association between VI and nutritional risk in this population is still limited.
Considering the importance and high prevalence of vision and nutritional problems among older adults with diabetes, this study aimed to identify the association between VI and nutritional risk among older adults with diabetes after controlling for other risk factors using nationally representative samples of older adults in South Korea.
METHODS
1. Study design
This secondary data analysis employed the 2020 National Survey of Older Koreans, a nationally representative survey of older adults in South Korea aged 65 and above. The survey was conducted and managed by the Korea Institute for Health and Social Affairs (KIHASA) and the Ministry of Health and Welfare every three years.
2. Study data and participants
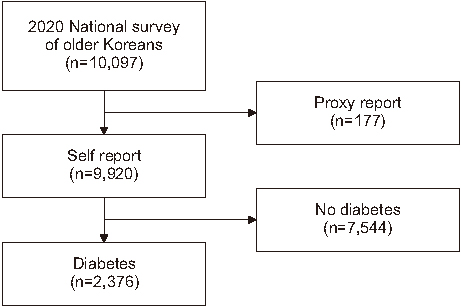
The original survey was intended for a deep understanding of older adults’ needs and living conditions. Fifteen teams, comprising one supervisor and four surveyors, conducted this survey using a complex sampling design from September 14 to November 20, 2020. The original sample was comprised of 10,097 older adults. As the target sample of this study was older adults with diabetes, we included 2,376 older adults with diabetes who answered by themselves (Figure 1). We excluded participants who provided proxy answers because several important variables, including self-reported VI, depression, self-rated health status, and social support were not answered.
Figure 1
Flow chart of the study population.
3. Measurement
1) Dependent variable
Nutritional risk refers to at-risk status for poor nutrition and was measured using the DETERMINE Your Nutritional Health Checklist [26] based on the warning signs of poor nutritional status. Nutritional risk levels, which are a bundle of warning signs, including disease, tooth loss, eating poorly, mouth pain, and economic strain, are only suggestive of risk; they are not a diagnosis of any condition. Response options for the DETERMINE Your Nutritional Health Checklist were “Yes” or “No.” The ten items included evaluated unintended body weight change, quantity and quality of intake, oral problems associated with intake, eating alone, economic strain to buy foods, and changing food types or amounts due to disease, among others. Each item has a different weight, from 1 to 4; therefore, the total score ranges from 1 to 21. The participants were classified into three levels of nutritional status according to cut-off scores: “good” (0~2), “moderate risk” (3~5), and “high risk” (6 or more). Scores of 3~5 indicated that the participants were at moderate nutritional risk, and a score of 6 or more indicated high nutritional risk. Thereafter, the moderate- and high-risk groups were combined into a single group, representing the nutritional risk group.
2) Independent variable
Self-reported VI was assessed using a single question: “Do you have difficulties watching TV or reading the newspaper, even when using visual aids?” [27, 28, 29, 30]. The answers were organized into ordinal categories as follows: 1 = no difficulties, 2 = slightly uncomfortable, and 3 = severely uncomfortable. These responses were categorized as no VI, mild VI, or severe VI.
3) Covariates
Covariates were selected through a literature review, including demographic, healthcare, and psychosocial/functional variables [21, 23]. Age (yr) and sex (male or female) were included as demographic variables. Polypharmacy and recent hospitalization were included as the healthcare variables. Numerical definitions were used to evaluate polypharmacy, which involves taking five or more prescribed medicines daily [31]. Polypharmacy was determined using a single question: “How many medications have you been taking daily for more than three months?” The answers were reclassified as dichotomized (0 = no polypharmacy, 1 = polypharmacy). If participants had experienced at least one hospitalization during the past year, they were classified as having a recent hospitalization event (0 = no hospitalization, 1 = hospitalization).
The psychosocial variables included depression and structural social support. Depression was assessed using the 15-item Korean version of the Short Form of Geriatric Depression Scale (SGDS-K) [32]. The questionnaire included items about feelings experienced in the past week, and the allowed answers were “yes” or “no.” The total score ranges from 0 to 15, and scores of 8 and above indicate depression. The item reliability, according to the Kuder-Richardson 20, was 0.88 in this study. Structural social support was measured based on the number of social relationships using a single question: “How many people do you have that you can open your heart to among family, friends, neighbors, and close relatives?”
