Search
- Page Path
- HOME > Search
- Mediating effect of grit on the influence of nurses’ silence behavior on medication safety competence: a cross-sectional study
- Haengsuk Kim, Wanju Park
- J Korean Acad Nurs 2025;55(1):81-92. Published online February 20, 2025
- DOI: https://doi.org/10.4040/jkan.24088
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
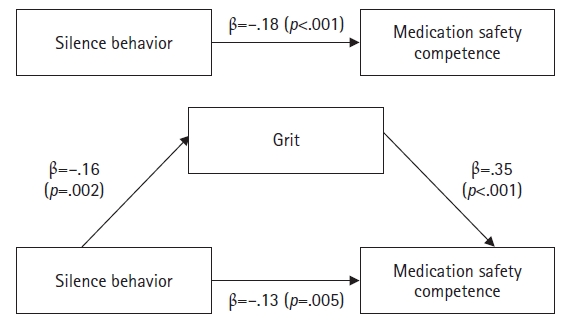
This study investigated the mediating effect of grit in the relationship between silence behavior and medication safety competence among nurses.
Methods
The study included 166 nurses from four university hospitals and general hospitals in Seoul and Gyeonggi-do, South Korea. Data were collected from March 1 to 10, 2024, using self-report questionnaires. Data were analyzed using the t-test, analysis of variance, Scheffé’s test, and Pearson’s correlation coefficients with IBM SPSS Statistics ver. 23.0 (IBM Corp.). A mediation analysis was performed using Hayes’s PROCESS macro model 4 and the bootstrapping method.
Results
Medication safety competence showed significant correlations with silence behavior (r=–.21, p=.008) and grit (r=.43, p<.001). Furthermore, grit partially mediated the relationship between silence behavior and medication safety competence.
Conclusion
This study indicates that grit is a significant mediator in the relationship between silence behavior and medication safety competence. Therefore, an integrated approach that reduces silence behavior and promotes grit is essential for strengthening nurses’ medication safety competence. Ultimately, these strategies will help ensure patient safety by improving medication safety competence.
- 5,405 View
- 468 Download

- Structural Topic Modeling Analysis of Patient Safety Interest among Health Consumers in Social Media
- Nari Kim, Nam-Ju Lee
- J Korean Acad Nurs 2024;54(2):266-278. Published online May 31, 2024
- DOI: https://doi.org/10.4040/jkan.23156
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to investigate healthcare consumers’ interest in patient safety on social media using structural topic modeling (STM) and to identify changes in interest over time.
Methods
Analyzing 105,727 posts from Naver news comments, blogs, internet cafés, and Twitter between 2010 and 2022, this study deployed a Python script for data collection and preprocessing. STM analysis was conducted using R, with the documents’ publication years serving as metadata to trace the evolution of discussions on patient safety.
Results
The analysis identified a total of 13 distinct topics, organized into three primary communities: (1) “Demand for systemic improvement of medical accidents,” underscoring the need for legal and regulatory reform to enhance accountability; (2) “Efforts of the government and organizations for safety management,” highlighting proactive risk mitigation strategies; and (3) “Medical accidents exposed in the media,” reflecting widespread concerns over medical negligence and its repercussions. These findings indicate pervasive concerns regarding medical accountability and transparency among healthcare consumers.
Conclusion
The findings emphasize the importance of transparent healthcare policies and practices that openly address patient safety incidents. There is clear advocacy for policy reforms aimed at increasing the accountability and transparency of healthcare providers. Moreover, this study highlights the significance of educational and engagement initiatives involving healthcare consumers in fostering a culture of patient safety. Integrating consumer perspectives into patient safety strategies is crucial for developing a robust safety culture in healthcare. -
Citations
Citations to this article as recorded by- From Posts to Protection: Understanding User-Generated Safety Content on Reddit
Mashael Yousef Almoqbel
International Journal of Computational and Experimental Science and Engineering.2025;[Epub] CrossRef
- From Posts to Protection: Understanding User-Generated Safety Content on Reddit
- 2,166 View
- 70 Download
- 1 Crossref

- Patient Safety Management Activities of Korean Nurses: A Meta-Analytic Path Analysis
- Seohee Jeong, Seok Hee Jeong
- J Korean Acad Nurs 2022;52(4):363-377. Published online August 31, 2022
- DOI: https://doi.org/10.4040/jkan.22022
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to test a hypothetical model of Korean nurses’ patient safety management activities using meta-analytic path analysis.
Methods
A systematic review, meta-analysis, and meta-analytic path analysis were conducted following the PRISMA and MOOSE guidelines. Seventy-four studies for the meta-analysis and 92 for the meta-analytic path analysis were included. The R software program (Version 3.6.3) was used for data analysis.
Results
Four variables out of 49 relevant variables were selected in the meta-analysis. These four variables showed large effect sizes (ESr = .54) or median effect sizes (ESr = .33∼.40) with the highest k (number of studies) in the individual, job, and organizational categories. The hypothetical model for the meta-analytic path analysis was established using these variables and patient safety management activities. Twelve hypothetical paths were set and tested. Finally, the perception of the importance of patient safety management and patient safety competency directly affected patient safety management activities. In addition, self-efficacy, the perception of the importance of patient safety management, patient safety competency, and patient safety culture, indirectly affected patient safety management activities.
