Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(3); 2024 > Article
- Research Paper Moderating Effect of General Self-Efficacy on the Relationship between Pregnancy Stress, Daily Hassles Stress, and Preterm Birth Risk in Women Experiencing Preterm Labor: A Cross-Sectional Study
- Hyun-Jeong Cho, Jeung-Im Kim
-
Journal of Korean Academy of Nursing 2024;54(3):329-339.
DOI: https://doi.org/10.4040/jkan.24008
Published online: August 31, 2024
2School of Nursing, College of Medicine, Soonchunhyang University, Cheonan, Korea
-
Corresponding author:
Jeung-Im Kim,
Email: jeungim@sch.ac.kr
Abstract
Purpose
This study investigated the moderating role of general self-efficacy (GSE) on how stress caused by pregnancy and daily hassle affect the risk of preterm birth (PTB) in women experiencing preterm labor.
Methods
This cross-sectional study included 196 pregnant women experiencing preterm labor before 37 weeks of gestation. We used IBM SPSS Statistics 27 and employed Hayes process macro version 4 (model 1) and hierarchical regression to analyze the moderating effect of GSE on the relationship between pregnancy stress, daily hassle stress, and PTB risk.
Results
Stress caused by pregnancy and daily hassle was positively correlated to PTB risk (r = .54, p < .001; r = .25, p < .001, respectively). While GSE did not significantly correlate with pregnancy stress, it negatively correlated with daily hassle stress (r = - .19, p = .009). GSE significantly moderated the relationship between combined stressors and PTB risk. As GSE levels increased, escalation in PTB risk in response to increasing stress levels was a more pronounced, highlighting a complex interaction between higher GSE levels and response to escalating stress levels. This model accounted for 39.5% of the variance in the PTB risk.
Conclusion
Higher GSE may amplify the impact of stress on PTB risk, rather than mitigate it, which suggests a more nuanced role of GSE in the stress response of pregnant women at risk of preterm labor. GSE should be considered in care strategies, and managing its impact on stress perception and responses in pregnant women is crucial.
Published online Aug 07, 2024.
https://doi.org/10.4040/jkan.24008
Moderating Effect of General Self-Efficacy on the Relationship between Pregnancy Stress, Daily Hassles Stress, and Preterm Birth Risk in Women Experiencing Preterm Labor: A Cross-Sectional Study
Abstract
Purpose
This study investigated the moderating role of general self-efficacy (GSE) on how stress caused by pregnancy and daily hassle affect the risk of preterm birth (PTB) in women experiencing preterm labor.
Methods
This cross-sectional study included 196 pregnant women experiencing preterm labor before 37 weeks of gestation. We used IBM SPSS Statistics 27 and employed Hayes process macro version 4 (model 1) and hierarchical regression to analyze the moderating effect of GSE on the relationship between pregnancy stress, daily hassle stress, and PTB risk.
Results
Stress caused by pregnancy and daily hassle was positively correlated to PTB risk (r = .54, p < .001; r = .25, p < .001, respectively). While GSE did not significantly correlate with pregnancy stress, it negatively correlated with daily hassle stress (r = − .19, p = .009). GSE significantly moderated the relationship between combined stressors and PTB risk. As GSE levels increased, escalation in PTB risk in response to increasing stress levels was a more pronounced, highlighting a complex interaction between higher GSE levels and response to escalating stress levels. This model accounted for 39.5% of the variance in the PTB risk.
Conclusion
Higher GSE may amplify the impact of stress on PTB risk, rather than mitigate it, which suggests a more nuanced role of GSE in the stress response of pregnant women at risk of preterm labor. GSE should be considered in care strategies, and managing its impact on stress perception and responses in pregnant women is crucial.
INTRODUCTION
Preterm is defined as babies born alive before 37 weeks of gestation. The rate of preterm birth (PTB) ranges from 4% to 16% for babies born in 2020 across different countries. Globally, prematurity is the leading cause of death in children under the age of 5 years [1]. It is a significant public health concern worldwide. In Korea, the rate of PTB has been increasing, with a recorded rate of 9.8% in 2022, showing a 0.6% increase from the previous year and a 1.6-fold increase compared to a decade ago [2]. Among PTB cases, preterm labor accounts for over 40.0% [3].
Preterm labor is characterized by regular uterine contractions accompanied by changes such as cervical dilatation or loss with a minimum cervical dilatation of 2 cm [4]. Maternal stress has been identified as one of the contributing factors to preterm labor [5]. Chronic stress resulting from unresolved stressors over an extended period can have detrimental effects, particularly during pregnancy [6].