The number of chronic diseases, cognitive impairment, activities of daily living (ADL), and self-rated health status were selected as the functional variables. We investigated the total number of diseases and chronic diseases, including cardiovascular, endocrine, musculoskeletal, respiratory, neurological, sensory, cancer, gastrointestinal, and genitourinary disorders. Cognitive impairment was measured using the Korean version of the Mini-Mental Status Examination for Dementia Screening [33], which comprises 19 items with a score range of 0~30. The tool guides classification as cognitive impairment considering participants’ age, education level, and sex [33, 34]; therefore, we classified cognitive impairment groups according to this guidance. ADL were assessed using the Korean ADL Scale [35]. The tool comprises seven items: dressing, washing, bathing, eating, transferring, toileting, and continence. Cronbach’s alpha was 0.94 in the development study and 0.95 in the current study. If the participant required assistance with at least one activity, we recorded the answer as “dependent.” Self-rated health was assessed using the question, “How do you feel about your health condition?” The answers were as follows: excellent, good, moderate, poor, and very poor. The answers were classified into three categories: excellent/good, moderate, and poor/very poor.
4. Statistical analysis
Complex sample data analysis considering strata and sampling weight was conducted because the survey utilized a complex sampling design. We presented the descriptive analysis results as estimated means, standard errors, unweighted counts, and weighted percentages according to the type of variables. Complex sample analysis of variance (ANOVA) and Rao–Scott chi-square tests were used to compare the characteristics of the groups by VI. In addition, the Bonferroni correction was used for multiple comparisons. Complex sample logistic regression was conducted to examine the association between VI and nutritional risk after adjusting for covariates. We entered only the VI variable in the first step, added demographic and health variables in the second step, and psychosocial and functional variables in the third step. Multicollinearity was not observed among variables. SPSS (version 26.0; IBM Corp., Armonk, NY, USA) was used for all analysis.
5. Ethical considerations
