Search
- Page Path
- HOME > Search
- Variables influencing digital health literacy in older adults: a systematic review and meta-analysis
- Jin Hwa Park, Eun Ju Mun
- J Korean Acad Nurs 2025;55(4):651-667. Published online November 27, 2025
- DOI: https://doi.org/10.4040/jkan.25112
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to synthesize existing evidence on digital health literacy (DHL) among older adults and to estimate the associations between related influencing factors through a systematic literature review and meta-analysis.
Methods
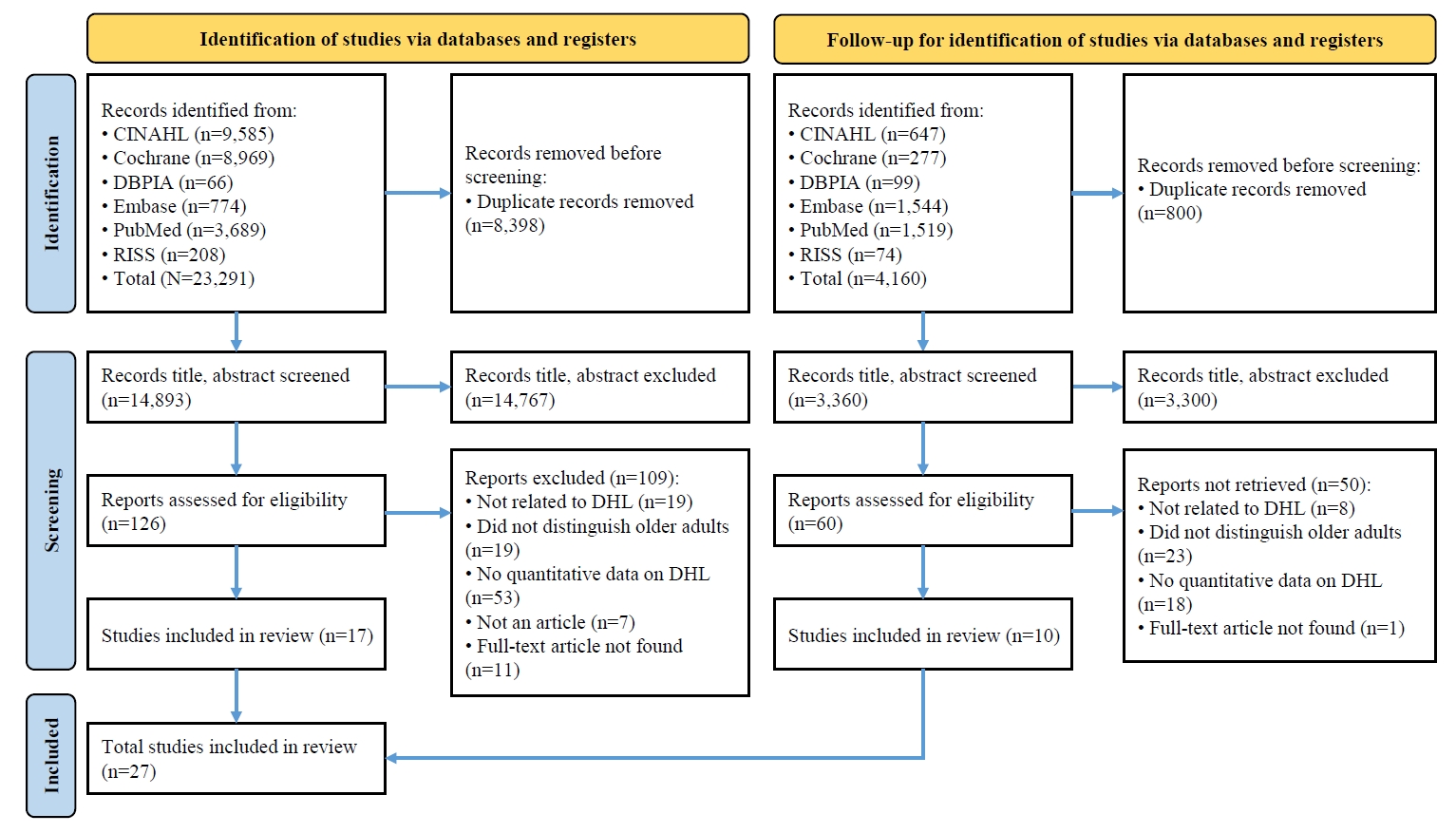
A systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines. Literature searches were performed across PubMed, EMBASE, Cochrane Library, CINAHL, RISS, and DBPIA. The search and screening process was conducted from December 24, 2023, to March 31, 2025. Effect sizes (ESr) using correlation coefficient for each variable were calculated, and meta-analyses were performed using Microsoft Excel and R version 4.3.1.
Results
Forty-seven variables were identified, including two demographic, six physical, six behavioral, 23 psychosocial, and 10 cognitive factors. Meta-analysis results showed that physical, behavioral, psychosocial, and cognitive factors had significant effects on DHL. Among these, digital information level (ESr=.62; 95% confidence interval [CI], 0.55 to 0.69) within the cognitive domain and technophobia (ESr=−.55; 95% CI, −0.47 to −0.40) within the psychosocial domain demonstrated the largest ESr.
Conclusion
Among factors influencing DHL, digital information level and technophobia showed the strongest associations. These findings suggest that improving DHL in older adults requires a dual approach targeting both cognitive and psychosocial dimensions—enhancing digital information skills while reducing technophobia—to effectively support digital engagement and health empowerment in this population (PROSPERO registration number: CRD42023487486).
- 1,246 View
- 128 Download

- Risk factors for the readmission of patients with diabetic ketoacidosis: a systematic review and meta-analysis
- Hyerim Ji, Sun-Kyung Hwang
- J Korean Acad Nurs 2025;55(4):634-650. Published online November 21, 2025
- DOI: https://doi.org/10.4040/jkan.25072
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to identify risk factors associated with the readmission of patients with diabetic ketoacidosis (DKA) through a systematic review and meta-analysis.
Methods
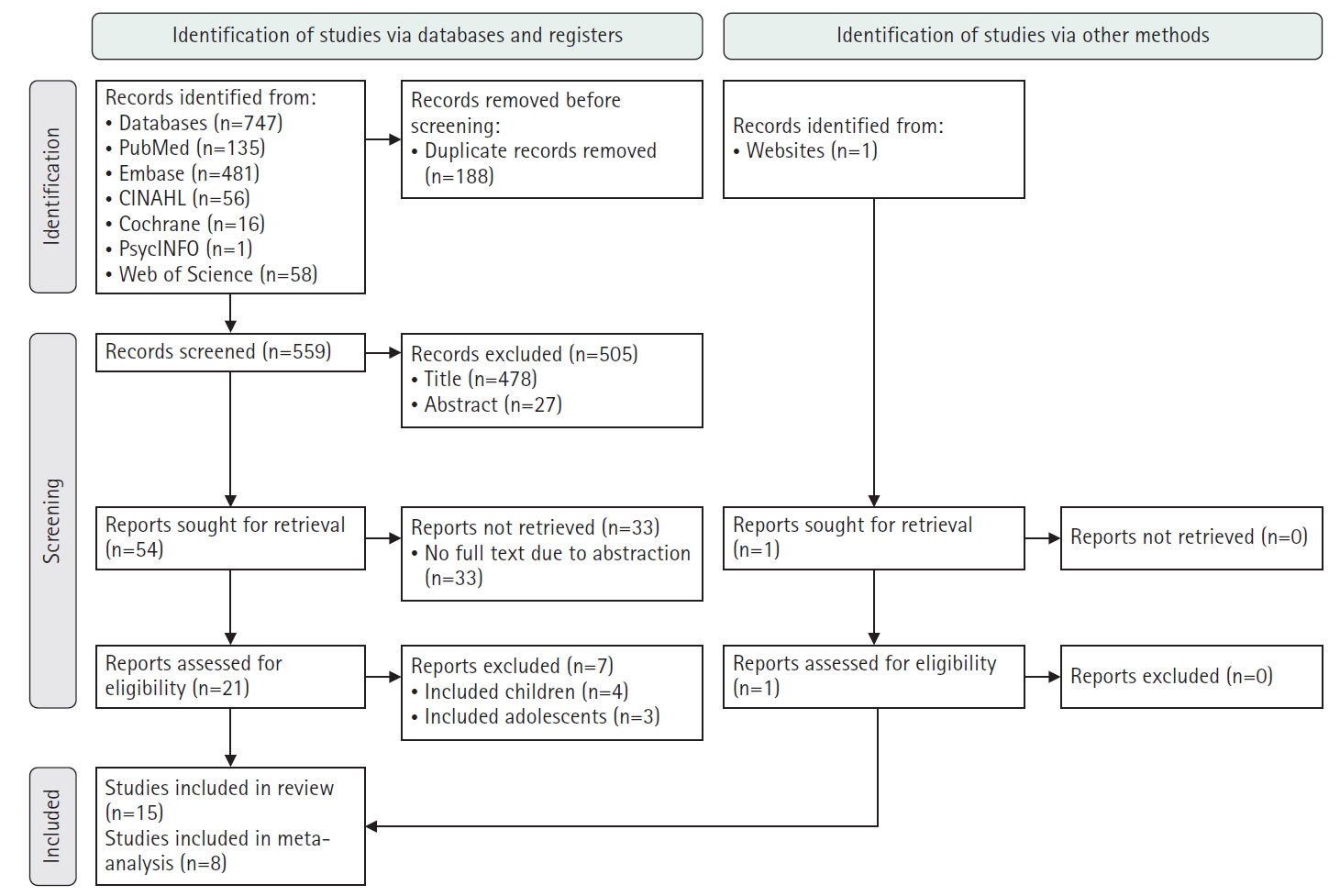
A systematic literature review was conducted in accordance with the PRISMA guidelines. Relevant studies were retrieved from international databases (PubMed, EMBASE, Cochrane Library, CINAHL, PsycINFO, and Web of Science) and Korean databases (RISS, KoreaMed, KMbase, KISS, and DBpia). Study quality was evaluated using the Newcastle-Ottawa Scale. Meta-analysis was performed using a random-effects model with the Hartung-Knapp-Sidik-Jonkman adjustment to account for the limited number of studies and heterogeneity.
Results
Fifteen studies were included in the review, and eight were eligible for meta-analysis. From the systematic review, 21 risk factors for DKA readmission were identified and categorized into five domains: demographic, socioeconomic, diabetes-related, comorbidity, and health-behavioral factors. In the meta-analysis, significant risk factors included low income, psychiatric disorders, and discharge against medical advice.
Conclusion
This study demonstrates that DKA readmissions result from the complex interplay of multiple clinical and social factors. By identifying these risk factors and suggesting risk-stratification criteria, the findings may support the development of tailored interventions, such as self-management education, integrated mental health care, structured discharge planning, and coordinated post-discharge follow-up.
