Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 44(3); 2014 > Article
-
Original Article
- Development and Evaluation of an Enteral Nutrition Protocol for Dysphagia in Patients with Acute Stroke
- Sung-Hee Yoo, So-Sun Kim
-
Journal of Korean Academy of Nursing 2014;44(3):280-293.
DOI: https://doi.org/10.4040/jkan.2014.44.3.280
Published online: June 30, 2014
1College of Nursing, Chonnam National University, Gwangju, Korea.
2College of Nursing, Yonsei University, Seoul, Korea.
- Address reprint requests to: Yoo, Sung-Hee. College of Nursing, Chonnam National University, 160 Baekseo-ro, Dong-gu, Gwangju 501-746, Korea. Tel: +82-62-530-4941, Fax: +82-62-220-4544, shyoo@jnu.ac.kr
© 2014 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- The study was done to develop an evidence-based enteral nutrition (EN) protocol for effective nutritional support for dysphagia in patients with acute stroke, and to evaluate effects of this protocol on clinical outcomes.
-
Methods
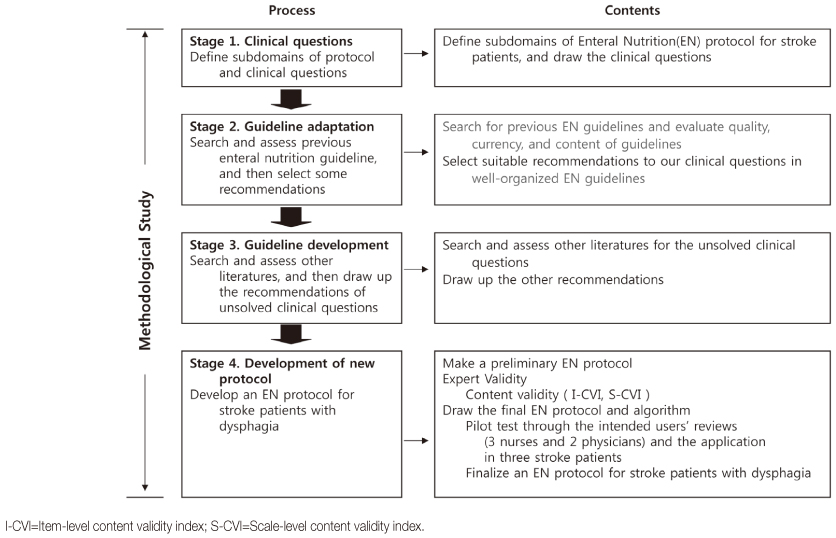
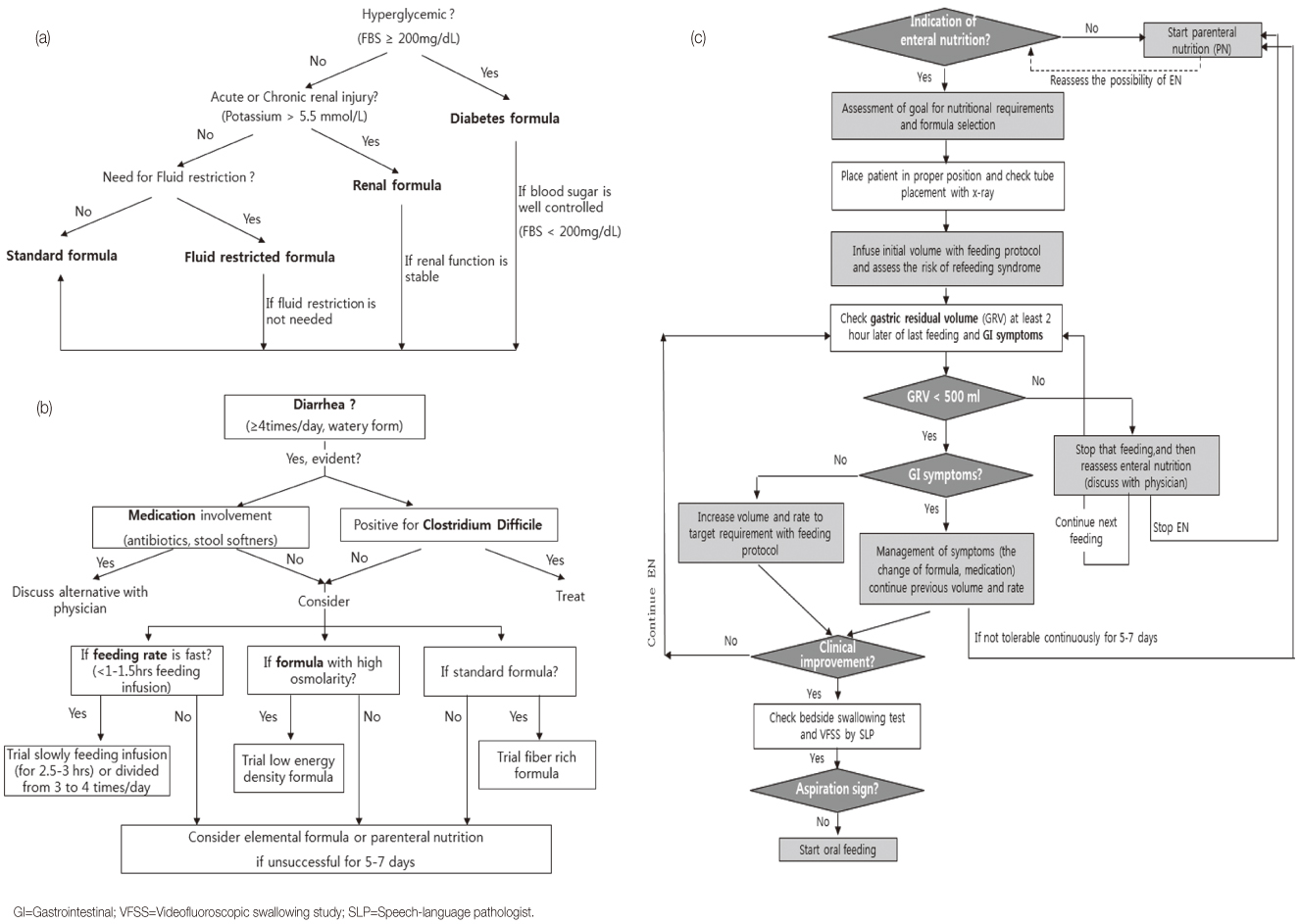