The original data for the current study were collected after receiving approval from the Institutional Review Board of KIHASA (IRB No. 2020-36). The requirement for informed consent was waived because the data were publicly available. The current study was exempted by the Institutional Review Board of Severance Hospital (No.4-2021-1044). All methods were implemented following relevant guidelines and regulations.
RESULTS
1. Characteristics of participants per VI
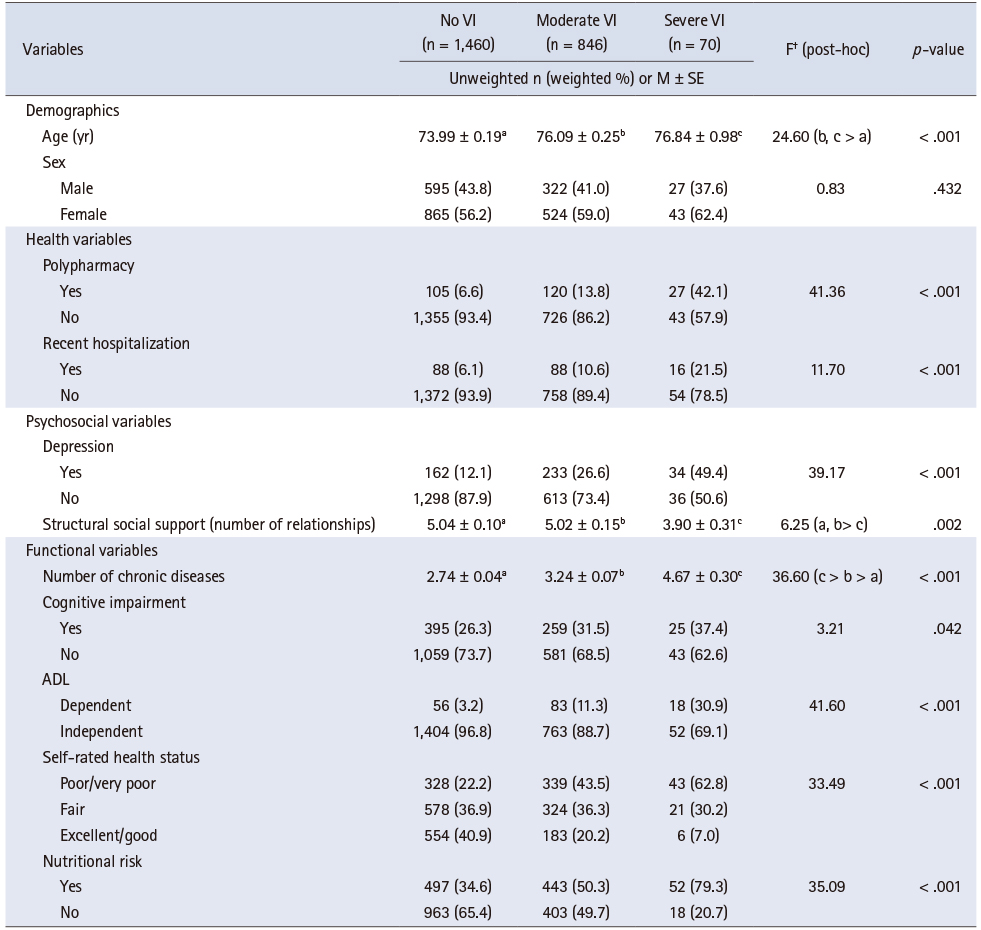
Participant characteristics according to the VI level are presented in Table 1. Among 2,376 older adults with diabetes, 58.9% had no VI, 36.8% had moderate VI, and 4.2% had severe VI. Older adults with diabetes with severe VI were more likely to be older, have polypharmacy, and experience recent hospitalization. Regarding psychosocial and functional factors, 49.4% of participants with severe VI, 26.6% with moderate VI, and 12.1% with no VI had depression. Structural social support, defined as the number of people with whom individuals had close relationships, was higher among participants with no VI or moderate VI than among those with severe VI. The prevalence of chronic diseases was also higher among participants with severe VI than among those with moderate or no VI. Furthermore, participants with severe VI were more likely to have cognitive impairment and dependent ADL. They had the highest proportion of self-reported poor/very poor health status health status among the three groups. Additionally, 79.3% of participants with severe VI, 50.3% with moderate VI, and 34.6% with no VI were classified into the nutritional risk group.
Table 1
Participant Characteristics by Visual Impairment Level (N = 2,376)
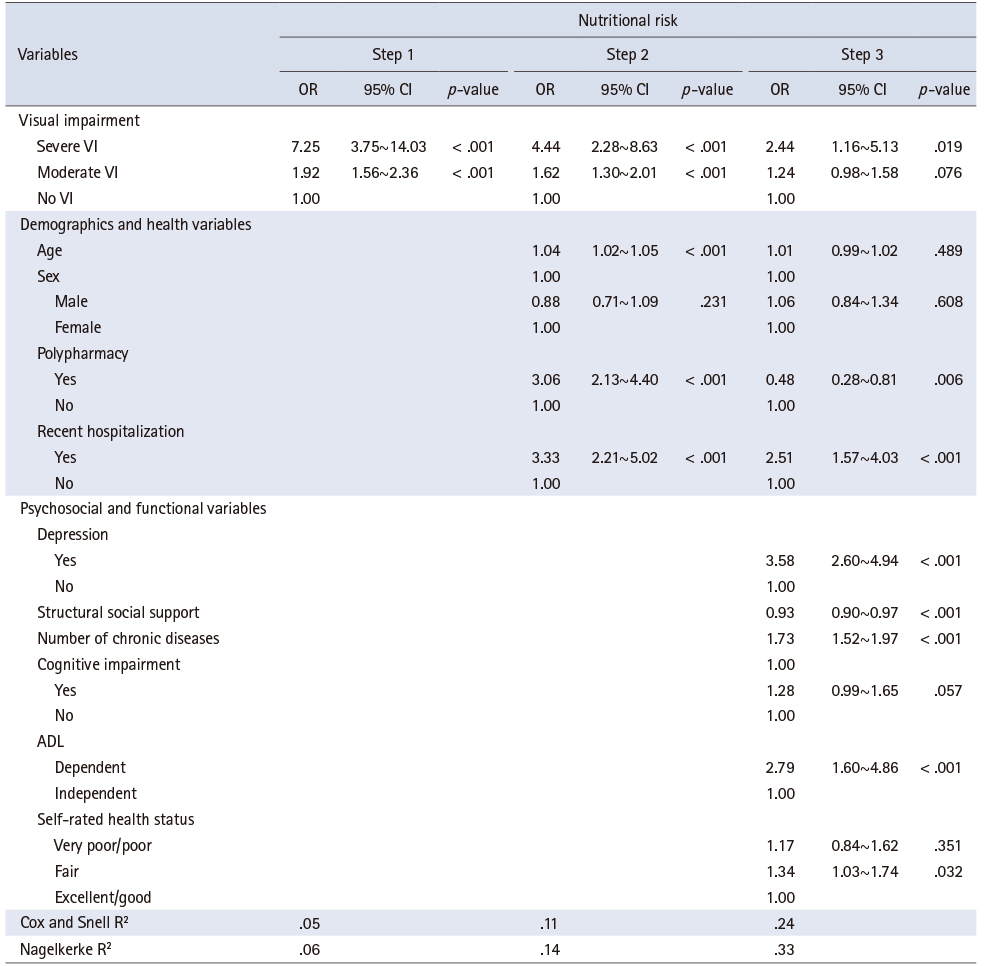
2. Results of logistic regression model
The results of the complex-sample logistic regression analysis are presented in Table 2. In step 1, participants with severe or moderate VI had a significantly higher nutritional risk than those without VI (odds ratio [OR] = 7.25, 95% confidence interval [CI] 3.75~14.03 for severe VI; OR = 1.92, 95% CI 1.56~2.36 for moderate VI). This relationship was still significant after including demographics and health variables in step 2; however, only severely visually impaired older adults had a statistically higher nutritional risk than those with no VI in the final model (OR = 2.44, 95% CI 1.16~5.13). Among the covariates, depression (OR = 3.58, 95% CI 2.60~4.94), dependent ADL status (OR = 2.79, 95% CI 1.60~4.86), and experience of hospitalization during the past year (OR = 2.51, 95% CI 1.57~4.03) were strongly associated with nutritional risk in the final model. In addition, polypharmacy, structural social support, number of chronic diseases, and fair self-rated health status were significantly associated with nutritional risk.
