Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 46(5); 2016 > Article
-
Original Article
- A Prediction Model for Unmet Needs of Elders with Dementia and Caregiving Experiences of Family Caregivers
- Sora Choi, Myonghwa Park
-
Journal of Korean Academy of Nursing 2016;46(5):663-674.
DOI: https://doi.org/10.4040/jkan.2016.46.5.663
Published online: October 31, 2016
1Department of Nursing, Chungbuk Health & Science University, Cheongju, Korea.
2College of Nursing, Chungnam National University, Daejeon, Korea.
- Address reprint requests to : Park, Myonghwa. College of Nursing, Chungnam National University, 266 Munhwa-ro, Jung-gu, Daejeon 35015, Korea. Tel: +82-42-580-8328, Fax: +82-42-580-8309, mhpark@cnu.ac.kr
© 2016 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
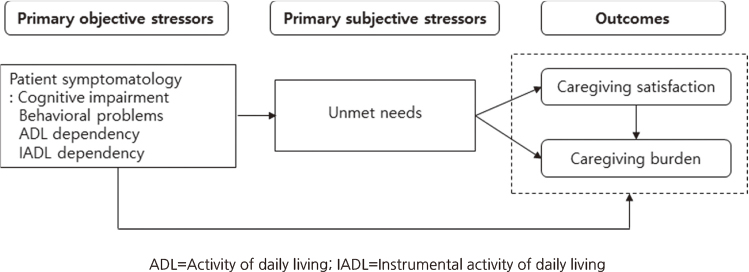
- The purposes of this study were to develop and test a prediction model for caregiving experiences including caregiving satisfaction and burden in dementia family caregivers.
-
Methods
- The stress process model and a two factor model were used as the conceptual frameworks. Secondary data analysis was done with 320 family caregivers who were selected from the Seoul Dementia Management Survey (2014) data set. In the hypothesis model, the exogenous variable was patient symptomatology which included cognitive impairment, behavioral problems, dependency in activity of daily living and in instrumental activity of daily living. Endogenous variables were caregiver's perception of dementia patient's unmet needs, caregiving satisfaction and caregiving burden. Data were analysed using SPSS/WINdows and AMOS program.
-
Results
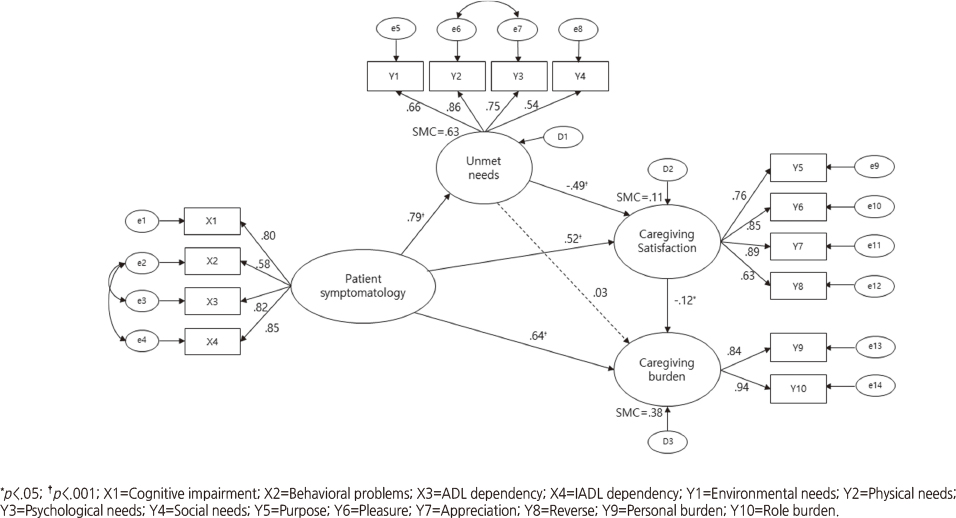
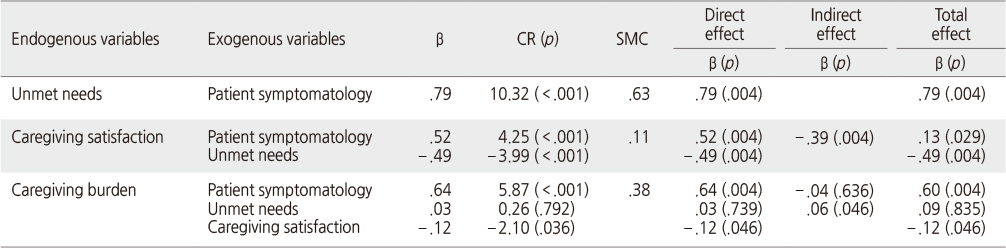
- Caregiving burden was explained by patient symptomatology and caregiving satisfaction indicating significant direct effects and significant indirect effect from unmet needs. The proposed model explained 37.8% of the variance. Caregiving satisfaction was explained by patient symptomatology and unmet needs. Mediating effect of unmet needs was significant in the relationship between patient symptomatology and caregiving satisfaction.