- A methodological study was used to develop the EN protocol and a quasi-experimental study to verify the effectiveness of the protocol. The preliminary EN protocol was drawn by selecting recommendations from previous well-designed EN guidelines, and then developing additional recommendations based on high-quality evidence. Content validation was assessed by an expert group, and clinical applicability by care providers and patients. The scale-level content validity index of the final EN protocol was 0.99. Assessment was done of differences in percentage of caloric goals achieved and presence of undernutrition, aspiration pneumonia, and gastrointestinal (GI) complications after application of the EN protocol.
-
Results
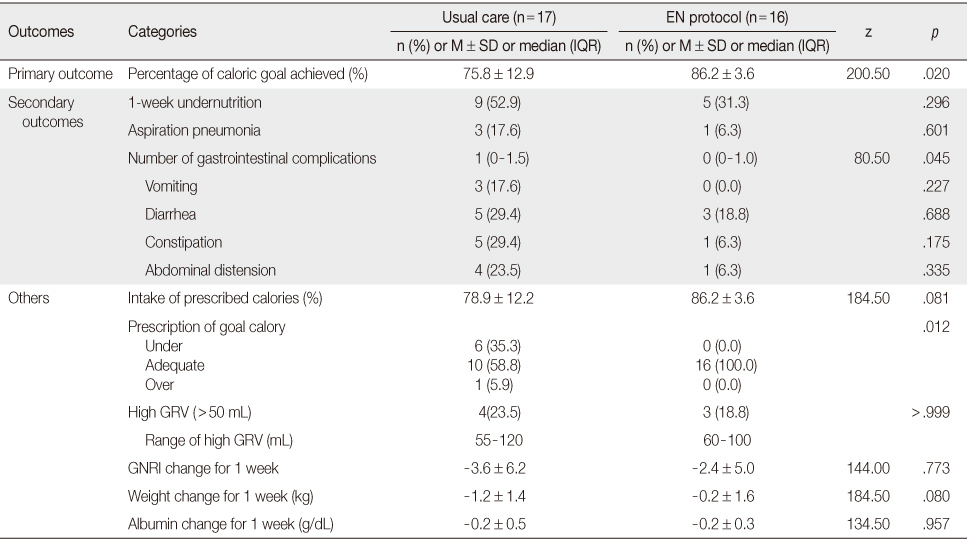
- In the EN protocol group, the percentage of caloric goals achieved (R2=.24, p=.001) and the reduction of GI complications (p=.045) were significantly improved, but the presence of undernutrition (p=.296) and aspiration pneumonia (p=.601) did not differ from the usual care group.