- 1,173 View
- 168 Download

- Effects of Health Education Using Virtual Reality for Adolescents: A Systematic Review and MetaAnalysis
- SoMi Park, ChaeWeon Chung, Gaeun Kim
- J Korean Acad Nurs 2023;53(2):177-190. Published online April 30, 2023
- DOI: https://doi.org/10.4040/jkan.23003
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to evaluate the effects of health interventions using virtual reality (VR) on improving knowledge, attitudes, and skills; and inducing behavioral change among adolescents.
Methods
This study is a systematic review and meta-analysis following PRISMA guidelines. We searched Cochrane, MEDLINE, Embase, CINAHL, Scopus, Web of Science, and Korean databases between database inception and April 10, 2021. Based on heterogeneity, a random- or fixed-effects model was used, as appropriate, to calculate effect sizes in terms of the standardized mean difference (SMD) and odds ratio (OR). Studies were selected if they verified the effects of health education using VR on adolescents; there was an appropriate control group; and if the effects of education were reported in terms of changes in knowledge, attitudes, skills, or behaviors.
Results
This analysis included six studies (n = 1,086). The intervention groups showed greater responses in knowledge and attitudes (SMD = 0.57, 95% confidence interval (CI) [0.12 to 1.02]), skills related to health behavior (SMD = -0.45, 95% CI [-0.71 to -0.19]), and behavioral change after 12 months (OR = 2.36, 95% CI [1.03 to 5.41]).
Conclusion
The results confirm the effectiveness of health interventions using virtual reality (VR). Although the analysis include a small number of studies, a case can be made for health interventions using VR to be utilized as educational methods and strategies to prevent risky behaviors among adolescents. -
Citations
Citations to this article as recorded by- Implementation of a Childcare-Based Obesity Prevention Program for Vulnerable Families During the COVID-19 Pandemic: Lessons for School Nurses
Jiyoung Park, Gill ten Hoor, Seohyun Won, Gahui Hwang, Sein Hwang, Siew Tiang Lau
The Journal of School Nursing.2025; 41(5): 579. CrossRef - Development and Evaluation of a Virtual Reality Intervention for Reducing Exposure to Endocrine Disruptors in Female Adolescents: A Pilot Study
SoMi Park, Yun Jeong Hwang, ChaeWeon Chung
Journal for Specialists in Pediatric Nursing.2025;[Epub] CrossRef - Chinese nurses’ perspectives on child-friendly healthcare practice assessment: a qualitative study
Wei Xiao Huang, Mei Chan Chong, Li Yoong Tang, Xiao Xia Liu, Mei Fang, Yun Yun Shen, Xiao Li Guo
BMC Nursing.2025;[Epub] CrossRef - Enhancing anatomy education with virtual reality: integrating three-dimensional models for improved learning efficiency and student satisfaction
Shuliang Niu, Jinlong Zhang, Jiang Lin, Binbin Wang, Jie Yan
Frontiers in Medicine.2025;[Epub] CrossRef
- Implementation of a Childcare-Based Obesity Prevention Program for Vulnerable Families During the COVID-19 Pandemic: Lessons for School Nurses
- 4,410 View
- 102 Download
- 4 Web of Science
- 4 Crossref

- Effect of Digital Health Interventions on Psychotic Symptoms among Persons with Severe Mental Illness in Community: A Systematic Review and Meta-Analysis
- Eunjin Oh, Moonhee Gang
- J Korean Acad Nurs 2023;53(1):69-86. Published online February 28, 2023
- DOI: https://doi.org/10.4040/jkan.22121
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to evaluate the effects of digital health interventions on the psychotic symptoms among people with severe mental illness in the community.
Methods
A systematic review and meta-analysis were conducted in accordance with the Cochrane Intervention Research Systematic Review Manual and PRISMA. A literature search was conducted of published randomized controlled trials (RCTs) for digital health interventions from January 2022 to April 2022. RevMan software 5.3 was used for quality assessment and meta-analysis.
Results
A total 14 studies out of 9,864 studies were included in the review, and 13 were included in meta-analysis. The overall effect size of digital health interventions on psychotic symptoms was - 0.21 (95% CI = - 0.32 to - 0.10). Sub-analysis showed that the reduction of the psychotic symptoms was effective in the schizophrenia spectrum group (SMD = - 0.22; 95% CI = - 0.36 to - 0.09), web (SMD = - 0.41; 95% CI = - 0.82 to 0.01), virtual reality (SMD = - 0.33; 95% CI = - 0.56 to - 0.10), mobile (SMD = - 0.15; 95% CI = - 0.28 to - 0.03), intervention period of less than 3 months (SMD = - 0.23; 95% CI = - 0.35 to - 0.11), and non-treatment group (SMD = - 0.23; 95% CI = - 0.36 to - 0.11).
Conclusion
These findings suggest that digital health interventions alleviate psychotic symptoms in patients with severe mental illnesses. However, well-designed digital health studies should be conducted in the future. -
Citations
Citations to this article as recorded by- A Review of Mobile App-Based Psychosocial Intervention for Personal and Clinical Recovery for People With Psychosis
Dowon You, Narae Jeong
Korean Journal of Schizophrenia Research.2024; 27(1): 1. CrossRef
- A Review of Mobile App-Based Psychosocial Intervention for Personal and Clinical Recovery for People With Psychosis
- 2,661 View
- 87 Download
- 1 Crossref

- Effect of Auriculotherapy on Musculoskeletal Pain: A Systematic Review and Meta-Analysis
- Sun Yeob Choi, Yeo Ju Kim, Bomi Kim
- J Korean Acad Nurs 2022;52(1):4-23. Published online February 28, 2022
- DOI: https://doi.org/10.4040/jkan.21121
-
 Abstract
Abstract
 PDF
PDF - Purpose
The aim of this study was to evaluate the effect of auriculotherapy on musculoskeletal pain in adults.
Methods
A total of 885 studies were retrieved from nine databases (PubMed, Scopus, CINAHL, Web of Science, Ovid Medline, Cochrane Library, RISS, KMbase, and KISS). Sixteen studies were selected for meta-analysis, which satisfied the inclusion criteria and the evaluation of risk of bias. Demographic data, auriculotherapy types, intervention characteristics, auricular points, and outcomes related to pain (subjective pain scale, and amount of analgesic) were extracted from all included studies. The effect size of auriculotherapy was analyzed through comprehensive meta analysis 3.0, and the presence of publication bias was analyzed through a funnel plot and Egger’s regression.
Results
The results of the meta-analysis (n = 16) revealed that the auriculotherapy was significantly superior to the control group on present pain in adults (Hedges’ g = - 0.35, 95% Confidence Interval [CI] = - 0.55~- 0.15). According to the results of subgroup analysis, the effect size of auricular acupuncture therapy (Hedges’ g = 0.45, 95% CI = - 0.75~- 0.15) was higher than the auricular acupuncture (Hedges’ g = 0.27, 95% CI = - 0.53~0.00): the longer the intervention period, the greater the effect size.
Conclusion
In this study, auriculotherapy demonstrates a significant reduction in musculoskeletal pain in adults. Therefore, it is necessary to refine the curriculum to include auriculotherapy as a nursing intervention to relieve musculoskeletal pain in adults and encourage its use in clinical settings. -
Citations
Citations to this article as recorded by- Effects of Auricular Acupressure on Nurses’ Perceived Stress, Sleep Quality, and Presenteeism
Hyunseo Sim, Younghee Park
Holistic Nursing Practice.2025; 39(1): 15. CrossRef - Effects of Auricular Acupressure on Pain and Stress in Nursing College Students With Cervical Pain: A Single-Blind Placebo-Controlled Trial
Yuna Cho, Eunmi Cho, Eunseol Cho, Yeonju Chae, Eunkyung Choi, Hyeongyeong Yoon
Pain Management Nursing.2025; 26(1): e59. CrossRef - Effect of Auriculotherapy on Stress: A Systematic Review and Meta-Analysis
Sunyeob Choi, Bomi Kim
Journal of Holistic Nursing.2025; 43(4): 336. CrossRef - Comparative Effectiveness of Ear and Body Acupressure for Postoperative Pain in Elderly Women Following Knee Arthroplasty: A Randomized Trial
Fatemeh Ghanbari, Nahid Rejeh, Tahereh Bahrami, Hooman Yahyazadeh, Kiarash Saatchi
Journal of Integrative and Complementary Medicine.2025; 31(11): 987. CrossRef - Estratégias de adaptação dos profissionais de enfermagem com dor musculoesquelética no trabalho hospitalar: uma revisão sistemática
Jorge Gabriel Tuz-Colli, Yolanda Flores-Peña, Heloisa Ehmke Cardoso dos Santos, Fernanda Ludmilla Rossi Rocha, Maria Helena Palucci Marziale
Revista Latino-Americana de Enfermagem.2025;[Epub] CrossRef - Adaptation strategies for nurses with musculoskeletal pain in hospital work: a systematic review
Jorge Gabriel Tuz-Colli, Yolanda Flores-Peña, Heloisa Ehmke Cardoso dos Santos, Fernanda Ludmilla Rossi Rocha, Maria Helena Palucci Marziale
Revista Latino-Americana de Enfermagem.2025;[Epub] CrossRef - Estrategias de adaptación de los profesionales de Enfermería con dolor musculoesquelético en el trabajo hospitalario: revisión sistemática
Jorge Gabriel Tuz-Colli, Yolanda Flores-Peña, Heloisa Ehmke Cardoso dos Santos, Fernanda Ludmilla Rossi Rocha, Maria Helena Palucci Marziale
Revista Latino-Americana de Enfermagem.2025;[Epub] CrossRef - Adapting and Evaluating a Theory-Driven, Non-Pharmacological Intervention to Self-Manage Pain
Jennifer Kawi, Chao Hsing Yeh, Lauren Grant, Johannes Thrul, Hulin Wu, Paul J. Christo, Lorraine S. Evangelista
Healthcare.2024; 12(10): 969. CrossRef - The State of 21st Century Acupuncture in the United States
Clasina Smith, Bill Reddy, Charis Wolf, Rosa Schnyer, Korina St John, Lisa Conboy, Jen Stone, Lixing Lao
Journal of Pain Research.2024; Volume 17: 3329. CrossRef - The effects of auricular acupressure on blood pressure, stress, and sleep in elders with essential hypertension: a randomized single-blind sham-controlled trial
Bomi Kim, Hyojung Park
European Journal of Cardiovascular Nursing.2023; 22(6): 610. CrossRef
- Effects of Auricular Acupressure on Nurses’ Perceived Stress, Sleep Quality, and Presenteeism
- 2,978 View
- 125 Download
- 10 Web of Science
- 10 Crossref

- Trends of Concept Development in Nursing Published in Korean Journals
- Sumi Lee, Jinhae Lee, Yugyeong Hwang, Il Sun Ko
- J Korean Acad Nurs 2020;50(2):178-190. Published online April 30, 2020
- DOI: https://doi.org/10.4040/jkan.2020.50.2.178
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study was to identify trends of nursing concept development in Korean journal papers to improve accurate understanding of nursing concepts.