Conclusion
Self-efficacy, the perception of the importance of patient safety management, patient safety competency, and the organization’s patient safety culture should be enhanced to improve nurses’ patient safety management activities. -
Citations
Citations to this article as recorded by- Development and validation of patient safety educational booklet to empower anesthesia process owners to improve safety compliance before, during and after anesthesia
Fatemeh Asadi, Azam Saei, Shanam Sedigh Maroufi, Jamileh Abolghasemi
Journal of Education and Health Promotion.2025;[Epub] CrossRef - Development of a patient safety management protocol for nurses in long-term care hospitals
Soon-Ock Kim
Scientific Reports.2025;[Epub] CrossRef - Impact of Clinical Nurses' Patient Safety Competency, Psychological Safety, and Nursing Unit Manager's Safety-Specific Transformational Leadership on Intention to Report Near Misses
Young hyun Cho, Seung Eun Lee, Mi Jeong Kwak, Hyun Joo Lee
Quality Improvement in Health Care.2025; 31(2): 60. CrossRef - The influencing factors of pediatric nurses’ perception of patient safety culture and partnership with patients’ parents on patient safety nursing activities in South Korea: a descriptive study
Seo Jin Lee, Young Ran Han
Child Health Nursing Research.2024; 30(4): 255. CrossRef - Effects of Nurse-Nurse Collaboration and Nurse-Physician Collaboration on Nursing Performance in Nurses: The Mediating Effect of Patient Safety Management Activities
JaHyun Kim, Seok Hee Jeong, Hee Sun Kim, Sunmi Kim
Journal of Korean Academy of Nursing Administration.2024; 30(4): 343. CrossRef - Mediating Effects of Job Satisfaction between Nurses’ Perceptions of Patient Safety Culture and Their Safety Nursing Activities
I Jung Han, Young Ran Han
Journal of Korean Academy of Fundamentals of Nursing.2023; 30(1): 46. CrossRef - The Effects of Professional Autonomy, Job Satisfaction, and Perceived Patient-Safety Culture on Nurses' Patient-Safety Management Activities: A Cross-Sectional Study
Bokja Koak, Junglim Seo, Eunji Song, Haneul Shin, Jaehee Jeon
Korean Journal of Adult Nursing.2023; 35(2): 117. CrossRef
- Development and validation of patient safety educational booklet to empower anesthesia process owners to improve safety compliance before, during and after anesthesia
- 3,901 View
- 196 Download
- 3 Web of Science
- 7 Crossref

- Effect of Patient Safety Training Program of Nurses in Operating Room
- Peijia Zhang, Xin Liao, Jie Luo
- J Korean Acad Nurs 2022;52(4):378-390. Published online August 31, 2022
- DOI: https://doi.org/10.4040/jkan.22017
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study developed an in-service training program for patient safety and aimed to evaluate the impact of the program on nurses in the operating room (OR).
Methods
A pretest–posttest self-controlled survey was conducted on OR nurses from May 6 to June 14, 2020. An in-service training program for patient safety was developed on the basis of the knowledge–attitude–practice (KAP) theory through various teaching methods. The levels of safety attitude, cognition, and attitudes toward the adverse event reporting of nurses were compared to evaluate the effect of the program. Nurses who attended the training were surveyed one week before the training (pretest) and two weeks after the training (posttest).
Results
A total of 84 nurses participated in the study. After the training, the scores of safety attitude, cognition, and attitudes toward adverse event reporting of nurses showed a significant increase relative to the scores before the training (p < .001). The effects of safety training on the total score and the dimensions of safety attitude, cognition, and attitudes toward nurses’ adverse event reporting were above the moderate level.
Conclusion
The proposed patient safety training program based on KAP theory improves the safety attitude of OR nurses. Further studies are required to develop an interprofessional patient safety training program. In addition to strength training, hospital managers need to focus on the aspects of workflow, management system, department culture, and other means to promote safety culture. -
Citations
Citations to this article as recorded by- Implementation strategies by leaders and health professionals to improve the safety climate in the operating room: a scoping review
Rosilene Alves Ferreira, Eduardo José Ferreira Santos, Olga Maria Pimenta Lopes Ribeiro, Danielle Mendonça Henrique, Flavia Giron Camerini, Andressa Aline Bernardo Bueno, Soraia Cristina de Abreu Pereira, Vivian Schutz, Marcia Valeria Rosa Lima, Cintia Si
BMJ Open.2026; 16(1): e109055. CrossRef - Correlation analysis of satisfaction with subspecialty management model in operating rooms: a cross-sectional survey in China
W. Wang, J. Shen, Y. Ma, Y. Chen, R. Gong, Q. Qian, Y. Sun
BMC Nursing.2025;[Epub] CrossRef - Effect of Counting Error Prevention Training on Operating Room Nurses’ Counting Error Prevention Awareness and Perceptions of Patient Safety
Myung Jin JANG, Mi Kyung HONG, Mi Jeong LEE, Kyung A LEE, Yang Ok KIM, Jin A JEON, Hana KO
Korean Journal of Health Promotion.2024; 24(1): 20. CrossRef
- Implementation strategies by leaders and health professionals to improve the safety climate in the operating room: a scoping review
- 5,023 View
- 201 Download
- 3 Web of Science
- 3 Crossref

- Effects of Second Victim Experiences after Patient Safety Incidents on Nursing Practice Changes in Korean Clinical Nurses: The Mediating Effects of Coping Behaviors
- Seohee Jeong, Seok Hee Jeong
- J Korean Acad Nurs 2021;51(4):489-504. Published online August 31, 2021
- DOI: https://doi.org/10.4040/jkan.21089
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was investigated the mediating effect of coping behaviors in the relationship between the second victim experiences after patient safety incidents and the nursing practice changes.
Methods
A cross-sectional survey was performed using structured questionnaires. Participants were 218 clinical nurses in general tertiary hospitals in South Korea. Data were collected through an online survey and snowball sampling from August 11 to September 6 2020. Data were analyzed using SPSS 23.0 program. A mediation analysis was performed using multiple regression and a simple mediation model applying the PROCESS macro with 95% bias-corrected bootstrap confidence interval.
Results
The mean scores of second victim experiences was 3.41/5. Approach coping (β = .55, p < .001) and the avoidant coping (β = - .23, p = .001) showed mediation effects in the relationship between second victim experiences and constructive change in nursing practice. Avoidant coping (β = .29, p < .001) showed a mediation effect in the relationship between second victim experiences and defensive change in nursing practice.