-
Conclusion
- Results indicate that the new EN protocol for dysphagia in patients with acute stroke significantly increased their nutritional intake and reduced GI complications.
This manuscript is based on a part of the first author's doctoral dissertation from Yonsei University
- 1. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: Prognosis and prognostic factors at 6 months. Stroke. 1999;30(4):744–748.ArticlePubMed
- 2. Foley NC, Martin RE, Salter KL, Teasell RW. A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med. 2009;41(9):707–713. http://dx.doi.org/10.2340/16501977-0415ArticlePubMed
- 3. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–2763. http://dx.doi.org/10.1161/01.STR.0000190056.76543.ebArticlePubMed
- 4. Davis JP, Wong AA, Schluter PJ, Henderson RD, O'Sullivan JD, Read SJ. Impact of premorbid undernutrition on outcome in stroke patients. Stroke. 2004;35(8):1930–1934. http://dx.doi.org/10.1161/01.STR.0000135227.10451.c9ArticlePubMed
- 5. Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65(1):39–43. http://dx.doi.org/10.1001/archneurol.2007.12ArticlePubMed
- 6. Pugh S, Mathiesen C, Meighan M, Summers D, Zrelak P. Guide to the care of the hospitalized patient with ischemic stroke. 2nd ed. Glenview, IL: American Association of Neuroscience Nurses; 2008.
- 7. Btaiche IF, Chan LN, Pleva M, Kraft MD. Critical illness, gastrointestinal complications, and medication therapy during enteral feeding in critically ill adult patients. Nutr Clin Pract. 2010;25(1):32–49. http://dx.doi.org/10.1177/0884533609357565ArticlePubMedPDF
- 8. Pinilla JC, Samphire J, Arnold C, Liu L, Thiessen B. Comparison of gastrointestinal tolerance to two enteral feeding protocols in critically ill patients: A prospective, randomized controlled trial. JPEN J Parenter Enteral Nutr. 2001;25(2):81–86. http://dx.doi.org/10.1177/014860710102500281PubMed
- 9. Moon SS, Lim H, Choi JW, Kim DK, Lee JW, Ko S, et al. Analysis of nutritional support status in the intensive care unit. Korean J Crit Care Med. 2009;24(3):129–133. http://dx.doi.org/10.4266/kjccm.2009.24.3.129Article
- 10. Chung HK, Lee SM, Lee JH, Shin CS. Energy deficiency aggravates clinical outcomes of critically ill patients. Korean J Crit Care Med. 2005;20(1):49–53.
- 11. Ros C, McNeill L, Bennett P. Review: Nurses can improve patient nutrition in intensive care. J Clin Nurs. 2009;18(17):2406–2415. http://dx.doi.org/10.1111/j.1365-2702.2008.02765.xArticlePubMed
- 12. Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P, Krenitsky J, et al. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33(2):122–167. http://dx.doi.org/10.1177/0148607108330314PubMed
- 13. Stroud M, Duncan H, Nightingale J. Guidelines for enteral feeding in adult hospital patients. Gut. 2003;52:Suppl 7. vii1–vii12.ArticlePubMedPMC
- 14. Park M. Understanding and application of evidence based nursing. Seoul: Koonja; 2006.