Methods
A systematic review of 216 concept development articles published from 1970 to 2018 that met the inclusion criteria was conducted using Research Information Sharing Service (RISS) databases.
Results
The most common method of concept development was Walker and Avant’s concept analysis method, identified in 139 (64.3%) of the 216 studies, followed by 48 examples of hybrid models (22.2%) and 15 examples of evolutionary methods (6.9%). Chinn and Kramer’s method, Norris’s clarification, Wilson’s method, and others were also used. The concepts of “spirituality” and “fatigue” were most frequently analyzed. Among the 139 studies that used Walker and Avant’s concept analysis method, 127 studies (91.4%) applied all the recommended steps; the others applied the recommended steps partially, omitting description of model cases/additional cases, antecedents/consequences, and empirical indicators. Among the studies using the hybrid model, among two (5.7%) did not describe attributes, three (8.5%) did not provide definitions, and 16 (45.7%) did not present empirical indicators in the final stage.
Conclusion
Among concept development studies published in Korean journals, Walker and Avant’s concept analysis method is most commonly used. In case of most studies using Walker and Avant’s method a suitable concept analysis process is applied, but in case of other studies using the other concept development method, a suitable concept analysis process is not applied. Therefore, a suitable concept analysis process must be applied for concept development in nursing research. -
Citations
Citations to this article as recorded by- Concept Analysis of Nurses’ Job Crafting
Sujeong Han, Eunha Jeong
Journal of Korean Academy of Fundamentals of Nursing.2022; 29(3): 375. CrossRef - Concept Analysis of Spiritual Distress in Cancer Patients Using a Hybrid Model
Jin Sook Kim, Il-Sun Ko
Korean Journal of Adult Nursing.2021; 33(2): 169. CrossRef
- Concept Analysis of Nurses’ Job Crafting
- 2,601 View
- 62 Download
- 2 Crossref

- Factors Related to Persistent Postoperative Pain after Cardiac Surgery: A Systematic Review and Meta-Analysis
- Jaewon Bae, Sujin Shin
- J Korean Acad Nurs 2020;50(2):159-177. Published online April 30, 2020
- DOI: https://doi.org/10.4040/jkan.2020.50.2.159
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed at identifying factors related to persistent postoperative pain after cardiac surgery and estimating their effect sizes.
Methods
The literature search and selection was conducted in four different databases (CINAHL, Cochrane Library, PubMed, and PQDT) using the Preferred Reporting Items for Systematic Review and Meta-Analysis Statement. A total of 14 studies met the inclusion criteria and were systematically reviewed. For the meta-analysis, R was used to analyze 30 effect sizes of for both individual and operative factors as well as publication biases from a total of nine studies.
Results
The meta-analysis revealed that persistent postoperative pain after cardiac surgery was related to one individual factor (gender) and two operative factors (acute postoperative pain and use of the internal mammary artery). Operative factors (OR=5.26) had a larger effect size than individual factors (OR=1.53).
Conclusion
Female gender, acute pain after surgery, and use of the internal mammary artery are related factors to persistent postoperative pain. The development of interventions focusing on modifiable related factors, such as acute postoperative pain, may help to minimize or prevent PPP after cardiac surgery. -
Citations
Citations to this article as recorded by- Pain-Friendly Strategies: Nursing Intervention in Postoperative Myocardial Revascularization
Debora Milena Alvarez Yañez, Gloria Carvajal Carrascal
Revista de Investigación e Innovación en Ciencias de la Salud.2025; 8(1): 1. CrossRef - Prognostic factors for chronic post‐surgical pain after lung and pleural surgery: a systematic review with meta‐analysis, meta‐regression and trial sequential analysis
P. R. D. Clephas, S. E. Hoeks, P. M. Singh, C. S. Guay, M. Trivella, M. Klimek, M. Heesen
Anaesthesia.2023; 78(8): 1005. CrossRef - Regional anesthesia in coronary artery bypass grafting: a narrative review
Viktor A. Koriachkin, Maksim A. Dzhopua, Beka S. Ezugbaia, Vaagn A. Avetisian, Dmitriy V. Zabolotskiy, Vladimir A. Evgrafov
Regional Anesthesia and Acute Pain Management.2023; 17(3): 161. CrossRef
- Pain-Friendly Strategies: Nursing Intervention in Postoperative Myocardial Revascularization
- 1,545 View
- 28 Download
- 1 Web of Science
- 3 Crossref

- Effects of Aromatherapy on Sleep Quality: A Systematic Review and Meta-Analysis
- Mi-Eun Kim, Ji Hee Jun, Muyng-Haeng Hur
- J Korean Acad Nurs 2019;49(6):655-676. Published online December 30, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.6.655
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to investigate the effects of aromatherapy on sleep quality.
Methods This is a systematic review of randomized controlled trial studies (PROSPERO registration number CRD42017064519). In this study, the PICO were adults and the elderly, aromatherapy intervention, a comparative intervention with the control and placebo oil groups, and sleep. The selected articles were in English, Korean, and Chinese.
Results The results of the meta-analysis showed that the effect sizes of the experimental group were 1.03 (n=763, SMD=1.03, 95% CI 0.66 to 1.39) (Z=5.47,
p <.001). In the aromatherapy intervention group, the effect size of sleep was statistically significant (QB=9.39, df=2,p =.009), with a difference of 0.77 for inhalation, 1.12 for oral intake and 2.05 for massage. A post-analysis showed that the effect of massage on sleep was significantly greater than the inhalation method. The regression coefficient of the intervention period, B=0.01 (Z=1.43,p =.154), also showed that the longer the intervention period, the larger the effect size; however, it was not statistically significant.Conclusion A total of 23 literature analyses showed that aromatherapy is effective in improving quality of sleep, and the massage method is more effective in improving quality of sleep than the inhalation method. A meta-ANOVA showed that the aromatherapy intervention affected the high heterogeneity of the effect size. Thus, future research with stricter control in methods and experimental procedures is necessary.
-
Citations
Citations to this article as recorded by- The effects of aroma inhalation on the quality of sleep, professional quality of life, and near-misses in medication errors among emergency room nurses on night duty in Korea: a randomized controlled trial
Jungha Son, Chul-Gyu Kim
Journal of Korean Biological Nursing Science.2025; 27(1): 25. CrossRef - Effects of a Multimodal Intervention on Sleep Quality and Duration in Intensive Care Unit Patients
Jieun Nam, Sukhee Ahn
Journal of Korean Critical Care Nursing.2025; 18(1): 70. CrossRef - Efficacy of Aromatherapy Against Behavioral and Psychological Disturbances in People With Dementia: A Meta-Analysis of Randomized Controlled Trials
Po-Hao Wang, Ho-Wei Lin, Truc Tran Thanh Nguyen, Chaur-Jong Hu, Li-Kai Huang, Ka-Wai Tam, Yi-Chun Kuan
Journal of the American Medical Directors Association.2024; 25(11): 105199. CrossRef - Meta-analysis of the Effect Size of Lavender Essential Oil and Lavender Blended Essential Oils on Psychological Factors in Adults
Mi-Na Yu, Ae-Jung Kim
Asian Journal of Beauty and Cosmetology.2024; 22(3): 477. CrossRef - THE EFFECT OF LAVENDER AROMA THERAPY ON THE SLEEP QUALITY OF PREGNANT WOMEN TM III
Hajar Nur Fathur Rohmah
Jurnal Midpro.2024; 16(1): 59. CrossRef - Effects of aromatherapy on sore throat, nasal symptoms and sleep quality in adults infected with COVID-19: A randomized controlled trial
Hye-Young Kang, Hye Young Ahn, Mi-Jung Kang, Myung-Haeng Hur
Integrative Medicine Research.2023; 12(4): 101001. CrossRef - Pain and sleep after open-heart surgery-inhalation peppermint essence: double-blind randomized clinical trial
Mahla Maghami, Mohammad-Sadegh Pour‑Abbasi, Safoura Yadollahi, Mahboobeh Maghami, Ismail Azizi-fini, Mohammad-Reza Afazel
BMJ Supportive & Palliative Care.2023; 13(e3): e1318. CrossRef - Effects of Aromatherapy on Cancer Patients' Sleep and Fatigue: A Systematic Review and Meta-Analysis
Ju Hyun Ahn, Myoungsuk Kim
Journal of Integrative and Complementary Medicine.2023; 29(4): 212. CrossRef - Harnessing the power of a good night's sleep
Karen Colombo
Nursing Made Incredibly Easy!.2023; 21(1): 34. CrossRef - Effectiveness of aromatherapy on anxiety and sleep quality among adult patients admitted into intensive care units: A systematic review
Jie Xi Jassie Tan, Junyao Stefanie Cai, Jeanette Ignacio
Intensive and Critical Care Nursing.2023; 76: 103396. CrossRef - Fatigue relief by aromatherapy use in prenatal and postnatal women: a systematic review and meta-analysis
Ji-Ah Song, Hyejin Yang
Korean Journal of Women Health Nursing.2022; 28(2): 87. CrossRef - Aromatherapy with single essential oils can significantly improve the sleep quality of cancer patients: a meta-analysis
Hui Cheng, Lu Lin, Shaotong Wang, Yueyue Zhang, Tingting Liu, Yang Yuan, Qiuyun Chen, Li Tian
BMC Complementary Medicine and Therapies.2022;[Epub] CrossRef - Effects of aromatherapy on fatigue, quality of sleep and quality of life in patients with inflammatory bowel disease: A feasibility study
Lili You, Na Guo, Tiantian Wang, Xiang Yu, Xiaofeng Kang, Yuxia Guan, Hongpeng Liu, Jing Dong, Peili Bian, Siyao Wang, Chenxiao Bai
Complementary Therapies in Clinical Practice.2022; 49: 101648. CrossRef - The Effects of Non-pharmacological Interventions on Sleep among Older Adults in Korean Long-term Care Facilities: A Systematic Review and Meta-analysis
Sun Ok Jung, Hyeyoung Kim, Eunju Choi
Journal of Korean Academy of Community Health Nursing.2022; 33(3): 340. CrossRef - Visualizing Research Trends and Identifying Hotspots of Traditional Chinese Medicine (TCM) Nursing Technology for Insomnia: A 18-Years Bibliometric Analysis of Web of Science Core Collection
Junxin Wang, Yufeng Chen, Xing Zhai, Yupeng Chu, Xiangdi Liu, Xueling Ma
Frontiers in Neurology.2022;[Epub] CrossRef - Effects of aromatherapy on sleep disorders
Xin Song, Jiahua Peng, Weiyu Jiang, Minghua Ye, Lisheng Jiang
Medicine.2021; 100(17): e25727. CrossRef - Effect of aromatherapy on sleep quality of adults and elderly people: A systematic literature review and meta-analysis
Jihoo Her, Mi-Kyoung Cho
Complementary Therapies in Medicine.2021; 60: 102739. CrossRef - Effect of Rosa damascena on improvement of adults’ sleep quality: a systematic review and meta-analysis of randomized controlled trials
Mohammad Sadegh Ghorbani Rami, Morteza Nasiri, Mohammad Sadegh Aghili Nasab, Zohre Jafari, Mahya Torkaman, Shahoo Feizi, Behnam Farahmandnia, Masoomeh Asadi
Sleep Medicine.2021; 87: 8. CrossRef - The Mediating Effect of Sleep Quality in the Relationship between Academic Stress and Social Network Service Addiction Tendency among Adolescents
Eun Sook Bae, Hye Seung Kang, Ha Na Lee
Journal of Korean Academy of Community Health Nursing.2020; 31(3): 290. CrossRef
- The effects of aroma inhalation on the quality of sleep, professional quality of life, and near-misses in medication errors among emergency room nurses on night duty in Korea: a randomized controlled trial
- 5,976 View
- 160 Download
- 13 Web of Science
- 19 Crossref

- Effect of Autogenic Training for Stress Response: A Systematic Review and Meta-Analysis
- Eunju Seo, Soukyoung Kim
- J Korean Acad Nurs 2019;49(4):361-374. Published online January 15, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.4.361
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose This study was conducted to evaluate the effectiveness of autogenic training on stress responses through a systematic review and meta-analysis.