Conclusion
Coping behaviors has a mediating effect on the relationship between second victim experiences and nursing practice changes. To ensure that nurses do not experience second victim, medical institutions should have a culture of patient safety that employs a systematic approach rather than blame individuals. They also need to develop strategies that enhance approach coping and reducing avoidant coping to induce nurses’ constructive practice changes in clinical nurses in experiencing second victims due to patient safety incidents. -
Citations
Citations to this article as recorded by- Influences of Clinical Nurses’ Second Victim Experience after Patient Safety Incidents, Individual and Organizational Support, and Job Satisfaction on Turnover Intention
Hyeran Kang, Jeong-Hee Kim
Journal of Korean Academy of Nursing Administration.2026; 32(1): 58. CrossRef - Factors influencing negative outcomes for nurses who experience patient safety incidents: An integrative review
Hanseulgi Lee, Nam‐Ju Lee, Nari Kim
International Nursing Review.2025;[Epub] CrossRef - How does just culture reduce negative work outcomes through second victim distress and demand for support in clinical nurses? A path analysis
Seohee Jeong, Sunmi Kim, Hyoung Eun Chang, Seok Hee Jeong
BMC Nursing.2025;[Epub] CrossRef - Changes in Nursing Practice Among Clinical Nurses After Experiencing a Patient Safety Incident: Partial Least Squares Structural Equation Modeling
Sunmi Kim, Seohee Jeong, Seok Hee Jeong, Majd Mrayyan
Journal of Nursing Management.2025;[Epub] CrossRef - Predictors of Nurses' Reporting Level by the Types of Patient Safety Incidents
Ju-Hee Kang, Yeojin Yi
Journal of Korean Academy of Nursing Administration.2025; 31(4): 434. CrossRef - The Relationship of Medication Safety Competence, Second Victim Experiences, Second Victim Support, and Negative Work Outcomes among Clinical Nurses
Ahlim Chang, Youngjin Lee, Minkyung Kang, Ji Yea Lee
Journal of Korean Academy of Nursing Administration.2025; 31(5): 493. CrossRef - “Learn from Errors”: Post-traumatic growth among second victims
Huanhuan Huang, Tong Liu, Ying Peng, Xingyao Du, Qi Huang, Qinghua Zhao, Mingzhao Xiao, Yetao Luo, Shuangjiang Zheng
BMC Public Health.2024;[Epub] CrossRef - Nurse Leader Perspectives and Experiences on Caregiver Support Following a Serious Medical Error
Marie M. Prothero, Madeline Sorhus, Katherine Huefner
JONA: The Journal of Nursing Administration.2024; 54(12): 664. CrossRef - Prevalence of the second victim phenomenon among intensive care unit nurses and the support provided by their organizations
Maria Kappes, Pilar Delgado‐Hito, Verónica Riquelme Contreras, Marta Romero‐García
Nursing in Critical Care.2023; 28(6): 1022. CrossRef - The mediating role of coping styles in the relationship between second victim experience and professional quality of life among nurses: a cross-sectional study
Xizhao Li, Chong Chin Che, Yamin Li, Ling Wang, Mei Chan Chong
BMC Nursing.2023;[Epub] CrossRef - Associations among workplace incivility, stress coping, and nursing performance in hospital nurses: A path analysis
Eun Ha Kim, Yeojin Yi
Journal of Nursing Scholarship.2023; 55(4): 834. CrossRef - Influence of Clinical Nurses’ Second-Victim Experience and Second-Victim Support in Relation to Patient Safety Incidents on Their Work-Related Outcomes
Su Jin Jung, Youngjin Lee, Sun Hyoung Bae
Journal of Korean Academy of Nursing Administration.2022; 28(4): 331. CrossRef - Profiles of second victim symptoms and desired support strategies among Korean nurses: A latent profile analysis
Eun Young Choi, Jeehee Pyo, Minsu Ock, Haeyoung Lee
Journal of Advanced Nursing.2022; 78(9): 2872. CrossRef
- Influences of Clinical Nurses’ Second Victim Experience after Patient Safety Incidents, Individual and Organizational Support, and Job Satisfaction on Turnover Intention
- 3,495 View
- 81 Download
- 10 Web of Science
- 13 Crossref

- Analysis of Subgroups with Lower Level of Patient Safety Perceptions Using Decision-Tree Analysis
- Sun Hwa Shin
- J Korean Acad Nurs 2020;50(5):686-698. Published online October 31, 2020
- DOI: https://doi.org/10.4040/jkan.20044
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was aimed to investigate experiences, perceptions, and educational needs related to patient safety and the factors affecting these perceptions.
Methods
Study design was a descriptive survey conducted in November 2019. A sample of 1,187 Koreans aged 20-80 years participated in the online survey. Based on previous research, the questionnaire used patient safety-related and educational requirement items, and the Patient Safety Perception Scale. Descriptive statistics and a decision tree analysis were performed using SPSS 25.0.
Results
The average patient safety perception was 71.71 (± 9.21). Approximately 95.9% of the participants reported a need for patient safety education, and 88.0% answered that they would participate in such education. The most influential factors in the group with low patient safety perceptions were the recognition of patient safety activities, age, preference of accredited hospitals, experience of patient safety problems, and willingness to participate in patient safety education.