- 15. Barr J, Hecht M, Flavin KE, Khorana A, Gould MK. Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest. 2004;125(4):1446–1457.ArticlePubMed
- 16. Heyland DK, Dhaliwal R, Day A, Jain M, Drover J. Validation of the Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients: Results of a prospective observational study. Crit Care Med. 2004;32(11):2260–2266.ArticlePubMed
- 17. Moon JR, Cho YA, Min SI, Yang JH, Huh J, Jung YY. Development and application of a feeding program for infants postoperatively following cardiac surgery. J Korean Acad Nurs. 2009;39(4):508–517. http://dx.doi.org/10.4040/jkan.2009.39.4.508ArticlePubMed
- 18. Braudis NJ, Curley MA, Beaupre K, Thomas KC, Hardiman G, Laussen P, et al. Enteral feeding algorithm for infants with hypoplastic left heart syndrome poststage I palliation. Pediatr Crit Care Med. 2009;10(4):460–466. http://dx.doi.org/10.1097/PCC.0b013e318198b167ArticlePubMed
- 19. Kenny DJ, Goodman P. Care of the patient with enteral tube feeding: An evidence-based practice protocol. Nurs Res. 2010;59:1 Suppl. S22–S31. http://dx.doi.org/10.1097/NNR.0b013e3181c3bfe9PubMed
- 20. McClave SA, Martindale RG, Vanek VW, McCarthy M, Roberts P, Taylor B, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of critical care medicine (SCCM) and American society for parenteral and enteral nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2009;33(3):277–316. http://dx.doi.org/10.1177/0148607109335234PubMed