Methods A systematic search was conducted using eight core electronic databases (Embase, CENTRAL, Medline, CINAHL, PsycInfo, DBpia, KISS, and RISS). To estimate the effect size, a meta-analysis of the studies was performed using RevMan 5.3.5 program.
Results A total 21 studies out of 950 studies were included in the review, and 11 were included for meta-analysis. These studies showed that autogenic training decreased anxiety and depression, and increased the high frequency of heart rate variability. Calculations to understand the effect of autogenic training on anxiety, through a meta-analysis, observed a reduction effect of anxiety score by 1.37 points (n=85, SMD=-1.37: 95% CI -2.07 to -0.67), in the studies on short-term intervention targeting healthy adults. On the other hand, similar calculations to understand the effect of autogenic training on depression observed, a reduction effect on the depression score by 0.29 point (n=327, SMD=-0.29: 95% CI -0.50 to -0.07), in the studies on long term intervention targeting the patient group.
Conclusion Autogenic training is effective for adults’ stress management, and nurses will be able to effectively perform autogenic training programs for workers’ stress relief at the workplace.
-
Citations
Citations to this article as recorded by- A peer-led group intervention based on relaxation (soRELAX) to improve well-being and mental health in nursing students: A mixed method pilot study
Maria Pilar Ramirez Garcia, Jérôme Leclerc-Loiselle, Christine Genest, Etienne Paradis-Gagné, Caroline Larue, Marikim Poitras-Crête, Sylvie Corbeil, Camille Saseville
Journal of Professional Nursing.2025; 57: 8. CrossRef - Effects of Autogenic Training on Pain Modulation in Burning Mouth Syndrome: A Preliminary Study
Keita Takizawa, Kana Ozasa, Kohei Shimizu, Noboru Noma
Cureus.2025;[Epub] CrossRef - Strengthening psychological resilience: The effectiveness of autogenic training of community pharmacists
Dragana Jocic
Vojnosanitetski pregled.2024; 81(11): 696. CrossRef - Ampliación del Informe de Sanidad: Evidencia Sobre la Seguridad y Eficacia del Entrenamiento Autógeno
Juan Manuel Guiote, Miguel Angel Vallejo Pareja, Blanca Mas
Papeles del Psicólogo - Psychologist Papers.2024; 45(3): 172. CrossRef - Autogenic Training in Mental Disorders: What Can We Expect?
Dagmar Breznoscakova, Milana Kovanicova, Eva Sedlakova, Maria Pallayova
International Journal of Environmental Research and Public Health.2023; 20(5): 4344. CrossRef - The effects of online enactive education on secondary school students
Deborah R. Vivo
The Journal of Educational Research.2023; 116(4): 230. CrossRef - Self-reported symptom burden in postural orthostatic tachycardia syndrome (POTS): A narrative review of observational and interventional studies
Iris Knoop, Federica Picariello, Emma Jenkinson, Nicholas Gall, Claudia Chisari, Rona Moss-Morris
Autonomic Neuroscience.2023; 244: 103052. CrossRef - Efficacy of Individualized Sensory-Based mHealth Interventions to Improve Distress Coping in Healthcare Professionals: A Multi-Arm Parallel-Group Randomized Controlled Trial
Hannes Baumann, Luis Heuel, Laura Louise Bischoff, Bettina Wollesen
Sensors.2023; 23(4): 2322. CrossRef - The Effect of Autogenic Training in a Form of Audio Recording on Sleep Quality and Physiological Stress Reactions of University Athletes—Pilot Study
Kamila Litwic-Kaminska, Martyna Kotyśko, Tadeusz Pracki, Monika Wiłkość-Dębczyńska, Błażej Stankiewicz
International Journal of Environmental Research and Public Health.2022; 19(23): 16043. CrossRef - Combined effect of autogenic relaxation and aerobic exercise on postmenopausal hypertension: A randomized clinical trial
Shreen R Aboelmagd, Afaf M Botla, Hossam ELdine Hussein, Sahar M. Ali, Nehad A. Abo-Zaid
International journal of health sciences.2022; 6(S10): 2314. CrossRef - Temporomandibular Myofascial Pain Syndrome—Aetiology and Biopsychosocial Modulation. A Narrative Review
Paulina Golanska, Klara Saczuk, Monika Domarecka, Joanna Kuć, Monika Lukomska-Szymanska
International Journal of Environmental Research and Public Health.2021; 18(15): 7807. CrossRef - To stress or not to stress: Brain-behavior-immune interaction may weaken or promote the immune response to SARS-CoV-2
Eva M.J. Peters, Manfred Schedlowski, Carsten Watzl, Ulrike Gimsa
Neurobiology of Stress.2021; 14: 100296. CrossRef - Non‐pharmacologic treatment of insomnia in primary care settings
Laura Hrehová, Kamal Mezian
International Journal of Clinical Practice.2021;[Epub] CrossRef - A Single Session of Heart Rate Variability Biofeedback Produced Greater Increases in Heart Rate Variability Than Autogenic Training
I-Mei Lin, San-Yu Wang, Sheng-Yu Fan, Erik Peper, Sui-Pi Chen, Ching-Yu Huang
Applied Psychophysiology and Biofeedback.2020; 45(4): 343. CrossRef - A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial
Marita Stier-Jarmer, Cornelia Oberhauser, Dieter Frisch, Götz Berberich, Thomas Loew, Carina Schels-Klemens, Birgit Braun, Angela Schuh
International Journal of Environmental Research and Public Health.2020; 17(24): 9227. CrossRef
- A peer-led group intervention based on relaxation (soRELAX) to improve well-being and mental health in nursing students: A mixed method pilot study
- 3,872 View
- 177 Download
- 13 Web of Science
- 15 Crossref

- Effects of Aromatherapy on Menopausal Symptoms, Perceived Stress and Depression in Middle-aged Women: A Systematic Review
- Shinmi Kim, Ji-Ah Song, Mi-Eun Kim, Myung-Haeng Hur
- J Korean Acad Nurs 2016;46(5):619-629. Published online October 31, 2016
- DOI: https://doi.org/10.4040/jkan.2016.46.5.619
-
 Abstract
Abstract
 PDF
PDF Purpose This study was a systematic review to evaluate the effects of aromatherapy on menopausal symptoms, perceived stress and depression in middle aged-women.
Methods Eight databases were searched from their inception September 8, 2015. Two reviewers independently performed the selection of the studies, data abstraction and validations. The risk of bias was assessed using Cochrane criteria. For analysis of the data, a meta-analysis of the studies was performed.
Results From the electronic databases, 73 articles were selected, and 19 removed due to duplication. After two reviewers read the abstracts of 54 studies, 34 studies were selected. Complete papers for 34 original articles were read and, 12 studies which met selection criteria were reviewed and the effects of aromatherapy on menopausal symptoms, stress and depression analyzed using meta-analysis with RevMan. In the 2 studies which included Randomized Controlled Trials testing of aromatherapy on menopausal symptoms and comparison of control and placebo groups were done. Aromatherapy massage was favorably effective in reducing the menopausal symptoms compared to the control group (n=118, MD=-6.33; 95% CI -11.51 to -1.15), and compared to the placebo group (n=117, MD=-4.14; 95% CI -7.63 to -0.64). Also aromatherapy was effective in reducing stress (n=72, SMD=-0.64; 95% CI -1.12 to -0.17) and depression (n=158, MD=-5.63; 95% CI -10.04 to -1.22).
Conclusion There is limited evidence suggesting that aromatherapy for middle-aged women may be effective in controlling menopausal symptoms, perceived stress and depression.
