Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 46(5); 2016 > Article
-
Original Article
- Influences of Oral Health Behaviors, Depression and Stress on Periodontal Disease in Pregnant Women
- Hae-Jin Park, Hae Jung Lee, Soo Hyun Cho
-
Journal of Korean Academy of Nursing 2016;46(5):653-662.
DOI: https://doi.org/10.4040/jkan.2016.46.5.653
Published online: October 31, 2016
1Division of Nursing, Ilsin Christian Hospital, Busan·College of Nursing, Pusan National University, Yangsan, Korea.
2College of Nursing, Pusan National University, Yangsan, Korea.
3Dental Department, Ilsin Christian Hospital, Busan, Korea.
- Address reprint requests to: Lee, Hae Jung. College of Nursing, Pusan National University, 20 Geumo-ro, Mulgeum-eup, Yangsan-si, Gyeongsangnam-do, 50612, Korea. Tel: +82-51-510-8344, Fax: +82-51-510-8308, haejung@pusan.ac.kr
© 2016 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- The purpose of this study was to identify the influences of oral health behaviors, depression, and stress on periodontal disease in pregnant women.
-
Methods
- The participants in this study were 129 pregnant women. Data were collected using questionnaires which included individual characteristics, oral health care behaviors, the Center for Epidemiological Studies-Depression scale (CES-D), a global measure of perceived stress, and pregnancy stress. A dentist measured periodontal probing depth and classified stages of periodontal disease according to the Community Periodontal Index (CPI). Data were analyzed using descriptive statistics, Pearson correlation, and multiple regression.