-
Conclusion
- Results indicate that interventions focusing on relieving caregiving burden and enhancing caregiver satisfaction should be provided to caregivers with high levels of dementia patients' unmet needs and low level of caregiving satisfaction.
This manuscript is a revision of the first author's doctoral dissertation from Chungnam National University.
This study was supported by Seoul Dementia Center and Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and future Planning (NRF. 2013R1A2A2A01069090).
The authors declared no conflict of interest
- 1. Ministry of Health & Welfare. National dementia strategy 2013- 2015 [Internet]. Seoul, Author. 2012;cited 2015 March 10. Available from: http://www.mw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=274723&page=1
- 2. Sung MR, Yi M, Lee DY, Jang HY. Overcoming experiences of family members caring for elderly patients with dementia at home. J Korean Acad Nurs. 2013;43(3):389–398. ArticlePubMed
- 3. Cho E, Cho E, Kim SS. Effects of family relationship on burden of family caregivers of older adult with dementia. J Korean Gerontol Soc. 2010;30(2):421–437.
- 4. Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol. 1991;46(4):P181–P189. ArticlePubMed
- 5. Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30(5):583–594.ArticlePubMed
- 6. Bass DM, Judge KS, Snow AL, Wilson NL, Looman WJ, McCarthy C, et al. Negative caregiving effects among caregivers of veterans with dementia. Am J Geriatr Psychiatry. 2012;20(3):239–247. ArticlePubMed
- 7. Orrell M, Hancock G. CANE: Camberwell assessment of need for the elderly. London, UK: Gaskell; 2004. p. 1–208.
- 8. Gaugler JE, Mittelman MS, Hepburn K, Newcomer R. Identifying at-risk dementia caregivers following institutionalization: The nursing home admission-burden and nursing home admission-depression prognostic tools. J Appl Gerontol. 2014;33(5):624–624. ArticlePubMedPDF
- 9. Lee YW, Lim JY, Kim JY, Cho HI, Ko GJ. A prediction model for caregiver burden and life satisfaction: Caring for a patient with dementia. J Korean Gerontol Nurs. 2011;13(3):204–214.
- 10. Contador I, Fernández-Calvo B, Palenzuela DL, Miguéis S, Ramos F. Prediction of burden in family caregivers of patients with dementia: A perspective of optimism based on generalized expectancies of control. Aging Ment Health. 2012;16(6):675–682.ArticlePubMed
- 11. de Labra C, Millán-Calenti JC, Buján A, Núñez-Naveira L, Jensen AM, Peersen MC, et al. Predictors of caregiving satisfaction in informal caregivers of people with dementia. Arch Gerontol Geriatr. 2015;60(3):380–388. ArticlePubMed
- 12. Hodge DR, Sun F. Positive feelings of caregiving among Latino Alzheimer's family caregivers: Understanding the role of spirituality. Aging Ment Health. 2012;16(6):689–698. ArticlePubMed
- 13. Hwang SS, Chang VT, Alejandro Y, Osenenko P, Davis C, Cogswell J, et al. Caregiver unmet needs, burden, and satisfaction in symptomatic advanced cancer patients at a Veterans Affairs(VA) medical center. Palliat Support Care. 2003;1(4):319–329. ArticlePubMed
- 14. Lim YM, Son GR, Song JA, Beattie E. Factors affecting burden of family caregivers of community-dwelling ambulatory elders with dementia in Korea. Arch Psychiatr Nurs. 2008;22(4):226–234. ArticlePubMed
- 15. Lee DY, Park M, Lee SJ, Kim YH, Kim JH, Kim HJ, et al. Dementia management survey for registered elders with dementia on the Seoul dementia management project. Seoul: Seoul Metropolitan Center for Dementia; 2014.