Conclusion
It was confirmed that the vulnerable group for patient safety perception is not aware of patient safety activities and did not prefer an accredited hospital. To prevent patient safety accidents and establish a culture of patient safety, appropriate educational strategies must be provided to the general public. -
Citations
Citations to this article as recorded by- Structural Topic Modeling Analysis of Patient Safety Interest among Health Consumers in Social Media
Nari Kim, Nam-Ju Lee
Journal of Korean Academy of Nursing.2024; 54(2): 266. CrossRef - Analysis of Factors Related to Domestic Patient Safety Incidents Using Decision Tree Technique
Jieun Shin, Ji-Hoon Lee, Nam-Yi Kim
Risk Management and Healthcare Policy.2023; Volume 16: 1467. CrossRef - Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis
Eun-Hye Lee, Sun-Hwa Shin, Goo-Churl Jeong
International Journal of Environmental Research and Public Health.2022; 19(5): 2841. CrossRef - Development and Effectiveness of a Patient Safety Education Program for Inpatients
Sun Hwa Shin, Mi Jung Kim, Ho Jin Moon, Eun Hye Lee
International Journal of Environmental Research and Public Health.2021; 18(6): 3262. CrossRef
- Structural Topic Modeling Analysis of Patient Safety Interest among Health Consumers in Social Media
- 1,253 View
- 15 Download
- 5 Web of Science
- 4 Crossref

- Development and Evaluation of Electronic Health Record Data-Driven Predictive Models for Pressure Ulcers
- Seul Ki Park, Hyeoun-Ae Park, Hee Hwang
- J Korean Acad Nurs 2019;49(5):575-585. Published online January 15, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.5.575
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to develop predictive models for pressure ulcer incidence using electronic health record (EHR) data and to compare their predictive validity performance indicators with that of the Braden Scale used in the study hospital.
Methods A retrospective case-control study was conducted in a tertiary teaching hospital in Korea. Data of 202 pressure ulcer patients and 14,705 non-pressure ulcer patients admitted between January 2015 and May 2016 were extracted from the EHRs. Three predictive models for pressure ulcer incidence were developed using logistic regression, Cox proportional hazards regression, and decision tree modeling. The predictive validity performance indicators of the three models were compared with those of the Braden Scale.
Results The logistic regression model was most efficient with a high area under the receiver operating characteristics curve (AUC) estimate of 0.97, followed by the decision tree model (AUC 0.95), Cox proportional hazards regression model (AUC 0.95), and the Braden Scale (AUC 0.82). Decreased mobility was the most significant factor in the logistic regression and Cox proportional hazards models, and the endotracheal tube was the most important factor in the decision tree model.
Conclusion Predictive validity performance indicators of the Braden Scale were lower than those of the logistic regression, Cox proportional hazards regression, and decision tree models. The models developed in this study can be used to develop a clinical decision support system that automatically assesses risk for pressure ulcers to aid nurses.
-
Citations
Citations to this article as recorded by- Effect of an educational intervention on pressure ulcer documentation among tertiary hospital nurses in Jordan
Emran A Abu Aqoulah, Rosliza Abaul Manaf, Suriani Ismail, Salam Bani Hani, Aya Al-Ali
British Journal of Nursing.2025; 34(12): S30. CrossRef - Application of Air Pillows and Left‐Right Lateral Tilt Position to Prevent Increased Risk of Pressure Injuries in Bedridden Patients in the ICU: A Quasi‐Experimental Study
Nur Chayati, Wantonoro Wantonoro, Mahsuna Alfianti, Tiara Marthias
Health Science Reports.2025;[Epub] CrossRef - Development of a Pressure Injury Machine Learning Prediction Model and Integration into Clinical Practice: A Prediction Model Development and Validation Study
Ju Hee Lee, Jae Yong Yu, So Yun Shim, Kyung Mi Yeom, Hyun A Ha, Se Yong Jekal, Ki Tae Moon, Joo Hee Park, Sook Hyun Park, Jeong Hee Hong, Mi Ra Song, Won Chul Cha
Korean Journal of Adult Nursing.2024; 36(3): 191. CrossRef - Could we prove the nursing outcomes utilising clinical data warehouse? Effectiveness of pressure ulcer intervention in Korean tertiary hospital
Moonsook Kim, Se Yeon Park, Meihua Piao, Earom Lim, Soon Hwa Yoo, Minju Ryu, Hyo Yeon Lee, Hyejin Won
International Wound Journal.2023; 20(1): 201. CrossRef - Data‐driven approach to predicting the risk of pressure injury: A retrospective analysis based on changes in patient conditions
Yinji Jin, Ji‐Sun Back, Sun Ho Im, Jong Hyo Oh, Sun‐Mi Lee
Journal of Clinical Nursing.2023; 32(19-20): 7273. CrossRef - Factors Associated with Pressure Injury Among Critically Ill Patients in a Coronary Care Unit
Eunji Ko, Seunghye Choi
Advances in Skin & Wound Care.2022; 35(10): 1. CrossRef - Data-Driven Learning Teaching Model of College English Based on Mega Data Analysis
Jie Zhang, Tongguang Ni
Scientific Programming.2022; 2022: 1. CrossRef
- Effect of an educational intervention on pressure ulcer documentation among tertiary hospital nurses in Jordan
- 2,152 View
- 55 Download
- 6 Web of Science
- 7 Crossref

- Patient Safety Teaching Competency of Nursing Faculty
- Shinae Ahn, Nam-Ju Lee, Haena Jang
- J Korean Acad Nurs 2018;48(6):720-730. Published online January 15, 2018
- DOI: https://doi.org/10.4040/jkan.2018.48.6.720
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to investigate patient safety teaching competency of nursing faculty and the extent of teaching patient safety topics in the nursing curriculum.
Methods A national survey was conducted with full-time nursing faculty in 4-year nursing schools. Regional quota sampling method was used. An online survey was sent to 1,028 nursing faculty and 207 of them were completed. Among the 207, we analyzed data from 184 participants. The revised Health Professional Education in Patient Safety Survey was used. Data were analyzed using descriptive statistics, independent t-test, one-way ANOVA, Pearson's correlation analysis, and multiple linear regression analyses.
Results The faculty's self-confidence was lower than their perceived importance of patient safety education. The mean score of teaching patient safety was 3.52±0.67 out of 5, and the contents were mostly delivered through lectures. The extent of faculty's teaching varied depending on faculty's clinical career, teaching subjects, participation in practicum courses, and previous experience of patient safety education. The significant predictors of the extent of teaching patient safety were the faculty's self-confidence in teaching patient safety (β=.39) during clinical practicum, their perceived importance of patient safety education during lectures (β=.23), and the teaching subject (β=.15).
Conclusion To enhance the competency of nursing faculty for effective patient safety education, a patient safety education program tailored to faculty characteristics should be developed and continuously provided for faculty. In addition, it is necessary to improve patient safety curriculum, strengthen clinical and school linkages, and utilize various education methods in patient safety education.