Daily stress is defined as mundane hassles, strains, or annoyances associated with routine daily activities and transactions of everyday life. Although daily stress is relatively minor, it has the potential to disrupt the flow of everyday life and add to overall levels of stress [7]. Some researchers have operationally defined prenatal stress as the number of major life events or daily hassles during pregnancy [8]. Increasing attention has been paid to the role of psychosocial factors in the etiology of PTB. Among such factors, stress increases the risk for poor birth outcomes including PTB, so further research is needed on various forms of stress, including chronic stressors, major life events, and daily hassles/perceived stress [9]. It is important to note that any stress perceived by pregnant women can increase the secretion of cortisol and cytokines, which may stimulate prostaglandin secretion and consequently lead to preterm labor [10]. Lifestyle changes in urbanization, health behavior, physical activities, employment, working condition, tobacco use, alcohol use, and illicit drug use can also affect psychosocial stress [11]. Perceived stress refers to feelings or thoughts that an individual has about how much a stress event or situation generates at a given point in time or over a given time period [12]. Perceived pregnancy stress has been identified as a contributing factor to PTB [13]. Impact of life event stressors on preterm birth depends on the timing of stressor and self-perceived stress [14]. Thus, it is crucial to investigate the impact of both pregnancy-specific stress and life event stress on preterm labor. Furthermore, stress tends to have a stronger effect when multiple factors of stress act simultaneously rather than individually [15, 16]. Hence, it is necessary to examine the cumulative effect of pregnancy-specific stress and daily hassles stress.
On the other hand, self-efficacy refers to an individual’s belief in their ability to successfully perform a task and achieve specific results in a given situation [17]. Self-efficacy represents a way to self-control an individual’s emotions which can bring multiple advantages in the area of stress. It is a variable that can reduce stress [18]. Higher level of self-efficacy measured by the general self-efficacy (GSE) scale is associated with lower levels of stress among pregnant women [19, 20, 21, 22]. Therefore, it is essential to measure GSE alongside stress in preterm labor pregnancies. However, to the best of our knowledge, existing studies investigating stress or self-efficacy [19, 22] have primarily focused on pregnancy-specific stress, neglecting the examination of daily hassles stress. Additionally, few studies have explored the moderating effect of GSE on stress in preterm labor pregnancy.
Thus, this study aimed to investigate the moderating effect of GSE in pregnant women experiencing preterm labor. By examining the relationship between pregnancy stress, daily hassles stress, and PTB risk, whether GSE might have a protective effect in mitigating the impact of stress on PTB risk was determined. Understanding the moderating effect of GSE in this context can provide valuable insights to healthcare providers in developing interventions and support strategies to reduce PTB risk in preterm labor women.
METHODS
1. Study design
This descriptive study aimed to examine the moderating effect of GSE on the relationship between pregnancy stress, daily hassles stress, and PTB risk in cases of preterm labor pregnancy.
2. Subjects
In this study, pregnant women who had received prenatal care at a women’s hospital or obstetrics and gynecology department and who were diagnosed with preterm labor by an obstetrician were recruited. The recruitment was conducted through an online platform called ‘Momsholic baby’ cafe. Inclusion criteria were: pregnant women who were less than 37 weeks pregnant and diagnosed with preterm labor. Exclusion criteria were: pregnant women who were not diagnosed with preterm labor and those who were more than 37 weeks pregnant.
To determine the required sample size, the G-power 3.1.9.4 program [23] was utilized. Based on a multiple regression analysis with a significance level (α) of .05, a power (1 − β) of .95, and an effect size of 0.15 [24], the minimum sample size required was calculated to be 172. Considering a potential dropout rate of 14.0%, a total of 200 participants were needed. Data collection was conducted through a Google survey using the link provided (https://forms.gle/7RtEpm7NUbqSUHzM8). Collected 200 data were reviewed. Duplicate answers and insufficient data (4 data) were excluded. Ultimately, a total of 196 datasets were included in the analysis, which satisfied the required sample size for multiple regression analysis.
3. Measures
Demographic characteristics assessed in the survey included age, education level, occupation, marital status, and religion. Obstetrical data items were focused on factors such as planned pregnancy, natural pregnancy, parity, history of PTB, history of abortion, and diagnosis of pregnancy complications, among others.
1) Pregnancy stress
The pregnancy stress scale developed by Kim & Chung [25] had eight subscales and a total of 43 items. These subscales were: physical and psychological change (S1), coping in daily life (S2), health of the mother and baby (S3), maternal role (S4), family support (S5), health care service (S6), and social atmosphere (S7), and reconciliation of work life (S8). After excluding 7 items of S8, a total of 36 items were surveyed. Participants evaluated these items using a Likert scale, with response options of ‘not at all’, ‘somewhat’, ‘very much’, and ‘very much so’ (scores of 1, 2, 3, and 4, respectively). Higher scores indicated higher levels of pregnancy stress. During the development of this scale, the reliability using Cronbach’s α coefficient was found to be .85 [25]. In the present study, the Cronbach’s α coefficient was found to be .91.