Table 2
Hierarchical Regression Analyses Examining the Association between Visual Impairment and Nutritional Risk (N = 2,376)
DISCUSSION
We identified factors related to nutritional risk in a nationally representative sample of older South Korean adults. The main findings revealed that poor vision was associated with greater nutritional risk among older adults with diabetes. Although the relationship between VI and nutritional risk was weakened by the addition of other essential factors such as depression, dependent ADL status, and recent hospitalization, severe VI remained statistically significant.
Impaired vision could affect lifestyles, such as patients’ dietary habits, meal shopping, and restaurant use among people with diabetes and VI. Furthermore, diabetic patients with vision-related problems find it difficult to choose healthy food and find nutrition facts indicated on the surface of food packets [24]. They face difficulty accessing readable nutritional information, such as tactile materials or those with large prints [36], and they also face limitations in cooking. A previous study revealed that visually impaired people with diabetes expressed a lack of educational opportunities and a desire to learn to cook diabetes-friendly meals and calculate their optimal calorie and food consumption [37]. Older adults with diabetes and visual problems face more difficulties in maintaining a healthy diet and in other self-care domains such as glucose monitoring and exercise. Therefore, diabetes educators who care for older adults with diabetes and visual problems need to pay more attention to older adults with VIs’ eagerness to learn about diabetes self-care, cooking healthy meals, adhering to optimal calories, and challenges to self-care when they deliver diabetes education. Our results support the relationship between VI and nutritional risk; therefore, appropriate interventions to improve nutritional status in older adults with vision-related problems are needed, and visual characteristics should be considered during nutritional interventions in this population [38].