-
Citations
Citations to this article as recorded by- The effect of aromatherapy on pain in individuals with diabetes: a systematic review and meta-analysis
Mi-Kyoung Cho, Mi Young Kim
Journal of Korean Biological Nursing Science.2024; 26(2): 71. CrossRef - Examining the Health-Related Needs of Females during Menopause: A Systematic Review Study
Masoumeh Rostami-Moez, Seyedeh Zahra Masoumi, Marzieh Otogara, Farhad Farahani, Shohreh Alimohammadi, Khodayar Oshvandi
Journal of Menopausal Medicine.2023; 29(1): 1. CrossRef - Effect of Aromatherapy with Essential oil of Lavandula Angustifolia Mill- Citrus Bergamia and Mindfulness-Based Intervention on Sexual Function, Anxiety, and Depression in Postmenopausal Women
Mandana Mojtehedi, Hanieh Salehi-Pourmehr, Alireza Ostadrahimi, Solmaz Asnaashari, Khalil Esmaeilpour, Azizeh Farshbaf-Khalili
Iranian Journal of Nursing and Midwifery Research.2022; 27(5): 392. CrossRef - Aromatherapy for Managing Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials
Hye Won Lee, Lin Ang, Jiae Choi, Myeong Soo Lee
The Journal of Alternative and Complementary Medicine.2021; 27(10): 813. CrossRef - Effects of the Healing Beats Program among University Students after Exposure to a Source of Psychological Stress: A Randomized Control Trial
Jiah Song, Wonjong Kim, Iklyul Bae
International Journal of Environmental Research and Public Health.2021; 18(21): 11716. CrossRef - Nano-Aromatic Drugs Based on Mesoporous Silica Nanoparticles and Bergamot Essential Oil for Anti-Depression
Xiao-Hong Yang, Huan Peng, Qiu-Lian Hao, Jian-Ze Wang, Zhi-Guo Lu, Yun-Wei Niu, Zuo-Bing Xiao, Xin Zhang
Journal of Biomedical Nanotechnology.2021; 17(6): 1242. CrossRef - The Effects of Providing Lavender Inhalation Therapy on Anxiety and Alleviation of Pain before Burn Dressings
Kyung Ja Kim, Jihyun Kim, Gye Seon Jeong
Journal of Korean Academy of Fundamentals of Nursing.2020; 27(1): 29. CrossRef - EEG Revealed That Fragrances Positively Affect Menopausal Symptoms in Mid-life Women
Sun Ae Moon, Jisub Bae, Kwangsu Kim, Si Young Cho, Gusang Kwon, Ran Lee, Seung Ho Ko, Soyeon Lim, Cheil Moon
Experimental Neurobiology.2020; 29(5): 389. CrossRef - Combination of 3-Dimensional Virtual Reality and Hands-On Aromatherapy in Improving Institutionalized Older Adults’ Psychological Health: Quasi-Experimental Study
Vivian Ya-Wen Cheng, Chiu-Mieh Huang, Jung-Yu Liao, Hsiao-Pei Hsu, Shih-Wen Wang, Su-Fei Huang, Jong-Long Guo
Journal of Medical Internet Research.2020; 22(7): e17096. CrossRef - How Strong is the Evidence for the Anxiolytic Efficacy of Lavender?: Systematic Review and Meta-analysis of Randomized Controlled Trials
Hyun-Ju Kang, Eun Sook Nam, Yongmi Lee, Myoungsuk Kim
Asian Nursing Research.2019; 13(5): 295. CrossRef - Effect of aromatherapy interventions on hemodialysis complications: A systematic review
Salehoddin Bouya, Sudabeh Ahmadidarehsima, Mahin Badakhsh, Abbas Balouchi, Maryam koochakzai
Complementary Therapies in Clinical Practice.2018; 32: 130. CrossRef - Effects of Aroma Inhalation on Stress, Fatigue and Depression among Nurses Working in Intensive Care Unit
Eun Young Jung, Ji-hyeun Song
Asian Journal of Beauty and Cosmetology.2018; 16(3): 321. CrossRef - Aromatherapy for managing menopausal symptoms
Jiae Choi, Hye Won Lee, Ju Ah Lee, Hyun-Ja Lim, Myeong Soo Lee
Medicine.2018; 97(6): e9792. CrossRef - Effect of Aromatherapy on the Treatment of Psychological Symptoms in Postmenopausal and Elderly Women: A Systematic Review and Meta-analysis
Masoudeh Babakhanian, Masumeh Ghazanfarpour, Leila Kargarfard, Nasibeh Roozbeh, Leili Darvish, Talat Khadivzadeh, Fatemeh Rajab Dizavandi
Journal of Menopausal Medicine.2018; 24(2): 127. CrossRef - Behavioral Characteristics and Cardiovascular Disease Risks Associated With Insomnia and Sleep Quality Among Middle‐Aged Women in South Korea
Ok Kyung Ham, Jinyoung Kim, Bo Gyeong Lee, Eunju Choi
Research in Nursing & Health.2017; 40(3): 206. CrossRef
- The effect of aromatherapy on pain in individuals with diabetes: a systematic review and meta-analysis
- 2,170 View
- 53 Download
- 15 Crossref

- Dysphagia Screening Measures for Use in Nursing Homes: A Systematic Review
- Yeon-Hwan Park, Hwal Lan Bang, Hae-Ra Han, Hee-Kyung Chang
- J Korean Acad Nurs 2015;45(1):1-13. Published online February 27, 2015
- DOI: https://doi.org/10.4040/jkan.2015.45.1.1
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to evaluate the psychometric quality and feasibility of measurements for screening dysphagia in older adults to identify the 'right tool' for nurses to use in nursing homes.
Methods A systematic review was done. Electronic databases were searched for studies related to dysphagia screening measurements. A checklist was used to evaluate the psychometric quality and applicability. Tools were evaluated for feasible incorporation into routine care by nurses.
Results 29 tools from 31 studies were identified. Dysphagia screening tools with an acceptable validity and reliability had sensitivity between 68% and 100% and specificity between 52% and 100%. The Gugging Swallowing Screen (GUSS) and the Standardized Swallowing Assessment (SSA) were the tools with high psychometric quality, especially with high sensitivity, that nurses could perform feasibly to identify the risk and to grade the severity of dysphagia and aspiration of nursing home residents.
Conclusion Results show that GUSS and SSA are reliable and sensitive tools for screening dysphagia which nurses can use in nursing homes. Further research is needed to examine feasibility of screening with identified tools, and also, to establish effective and standardized protocols for these tools so they can be effectively incorporated into routine care.
-
Citations
Citations to this article as recorded by- eTWST: An Extension to the Timed Water Swallow Test for Increased Dysphagia Screening Accuracy
Louise Brage, Fredrik Nylén, Patricia Hägglund, Thorbjörn Holmlund
Dysphagia.2025; 40(4): 801. CrossRef - Evaluation of the performance of screening tools for dysphagia in older adults: A diagnostic meta-analysis
Lingli Zhang, Ran Hou, Lin Liu, Yan Liu, Qinqin Yu
Geriatric Nursing.2025; 61: 629. CrossRef - Effect of artificial intelligence-based video-game system on dysphagia in patients with stroke: A randomized controlled trial
Bohan Zhang, Ka Po Wong, Mingyue Liu, Vivian Hui, Cai Guo, Zihan Liu, Yue Liu, Qian Xiao, Jing Qin
Clinical Nutrition.2025; 45: 81. CrossRef - Progress on aspiration assessment methods for patients after esophageal cancer surgery in early: A review
Yushuang Su, Yan Li, Zhongbin Chen, Hong Gao, Yaxie He, Xiaohua Li, Xiaying Zeng, Wei Lan, Qin Yang
Medicine.2025; 104(3): e41214. CrossRef - Reliability and validity of the Standardized swallowing assessment among community-dwelling older adults in China
Jing Wang, Caixia Chen, Yuzhen Qin, Jing Zeng, Chunhua Zhang, Liugen Wang, Heping Li, Xi Zeng
Annals of Medicine.2025;[Epub] CrossRef - Occurrence of impaired swallowing ability and change over a year in older adults living in nursing homes
Ida Crossler, Clara Shrestha Jensen, Karin Eriksson, Lisa Tuomi
Scientific Reports.2025;[Epub] CrossRef - Dental Factors Associated With Oropharyngeal Dysphagia in Institutionalised Older Adults: A Systematic Review
Raquel Soncini de Morais, Juliana Balbinot Hilgert, Fernando Neves Hugo, Rafaela Soares Rech
Gerodontology.2025;[Epub] CrossRef - Feasibility of Oral Function Evaluation According to Dementia Severity in Older Adults with Alzheimer’s Disease
Maki Shirobe, Ayako Edahiro, Keiko Motokawa, Shiho Morishita, Yoshiko Motohashi, Chiaki Matsubara, Masanori Iwasaki, Yutaka Watanabe, Hirohiko Hirano
Nutrients.2024; 16(7): 992. CrossRef - Research trends on dysphagia among Korean older adults in long-term care facilities: A scoping review
Seyoung Cho, Dukyoo Jung, Jisung Park
Journal of Korean Gerontological Nursing.2024; 26(2): 134. CrossRef - Appropriate volumes of water for non-invasive swallowing assessments of nursing home residents: A descriptive correlational study
Meng Rung Tsai, Wann Yun Shieh, Hsiu Hsin Tsai, Yea Ing Lotus Shyu, Kuo Hsuan Chang, Fur Hsing Wen, Chia Yih Liu
Heliyon.2024; 10(17): e37340. CrossRef - Aspiration pneumonia in nursing literature—a mapping review
Dominika Lisiecka, Áine Kearns, William Evans, Dawn Farrell
Frontiers in Rehabilitation Sciences.2024;[Epub] CrossRef - Development and validation of a nomogram for predicting dysphagia in long-term care facility residents
Jinmei Liu, Mingshu Liao, Hui Yang, Xiaofang Chen, Yang Peng, Jing Zeng
Aging Clinical and Experimental Research.2023; 35(6): 1293. CrossRef - Understanding how primary care practitioners can be supported to recognise, screen and initially diagnose oropharyngeal dysphagia: protocol for a behavioural science realist review
Caroline Smith, Debi Bhattacharya, Sion Scott
BMJ Open.2023; 13(2): e065121. CrossRef - Effects of chin tuck against resistance exercise on post-stroke dysphagia rehabilitation: A systematic review and meta-analysis
Jing Liu, Qiuyi Wang, Jing Tian, Wanqiong Zhou, Yitian Gao, Xuemei Chen, Wei Zhang, Yajing Gao, Lanshu Zhou
Frontiers in Neurology.2023;[Epub] CrossRef - Development and validation of a predictive model for patients with post-extubation dysphagia
Jia-ying Tang, Xiu-qin Feng, Xiao-xia Huang, Yu-ping Zhang, Zhi-ting Guo, Lan Chen, Hao-tian Chen, Xiao-xiao Ying
World Journal of Emergency Medicine.2023; 14(1): 49. CrossRef - Evaluation of preventive care for swallowing difficulty through policy changes in Japanese long-term care insurance: analysis of a nationwide claims dataset for long-term care insurance
Hiroko Mori, Ayako Nakane, Haruka Tohara, Takeo Nakayama
BMC Health Services Research.2023;[Epub] CrossRef - Are Oropharyngeal Dysphagia Screening Tests Effective in Preventing Pneumonia?