2) Daily hassles stress
For the measurement of daily hassles, Kim [26] has adapted the scale originally developed by DeLongis et al. [27]. This scale consisted of a total of 36 items. It aimed to assess stress experienced in the past 24 hours in response to various daily life events, including interpersonal relationships, household chores, environment, politics, social issues, and so on.
Each question was measured with a 4-point Likert scale, with a higher score meaning a higher level of daily stress. Response options ranged from ‘not at all’ to ‘very much so’, with a score of 4 assigned to ‘very much so’. At the time of the development of this scale, the reliability of the scale had a Cronbach’s α of .92 [26]. In the present study, the Cronbach’s α was .93.
3) General self-efficacy
GSE was measured using the GSE scale adapted for Koreans [28] based on the original one developed by Schwarzer & Jerusalem [29]. The adapted scale consisted of a total of 10 items. Each question was rated on a 4-point Likert scale, ranging from ‘not at all’ to ‘very much so’. A higher score indicated a higher level of GSE. During the development of the scale, Cronbach’s α was .90 [28]. In the present study, the Cronbach’s α coefficient was .78.
4) Preterm birth risk
PTB risk assessment scale used in this study was developed by Kim [30]. It consisted of a total of 23 items. Each item was assessed using a 4-point Likert scale, where participants rated their responses as ‘not at all’, ‘somewhat so’, ‘quite so’, and ‘very much so’ with corresponding scores of 0, 1, 2, and 3 points, respectively. A higher score of the scale indicated a higher risk of PTB. During the development of the scale, Cronbach’s α was .85 [30], and it was .91 in this study.
5) Data collection
Data collection for this study was conducted using non-face-to-face approach to adhere to quarantine measures during the COVID-19 pandemic. The research protocol received approval from the Institutional Review Board (IRB) before performing data collection. Data collection period spanned from August 21, 2021 to September 18, 2021.
To recruit participants, researchers utilized the ‘Momsholic baby’ cafe, a well-known online community for pregnant women. We announced the study purpose and instructions on how to participate in the survey on the cafe’s platform. The ‘Mom’s Holic Baby’ cafe has a significant user base, with approximately 3.06 million registered members as of November 2021. It serves as a popular online community for topics related to pregnancy, childbirth, and childcare, with an average of 12 million monthly search views in October 2021. The cafe boasts around 350,000 posts, making it a representative and active platform in the field. It is important to note that the cafe primarily caters to a female audience. Its membership is limited to individuals born after 1972 and before 2003. The platform allows posting of surveys for non-commercial research purposes, aligning with goals of this study.
For the response method, pregnant women who voluntarily agreed to participate after reading the notice were directed to access the survey link to complete the survey. The first screen of the survey provided a clear description of the purpose and methodology of this study. Participants were then asked to indicate their decision to either ‘agree’ or ‘disagree’ to participate in the survey. Subsequently, participants who agreed to participate proceeded to the survey. For the next screen, the criteria for selecting and excluding study subjects were presented and participants were required to confirm their eligibility by selecting appropriate options. Specifically, participants had to affirm that they were receiving prenatal care at a women’s hospital or obstetrics and gynecology department and that they were pregnant women diagnosed with preterm labor by an obstetrician and were under 37 weeks of pregnancy. Only those who met these criteria were included in this study. The survey was closed once the desired number of subjects required for the study was reached.
6) Statistical analysis
Data collected for this study were analyzed using IBM SPSS Statistics 27 (IBM Co.). General and obstetric characteristics of subjects were described using frequency, percentage, mean, and standard deviation. Descriptive statistics, including mean and standard deviation, were used to describe levels of pregnancy stress, daily hassles stress, GSE, and PTB risk among subjects. Correlations among pregnancy stress, daily hassles stress, GSE, and PTB risk were examined using Pearson’s correlation coefficient.
Differences in pregnancy stress, daily hassles stress, GSE, and PTB risk based on general and obstetric characteristics of subjects were analyzed using independent t-tests and one-way analysis of variance. Post hoc tests such as the Scheffé test were performed to determine group differences.
To examine the moderating effect of GSE on relationships between pregnancy stress, daily hassles stress, and PTB risk, hierarchical regression analysis was conducted. Furthermore, we utilized the Hayes process macro version 4 with model 1, a statistical tool specifically designed for investigating moderation effects.
7) Ethical considerations
This study obtained approval from the IRB of Soonchunhyang University (IRB No. 1040875-202105-SB-048) prior to conducting this research. Subjects were provided with a clear explanation of this study’s purpose and methodology. They were informed that collected data would be used solely for research purposes and that their anonymity would be maintained. Participants who agreed to participate in the online survey were required to confirm their consent by checking a checkbox on the consent form before proceeding to answer the questionnaire.