Among the covariates, depression, dependent ADL status, and hospitalization during the past year were strongly associated with nutritional risk, with depression being the most substantial factor. Previous studies have revealed that people with VI are more likely to have depression [39, 40]; depression is widely regarded as a barrier to diabetes management in older adults [41]. Since depression is prevalent among older adults with diabetes and is preventable and treatable, it should be screened for and prevented by incorporating it into diabetes self-management and nutritional education. Diabetes impairs mobility and ADL [42], with our study revealing that dependent ADL is a robust factor among the covariates for increasing nutritional risk, which is consistent with the findings of a previous longitudinal study [23]; recent hospitalization events are also a significant factor for nutritional risk. This means that older adults discharged from the hospital have a high nutritional risk for some time after discharge. It is obvious that hospitalization-related illnesses increase nutritional requirements and contribute to malnutrition among hospitalized older adults [43]. Nurses, doctors, and nutritionists must engage in multidisciplinary efforts to meet the nutritional requirements of older adults with diabetes who have been hospitalized recently. Such efforts may include additional nutritional support and careful discharge of nutritional plans.
Of the total number of older adults with diabetes in this study, 36.8% had moderate VI, and 4.2% had severe VI; these estimates were higher than for those without diabetes [44]. They were also higher than the low vision prevalence reported in the United States using best-corrected visual acuity [45] and 6.9% VI prevalence estimated by subjective measures [46]. This estimation in the current study may reflect a high prevalence of VI in the diabetic population [47] or may be attributed to our broad definition of VI. In this study, 42.3% of the participants were at nutritional risk. As nutrition is a crucial area in diabetes management, poor nutrition could worsen vision and other diabetes-related vascular complications [48]. Impaired vision increases the nutritional risk, and poor nutritional status increases the risk of diabetes-related complications, creating a vicious circle. Considering that many previous studies regarding VI and nutritional risk used a small sample size [24] and did not include older adults with diabetes, our findings with a large sample could provide evidence for the positive relationship between VI and nutritional risk in this population. Previous studies on diabetes patients focused on health outcomes, such as mortality and length of hospital stay, caused by nutritional risk among hospitalized patients [6, 7, 49]; however, our study investigated factors associated with nutritional risks, such as VI, which is a pervasive condition among diabetic patients. This study could provide insights into preventing nutritional risk in this population and fill the gaps in previous studies. Diabetes education and improving patients’ diabetes self-care management ability are important aspects of nursing interventions for persons with diabetes. Therefore, for diabetes educators and gerontological nurses, more attention to patients’ visual function will be needed. Appropriate screening, assessment, diagnosis, and treatment of older adults’ visual function and nutritional status should be considered in diabetes education to prevent both decreased vision and malnourishment in older adults with diabetes.
This study had some limitations. First, as this was a secondary data analysis, diverse variables related to known nutritional risk factors, laboratory variables, and diabetes-related factors, such as duration of diabetes and diabetes medication adherence, were not included in the original survey and, thus, excluded from this study. Therefore, future studies should consider these variables as covariates to ensure more rigorous findings. Second, the VI questions were based on self-reports rather than objective measurements. Third, this cross-sectional survey was unable to infer causal relationships. Nevertheless, this study had a large sample size that could provide data to estimate VI and nutritional prevalence among older adults with diabetes, and it can be generalized to South Korea.
CONCLUSION
Our findings suggest that severe VI positively correlates with nutritional risk in older adults with diabetes. Given the association between VI and nutritional risk, it is vital to prevent VI caused by exacerbation of diabetes through appropriate management. Additionally, tailored nutritional interventions considering visual characteristics, such as evaluating the participants’ preferences for materials and places and providing information to visually impaired older adults in accessible ways, are needed.