-
Citations
Citations to this article as recorded by- Factors influencing patient safety competency in baccalaureate nursing students: A descriptive cross-sectional study
Shinae Ahn
Nurse Education Today.2025; 145: 106498. CrossRef - Transcultural Adaptation and Psychometric Properties of the Persian Version of the Nursing Student Competence Scale (NSCS)
Amir Jalali, Fatemeh Chavoshani, Raheleh Rasad, Niloufar Darvishi, Fatemeh Merati Fashi, Mahbod Khodamorovati, Khalil Moradi
SAGE Open Nursing.2024;[Epub] CrossRef - Comparing the effects of patient safety education using design thinking and case based learning on nursing students’ competence and professional socialization: A quasi-experimental design
Seongmi Moon, Soo Jung Chang
Heliyon.2024; 10(9): e29942. CrossRef - Analysis of the innovative development path of university civic education based on the era of big data
Xingang Chen, Ye Dong
Applied Mathematics and Nonlinear Sciences.2024;[Epub] CrossRef - The effects of flipped learning and gamification on nursing students’ patient safety education: A mixed method study
Soo Jung Chang, Geun Myun Kim, Jeong Ah Kim
Heliyon.2024; 10(8): e29538. CrossRef - Experiences of Patient Safety Education and Factors Affecting the Willingness to Participate in Patient Safety in Undergraduate Nursing Students in South Korea
Sun-Hwa Shin, On-Jeon Baek
Healthcare.2023; 12(1): 54. CrossRef - Evaluating a patient safety course for undergraduate nursing students: A quasi-experimental study
Seung Eun Lee, V. Susan Dahinten
Collegian.2023; 30(1): 75. CrossRef - Continuing professional development among social‐ and health‐care educators
Minna Koskimäki, Marja‐Leena Lähteenmäki, Kristina Mikkonen, Maria Kääriäinen, Camilla Koskinen, Hanne Mäki‐Hakola, Tuulikki Sjögren, Meeri Koivula
Scandinavian Journal of Caring Sciences.2021; 35(2): 668. CrossRef - Nursing Students’ Informal Learning of Patient Safety Management Activities
Nam-Yi Kim
Healthcare.2021; 9(12): 1635. CrossRef - Development and Validation of a Self-Efficacy Scale for Nursing Educators’ Role in Sri Lanka
Shyamamala S. Weerasekara, Jina Oh, Haeryun Cho, Mihae Im
International Journal of Environmental Research and Public Health.2021; 18(15): 7773. CrossRef - Developing an integrated curriculum for patient safety in an undergraduate nursing program: a case study
Yoonjung Ji, Hyeonkyeong Lee, Taewha Lee, Mona Choi, Hyejung Lee, Sanghee Kim, Hyunok Kim Do, Sunah Kim, Sang Hui Chu, Jeongok Park, Young Man Kim, Soyoon Park
BMC Nursing.2021;[Epub] CrossRef - Development and Evaluation of an Informatics System for Nursing Faculty to Improve Patient Safety Teaching Competency
Nam-Ju Lee, Shinae Ahn, Miseon Lee, Haena Jang
Journal of Korean Academy of Nursing Administration.2020; 26(5): 488. CrossRef - Patient safety education in pre‐registration nursing programmes in South Korea
S. E. Lee, V. Susan Dathinten, H. Do
International Nursing Review.2020; 67(4): 512. CrossRef
- Factors influencing patient safety competency in baccalaureate nursing students: A descriptive cross-sectional study
- 3,783 View
- 76 Download
- 11 Web of Science
- 13 Crossref

- Characteristics and Risk Factors for Falls in Tertiary Hospital Inpatients
- Eun-Ju Choi, Young-Shin Lee, Eun-Jung Yang, Ji-Hui Kim, Yeon-Hee Kim, Hyeoun-Ae Park
- J Korean Acad Nurs 2017;47(3):420-430. Published online January 15, 2017
- DOI: https://doi.org/10.4040/jkan.2017.47.3.420
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The aim of this study was to explore characteristics of and risk factors for accidental inpatient falls.
Methods Participants were classified as fallers or non-fallers based on the fall history of inpatients in a tertiary hospital in Seoul between June 2014 and May 2015. Data on falls were obtained from the fall report forms and data on risk factors were obtained from the electronic nursing records. Characteristics of fallers and non-fallers were analyzed using descriptive statistics. Risk factors for falls were identified using univariate analyses and logistic regression analysis.
Results Average length of stay prior to the fall was 21.52 days and average age of fallers was 61.37 years. Most falls occurred during the night shifts and in the bedroom and were due to sudden leg weakness during ambulation. It was found that gender, BMI, physical problems such elimination, gait, vision and hearing and medications such as sleeping pills, antiarrhythmics, vasodilators, and muscle relaxant were statistically significant factors affecting falls.
Conclusion The findings show that there are significant risk factors such as BMI and history of surgery which are not part of fall assessment tools. There are also items on fall assessment tools which are not found to be significant such as mental status, emotional unstability, dizziness, and impairment of urination. Therefore, these various risk factors should be examined in the fall risk assessments and these risk factors should be considered in the development of fall assessment tools.