RESULTS
1. General & obstetric characteristics of subjects
Subjects included in this study were diagnosed with preterm labor before 37 weeks (between 20 weeks and 36 weeks 6 days of gestation) by obstetrician. Average age of subjects was 32.7 ± 4.07 years. Among study participants, 149 (76.0%) were in their 30s, 36 (18.4%) were in their 20s, and 11 (5.6%) were in their 40s. Of all subjects (n = 196), 79 (40.3%) had a job and 76 (38.8%) had a religion. In terms of education level, 163 (83.2%) had a college degree or higher.
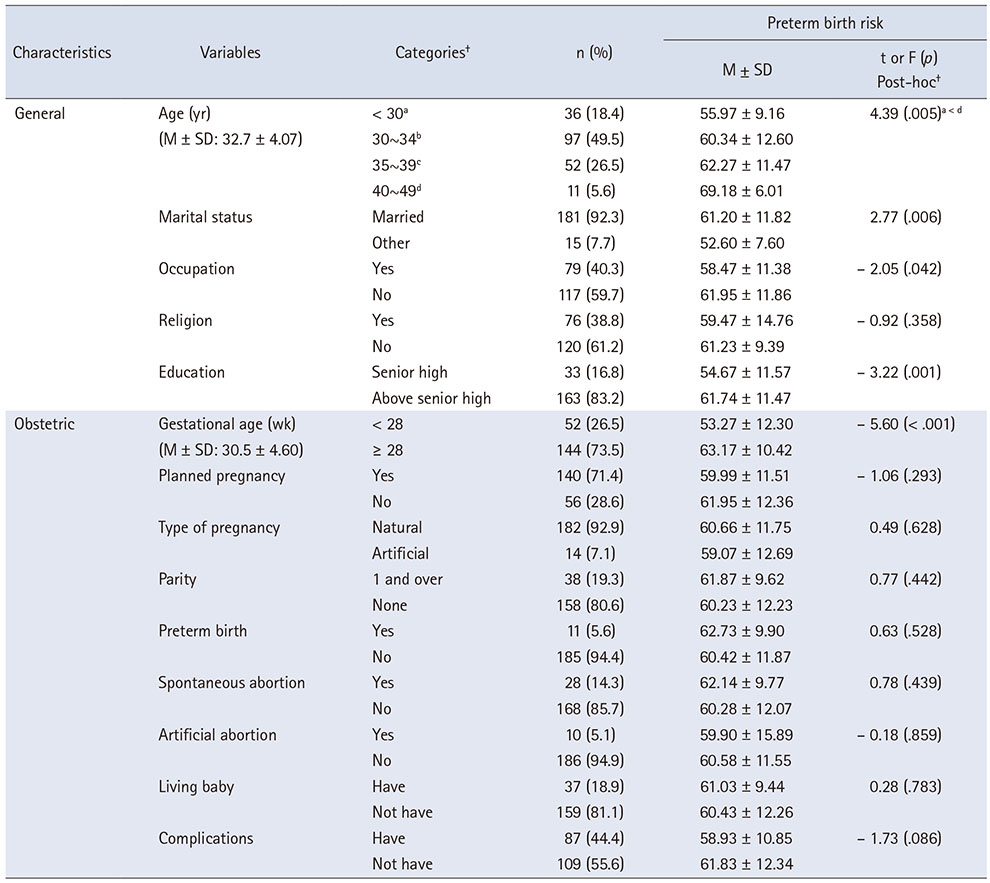
Regarding obstetric characteristics, the average gestational age was 30.5 ± 4.6 weeks. Among participants, 140 (71.4%) reported having planned pregnancies, 182 (92.9%) had natural pregnancies, and 14 (7.1%) had artificial pregnancies. Among all subjects, 87 (44.4%) experienced pregnancy complications. Gestational diabetes (n = 29, 14.8%) was the most common complication reported, followed by gestational hypertension (n = 15, 7.7%), cervical incompetence (n = 11, 5.6%), severe anemia requiring drug treatment other than iron supplements (n = 9, 4.6%), placenta previa (n = 5, 2.6%), and premature rupture of membrane (n = 4, 2.0%) (Table 1).