- 21. Marik PE, Zaloga GP. Gastric versus post-pyloric feeding: A systematic review. Crit Care. 2003;7(3):R46–R51. http://dx.doi.org/10.1186/cc2190ArticlePubMedPMCPDF
- 22. Reeves MM, Capra S. Predicting energy requirements in the clinical setting: Are current methods evidence based? Nutr Rev. 2003;61(4):143–151.ArticlePubMed
- 23. Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric nutritional risk index: A new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–783.ArticlePubMed
- 24. Isselbacher KJ, Braunwald E, Wilson JD, Martin JB, Fauci AS, Kasper D. Harrison's principles of internal medicine. 13th ed. New York, NY: McGraw-Hill, Inc; 1994.
- 25. Heyland DK, Cahill NE, Dhaliwal R, Sun X, Day AG, McClave SA. Impact of enteral feeding protocols on enteral nutrition delivery: Results of a multicenter observational study. JPEN J Parenter Enteral Nutr. 2010;34(6):675–684. http://dx.doi.org/10.1177/0148607110364843PubMed
- 26. Cereda E. Evaluation of the risk factors for short-term mortality after acute ischemic stroke in the elderly: Is there a role for nutritional risk assessment? Gerontology. 2007;53(2):61–62. http://dx.doi.org/10.1159/000096084ArticlePubMedPDF