- 16. Yu JP. The concept and understanding of structural equation modelng. Seoul: Hannare Publishing Co; 2012. p. 1–567.
- 17. Reynolds T, Thornicroft G, Abas M, Woods B, Hoe J, Leese M, et al. Camberwell Assessment of Need for the Elderly(CANE). Development, validity and reliability. Br J Psychiatry. 2000;176:444–452. ArticlePubMed
- 18. Nolan M, Grant G, Keady J. Assessing the needs of family carers: A guide for practitioners. Brighton, UK: Pavilion Publishing; 1998. p. 1–39.
- 19. Andrén S, Elmståhl S. Family caregivers' subjective experiences of satisfaction in dementia care: Aspects of burden, subjective health and sense of coherence. Scand J Caring Sci. 2005;19(2):157–168. ArticlePubMed
- 20. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. ArticlePubMed
- 21. Bae KY, Shin IS, Kim SW, Kim JM, Yang SJ, Mun JU, et al. Care burden caregivers according to cognitive function of elderly persons. J Korean Soc Biol Ther Psychiatry. 2006;12(1):66–75.
- 22. Park M, Sung M, Kim SK, Kim S, Lee DY. Multidimensional determinants of family caregiver burden in Alzheimer's disease. Int Psychogeriatr. 2015;27(8):1355–1364. ArticlePubMed
- 23. Han EJ, Lee JM, Kwon JH, Shin SB, Lee JS. Factors related to family caregivers' burden with the community-dwelling disabled elderly under the long-term care insurance system. Health Policy Manag. 2014;24(1):71–84. Article
- 24. Holst G, Edberg AK. Wellbeing among people with dementia and their next of kin over a period of 3 years. Scand J Caring Sci. 2011;25(3):549–557. ArticlePubMed
- 25. Goetzinger AM. Predictors of caregiver well-being and satisfaction: The development of a comprehensive model [dissertation]. Kansas City, MO, University of Missouri-Kansas City. 2008;1–165.