Ikuko Okuni, Satoru Ebihara
Journal of Clinical Medicine.2022; 11(2): 370. CrossRef - Altered Brain Function Activity in Patients With Dysphagia After Cerebral Infarction: A Resting-State Functional Magnetic Resonance Imaging Study
Lei Li, Jiayu Liu, Fenxiong Liang, Haidong Chen, Rungen Zhan, Shengli Zhao, Tiao Li, Yongjun Peng
Frontiers in Neurology.2022;[Epub] CrossRef - The Role of Instrumental Swallowing Assessment in Adults in Residential Aged Care Homes: A National Modified Delphi Survey Examining Beliefs and Practices
Olga Birchall, Michelle Bennett, Nadine Lawson, Susan M. Cotton, Adam P. Vogel
Dysphagia.2022; 37(3): 510. CrossRef - Predicting feeding-tube dependence in patients following endotracheal extubation: a two-item swallowing screen
Shu-Fen Siao, Wen-Hsuan Tseng, Tyng-Guey Wang, Yu-Chung Wei, Tzu-Yu Hsiao, Shih-Chi Ku, Cheryl Chia-Hui Chen
BMC Pulmonary Medicine.2021;[Epub] CrossRef - European white paper: oropharyngeal dysphagia in head and neck cancer
Laura W. J. Baijens, Margaret Walshe, Leena-Maija Aaltonen, Christoph Arens, Reinie Cordier, Patrick Cras, Lise Crevier-Buchman, Chris Curtis, Wojciech Golusinski, Roganie Govender, Jesper Grau Eriksen, Kevin Hansen, Kate Heathcote, Markus M. Hess, Sefik
European Archives of Oto-Rhino-Laryngology.2021; 278(2): 577. CrossRef - Dysphagia screening in residential care settings: A scoping review
Constantino Estupiñán Artiles, Julie Regan, Claire Donnellan
International Journal of Nursing Studies.2021; 114: 103813. CrossRef - A Swallowing Screening Test Enhances a Better Recognition of Patients with a Hip Fracture at Risk for Oropharyngeal Dysphagia
Hugo Wijnen, Peter P. Schmitz, Martine Jansen, Linda Hendrix, Job L. C. van Susante, Hanna Willems
Orthopaedic Nursing.2021; 40(2): 94. CrossRef - Comparison studies of ultrasound-guided botulinum toxin injection and balloon catheter dilatation in the treatment of neurogenic cricopharyngeal muscle dysfunction
Shuo Luan, Shao-Ling Wu, Ling-Jun Xiao, Hai-Yun Yang, Mei-Xin Liao, Shao-Ling Wang, Sheng-Nuo Fan, Chao Ma
NeuroRehabilitation.2021; 49(4): 629. CrossRef - Instrumental Swallowing Assessment in Adults in Residential Aged Care Homes: A Scoping Review
Olga Birchall, Michelle Bennett, Nadine Lawson, Susan M. Cotton, Adam P. Vogel
Journal of the American Medical Directors Association.2021; 22(2): 372. CrossRef - Validation of the Munich Swallowing Score (MUCSS) in patients with neurogenic dysphagia: A preliminary study
G. Bartolome, U. Starrost, H. Schröter-Morasch, B. Schilling, L. Fischbacher, L. Kues, S. Graf, W. Ziegler
NeuroRehabilitation.2021; 49(3): 445. CrossRef - Dietary inflammatory index is associated with pain intensity and some components of quality of life in patients with knee osteoarthritis
Vahideh Toopchizadeh, Neda Dolatkhah, Dawood Aghamohammadi, Mahrokh Rasouli, Maryam Hashemian
BMC Research Notes.2020;[Epub] CrossRef - Dysphagia and mealtime difficulties in dementia: Speech and language therapists’ practices and perspectives
Aisling Egan, Carolyn Andrews, Anja Lowit
International Journal of Language & Communication Disorders.2020; 55(5): 777. CrossRef - The Gugging Swallowing Screen in dysphagia screening for patients with stroke: A systematic review
Ki Deok Park, Tae Hee Kim, Seon Heui Lee
International Journal of Nursing Studies.2020; 107: 103588. CrossRef - Optimising Medicines Administration for Patients with Dysphagia in Hospital: Medical or Nursing Responsibility?
David J. Wright, David G. Smithard, Richard Griffith
Geriatrics.2020; 5(1): 9. CrossRef - Risk Factors of Dysphagia Among Community-Dwelling Middle-Aged Women
Young Hee Lee, Dukyoo Jung, Ok Jong Yun, Hyesoon Lee, Minkyung Lee
Gastroenterology Nursing.2020; 43(2): 164. CrossRef - Developing and Testing the Diagnostic Accuracy of a Brief Nursing Dysphagia Screen
Sarah Groppo-Lawless, Claire C. Davies, Alex Lengerich
Rehabilitation Nursing.2020; 45(6): 367. CrossRef - The Easy Dysphagia Symptom Questionnaire (EDSQ): a new dysphagia screening questionnaire for the older adults
Kyeong Eun Uhm, Minsun Kim, Yong Min Lee, Bo-Ram Kim, Yoon-Sook Kim, Jaekyung Choi, Seol-Heui Han, Hee Joung Kim, Kwang Ha Yoo, Jongmin Lee
European Geriatric Medicine.2019; 10(1): 47. CrossRef - Sarcopenia is an Independent Risk Factor for Dysphagia in Community-Dwelling Older Adults
Seungwoo Cha, Won-Seok Kim, Ki Woong Kim, Ji Won Han, Hak Chul Jang, Soo Lim, Nam-Jong Paik
Dysphagia.2019; 34(5): 692. CrossRef - The GUSS test as a good indicator to evaluate dysphagia in healthy older people: a multicenter reliability and validity study
Ebru Umay, Sibel Eyigor, Ali Yavuz Karahan, Ilknur Albayrak Gezer, Ayse Kurkcu, Dilek Keskin, Gulten Karaca, Zeliha Unlu, Canan Tıkız, Meltem Vural, Banu Aydeniz, Ebru Alemdaroglu, Emine Esra Bilir, Ayse Yalıman, Ekin Ilke Sen, Mazlum Serdar Akaltun, Ozle
European Geriatric Medicine.2019; 10(6): 879. CrossRef - Repetitive Saliva Swallowing Test: Norms, Clinical Relevance and the Impact of Saliva Secretion
Emmelie Persson, Inger Wårdh, Per Östberg
Dysphagia.2019; 34(2): 271. CrossRef - Dysphagia in Frail Older Persons: Making the Most of Current Knowledge
Nicole Rogus-Pulia, Rainer Wirth, Philip D. Sloane
Journal of the American Medical Directors Association.2018; 19(9): 736. CrossRef - Frailty, Swallowing and Dysphagia
David G. Smithard, Mariyam Shazra, Dharinee Hansjee, Ian Swaine
Current Physical Medicine and Rehabilitation Reports.2018; 6(3): 192. CrossRef - Nursing interventions in adult patients with oropharyngeal dysphagia: a systematic review
Lorena Molina, Susana Santos-Ruiz, Pere Clavé, Luis González-de Paz, Esther Cabrera
European Geriatric Medicine.2018; 9(1): 5. CrossRef - Nursing home-acquired pneumonia, dysphagia and associated diseases in nursing home residents: A retrospective, cross-sectional study
Vanessa R.Y. Hollaar, Gert-Jan van der Putten, Claar D. van der Maarel-Wierink, Ewald M. Bronkhorst, Bert J.M. de Swart, Cees de Baat, Nico H.J. Creugers
Geriatric Nursing.2017; 38(5): 437. CrossRef - Oropharyngeal dysphagia: manifestations and diagnosis
Nathalie Rommel, Shaheen Hamdy
Nature Reviews Gastroenterology & Hepatology.2016; 13(1): 49. CrossRef - Dysphagia and Aspiration
John E. Morley
Journal of the American Medical Directors Association.2015; 16(8): 631. CrossRef - Expanding Instrumental Options for Dysphagia Diagnosis and Research: Ultrasound and Manometry
Maggie-Lee Huckabee, Phoebe Macrae, Kristin Lamvik
Folia Phoniatrica et Logopaedica.2015; 67(6): 269. CrossRef
- eTWST: An Extension to the Timed Water Swallow Test for Increased Dysphagia Screening Accuracy
- 3,705 View
- 57 Download
- 43 Crossref

- Effects of Foot Reflexology on Fatigue, Sleep and Pain: A Systematic Review and Meta-analysis
- Jeongsoon Lee, Misook Han, Younghae Chung, Jinsun Kim, Jungsook Choi
- J Korean Acad Nurs 2011;41(6):821-833. Published online December 31, 2011
- DOI: https://doi.org/10.4040/jkan.2011.41.6.821
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to evaluate the effectiveness of foot reflexology on fatigue, sleep and pain.
Methods A systematic review and meta-analysis were conducted. Electronic database and manual searches were conducted on all published studies reporting the effects of foot reflexology on fatigue, sleep, and pain. Forty four studies were eligible including 15 studies associated with fatigue, 18 with sleep, and 11 with pain. The effects of foot reflexology were analyzed using Comprehensive Meta-Analysis Version 2.0. The homogeneity and the fail-safe N were calculated. Moreover, a funnel plot was used to assess publication bias.
Results The effects on fatigue, sleep, and pain were not homogeneous and ranged from 0.63 to 5.29, 0.01 to 3.22, and 0.43 to 2.67, respectively. The weighted averages for fatigue, sleep, and pain were 1.43, 1.19, and 1.35, respectively. No publication bias was detected as evaluated by fail-safe N. Foot reflexology had a larger effect on fatigue and sleep and a smaller effect on pain.
Conclusion This meta-analysis indicates that foot reflexology is a useful nursing intervention to relieve fatigue and to promote sleep. Further studies are needed to evaluate the effects of foot reflexology on outcome variables other than fatigue, sleep and pain.
-
Citations
Citations to this article as recorded by- Combined effects of reflexology massage and respiratory relaxation on pain following chest tube removal in heart surgery patients
Zainab Bahramian, Majid Kazemi, Reza Vazirinejad, Hadi Hasani
Journal of Cardiothoracic Surgery.2025;[Epub] CrossRef - Foot Reflexology for Managing Menopausal Symptoms in Women: A Systematic Review and Meta-Analysis
Mahsa Maghalian, Maryam Alikamali, Farzaneh Aslanpur, Mojgan Mirghafourvand
Current Women s Health Reviews.2025;[Epub] CrossRef - The Effect of Foot Reflexology on Postpartum Comfort and Breastfeeding Outcomes in Postpartum Women: A Meta-Analysis Study
Dilek Menekse, Ahsen Demirhan Kayacik, Kevser Ilcioglu
Breastfeeding Medicine.2025; 20(6): 441. CrossRef - The Effectiveness of Reflexology on Fatigue, Constipation, Nausea and Vomiting During Pregnancy: A Narrative Review
Niloofar Nezhadahmad, Fereshteh Khoshkhoo, Mansour Arad, Zahra Zarei
Journal of Health Reports and Technology.2025;[Epub] CrossRef - A Review of Nursing Thesis on Complementary and Supportive Medicine Practices for Patients with Osteoarthritis: A Systematic Review
Alev Yildirim Keskin, Deniz Zeynep Sönmez
Sakarya Üniversitesi Holistik Sağlık Dergisi.2025; 8(1): 44. CrossRef - Effect of foot reflexology on chronic pain in Parkinson’s disease: A randomized controlled trial
Karel Joineau, Estelle Harroch, Mathilde Boussac, Margherita Fabbri, Clémence Leung, Fabienne Ory-Magne, Vanessa Rousseau, Patrice Peran, Christine Brefel-Courbon, Emeline Descamps, Federico Giove
PLOS One.2025; 20(7): e0327865. CrossRef - The Effect of Foot Reflexology Massage on Fatigue and Sleep Quality in Hemodialysis Patients
Raheleh Rajabi, Fatemeh Akhlaghi, Neda Asadi, Fatemeh Zamani Babgohari, Fatemeh Arabpoor
SAGE Open Nursing.2025;[Epub] CrossRef - Leitlinie „Insomnie bei Erwachsenen“ – Update 2025 (AWMF-Registernummer 063-003)
K. Spiegelhalder, E. Baum, M. Becker, C. Cornaro, T. Crönlein, L. Frase, V. Harth, E. Hertenstein, A. F. Johann, I. Mertel, D. Kunz, J. Langhorst, J. T. Maurer, G. Mayer, C. Nissen, R. Pietrowsky, T. Pollmächer, C. Schumacher, H. Sitter, A. Steffen, H. G.