- 27. Montejo JC, Minambres E, Bordeje L, Mesejo A, Acosta J, Heras A, et al. Gastric residual volume during enteral nutrition in ICU patients: The REGANE study. Intensive Care Med. 2010;36(8):1386–1393. http://dx.doi.org/10.1007/s00134-010-1856-yArticlePubMedPDF
- 28. Poulard F, Dimet J, Martin-Lefevre L, Bontemps F, Fiancette M, Clementi E, et al. Impact of not measuring residual gastric volume in mechanically ventilated patients receiving early enteral feeding: A prospective before-after study. JPEN J Parenter Enteral Nutr. 2010;34(2):125–130. http://dx.doi.org/10.1177/0148607109344745PubMed
- 29. Jones NE, Suurdt J, Ouelette-Kuntz H, Heyland DK. Implementation of the Canadian clinical practice guidelines for nutrition support: A multiple case study of barriers and enablers. Nutr Clin Pract. 2007;22(4):449–457.ArticlePubMedPDF
REFERENCES
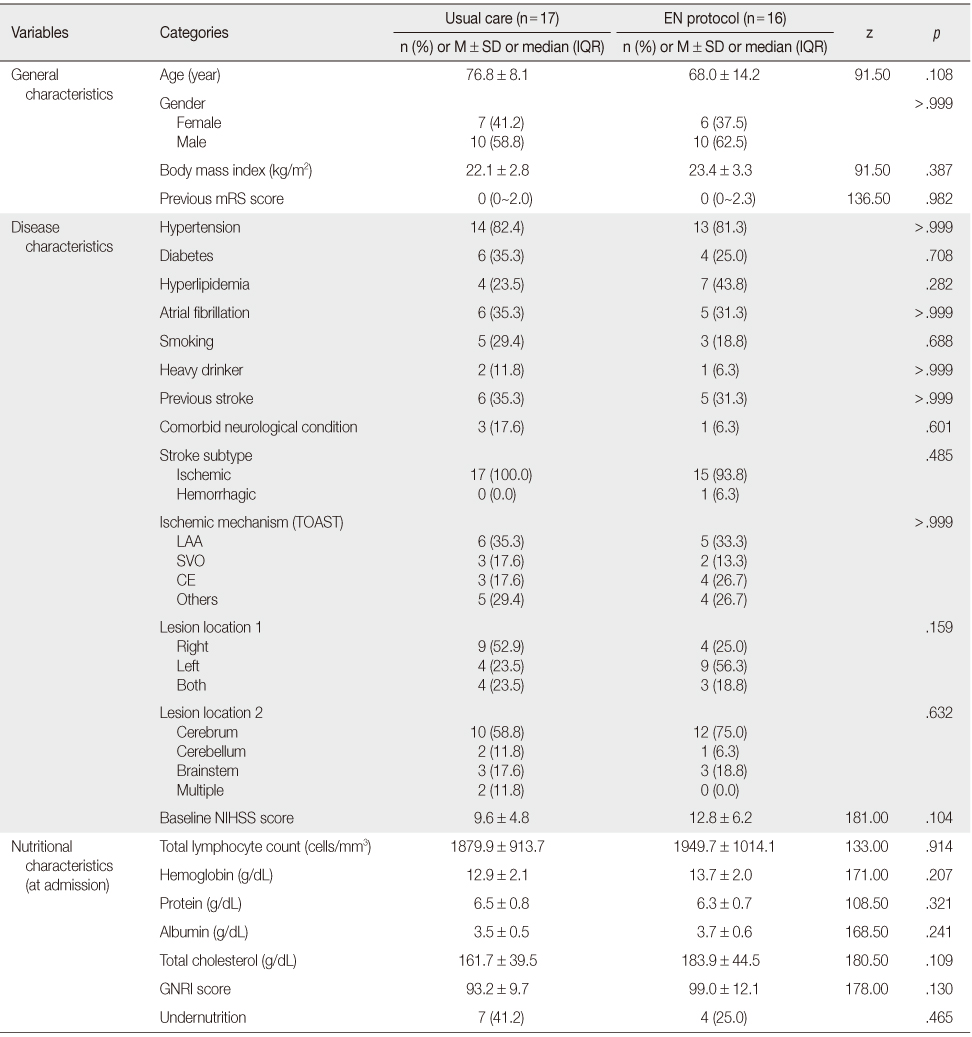
p values were calculated using Fisher's exact test or Mann-Whitney U test, where appropriate; EN=Enteral nutrition; IQR=Interquartile range; mRS=modified Rankin Scale; TOAST=the Trial of ORG 10172 in Acute Stroke Treatment; LAA=Large artery atherosclerosis; SVO=Small vessel occlusion; CE=Cardiac embolism; NIHSS=National Institutes of Health stroke scale; GNRI=Geriatric nutritional risk index.
Figure & Data
REFERENCES
Citations

- Nursing Algorithm for Stroke Patients with Sensory Disorder
Yoonjeong Lee, Jia Lee