- 26. National Collaborating Centre for Mental Health. Dementia: A NICE–SCIE guideline on supporting people with dementia and their carers in health and social care [Internet]. London, UK, The British Psychological Society, The Royal College of Psychiatrists. 2007;cited 2015 December 21. Available from: http://www.scie.org.uk/publications/misc/dementia/dementia-fullguideline.pdf
- 27. Bass DM, Judge KS, Snow AL, Wilson NL, Morgan R, Looman WJ, et al. Caregiver outcomes of partners in dementia care: Effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61(8):1377–1386. ArticlePubMedPDF
- 28. Kajiwara K, Nakatani H, Ono M, Miyakoshi Y. Positive appraisal of in-home family caregivers of dementia patients as an influence on the continuation of caregiving. Psychogeriatrics. 2015;15(1):26–31. ArticlePubMed
- 29. Park M, Park MH, Kim HH. Effects of a multimodal psychoeducational program on burden, depression, and problem coping behaviors in family caregivers of patients with dementia. J Korean Gerontol Nurs. 2015;17(1):10–19. Article
- 30. Shim B, Barroso J, Gilliss CL, Davis LL. Finding meaning in caring for a spouse with dementia. Appl Nurs Res. 2013;26(3):121–126. ArticlePubMed
REFERENCES
Figure & Data
REFERENCES
Citations

- Experiences of Family Caregivers Utilizing Care Support of Dementia Center
Chun-Gill Kim, Myung Soon Kwon, Young Hee Lee
Korean Journal of Adult Nursing.2018; 30(3): 314. CrossRef
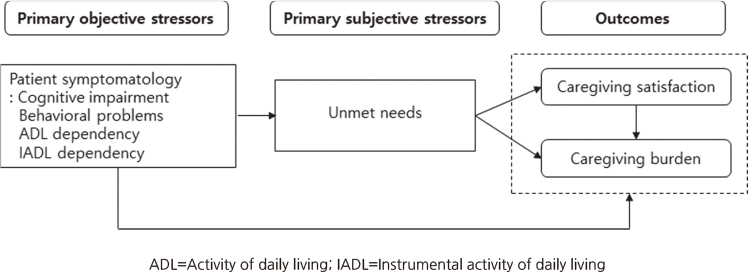
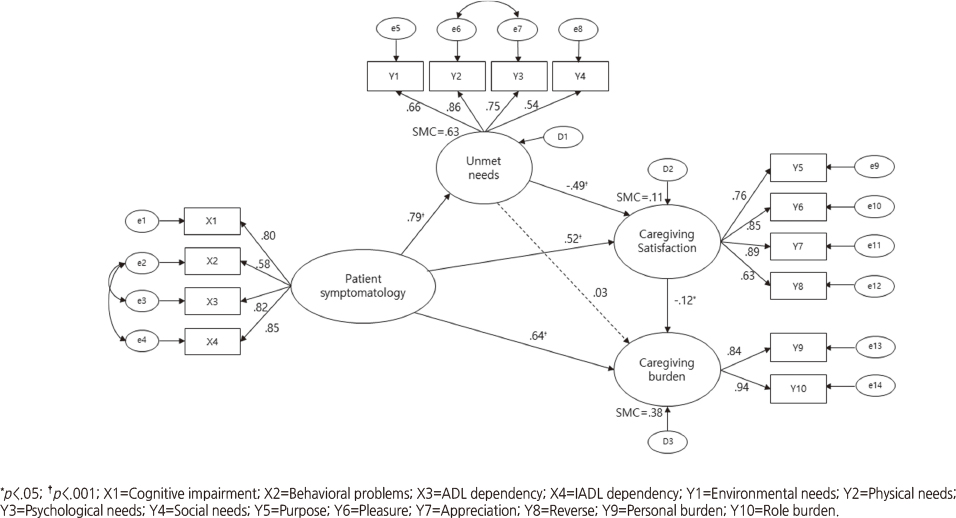
Figure 1
Figure 2
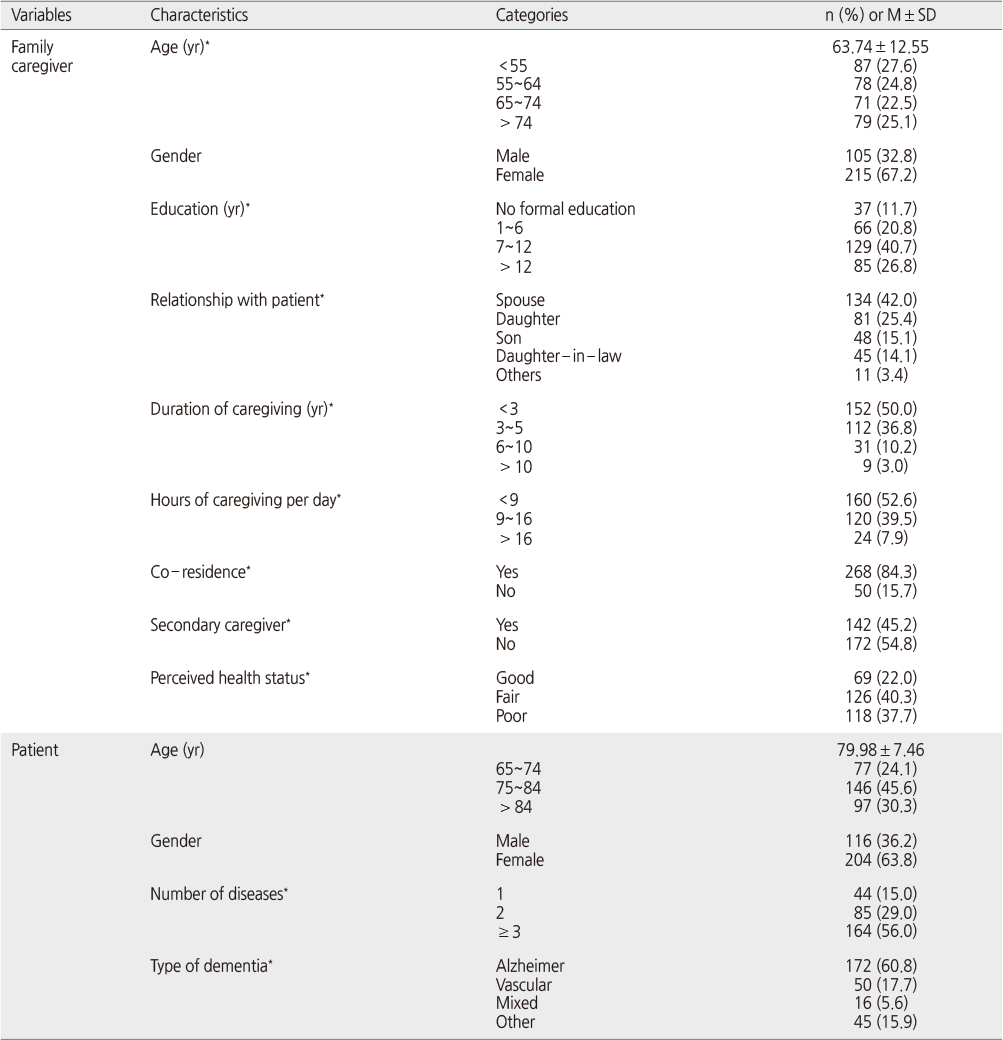
General and Care-related Characteristics of Patients and Family Caregivers (N=320)
*Missing data were excluded.