Table 1
Differences of Preterm Birth Risk by General and Obstetric Characteristics (N = 196)
2. Pregnancy stress, daily hassles stress, general self-efficacy, and preterm birth risk
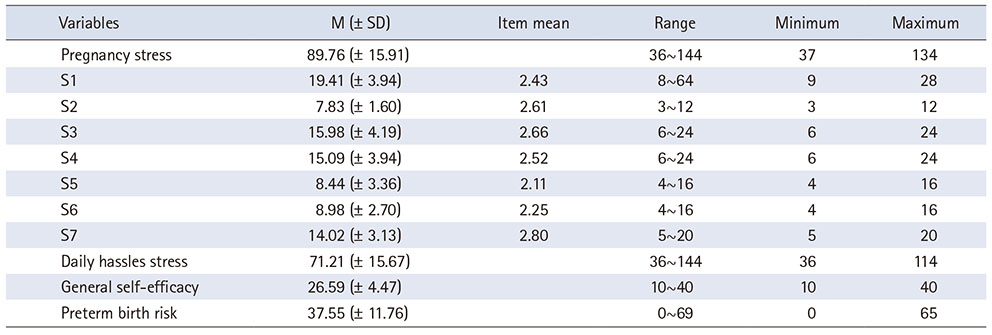
Average scores of variables were as follows: 89.76 ± 15.91 points for pregnancy stress, 71.21 ± 15.67 points for daily hassles stress, 26.59 ± 4.47 points for GSE, and 37.55 ± 11.76 points for PTB risk. When examining each subscale of pregnancy stress, average scores were as follows: S1, 19.41 ± 3.94; S2, 7.83 ± 1.60; S3, 15.98 ± 4.19; S4, 15.09 ± 3.94; S5, 8.44 ± 3.36; S6, 8.98 ± 2.70; and S7, 14.02 ± 3.13. Among these subscales, S7 had the highest mean score of 2.80 points, indicating a higher level of stress related to social atmosphere. On the other hand, S5 had the lowest mean score of 2.11 points, suggesting relatively lower stress related to family support (Table 2).
Table 2
Pregnancy Stress, Daily Hassles Stress, General Self-Efficacy and Preterm Birth Risk (N = 196)
3. Correlation among pregnancy stress, daily hassles stress, general self-efficacy, and preterm birth risk
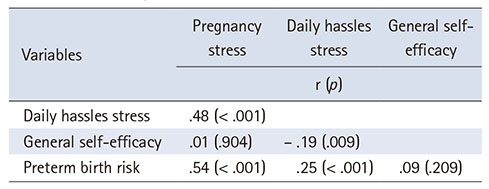
PTB risk had a significant positive correlations with pregnancy stress (r = .54, p < .001) and daily hassles stress (r = .25, p < .001). There was a weak negative correlation between GSE and daily hassles stress (r = − .19, p = .009) (Table 3).
Table 3
Correlations among Pregnancy Stress, Daily Hassles Stress, General Self-Efficacy, and Preterm Birth Risk (N = 196)
4. Differences of preterm birth risk by general and obstetric characteristics
There was a significant difference in PTB risk by age (t = 4.39, p = .005). Post-hoc analysis using the Scheffé test revealed that PTB risk was significantly higher in pregnant women aged 40 years or older than in those in their 20s (less than 30 years old). PTB risk was also found to significantly different by marital status (t = 2.77, p = .006), job status (t = − 2.05, p = .042), and education level (t = −3.22, p = .001).
When PTB risk was analyzed according to obstetrical characteristics, it was significantly higher in pregnant women who were over 28 weeks of pregnant than in those who were under 28 weeks pregnant (63.17 vs. 53.27, t = −5.60, p < .001) (Table 1).
5. Moderating effects of general self-efficacy on the relationship between pregnancy stress, daily hassles stress, and preterm birth risk
To examine moderating effects of GSE on relationships between pregnancy stress and daily hassles stress, and PTB risk, we used a hierarchical regression first and then Hayes process macro version 4 with model 1. Standardized scores were used to address multicollinearity among independent and control variables. The Durbin-Watson index for measuring autocorrelation between errors indicated no significant autocorrelation. Tolerance limit and variance inflation factor showed no multicollinearity.
After controlling for demographic variables and gestational age, the moderating effect of GSE on the relationship between pregnancy stress and PTB risk was significant (β = .20, p = .001), explaining 43.2% of the variance (Supplementary Table 1). Similarly, the moderating effect of GSE on the relationship between daily hassles stress and PTB risk was also significant (β = .36, p < .001), accounting for 36.4% of the variance (Supplementary Table 2). Furthermore, when the interaction between pregnancy stress and daily hassles stress was examined, the moderating effect of GSE was significant (β = − .39, p < .001, F = 15.28, p < .001), explaining for 36.9% of the variance (Supplementary Table 3).