Somnologie.2025; 29(4): 240. CrossRef - Comparing the impact of acupressure and reflexology on fatigue in chronic lymphocytic leukemia patients: A randomized controlled trial with three arms
Naser Parizad, Amireh Hassanpour, Rasoul Goli, Hamidreza Khalkhali, Aysan Nozad
European Journal of Oncology Nursing.2024; 70: 102573. CrossRef - A narrative review of research linking non‐sexual social touch to sleep quality
Yuxi Xie, Brooke C. Feeney
Journal of Sleep Research.2024;[Epub] CrossRef - COMPARISON OF THE EFFECT OF AURICULOTHERAPY AND FOOT REFLEXOLOGY ON THE SENSORY AND EMOTIONAL ASPECTS OF PAIN AND THE USE OF PAINKILLERS AFTER ELECTIVE CAESAREAN SECTION
Fatemeh Sadat Mousavi, Nahid Golmakani, Seyyedeh adeleh Rahmanian
Studies in Medical Sciences.2024; 35(1): 30. CrossRef - Reflexology evidence map
Erika Cardozo Pereira, Caio Fabio Schlechta Portella, Ricardo Ghelman, Carmen Verônica Mendes Abdala, Ana Cláudia Moraes Barros Leite-Mor, Arthur Schveitzer Ferreira, Pamela Gissi Lima, Mariana Cabral Schveitzer
Advances in Integrative Medicine.2024; 11(4): 191. CrossRef - Effect of Reflexology on Pain, Fatigue, Sleep Quality, and Lactation in Postpartum Primiparous Women After Cesarean Delivery: A Randomized Controlled Trial
Ayşegül Kiliçli ID, Simge Zeyneloglu ID
Journal of Human Lactation.2024; 40(2): 221. CrossRef - A Review of the Effect of Foot Reflexology on Pain in Patients
Kinga Vindis, Călin Tudor Hozan, Adrian Coțe, Gheorghe Szilagyi
Archives of Pharmacy Practice.2024; 15(1): 12. CrossRef - The Effect of Foot Reflexology on Fatigue, Sleep Quality, Physiological Indices, and Electrocardiogram Changes in Patients with Acute Myocardial Infarction: A Randomized Clinical Trial
Nilofar Pasyar, Masoume Rambod, Zahra Najafian, Mohammad Hossein Nikoo, Amin Kordi Yoosefinejad, Mahdi Salmanpour
Iranian Journal of Nursing and Midwifery Research.2024; 29(5): 608. CrossRef - Effects of foot reflexology on disease
Ming-Ying He, M Jalal Ud Din, Hai-Feng Xu, Shang-Yu Wang, Guo-Huan Ying, Hao Qian, Bing Wu, Hong-Dan Qi, Xin Wang, Gang Zhang
World Journal of Clinical Cases.2024; 12(35): 6851. CrossRef - Mental Fatigue Classification Aided by Machine Learning-Driven Model Under the Influence of Foot and Auditory Binaural Beats Brain Massages via fNIRS
Nazo Haroon, Hamid Jabbar, Umar Shahbaz Khan, Taikyeong Ted. Jeong, Noman Naseer
IEEE Access.2024; 12: 187160. CrossRef - Comparing the Effects of Hand and Foot Reflexology on Chest Pain in Patients After Primary Percutaneous Coronary Intervention
Nasrin Hanifi, Sahar Asali, Ali Imani
Journal of Archives in Military Medicine.2024;[Epub] CrossRef - The Effect of Reflexology on the Anxiety of Pregnant Women During
Labor: A Systematic Review and Meta-Analysis
Zeinab Abbaszadeh, Jamileh Malakouti, Mahsa Maghalian, Mojgan Mirghafourvand
Current Women s Health Reviews.2023;[Epub] CrossRef - Massage therapy significantly improves cancer-related fatigue in cancer patients: a meta-analysis of randomized controlled trials
Shengnan Shan, Lu Lin, Qian Fang, Fengmei Tian, Daoxia Guo, Yanling Zhou, Li Tian
Supportive Care in Cancer.2023;[Epub] CrossRef - El efecto de la reflexología podal sobre la fatiga en pacientes en hemodiálisis: un estudio de metaanálisis
Seda Şahan, Sevil Güler
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - The effect of foot reflexology on fatigue in hemodialysis patients: a meta-analysis study
Seda Şahan, Sevil Güler
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - Development and Peer Review of an Evidence-Based Decision-Support Tool for Non-Drug Prescribing for Healthy Ageing
Zara Quail, Mark Carter, Charles Young
Journal of Ageing and Longevity.2023; 3(2): 116. CrossRef - Comparing the influence of foot reflexology and fasting mimicking diet on quality of life and sleep quality in obesity hypoventilation syndrome
Rana Hesham Mohamed Elbanna, Sherif Osama Abdelsalam Elabd, Salma Ibrahim Abdelmohsen Alghitany
Journal of Complementary and Integrative Medicine.2023; 20(1): 207. CrossRef - O efeito da reflexologia podal sobre a fadiga em pacientes em hemodiálise: um estudo de metanálise
Seda Şahan, Sevil Güler
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - The Impact of Foot Reflexology on Nausea-Vomiting and Sleep Quality for Lung Cancer Patients Receiving Chemotherapy in Turkey
Hilal Pekmezci, Sevilay Hintistan
Cyprus Journal of Medical Sciences.2022; 7(5): 614. CrossRef - Impact of Nonpharmacologic Interventions Targeting Sleep Disturbances or Disorders in Patients With Inflammatory Arthritis: A Systematic Review and Meta‐Analysis of Randomized Trials
Kristine M. Latocha, Katrine B. Løppenthin, Safa Al‐Bazy, Tannie L. Albrechtsen, Helle E. Jensen, Mikkel Østergaard, Poul J. Jennum, Bente A. Esbensen, Robin Christensen
Arthritis Care & Research.2022; 74(12): 2108. CrossRef - Effect of Complementary and Integrative Treatments on Fatigue Symptoms in Hemodialysis Patients
Melek Yeşil Bayülgen, Meral Gün
Holistic Nursing Practice.2022; 36(1): 17. CrossRef - The impact of foot massage given to postmenopausal women on anxiety, fatigue, and sleep: a randomized-controlled trial
Nilay Gökbulut, Emine Ibici Akça, Çiğdem Karakayali Ay
Menopause.2022; 29(11): 1254. CrossRef - Psychometric properties of the Turkish version of the attitudes toward massage (ATOM) scale
Gizem Göktuna, Gülşah Gürol Arslan, Dilek Özden
European Journal of Integrative Medicine.2022; 55: 102178. CrossRef - The Effects of Foot Reflexology on Vital Signs: A Meta-Analysis of Randomized Controlled Trials
Yunyan Jing, Shanxin Liu, Chunqi Pan, Ying Jian, Mingwei Wang, Bin Ni, Chan-Yen Kuo
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Effects of nonpharmacological intervention on sleep quality in hemodialysis patients
Hui Li, Long Zuo, Siyu Long, Baifei Li
Medicine.2021; 100(27): e26401. CrossRef - The effect of foot reflexology massage on delirium and sleep quality following cardiac surgery: A randomized clinical trial
Ahmad Fazlollah, Hosein Babatabar Darzi, Esmail Heidaranlu, Seyed Tayeb Moradian
Complementary Therapies in Medicine.2021; 60: 102738. CrossRef - Comparing the Effect of Reflexology and Effleurage Massages on Fatigue and Insomnia in Multiple Sclerosis Patients
Sh. Sehat Nejad, A. Pour Samad, M. Behnam Moghadam, A. Mousavi zadeh, N. kaidani
Journal of Clinical Care and Skills.2021; 2(3): 139. CrossRef - Randomized controlled trial of the foot reflexology on pain and anxiety severity during dressing change in burn patients
Fahimeh Davodabady, Vahid Naseri-Salahshour, Mahbobeh Sajadi, Abolfazl Mohtarami, Fatemeh Rafiei
Burns.2021; 47(1): 215. CrossRef - Can foot reflexology be a complementary therapy for sleep disturbances? Evidence appraisal through a meta‐analysis of randomized controlled trials
Hui‐Chuan Huang, Kee‐Hsin Chen, Shu‐Fen Kuo, I‐Hui Chen
Journal of Advanced Nursing.2021; 77(4): 1683. CrossRef - Effect of foot reflexology on chest pain and anxiety in patients with acute myocardial infarction: A double blind randomized clinical trial
Saeedeh Sayari, Monir Nobahar, Raheb Ghorbani
Complementary Therapies in Clinical Practice.2021; 42: 101296. CrossRef - How Long Can they Stand it? Examining the Effectiveness of Reflexology and a Passive Relaxation Intervention in Improving Health Outcomes in Workers Who Stand
Kathryn Kavanagh, Linda Rhoades Shanock
Occupational Health Science.2021; 5(1-2): 95. CrossRef - The effects of reflexology on anxiety, depression and quality of life in patients with gynecological cancers with reference to Watson's theory of human caring
Sinem Göral Türkcü, Sevgi Özkan
Complementary Therapies in Clinical Practice.2021; 44: 101428. CrossRef - The effect of reflexology on sleep quality and fatigue in postmenopausal women: A randomized control trial
Leyla Zengin Aydın, Gülhan Yiğitalp
European Journal of Integrative Medicine.2021; 43: 101281. CrossRef - The Challenges and Perspectives of the Integration Between Virtual and Augmented Reality and Manual Therapies
Francesco Cerritelli, Marco Chiera, Marco Abbro, Valentino Megale, Jorge Esteves, Alberto Gallace, Andrea Manzotti
Frontiers in Neurology.2021;[Epub] CrossRef - Regards sur l’utilisation de la réflexologie palmaire lors d’entretiens cliniques auprès de personnes âgées institutionnalisées : un outil vecteur de bien-être et de qualité de vie ?