CONFLICTS OF INTEREST:Lee, Kyung Hee has been the Editorial Board Member of JKAN since 2022 but has no role in the review process. Except for that, no potential conflict of interest relevant to this article was reported.
FUNDING:This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No.2020 R1A6A1A03041989).
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Yang E & Lee KH.
Data curation or/and Analysis: Yang E.
Funding acquisition: Lee KH.
Investigation: Yang E & Lee KH.
Project administration or/and Supervision: Lee KH.
Resources or/and Software: Lee KH.
Validation: Yang E & Lee KH.
Visualization: Yang E & Lee KH.
Writing original draft or/and review & editing: Yang E & Lee KH.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research and Clinical Practice 2022;183:109119 [doi: 10.1016/j.diabres.2021.109119]
-
-
Korea Disease Control and Prevention Agency (KDCA). 2022 Chronic disease fact book [Internet]. Cheongju: KDCA; c2022 [cited 2022 Nov 11].Available from: https://www.kdca.go.kr/gallery.es?mid=a20503020000&bid=0003&b_
list=9&act=view&list_ no=145880&nPage=5&vlist_ no_ npage=9&keyField=&keyWord=&orderby= .
-
-
Yildirim ZG, Uzunlulu M, Caklili OT, Mutlu HH, Oğuz A. Malnutrition rate among hospitalized patients with type 2 diabetes mellitus. Progress in Nutrition 2018;20(2):183–188. [doi: 10.23751/pn.v20i2.6164]
-
-
Vural Keskinler M, Feyİzoglu G, Yildiz K, Oguz A. The frequency of malnutrition in patients with type 2 diabetes. Medeniyet Medical Journal 2021;36(2):117–122. [doi: 10.5222/MMJ.2021.44270]
-
-
Liu GX, Chen Y, Yang YX, Yang K, Liang J, Wang S, et al. Pilot study of the Mini Nutritional Assessment on predicting outcomes in older adults with type 2 diabetes. Geriatrics & Gerontology International 2017;17(12):2485–2492. [doi: 10.1111/ggi.13110]
-
-
Sanz París A, García JM, Gómez-Candela C, Burgos R, Martín Á, Matía P. Malnutrition prevalence in hospitalized elderly diabetic patients. Nutricion Hospitalaria 2013;28(3):592–599. [doi: 10.3305/nh.2013.28.3.6472]
-
-
Turnbull PJ, Sinclair AJ. Evaluation of nutritional status and its relationship with functional status in older citizens with diabetes mellitus using the mini nutritional assessment (MNA) tool--a preliminary investigation. The Journal of Nutrition, Health & Aging 2002;6(3):185–189.
-
-
Ahmed N, Choe Y, Mustad VA, Chakraborty S, Goates S, Luo M, et al. Impact of malnutrition on survival and healthcare utilization in Medicare beneficiaries with diabetes: A retrospective cohort analysis. BMJ Open Diabetes Research & Care 2018;6(1):e000471 [doi: 10.1136/bmjdrc-2017-000471]
-
-
The British Association for Parenteral and Enteral Nutrition (BAPEN). Introduction to malnutrition [Internet]. Letchworth: BAPEN; c2018 [cited 2023 Feb 9].
-
-
Ramage-Morin PL, Garriguet D. Nutritional risk among older Canadians. Health Reports 2013;24(3):3–13.