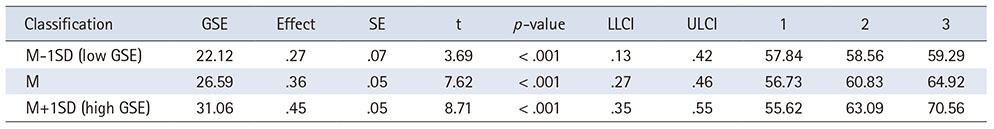
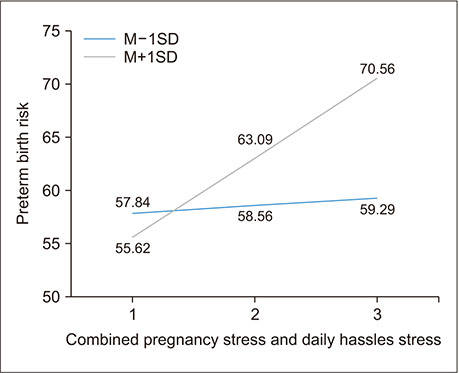
In the final step, a comparison of the regression lines representing the moderating effect based on mean score of GSE was conducted using Hayes process macro version 4 with model 1. The analysis revealed that GSE significantly moderates the relationship between combined pregnancy stress and daily hassles stress and PTB risk. Key findings include, with increasing levels of GSE (from low to high), there is a notable escalation in the effect of stress on the PTB risk, indicated by effect sizes of 22.12 for low GSE, 26.59 for mean GSE, and 31.06 for high GSE, all with p < .001 (Table 4).
Table 4
Moderating Effect of General Self-Efficacy on Impact of Pregnancy Stress and Daily Hassles Stress on Preterm Birth Risk by Hayes Process Macro Version 4 (N = 196)
The regression analysis depicted through Figure 1 further illustrated this relationship, showing a gradual increase in PTB risk with stress levels in the low GSE group and a more pronounced increase in the high GSE group. Specifically, the PTB risk scores for the low GSE group increased modestly from 57.84 to 59.29 as stress levels rose. In contrast, for the high GSE group, the PTB risk scores started lower at 55.62 but surged significantly to 70.56 with increasing stress. These results underscore the moderating influence of GSE on the stress-PTB risk nexus, demonstrating a complex interaction where higher GSE levels correspond to a more pronounced response to escalating stress levels in terms of PTB risk (Table 4, Figure 1). This model accounted for 39.5% of the variance in PTB risk.
Figure 1
Regression lines of low and high general self-efficacy groups showing a moderating effect of general self-efficacy.
DISCUSSION
The primary goal of this study aimed to investigate moderating effects of GSE on the relationship between pregnancy stress and daily hassles stress, and PTB risk in women experiencing preterm labor. Our results revealed a several key insights that deepen our understanding of these interactions.
The mean age of women experiencing preterm labor in this study was 32.7 years. In terms of the relationship between age and preterm labor, we observed a significantly higher PTB risk in women aged 40 years or older compared to those in their 20s. This result supports previous research suggesting increased PTB risks associated with advanced maternal age [31, 32]. These findings underscore the need for healthcare providers to tailor monitoring and intervention strategies for older pregnant women.
Next, let’s discuss the impact of stress on PTB risk. According to Bandura’s theory of self-efficacy, higher GSE may lead individuals to perceive stressful situations as more manageable, thereby potentially mitigating the adverse effects of stress [17]. However, our study suggests this relationship can be complex and may not always act protectively, especially under high stress levels. In this study, both pregnancy and daily hassles stress contribute significantly to PTB risk, with GSE playing a moderating role. Interestingly, higher levels of GSE were associated with an amplified response to stress, particularly at higher stress levels, potentially supporting the idea that high GSE could alter stress responses [33], challenging the conventional view of GSE as solely protective. This suggests that while GSE can enhance coping capacities, it may also exacerbate stress responses under high-stress conditions, leading to increased PTB risk.
On the other hand, comparing daily hassles stress with prior studies was challenging due to the limited research. However, our findings suggest that daily hassles stress is more pronounced in pregnancies with preterm labor compared to general adult women [34]. This emphasized the need to address both pregnancy-specific and daily hassles stress in prenatal care. Furthermore, it is worth noting that various terms such as "daily life stress", "life stress", and "life event stress" have been used interchangeably with "daily hassles stress" [27]. Therefore, researchers should strive to unify these terminologies and develop a suitable scale specifically designed for pregnant women, including those experiencing preterm labor.
Regarding the relationship between both stresses and GSE, daily hassles stress showed a negative correlation with GSE, while pregnancy stress exhibited no significant relationship with GSE in our study. This finding aligned with a study by Pasha et al. [22]. Previous studies [22, 35] have demonstrated that individuals with higher GSE tend to perceive stress as being lower, different from this study results.
The complex role of GSE observed in our study suggests a dual-edged nature: GSE can be beneficial under lower stress conditions but may intensify stress responses as stress levels escalate. This finding indicates that interventions aimed at enhancing GSE should be carefully tailored to individual stress levels and coping mechanisms.