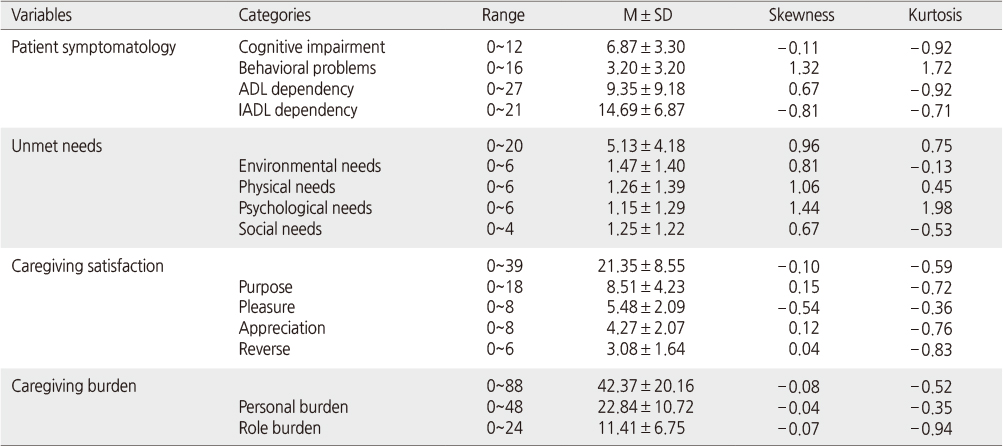
Descriptive Statistics of Observed Variables (N=320)
ADL=Activity of daily living; IADL=Instrumental activity of daily living.
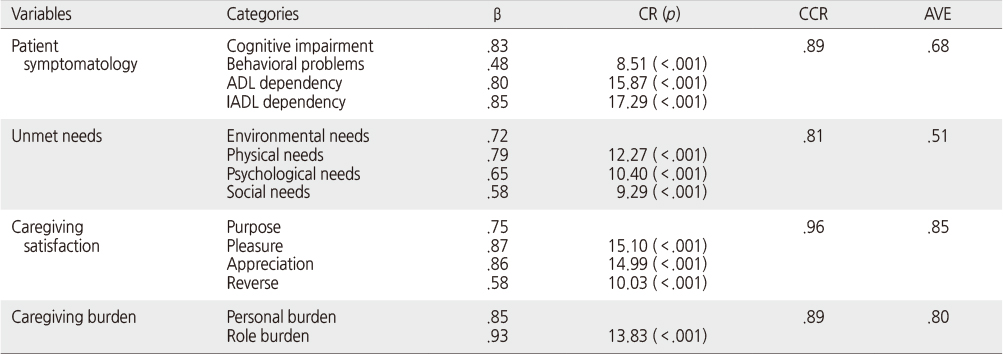
Factor Loading of Confirmatory Factor Analysis (N=320)
β=Standardized coefficients; CR=Critical ratio; CCR=Composite construct reliability; AVE=Average variance extracted; ADL=Activity of daily living; IADL=Instrumental activity of daily living.
Standardized Direct, Indirect, and Total Effects for the Final Model
β=Standardized coefficients; CR=Critical ratio; SMC=Squared multiple correlation
*Missing data were excluded.
ADL=Activity of daily living; IADL=Instrumental activity of daily living.
β=Standardized coefficients; CR=Critical ratio; CCR=Composite construct reliability; AVE=Average variance extracted; ADL=Activity of daily living; IADL=Instrumental activity of daily living.
β=Standardized coefficients; CR=Critical ratio; SMC=Squared multiple correlation
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