-
Citations
Citations to this article as recorded by- Perceptions and practices of rehabilitation specialist nurses in fall management: a qualitative study
Heli Zhang, Jianfen Luo, Xiaotian Zhang, Yuting Jiang, Xiaoyu Sun, Qi Tang, Xin Wang, Baohua Li
Frontiers in Public Health.2026;[Epub] CrossRef - Evaluation of intrinsic and extrinsic fall risk factors in hospitals, long-term facilities, and homes: A narrative review
A.C. Dondi, K.G. Davis
Human Factors in Healthcare.2026; 9: 100125. CrossRef - Prevalence of bed falls among inpatients in Iranian hospitals: A meta-analysis
Parvaneh Isfahani, Mohammad Sarani, Mina Salajegheh, Somayeh Samani, Aliyeh Bazi, Mahdieh Poodineh Moghadam, Fatemeh Boulagh, Mahnaz Afshari
Human Factors in Healthcare.2025; 7: 100093. CrossRef - Evaluation of Risk Factors for Fall Incidence Based on Statistical Analysis
Da Hye Moon, Tae-Hoon Kim, Myoung-Nam Lim, Seon-Sook Han
International Journal of Environmental Research and Public Health.2025; 22(5): 748. CrossRef - Experiences of nurse managers in preventing and managing inpatient falls: a qualitative descriptive study
Erge Jia, Yan Kang, Runv Zhou, Weiying Zhang, Xueyan Li
BMJ Open.2025; 15(12): e106509. CrossRef - Sensitivity of Fall Risk Perception and Associated Factors in Hospitalized Patients with Mental Disorders
Ji Young Kim, Sung Reul Kim, Yusun Park, Jin Kyeong Ko, Eunmi Ra
Asian Nursing Research.2024; 18(5): 443. CrossRef - Psychometric Properties of the Fall Risk Perception Questionnaire-Short Version for Inpatients in Acute Care Hospitals
Jeeeun Choi, Sujin Lee, Eunjin Park, Sangha Ku, Sunhwa Kim, Wonhye Yu, Eunmi Jeong, Sukhee Park, Yusun Park, Hye Young Kim, Sung Reul Kim
Journal of Korean Academy of Nursing.2024; 54(2): 151. CrossRef - The Impact of Physical Performance and Fear of Falling on Fall Risk in Hemodialysis Patients: A Cross-Sectional Study
Jiwon Choi, Sun-Kyung Hwang
Korean Journal of Adult Nursing.2024; 36(1): 63. CrossRef - The Impact of Possible Sarcopenia and Obesity on the Risk of Falls in Hospitalized Older Patients
Kahyun Kim, Dukyoo Jung
The Korean Journal of Rehabilitation Nursing.2023; 26(1): 18. CrossRef - Analysis of Data on Accidental Falls from the Hospital Incident Reporting in a General Hospital
Yu-ri Jang, Jeong Yun Park
Quality Improvement in Health Care.2023; 29(1): 15. CrossRef - Predication of Falls in Hospitalized Cancer Patients
Jun-Nyun Kim, Sun-Hwa Beak, Bo-Seop Lee, Mi-Ra Han
Asian Oncology Nursing.2023; 23(2): 56. CrossRef - Nurses’ Burden of Elimination Care: Sequential Explanatory Mixed-Methods Design
Se Young Jung, Hui-Woun Moon, Da Som Me Park, Sumi Sung, Hyesil Jung
International Journal of General Medicine.2023; Volume 16: 4067. CrossRef - Clinical study of falls among inpatients with hematological diseases and exploration of risk prediction models
Jing Wang, Bin Chen, Fang Xu, Qin Chen, Jing Yue, Jingjing Wen, Fang Zhao, Min Gou, Ya Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - A Clinical Data Warehouse Analysis of Risk Factors for Inpatient Falls in a Tertiary Hospital: A Case-Control Study
Eunok Kwon, Sun Ju Chang, Mikyung Kwon
Journal of Patient Safety.2023; 19(8): 501. CrossRef - Z-drugs and falls in nursing home patients: data from the INCUR study
Sarah Damanti, Moreno Tresoldi, Philipe de Souto Barreto, Yves Rolland, Matteo Cesari
Aging Clinical and Experimental Research.2022; 34(12): 3145. CrossRef - The Fall Risk Screening Scale Is Suitable for Evaluating Adult Patient Fall
Li-Chen Chen, Yung-Chao Shen, Lun-Hui Ho, Whei-Mei Shih
Healthcare.2022; 10(3): 510. CrossRef - Comparisons of Fall Prevention Activities Using Electronic Nursing Records: A Case-Control Study
Hyesil Jung, Hyeoun-Ae Park, Ho-Young Lee
Journal of Patient Safety.2022; 18(3): 145. CrossRef - Risk Factors according to Fall Risk Level in General Hospital Inpatients
Yeon Hwa Lee, Myo Sung Kim
Journal of Korean Academy of Fundamentals of Nursing.2022; 29(1): 35. CrossRef - Development and validation of the fall risk perception questionnaire for patients in acute care hospitals
Jieun Choi, Se Min Choi, Jeong Sin Lee, Soon Seok Seo, Ja Yeon Kim, Hye Young Kim, Sung Reul Kim
Journal of Clinical Nursing.2021; 30(3-4): 406. CrossRef - Factors Affecting the Degree of Harm from Fall Incidents in Hospitals
Shinae Ahn, Da Eun Kim
Journal of Korean Academy of Nursing Administration.2021; 27(5): 334. CrossRef - A Machine Learning–Based Fall Risk Assessment Model for Inpatients
Chia-Hui Liu, Ya-Han Hu, Yu-Hsiu Lin
CIN: Computers, Informatics, Nursing.2021; 39(8): 450. CrossRef - Factors Influencing Falls in High- and Low-Risk Patients in a Tertiary Hospital in Korea
Young-Shin Lee, Eun-Ju Choi, Yeon-Hee Kim, Hyeoun-Ae Park
Journal of Patient Safety.2020; 16(4): e376. CrossRef - Impact of Hearing Loss on Patient Falls in the Inpatient Setting
Victoria L. Tiase, Kui Tang, David K. Vawdrey, Rosanne Raso, Jason S. Adelman, Shao Ping Yu, Jo R. Applebaum, Anil K. Lalwani
American Journal of Preventive Medicine.2020; 58(6): 839. CrossRef - Improving Prediction of Fall Risk Using Electronic Health Record Data With Various Types and Sources at Multiple Times
Hyesil Jung, Hyeoun-Ae Park, Hee Hwang
CIN: Computers, Informatics, Nursing.2020; 38(3): 157. CrossRef - Triggers and Outcomes of Falls in Hematology Patients: Analysis of Electronic Health Records
Min Kyung Jung, Sun-Mi Lee
Journal of Korean Academy of Fundamentals of Nursing.2019; 26(1): 1. CrossRef - Incidence of Falls and Risk Factors of Falls in Inpatients
Soo-Jin Yoon, Chun-Kyon Lee, In-Sun Jin, Jung-Gu Kang
Quality Improvement in Health Care.2018; 24(2): 2. CrossRef
- Perceptions and practices of rehabilitation specialist nurses in fall management: a qualitative study
- 2,668 View
- 44 Download
- 26 Crossref

- Operating Room Nurses' Experiences of Securing for Patient Safety
- Kwang-Ok Park, Jong Kyung Kim, Myoung-Sook Kim
- J Korean Acad Nurs 2015;45(5):761-772. Published online October 30, 2015
- DOI: https://doi.org/10.4040/jkan.2015.45.5.761
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to evaluate the experience of securing patient safety in hospital operating rooms.