Given the complex interplay between GSE, stress, and PTB risk, further research should explore additional factors influencing this relationship and develop interventions that adjust to the varying impacts of GSE. Additionally, our study highlights the importance of comprehensive stress management strategies in prenatal care that consider individual differences in GSE.
However, it is crucial to recognize certain limitations of our study. This study’s methodology, particularly the exclusion of specific scale items and the use of a general rather than a childbirth-specific efficacy scale, may limit the applicability of our findings across all cases of preterm labor.
Additionally, employing a GSE scale rather than a childbirth efficacy scale might limit the applicability of our results across all preterm labor cases. Future research should consider incorporating a childbirth efficacy scale [36] to facilitate a direct comparison between childbirth efficacy and GSE. Despite these limitations, our study is pioneering in examining the intricate role of GSE in the stress-PTB risk dynamic, paving the way for further exploration of this important area.
Implications for practice
This study indicated that higher levels of GSE may amplify the stress-related risks of PTB rather than mitigate them. Healthcare professionals should consider this complex role of GSE when integrating strategies aimed at managing stress in pregnant women facing preterm labor. These strategies might need to focus on understanding how individual differences in GSE influence stress perception and responses, potentially leading to tailored interventions that address these nuances.
Our findings enrich the understanding of GSE’s role in navigating the complexities of preterm labor, highlighting the importance of considering individua differences like GSE in evaluating and addressing the stress factors associated with pregnancy. It is crucial to conduct further investigations into other elements that may affect the interplay between stress and PTB, including a deeper look at how GSE can be effectively managed or supported in this population.
CONCLUSION
Our research explored how pregnancy stress and daily hassles stress affect women facing preterm labor and examined the role of GSE plays in moderating these stresses and their combined impact on the risk of PTB. Contrary to expectations, higher GSE was found to amplify the effect of stress on PTB risk. This revelation prompts several recommendations for clinical practice and further study.
Firstly, there’s a need to investigate how different levels of GSE impact the stress response in such contexts, which could inform targeted support and intervention strategies. Secondly, future studies should aim to include a wider range of participants to uncover additional individual and contextual factors affecting PTB risk. Lastly, considering the notable impact of daily hassles stress, identifying and addressing these stressors in tailored ways could be key to managing PTB risk effectively.
In summary, this study enhances our understanding of the interactions among stress, GSE, and PTB risk in the context of preterm labor. These insights pave the way for healthcare providers and researchers to develop precise interventions and support systems, aiming to improve outcomes for women susceptible to PTB.
SUPPLEMENTARY MATERIALS
Supplementary data to this article can be found online at https://doi.org/10.4040/jkan.24008.
Moderating Effect of General Self-Efficacy on Impact of Pregnancy Stress on Preterm Birth Risk (N = 196)Supplementary Table 1
Moderating Effect of General Self-Efficacy on Impact of Daily Hassles Stress on Preterm Birth Risk (N = 196)Supplementary Table 2
Moderating Effect of General Self-Efficacy on Impact of Pregnancy Stress and Daily Hassles Stress on Preterm Birth Risk by Hierachical Regression (N = 196)Supplementary Table 3
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
FUNDING:This work was supported by Soonchunhyang University and Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Thesis: NRF No. 2019R1F1A104579912- 3rd year; Restructure and reanalysis: 2023R1A2C1003355).
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Cho H & Kim J.
Data curation or/and Analysis: Cho H & Kim J.
Funding acquisition: Kim J.
Investigation: Cho H & Kim J.
Project administration or/and Supervision: Kim J.
Resources or/and Software: Cho H & Kim J.
Validation: Cho H & Kim J.
Visualization: Cho H & Kim J.
Writing original draft or/and Review & Editing: Cho H & Kim J.
ACKNOWLEDGEMENTS
We appreciate all women who participated in this study. For written English check, we used OpenAI. (2024). ChatGPT (4) [Large language model]. https://chat.openai.com.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
World Health Organization (WHO). Preterm birth [Internet]. WHO; c2023 [cited 2024 Mar 28].Available from: https://www.who.int/news-
room/fact- sheets/detail/preterm- birth.
-
-
Statistics Korea. Birth statistics for 2022 [Internet]. Statistics Korea; c2023 [cited 2024 Mar 28].Available from: https://kostat.go.kr/board.es?mid=a10301010000&bid=204&list_
no=426806&act=view&mainXml=Y.
-
-
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. Practice bulletin No. 171: Management of preterm labor. Obstetrics and Gynecology 2016;128(4):e155–e164. [doi: 10.1097/aog.0000000000001711]
-
-
Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS. In: Williams obstetrics. 24th ed. McGraw-Hill; 2014.