-
-
Matsuura S, Shibazaki K, Uchida R, Imai Y, Mukoyama T, Shibata S, et al. Sarcopenia is associated with the Geriatric Nutritional Risk Index in elderly patients with poorly controlled type 2 diabetes mellitus. Journal of Diabetes Investigation 2022;13(8):1366–1373. [doi: 10.1111/jdi.13792]
-
-
Cobo A, Vázquez LA, Reviriego J, Rodríguez-Mañas L. Impact of frailty in older patients with diabetes mellitus: An overview. Endocrinología y Nutrición (English Edition) 2016;63(6):291–303. [doi: 10.1016/j.endoen.2016.07.001]
-
-
Trevisan C, Crippa A, Ek S, Welmer AK, Sergi G, Maggi S, et al. Nutritional status, body mass index, and the risk of falls in community-dwelling older adults: A systematic review and meta-analysis. Journal of the American Medical Directors Association 2019;20(5):569–582.e7. [doi: 10.1016/j.jamda.2018.10.027]
-
-
Söderström L, Rosenblad A, Thors Adolfsson E, Bergkvist L. Malnutrition is associated with increased mortality in older adults regardless of the cause of death. British Journal of Nutrition 2017;117(4):532–540. [doi: 10.1017/S0007114517000435]
-
-
Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clinical Interventions in Aging 2010;5:207–216. [doi: 10.2147/cia.s9664]
-
-
O’Keeffe M, Kelly M, O’Herlihy E, O’Toole PW, Kearney PM, Timmons S, et al. Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clinical Nutrition 2019;38(6):2477–2498. [doi: 10.1016/j.clnu.2018.12.007]
-
-
Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, Vereecken C, Vanhauwaert E, Declercq A, et al. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Advances in Nutrition 2016;7(3):507–522. [doi: 10.3945/an.115.011254]
-
-
Jones N, Bartlett H. The impact of visual impairment on nutritional status: A systematic review. British Journal of Visual Impairment 2018;36(1):17–30. [doi: 10.1177/0264619617730860]
-
-
Centers for Disease Control and Prevention (CDC). Prevalence of visual impairment and selected eye diseases among persons aged >/=50 years with and without diabetes--United States, 2002. MMWR Morbidity and Mortality Weekly Report 2004;53(45):1069–1071.
-
-
Crews JE, Chou CF, Zhang X, Zack MM, Saaddine JB. Health-related quality of life among people aged ≥65 years with self-reported visual impairment: Findings from the 2006-2010 behavioral risk factor surveillance system. Ophthalmic Epidemiology 2014;21(5):287–296. [doi: 10.3109/09286586.2014.926556]
-
-
Han JW, Kim TH, Jhoo JH, Park JH, Kim JL, Ryu SH, et al. A normative study of the Mini-Mental State Examination for Dementia Screening (MMSE-DS) and its short form(SMMSE-DS) in the Korean elderly. Journal of Korean Geriatric Psychiatry 2010;14(1):27–37.
-
-
National Institute of Dementia. MMSE-DS score converter [Internet]. Seoul: National Institute of Dementia; c2012 [cited 2022 Nov 11].Available from: https://www.nid.or.kr/info/dataroom_
view.aspx?BID=21 .
-
-
Won CW, Rho YG, Kim SY, Cho BR, Lee YS. The validity and reliability of Korean Activities of Daily Living(K-ADL) scale. Journal of the Korean Geriatrics Society 2002;6(2):98–106.
-
-
Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, Stevenson C, et al. Diabetes and risk of physical disability in adults: A systematic review and meta-analysis. The Lancet Diabetes & Endocrinology 2013;1(2):106–114. [doi: 10.1016/S2213-8587(13)70046-9]
-
-
Ligthart-Melis GC, Luiking YC, Kakourou A, Cederholm T, Maier AB, de van der Schueren MAE. Frailty, sarcopenia, and malnutrition frequently (Co-)occur in hospitalized older adults: A systematic review and meta-analysis. Journal of the American Medical Directors Association 2020;21(9):1216–1228. [doi: 10.1016/j.jamda.2020.03.006]
-
-
Lee Y, Kim S, Hwang N, Lim JM, Joo B, NamKung EH, et al. In: 2020 National survey of older Koreans. Sejong: Korea Institute for Health and Social Affairs; 2020 Nov.Report No.: 2020-35.
-
-
Xie Y, Zhang H, Ye T, Ge S, Zhuo R, Zhu H. The Geriatric Nutritional Risk Index independently predicts mortality in diabetic foot ulcers patients undergoing amputations. Journal of Diabetes Research 2017;2017:5797194 [doi: 10.1155/2017/5797194]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