-
Results
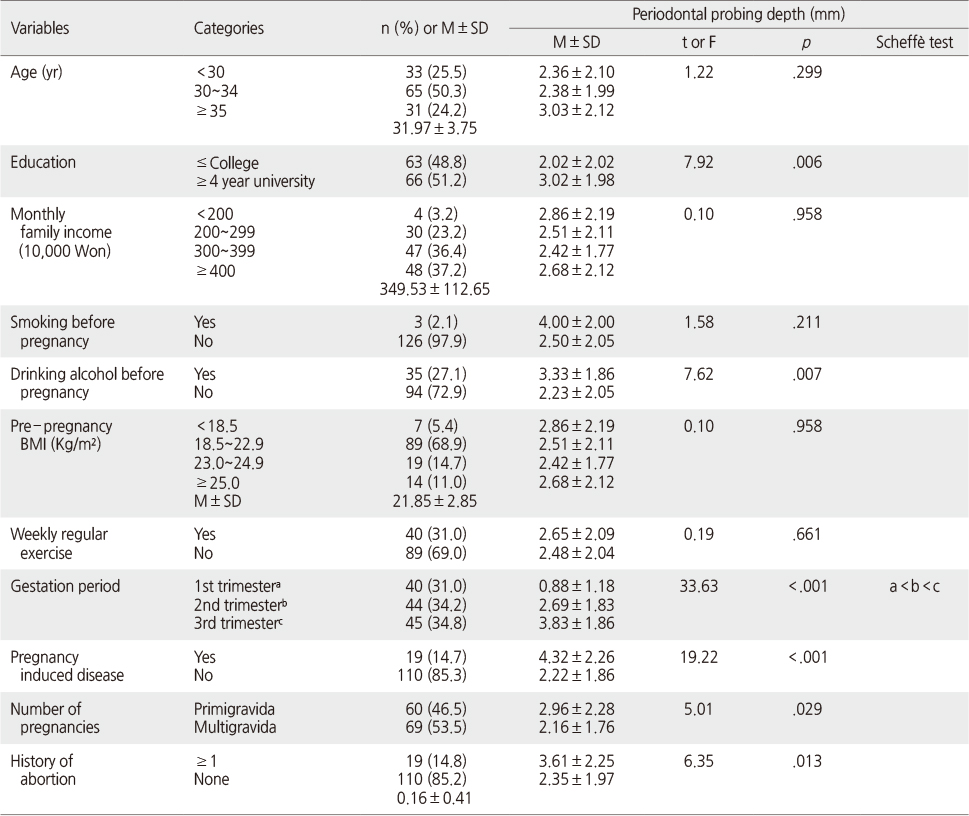
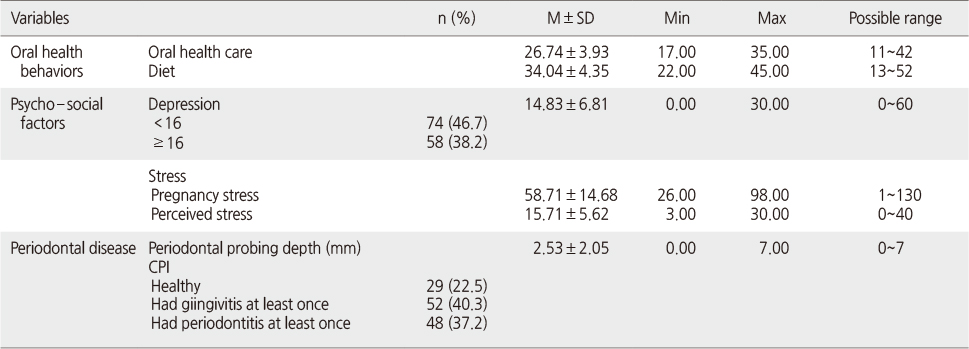
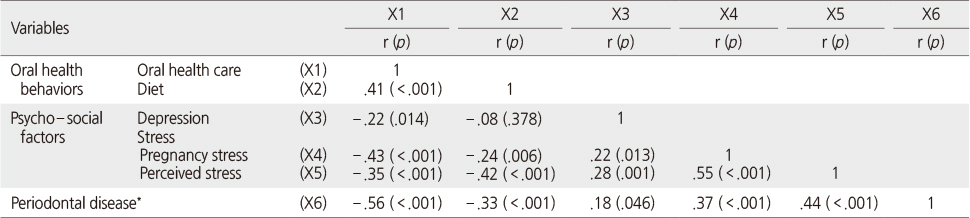
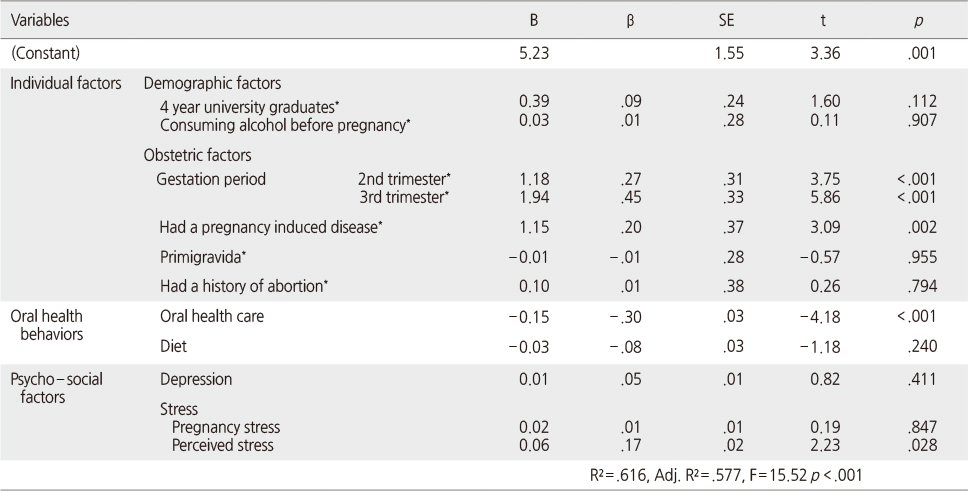
- Periodontal disease had significant correlations with oral health care behaviors (r=-.56, p <.001), perceived stress (r=.44 p <.001), pregnancy stress (r=.37 p <.001), diet (r=-.33, p <.001) and depression (r=.18 p =.046). Factors influencing periodontal disease for these pregnant women were being in the 2nd (β=.27, p <.001) or 3rd trimester (β=.45, p <.001), having a pregnancy induced disease (β=.20, p =.002), performing higher oral health behaviors (β=-.30, p <.001), and having higher perceived stress (β=.17, p =.028). The explanation power of this regression model was 61.6% (F=15.52, p <.001).
-
Conclusion
- The findings of this study indicated that periodic assessment of periodontal disease is essential for pregnant women who are in 2nd or 3rd trimester and have pregnancy induced diseases. Enhancing oral health care behaviors and reducing perceived stress are indicated as effective strategies to reduce periodontal disease in pregnant women.
This work was supported by a 2-Year Research Grant of Pusan National University.
The authors declared no conflict of interest.
- 1. Kushnir D, Zusman SP, Robinson PG. Validation of a Hebrew version of the oral health impact profile 14. J Public Health Dent. 2004;64(2):71–75.ArticlePubMed
- 2. Hong NP, Nam YY. All kinds of learning of oral cavity. Paju: Kidaribook; 2000.