-
-
Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: An expert review. American Journal of Obstetrics & Gynecology MFM 2020;2(4):100229 [doi: 10.1016/j.ajogmf.2020.100229]
-
-
Upchurch Sweeney CR. Daily stress. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. Springer; 2013. pp. 537-538.
-
-
Patel I, Dev A. What is prenatal stress? A scoping review of how prenatal stress is defined and measured within the context of food insecurity, housing instability, and immigration in the United States. Women’s Health 2023;19:17455057231191091 [doi: 10.1177/17455057231191091]
-
-
McDonald SW, Kingston D, Bayrampour H, Dolan SM, Tough SC. Cumulative psychosocial stress, coping resources, and preterm birth. Archives of Women’s Mental Health 2014;17(6):559–568. [doi: 10.1007/s00737-014-0436-5]
-
-
Tanpradit K, Kaewkiattikun K. The effect of perceived stress during pregnancy on preterm birth. International Journal of Women’s Health 2020;12:287–293. [doi: 10.2147/ijwh.s239138]
-
-
Phillips AC. Perceived stress. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. Springer; 2013. pp. 1453-1454.
-
-
Sanchez SE, Puente GC, Atencio G, Qiu C, Yanez D, Gelaye B, et al. Risk of spontaneous preterm birth in relation to maternal depressive, anxiety, and stress symptoms. The Journal of Reproductive Medicine 2013;58(1-2):25–33.
-
-
Cha S, Masho SW. Preterm birth and stressful life eventsErez OPreterm birth [Internet]. IntechOpen; 2013 [cited 2023 Dec 10].Available from: https://www.intechopen.com/chapters/42170.
-
-
Orr JA, Vinebrooke RD, Jackson MC, Kroeker KJ, Kordas RL, Mantyka-Pringle C, et al. Towards a unified study of multiple stressors: Divisions and common goals across research disciplines. Proceedings of the Royal Society B: Biological Sciences 2020;287(1926):20200421 [doi: 10.1098/rspb.2020.0421]
-
-
Sebastian V. A theoretical approach to stress and self-efficacy. Procedia - Social and Behavioral Sciences 2013;78:556–561. [doi: 10.1016/j.sbspro.2013.04.350]
-
-
Tsai YJ, Hsu YY, Hou TW, Chang CH. Effects of a web-based antenatal care system on maternal stress and self-efficacy during pregnancy: A study in Taiwan. Journal of Midwifery & Women’s Health 2018;63(2):205–213. [doi: 10.1111/jmwh.12685]
-
-
Ngai FW, Chan SW. Stress, maternal role competence, and satisfaction among Chinese women in the perinatal period. Research in Nursing & Health 2012;35(1):30–39. [doi: 10.1002/nur.20464]
-
-
Reece SM, Harkless G. Self-efficacy, stress, and parental adaptation: Applications to the care of childbearing families. Journal of Family Nursing 1998;4(2):198–215. [doi: 10.1177/107484079800400206]
-
-
Cohen J, Cohen P, West SG, Aiken LS. In: Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Routledge; 2002. pp. 536.
-
-
Kim CH. Relationship of the daily hassles, stress appraisal and coping strategies with emotional experiences. Korean Journal of Counseling and Psychotherapy 1995;7(1):44–69.
-
-
Lee YM, Schwarzer R, Jerusalem M. Korean adaptation of the general self-efficacy scale [Internet]. Freie Universität Berlin; 1994 [cited 2021 Nov 20].Available from: http://userpage.fu-
berlin.de/~health/korean.htm.
-
-
Schwarzer R, Jerusalem M. The general self-efficacy scale (GSE) [Internet]. Freie Universität Berlin; 1995 [cited 2021 Nov 20].Available from: http://userpage.fu-
berlin.de/~health/engscal.htm.
-
-
Ju KS, Kim HS. Association between maternal age and complications of pregnancy in primipara. Journal of Health Informatics and Statistics 2022;47(4):349–356. [doi: 10.21032/jhis.2022.47.4.349]
-
-
Dolatian M, Mirabzadeh A, Forouzan AS, Sajjadi H, Alavimajd H, Mahmoodi Z, et al. Relationship between structural and intermediary determinants of health and preterm delivery. Journal of Reproduction & Infertility 2014;15(2):78–86.
-
-
Jerusalem M, Schwarzer R. Self-efficacy as a resource factor in stress appraisal processes. In: Schwarzer R, editor. Self-Efficacy: Thought Control of Action. Taylor & Francis; 1992. pp. 195-213.
-
-
Ryu Y. In: Korean adult women’s mindfulness effect on daily hassles: Verification of the intermediate effect of self-compassion and anger expression [master’s thesis]. Hwaseong: Neungin Graduate School; 2020. pp. 1-69.
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