Methods Experiential data were collected from 15 operating room nurses through in-depth interviews. The main question was "Could you describe your experience with patient safety in the operating room?". Qualitative data from the field and transcribed notes were analyzed using Strauss and Corbin's grounded theory methodology.
Results The core category of experience with patient safety in the operating room was 'trying to maintain principles of patient safety during high-risk surgical procedures'. The participants used two interactional strategies: 'attempt continuous improvement', 'immersion in operation with sharing issues of patient safety'.
Conclusion The results indicate that the important factors for ensuring the safety of patients in the operating room are manpower, education, and a system for patient safety. Successful and safe surgery requires communication, teamwork and recognition of the importance of patient safety by the surgical team.
-
Citations
Citations to this article as recorded by- AMELİYATHANEDE STAJ YAPAN ÖĞRENCİLERİN STAJLARINA İLİŞKİN GÖRÜŞLERİNİN İNCELENMESİ
Gül Özlem Yıldırım, Bektaş Sarı
İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi.2024; 12(2): 735. CrossRef - Influences of Teamwork and Job Burnout on Patient Safety Management Activities among Operating Room Nurses
Ayoung Kim, Haein Lee
Journal of Korean Academy of Nursing Administration.2022; 28(5): 605. CrossRef - Effects of Patient Safety Culture on Nurse Burnout in the Operating Room
Ye Sol Lee, Chin Kang Koh
Stress.2020; 28(3): 118. CrossRef - Development of a protocol for procedures utilizing local anaesthesia and moderate sedation in the operating room
Eunha Ryoo, Soyoung Yu
Perioperative Care and Operating Room Management.2020; 20: 100100. CrossRef - Experience of Communication for Patient Safety by Perioperative Nurses
Shinae Ahn, Nam-Ju Lee
Journal of Korean Academy of Nursing Administration.2019; 25(4): 329. CrossRef - Effect of Nurses' Perception of Patient Safety Culture on Reporting of Patient Safety Events
Sun Aee Kim, Eun-Mi Kim, Ju-Ry Lee, Eui Geum Oh
Journal of Korean Academy of Nursing Administration.2018; 24(4): 319. CrossRef - The Impact of Safety Climate and Fatigue on Safety Performance of Operating Room Nurses
U-Eun Choi, Hyun-Young Kim
Journal of Korean Academy of Nursing Administration.2016; 22(5): 471. CrossRef
- AMELİYATHANEDE STAJ YAPAN ÖĞRENCİLERİN STAJLARINA İLİŞKİN GÖRÜŞLERİNİN İNCELENMESİ
- 1,823 View
- 41 Download
- 7 Crossref

- Factors related to Nurses' Patient Identification Behavior and the Moderating Effect of Person-organization Value Congruence Climate within Nursing Units
- Young Mee Kim, Seung-Wan Kang, Se Young Kim
- J Korean Acad Nurs 2014;44(2):198-208. Published online April 30, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.2.198
-
 Abstract
Abstract
 PDF
PDF Purpose This research was an empirical study designed to identify precursors and interaction effects related to nurses' patient identification behavior. A multilevel analysis methodology was used.
Methods A self-report survey was administered to registered nurses (RNs) of a university hospital in South Korea. Of the questionnaires, 1114 were analyzed.
Results The individual-level factors that had a significantly positive association with patient identification behavior were person-organization value congruence, organizational commitment, occupational commitment, tenure at the hospital, and tenure at the unit. Significantly negative group-level precursors of patient identification behavior were burnout climate and the number of RNs. Two interaction effects of the person-organization value congruence climate were identified. The first was a group-level moderating effect in which the negative relationship between the number of RNs and patient identification behavior was weaker when the nursing unit's value congruence climate was high. The second was a cross-level moderating effect in which the positive relationship between tenure at the unit and patient identification behavior was weaker when value congruence climate was high.
Conclusion This study simultaneously tested both individual-level and group-level factors that potentially influence patient identification behavior and identified the moderating role of person-organization value congruence climate. Implications of these results are discussed.
-
Citations
Citations to this article as recorded by- Content Analysis of Patient Safety Incident Reports Using Text Mining: A Secondary Data Analysis
On-Jeon Baek, Ho Jin Moon, Hyosun Kim, Sun-Hwa Shin
Korean Journal of Adult Nursing.2024; 36(4): 298. CrossRef - Compare Value Congruence of Nurse-Patient Assignment with Work Performance in Neonatal Intensive Care Unit
Hye Min Kim, Dong Yeon Kim, Ji Young Kim, Ga Young Kim, Seol Hee Moon
Journal of Korean Academy of Nursing Administration.2021; 27(5): 355. CrossRef - Structural empowerment and nurses’ patient identification behaviors: a cross-sectional study
Young Mee Kim, Se Young Kim
International Journal of Health Care Quality Assurance.2019; 32(5): 832. CrossRef
- Content Analysis of Patient Safety Incident Reports Using Text Mining: A Secondary Data Analysis
- 1,006 View
- 9 Download
- 3 Crossref

- Development and Validation of the Korean Patient Safety Culture Scale for Nursing Homes
- Sook Hee Yoon, Byungsoo Kim, Se Young Kim
- J Korean Acad Nurs 2013;43(3):379-388. Published online June 28, 2013
- DOI: https://doi.org/10.4040/jkan.2013.43.3.379
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to develop a tool to evaluate patient safety culture in nursing homes and to test its validity and reliability.