- 3. Warren KR, Postolache TT, Groer ME, Pinjari O, Kelly DL, Reynolds MA. Role of chronic stress and depression in periodontal diseases. Periodontol 2000. 2014;64(1):127–138. ArticlePubMed
- 4. Silk H, Douglass AB, Douglass JM, Silk L. Oral health during pregnancy. Am Fam Physician. 2008;77(8):1139–1144.PubMed
- 5. Centers for Disease Control and Prevention. Periodontal disease [Internet]. Atlanta, GA, Author. 2013;cited 2014 October 25. Available from: http://www.cdc.gov/OralHealth/periodontal_disease/
- 6. Ha JE, Yeo BM, Roh HY, Paik DI, Bae KH. Periodontal condition and pathogens distribution of pregnant women. J Korean Acad Oral Health. 2010;34(4):587–594.
- 7. Giannella L, Giulini S, Cerami LB, La Marca A, Forabosco A, Volpe A. Periodontal disease and nitric oxide levels in low risk women with preterm labor. Eur J Obstet Gynecol Reprod Biol. 2011;158(1):47–51. ArticlePubMed
- 8. Vogt M, Sallum AW, Cecatti JG, Morais SS. Factors associated with the prevalence of periodontal disease in low-risk pregnant women. Reprod Health. 2012;9:3ArticlePubMedPMCPDF
- 9. Vogt M, Sallum AW, Cecatti JG, Morais SS. Periodontal disease and some adverse perinatal outcomes in a cohort of low risk pregnant women. Reprod Health. 2010;7:29ArticlePubMedPMCPDF
- 10. Piscoya MD, Ximenes RA, Silva GM, Jamelli SR, Coutinho SB. Periodontitis-associated risk factors in pregnant women. Clinics (Sao Paulo). 2012;67(1):27–33. ArticlePubMedPMC
- 11. Martinez-Beneyto Y, Vera-Delgado MV, Perez L, Maurandi A. Self-reported oral health and hygiene habits, dental decay, and periodontal condition among pregnant European women. Int J Gynaecol Obstet. 2011;114(1):18–22. ArticlePubMedPDF
- 12. Geisinger ML, Robinson M, Kaur M, Gerlach RW, Griffin R, Geurs NC, et al. Individualized oral health education improves oral hygiene compliance and clinical outcomes in pregnant women with gingivitis. J Oral Hyg Health. 2013;1(2):1000111
- 13. American Dental Association. Diet and dental health [Internet]. Chicago, IL, Author. 2015;cited 2015 April 24. Available from: http://www.mouthhealthy.org/en/az-topics/d/diet-and-dentalhealth
- 14. Saletu A, Pirker-Frühauf H, Saletu F, Linzmayer L, Anderer P, Matejka M. Controlled clinical and psychometric studies on the relation between periodontitis and depressive mood. J Clin Periodontol. 2005;32(12):1219–1225. ArticlePubMed
- 15. Rosania AE, Low KG, McCormick CM, Rosania DA. Stress, depression, cortisol, and periodontal disease. J Periodontol. 2009;80(2):260–266. ArticlePubMed
- 16. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. p. 1–400.
- 17. Kloetzel MK, Huebner CE, Milgrom P. Referrals for dental care during pregnancy. J Midwifery Womens Health. 2011;56(2):110–117. ArticlePubMedPMCPDF
- 18. American Dental Association. Brushing your teeth [Internet]. Chicago, IL, Author. 2015;cited 2015 April 24. Available from: http://www.mouthhealthy.org/en/az-topics/b/brushing-your-teeth
- 19. Moynihan PJ. Dietary advice in dental practice. Br Dent J. 2002;193(10):563–568. ArticlePubMedPDF
- 20. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
- 21. Chon KK, Rhee MK. Preliminary development of Korean version of CES-D. Korean J Clin Psychol. 1992;11(1):65–76.
- 22. Ahn HL. A pilot study of stressor and stress situation and nursing intervention of pregnant woman. J Nurs Acad Soc. 1983;13(3):75–85.ArticlePDF
- 23. Cohen S, Kamarck T, Mermelstein R. A global measures of perceived stress. J Health Soc Behav. 1983;24(4):385–396.PubMed
- 24. Lee J, Shin C, Ko YH, Lim JH, Joe SH, Hyun KS, et al. The reliability and validity studies of the Korean version of the perceived stress scale. Korean J Psychosom Med. 2012;20(2):127–134.
- 25. Kim BO, Shim HS, Lee CS, Chung SH, Han YK, Cho MS, et al. Periodontology. Seoul: DaehanNarae Publishing, Inc.; 2003.
- 26. World Health Organization. Oral health surveys: Basic methods. 4th ed. Geneva, CH: Author; 1997. p. 1–66.
- 27. Xiong X, Elkind-Hirsch KE, Vastardis S, Delarosa RL, Pridjian G, Buekens P. Periodontal disease is associated with gestational diabetes mellitus: A case-control study. J Periodontol. 2009;80(11):1742–1749. ArticlePubMedPMC
- 28. Park YN, Shim CS. A study on the awareness and practice of the pregnant women about oral health care. J Korean Acad Dent Hyg Educ. 2008;8(3):53–64.