C. Moretto, A. Soubelet, C. Bonardi
NPG Neurologie - Psychiatrie - Gériatrie.2021; 21(121): 52. CrossRef - Relaxation interventions for improving sleep outcomes in perinatal women: A systematic review and meta-analysis of randomized controlled trials
Xing Yee Jolyn Tan, Shanise Yi Xin Choong, Ling Jie Cheng, Ying Lau
Midwifery.2021; 103: 103151. CrossRef - Effect of Foot Reflexology and Aromatherapy on Anxiety and Pain During Brachytherapy for Cervical Cancer
Lisa Blackburn, Catherine Hill, Amy Lindsey, Loraine Sinnott, Kathrynn Thompson, Allison Quick
Oncology Nursing Forum.2021; 48(3): 265. CrossRef - Effect of Reflexology in Treating Cancer Pain: A Meta-Analysis
Zhila Najafpour, Kamran Shayanfard
International Journal of Cancer Management.2020;[Epub] CrossRef - Effect of Foot Reflexology Intervention on Depression, Anxiety, and Sleep Quality in Adults: A Meta‐Analysis and Metaregression of Randomized Controlled Trials
Wei-Li Wang, Hao-Yuan Hung, Ying-Ren Chen, Kuang-Huei Chen, Szu-Nian Yang, Chi-Ming Chu, Yuan-Yu Chan, Gerhard Litscher
Evidence-Based Complementary and Alternative Medicine.2020;[Epub] CrossRef - The effect of foot reflexology massage on burn-specific pain anxiety and sleep quality and quantity of patients hospitalized in the burn intensive care unit (ICU)
Reza Alinia-najjar, Masoumeh Bagheri-Nesami, Seyed Afshin Shorofi, Seyed Nouraddin Mousavinasab, Kiarash Saatchi
Burns.2020; 46(8): 1942. CrossRef - Effect of Foot Reflexology on Pain, Fatigue, and Quality of Sleep after Kidney Transplantation Surgery: A Parallel Randomized Controlled Trial
Atena Samarehfekri, Mahlagha Dehghan, Mansoor Arab, Mohammad Reza Ebadzadeh, Albert Moraska
Evidence-Based Complementary and Alternative Medicine.2020;[Epub] CrossRef - Effect of reflexology on anxiety and sleep of informal cancer caregiver: Randomized controlled trial
İsmail Toygar, Öznur Usta Yeşilbalkan, Yasemin Güzel Malseven, Esra Sönmez
Complementary Therapies in Clinical Practice.2020; 39: 101143. CrossRef - Effectiveness of reflexology on anxiety of patients undergoing cardiovascular interventional procedures: A systematic review and meta‐analysis of randomized controlled trials
Ramesh Chandrababu, Eilean Lazarus Rathinasamy, C. Suresh, Jyothi Ramesh
Journal of Advanced Nursing.2019; 75(1): 43. CrossRef - Effects of reflexology on premenstrual syndrome: a systematic review and meta-analysis
Marzieh Hasanpour, Mohammad Mehdi Mohammadi, Habib Shareinia
BioPsychoSocial Medicine.2019;[Epub] CrossRef - La réflexologie plantaire
Emmanuelle Pinon Cartron
Soins Aides-Soignantes.2019; 16(89): 17. CrossRef - Réflexologie dans les troubles du sommeil
Alexandra Lemercier
Hegel.2019; N° 3(3): 246. CrossRef - The effects of sleep hygiene education and reflexology on sleep quality and fatigue in patients receiving chemotherapy
Leyla Zengin, Rukuye Aylaz
European Journal of Cancer Care.2019;[Epub] CrossRef - The effect of foot reflexology massage on breast milk volume of mothers with premature infants: A randomized controlled trial
Parisa Mirzaie, Sakineh Mohammad-Alizadeh-Charandabi, Sakineh Goljarian, Mojgan Mirghafourvand, Mohammad Bager Hoseinie
European Journal of Integrative Medicine.2018; 17: 72. CrossRef - Evaluation des réflexothérapies en 2018
Nathalie Thilly
Hegel.2018; N° 1(1): 76a. CrossRef - The Effectiveness of Foot Reflexology in the Severity of Restless Legs Syndrome in Female Patients Undergoing Dialysis: A Randomized Controlled Trial
Mahbobeh Ghasemi, Nahid Rejeh, Majideh Heravi-Karimooi, Seyed Davood Tadrisi, Parvaneh Samady Kia
Critical Care Nursing.2018;[Epub] CrossRef - Investigating the Impact of Foot Reflexology on Severity of Fatigue in Patients Undergoing Hemodialysis: A Clinical Trial Study
Simin Sharifi, Ali Navidian, Mozhgan Jahantigh, Abouzar Shamsoddini Lori
Medical - Surgical Nursing Journal.2018;[Epub] CrossRef - The effects of reflexology on pain and sleep deprivation in patients with rheumatoid arthritis: A randomized controlled trial
Ercan Bakir, Sevgin Samancioglu Baglama, Savas Gursoy
Complementary Therapies in Clinical Practice.2018; 31: 315. CrossRef - Réflexologie dans les troubles du sommeil
Alexandra Lemercier
Hegel.2018; N° 1(1): 95. CrossRef - The effect of acupressure stimulation of ST-36 – Zusanli, point on lower limbs explosive strength
Dariusz Mucha, Tadeusz Ambroży, Dawid Mucha
European Journal of Integrative Medicine.2017; 11: 59. CrossRef - Effects of foot massage applied in two different methods on symptom control in colorectal cancer patients: Randomised control trial
Neşe Uysal, Sevinç Kutlutürkan, Işıl Uğur
International Journal of Nursing Practice.2017;[Epub] CrossRef - El masaje, una técnica basada en la evidencia
T. Rulleau, C. Rivette, L. Toussaint
EMC - Kinesiterapia - Medicina Física.2017; 38(3): 1. CrossRef - A comparison the effects of reflexology and relaxation on the psychological symptoms in women with multiple sclerosis
Mozhgan Soheili, Fatemeh Nazari, Vahid Shaygannejad, Mahboobeh Valiani
Journal of Education and Health Promotion.2017;[Epub] CrossRef - Reflexology and polysomnography: Changes in cerebral wave activity induced by reflexology promote N1 and N2 sleep stages
N. Esmel-Esmel, E. Tomás-Esmel, M. Tous-Andreu, A. Bové-Ribé, M. Jiménez-Herrera
Complementary Therapies in Clinical Practice.2017; 28: 54. CrossRef - European guideline for the diagnosis and treatment of insomnia
Dieter Riemann, Chiara Baglioni, Claudio Bassetti, Bjørn Bjorvatn, Leja Dolenc Groselj, Jason G. Ellis, Colin A. Espie, Diego Garcia‐Borreguero, Michaela Gjerstad, Marta Gonçalves, Elisabeth Hertenstein, Markus Jansson‐Fröjmark, Poul J. Jennum, Damien Leg
Journal of Sleep Research.2017; 26(6): 675. CrossRef - S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen
D. Riemann, E. Baum, S. Cohrs, T. Crönlein, G. Hajak, E. Hertenstein, P. Klose, J. Langhorst, G. Mayer, C. Nissen, T. Pollmächer, S. Rabstein, A. Schlarb, H. Sitter, H.-G. Weeß, T. Wetter, K. Spiegelhalder
Somnologie.2017; 21(1): 2. CrossRef - Il massaggio, approccio basato sulle evidenze
T. Rulleau, C. Rivette, L. Toussaint
EMC - Medicina Riabilitativa.2017; 24(3): 1. CrossRef - Foot Reflexotherapy Induces Analgesia in Elderly Individuals with Low Back Pain: A Randomized, Double‐Blind, Controlled Pilot Study
Bruna Hoffmann de Oliveira, Anna Quialheiro de Abreu da Silva, Daniela Dero Ludtke, Fernanda Madeira, Graciela Mendonça da Silva Medeiros, Rodolfo Borges Parreira, Afonso Shiguemi Inoue Salgado, Luiz Augusto Oliveira Belmonte, Francisco José Cidral-Filho,
Evidence-Based Complementary and Alternative Medicine.2017;[Epub] CrossRef - The effect of foot reflexology and back massage on hemodialysis patients' fatigue and sleep quality
Kevser Sevgi Unal, Reva Balci Akpinar
Complementary Therapies in Clinical Practice.2016; 24: 139. CrossRef - Influence of Study Design on Outcomes Following Reflexology Massage: An Integrative and Critical Review of Interventional Studies
Andrew McVicar, Christina Greenwood, Carol Ellis, Chantelle LeForis
The Journal of Alternative and Complementary Medicine.2016; 22(9): 739. CrossRef - A comparison of the effects of reflexology and relaxation on pain in women with multiple sclerosis
Fatemeh Nazari, Mozhgan Soheili, SayedMohsen Hosseini, Vahid Shaygannejad
Journal of Complementary and Integrative Medicine.2016; 13(1): 65. CrossRef - L’impact de la réflexologie plantaire sur le stress des professionnels de santé
Mireille Guillon, Françoise Bourdarias, Nathalie Lecour
Revue internationale de soins palliatifs.2016; Vol. 30(3): 135. CrossRef - The effects of two methods of reflexology and stretching exercises on the severity of restless leg syndrome among hemodialysis patients
Nahid Shahgholian, ShahrzadKhojandi Jazi, Jahangir Karimian, Mahboubeh Valiani
Iranian Journal of Nursing and Midwifery Research.2016; 21(3): 219. CrossRef - Complementary and Alternative Medicine Therapies as Symptom Management Strategies for the Late Effects of Breast Cancer Treatment
Ashley M. Henneghan, Tracie Harrison
Journal of Holistic Nursing.2015; 33(1): 84. CrossRef - Topography of spinal column and kidney receptors as illustrated by microsystem of the foot
Tadeusz Kasperczyk, Robert Walaszek
Journal of Traditional Chinese Medicine.2015; 35(3): 329. CrossRef - Self-Administered Foot Reflexology for the Management of Chronic Health Conditions: A Systematic Review
Hyun Jin Song, Sun Mi Choi, Hyun-Ju Seo, Heeyoung Lee, Heejeong Son, Sanghun Lee
The Journal of Alternative and Complementary Medicine.2015; 21(2): 69. CrossRef - Effect of self-administered foot reflexology for symptom management in healthy persons: A systematic review and meta-analysis
Hyun Jin Song, Heejeong Son, Hyun-Ju Seo, Heeyoung Lee, Sun Mi Choi, Sanghun Lee
Complementary Therapies in Medicine.2015; 23(1): 79. CrossRef - The effect of foot reflexology on physiologic parameters and mechanical ventilation weaning time in patients undergoing open-heart surgery: A clinical trial study
Abbas Ebadi, Parastoo Kavei, Seyyed Tayyeb Moradian, Yaser Saeid
Complementary Therapies in Clinical Practice.2015; 21(3): 188. CrossRef - Healing Art of Hand: Reflexology
H. Dilek Doğan
European Journal of Basic Medical Sciences.2014; 4(4): 89. CrossRef - The Physiological and Biochemical Outcomes Associated with a Reflexology Treatment: A Systematic Review
J. E. M. McCullough, S. D. Liddle, M. Sinclair, C. Close, C. M. Hughes, Peter Mackereth
Evidence-Based Complementary and Alternative Medicine.2014;[Epub] CrossRef - Meta-Analysis of Spiritual Intervention Studies on Biological, Psychological, and Spiritual Outcomes
Pok-Ja Oh, Young-Hyun Kim
Journal of Korean Academy of Nursing.2012; 42(6): 833. CrossRef - RECENT LITERATURE
Focus on Alternative and Complementary Therapies.2012;[Epub] CrossRef - RECENT LITERATURE
Focus on Alternative and Complementary Therapies.2012;[Epub] CrossRef
- Combined effects of reflexology massage and respiratory relaxation on pain following chest tube removal in heart surgery patients
- 3,587 View
- 99 Download
- 84 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