Methods A preliminary tool was developed through interviews with focus group, content validity tests, and a pilot study. A nationwide survey was conducted from February to April, 2011, using self-report questionnaires. Participants were 982 employees in nursing homes. Data were analyzed using Cronbach's alpha, item analysis, factor analysis, and multitrait/multi-Item analysis.
Results From the results of the analysis, 27 final items were selected from 49 items on the preliminary tool. Items with low correlation with total scale were excluded. The 4 factors sorted by factor analysis contributed 63.4% of the variance in the total scale. The factors were labeled as leadership, organizational system, working attitude, management practice. Cronbach's alpha for internal consistency was .95 and the range for the 4 factors was from .86 to .93.
Conclusion The results of this study indicate that the Korean Patient Safety Culture Scale has reliability and validity and is suitable for evaluation of patient safety culture in Korean nursing homes.
-
Citations
Citations to this article as recorded by- Factors Associated With Registered Nurses’ Safety Nursing Activities in Nursing Homes
Jiyeon Lee, Sunyeob Choi
Asian Nursing Research.2025; 19(1): 19. CrossRef - Factors Associated with the Patient Safety Activities among Home-Visit Caregiver: A Cross-Sectional Study
Soon-hee Cho, Sujin Kang, Youngji Kim
Annals of Geriatric Medicine and Research.2025; 29(2): 159. CrossRef - Institutional factors affecting patient safety culture and resident safety activities in long-term care facilities
Deulle Min
Geriatric Nursing.2025; 65: 103520. CrossRef - Psychometric evaluation of a Korean-language version of the Nursing Home Survey on Patient Safety Culture (K-NHSPSC)
Seung Eun Lee, So Young Park
BMC Nursing.2025;[Epub] CrossRef - Development and validation of the resident safety activity questionnaire for long-term care facility staff
Deulle Min, Suhee Kim
Geriatric Nursing.2024; 56: 278. CrossRef - The mediating effect of patient safety culture on the relationship between professionalism, self-leadership, and compliance with infection prevention activity against emerging respiratory infectious disease among nurses working in geriatric long-term care
Sun Young Jeong, Min Sun Song, Heeja Jung
Journal of Korean Gerontological Nursing.2024; 26(4): 360. CrossRef - Study of Patient Safety Culture Awareness of Radiological Technologists in Magnetic Resonance Imaging Laboratories
Min-Seo Park, Dong-Ha Lee, Hyun-Jin Jo, Hea-Youn Cho, Yeong-Cheol Heo
Journal of the Korean Society of MR Technology.2024; 34(1): 9. CrossRef - Developing a Cross-National Disability Measure for Older Adult Populations across Korea, China, and Japan
Sanghun Nam, Mi Jung Lee, Ickpyo Hong
International Journal of Environmental Research and Public Health.2022; 19(16): 10338. CrossRef - Patient safety measurement tools used in nursing homes: a systematic literature review
Kyoung-A Kim, Jungeun Lee, Dahee Kim, Deulle Min
BMC Health Services Research.2022;[Epub] CrossRef - Influence of Communication Self-efficacy and Perception of Patient Safety Culture on Experience of Nursing Errors among Operating Room Nurses
Jiin Seo, Yujeong Kim
Journal of Korean Academy of Nursing Administration.2021; 27(3): 181. CrossRef - Analysis of Subgroups with Lower Level of Patient Safety Perceptions Using Decision-Tree Analysis
Sun Hwa Shin
Journal of Korean Academy of Nursing.2020; 50(5): 686. CrossRef - Clinical Nurses' Safety Management Experiences with Older Patients
Hyunmee Cho, Suhye Kwon, Younhyang Lee, Yunjeong Kim, Jungmi Kang
Journal of Korean Gerontological Nursing.2020; 22(2): 105. CrossRef - Why Do They Stay? Intention to Stay among Registered Nurses in Nursing Homes
Ji Yeon Lee, Juh Hyun Shin
International Journal of Environmental Research and Public Health.2020; 17(22): 8485. CrossRef - Development and Validation of the Patient Safety Perception Scale for hospitalized Patients
Kyung Ja Kim, Eun Hee Lee, Sun Hwa Shin
Korean Journal of Adult Nursing.2018; 30(4): 404. CrossRef - Characteristics and Mortality Risk Factors in Geriatric Hospital Patients visiting One Region-wide Emergency Department
Kyoung Wan Kim, Soongnang Jang
Journal of Korean Academy of Community Health Nursing.2016; 27(4): 327. CrossRef - Awareness of Hospital Safety Culture and Safety Activities of Workers in a Tertiary Care Hospital
Eun-Ho Ha, Kyoung-Soon Hyun, Jin-Young Cho
The Journal of Korean Academic Society of Nursing Education.2016; 22(2): 191. CrossRef - A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study
Andrea Herepath, Martin Kitchener, Justin Waring
Health Services and Delivery Research.2015; 3(40): 1. CrossRef - Influence of Safety Culture Perception, Safety Control and Safety Management Activities as Perceived for Nurses in Nursing Home
Young-Sook Seo, Eun-Su Do
Journal of Digital Convergence.2015; 13(9): 303. CrossRef - Perception of Workers on Patient Safety Culture and Degree of Patient Safety in Nursing Homes in Korea
Sook Hee Yoon, Se Young Kim, XiangLian Wu
Journal of Korean Academy of Nursing Administration.2014; 20(3): 247. CrossRef
- Factors Associated With Registered Nurses’ Safety Nursing Activities in Nursing Homes
- 1,867 View
- 21 Download
- 19 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