- 29. Li D, Liu L, Odouli R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: A prospective cohort study. Hum Reprod. 2009;24(1):146–153. ArticlePubMed
- 30. Giurgescu C, Misra DP, Sealy-Jefferson S, Caldwell CH, Templin TN, Slaughter-Acey JC, et al. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. Soc Sci Med. 2015;130:172–180. ArticlePubMedPMC
- 31. Lee EJ, Park JS. Status of antepartum depression and its influencing factors in pregnant women. J Korea Acad Ind Coop Soc. 2013;14(8):3897–3906. Article
REFERENCES
Figure & Data
REFERENCES
Citations

- Oral Health, Anxiety, Depression, and Stress in Pregnancy: A Rapid Review of Associations and Implications for Perinatal Care
Abiola A. Adeniyi, Swathi Ramachandran, Cecilia Marie Jevitt
International Journal of Environmental Research and Public Health.2024; 22(1): 32. CrossRef - Effects of depression and stress on oral self‐care among perinatal women in Appalachia: A longitudinal study
Jeongwi An, Christa Lilly, John R. Shaffer, Betsy Foxman, Mary L. Marazita, Daniel W. McNeil
Community Dentistry and Oral Epidemiology.2024; 52(6): 871. CrossRef - Dental caries and depression in pregnant women: The role of oral health self‐perception as mediator
Mariana G. Cademartori, Flavio F. Demarco, Mariangela Freitas da Silveira, Fernando C. Barros, Marcos B. Corrêa
Oral Diseases.2022; 28(6): 1733. CrossRef - Comparison of Diagnosed Depression and Self-Reported Depression Symptom as a Risk Factor of Periodontitis: Analysis of 2016–2018 Korean National Health and Nutrition Examination Survey Data
Seon-Rye Kim, Seoul-Hee Nam
International Journal of Environmental Research and Public Health.2021; 18(3): 871. CrossRef - Factors Related to Maternal Oral Health Status: Focus on Pregnant and Breastfeeding Women
Eun Gyeong Kim, Sook Kyoung Park, Ju-Hee Nho
Healthcare.2021; 9(6): 708. CrossRef - Factors contributing to unmet needs for dental health care in adult population of Serbia
Milica Veličković, Snežana Radovanović, Vesna Dimitrijević, Danijela Gračić, Sanja Krulj, Jasna Milosavljević, Tanja Milićević, Ana Marinković, Tatjana Kanjevac
Zdravstvena zastita.2020; 49(1): 1. CrossRef - The Impact of Oral Health on Work Performance of Japanese Workers
Takashi Zaitsu, Tomoya Saito, Akiko Oshiro, Takeo Fujiwara, Yoko Kawaguchi
Journal of Occupational & Environmental Medicine.2020; 62(2): e59. CrossRef - Predictive Model of Clinical Attachment Loss and Oral Health-Related Quality of Life through Depressive Symptomatology, Oral Hygiene Habits, and Proinflammatory Biomarkers: A Pilot Study
Norma Idalia Rodríguez Franco, José Moral de la Rubia, Andrea Guadalupe Alcázar Pizaña
Dentistry Journal.2020; 8(1): 20. CrossRef - Stress, allostatic load, and periodontal diseases
Wael Sabbah, Noha Gomaa, Aswathikutty Gireesh
Periodontology 2000.2018; 78(1): 154. CrossRef - Comparison of Effects of Oral Health Program and Walking Exercise Program on Health Outcomes for Pregnant Women
Hae-jin Park, Haejung Lee
Journal of Korean Academy of Nursing.2018; 48(5): 506. CrossRef - Periodontal Disease and Health Related Quality of Life (HRQoL) in Pregnant Women
Hae-jin Park, Haejung Lee, Soohyun Cho
Korean Journal of Women Health Nursing.2016; 22(4): 191. CrossRef
Differences in Periodontal Disease according to Individual Characteristics (N=129)
Levels of Oral Health Behaviors, Psycho-Social Factors and Periodontal Disease (N=129)
CPI=Community Periodontal Index.
Correlations between Oral Health Care Behaviors, Psycho-Social Factors, and Periodontal Disease (N=129)
*Periodontal probing depth (mm).
Factors Influencing Periodontal Disease† (N=129)
*Dummy variables; †Periodontal probing depth (mm).
CPI=Community Periodontal Index.
*Periodontal probing depth (mm).
*Dummy variables; †Periodontal probing depth (mm).
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