Korean Journal of Adult Nursing.2018; 30(3): 301. CrossRef - Adaptation and Evaluation of the Incontinence Care Protocol
Kyung Hee Park, Heejung Choi
Journal of Korean Academy of Nursing.2015; 45(3): 357. CrossRef - Effects of a Dysphagia Nursing Protocol on Reducing Aspiration Pneumonia and Improving Daily Activity Dependency in Patients with Acute Stroke
Jung-Hee Han, Gee-Eun Lee, Joo-Hyun Jun, Yoo-Jin Lim, Eun-Jin Yoon, Yeo-Ok Kim
Korean Journal of Adult Nursing.2015; 27(3): 304. CrossRef
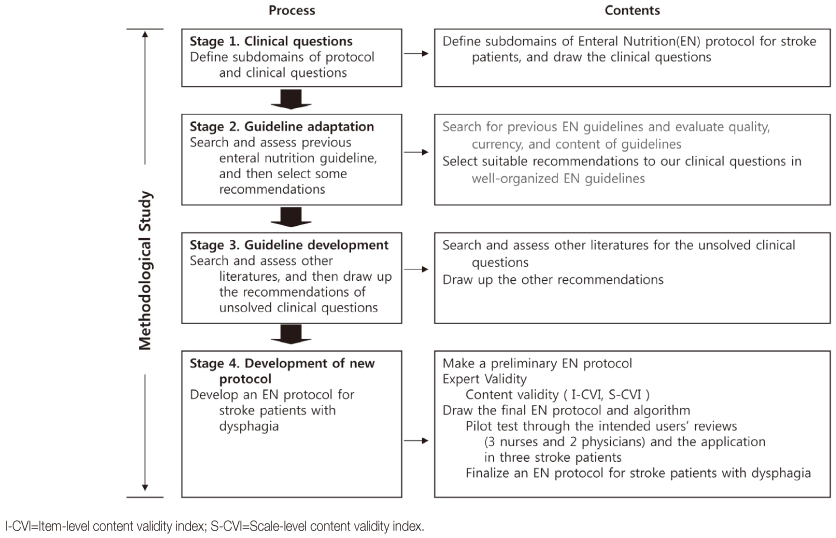
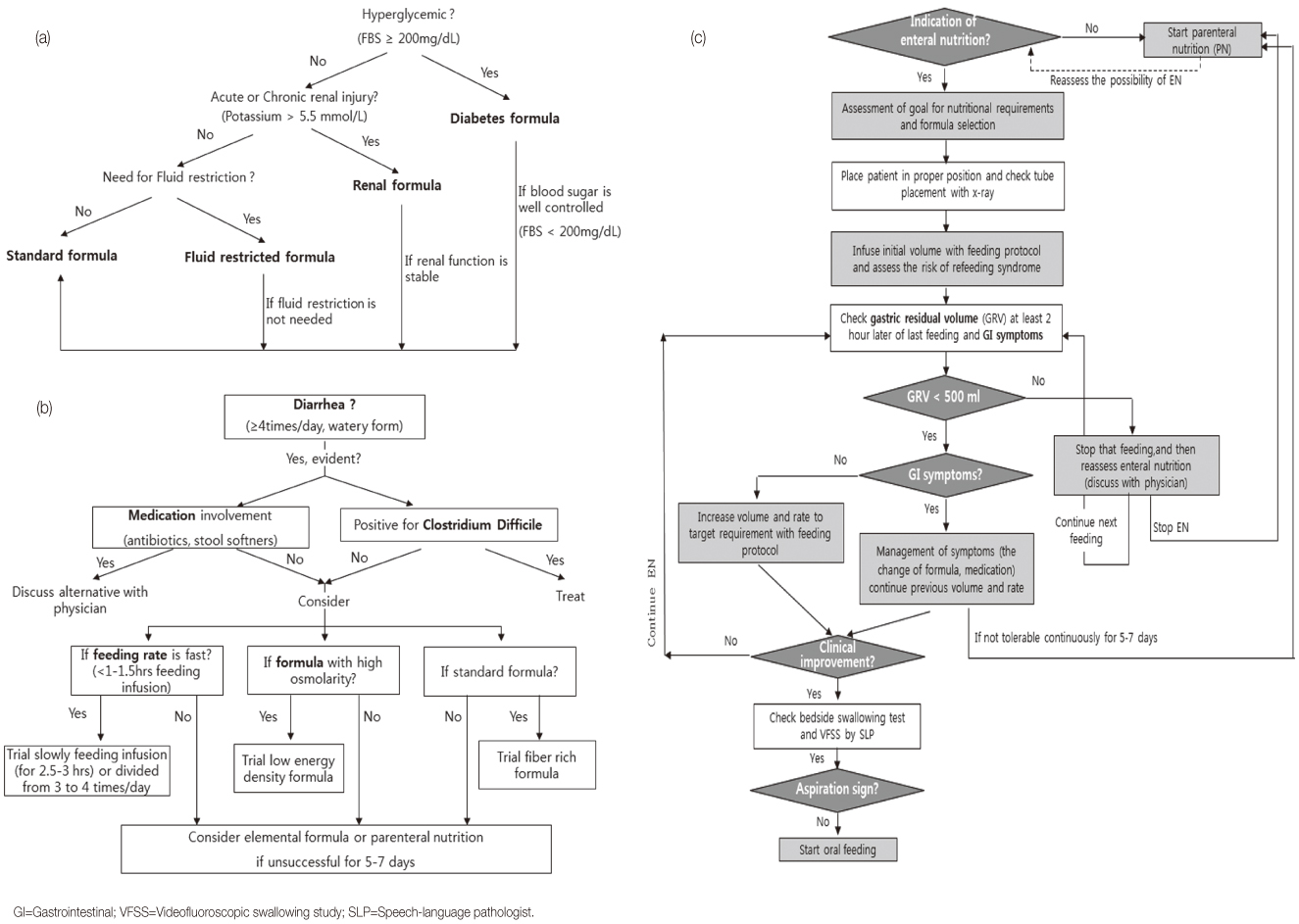
Figure 1
Figure 2
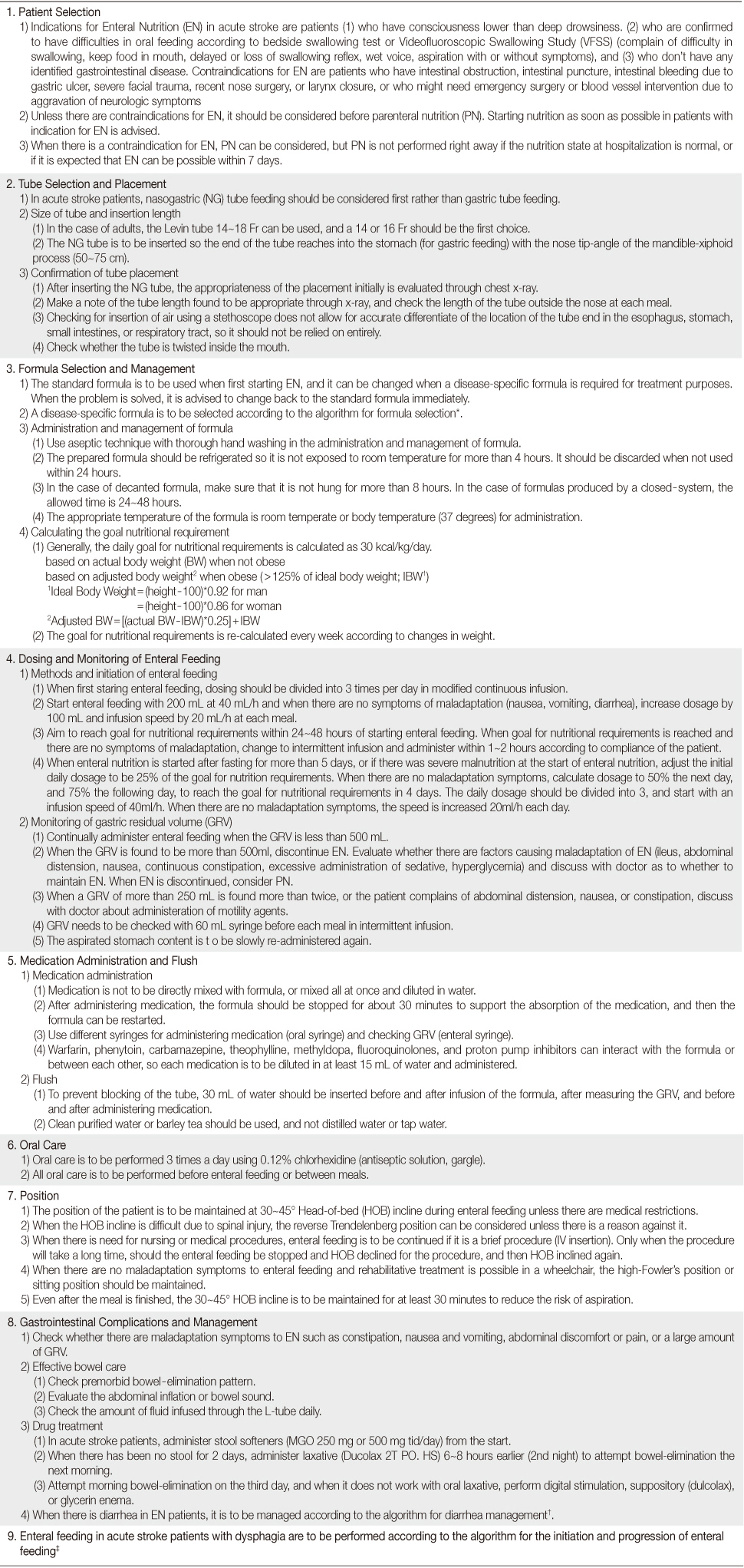
Final Enteral Nutrition Protocol
*The algorithm for formula selection (
General, Disease, and Nutritional Characteristics (N=33)
p values were calculated using Fisher's exact test or Mann-Whitney U test, where appropriate; EN=Enteral nutrition; IQR=Interquartile range; mRS=modified Rankin Scale; TOAST=the Trial of ORG 10172 in Acute Stroke Treatment; LAA=Large artery atherosclerosis; SVO=Small vessel occlusion; CE=Cardiac embolism; NIHSS=National Institutes of Health stroke scale; GNRI=Geriatric nutritional risk index.
Clinical Outcomes between Usual Care Group and EN Protocol Group (N=33)
p values were calculated using Fisher's exact test or Mann-Whitney U test, where appropriate; EN=Enteral nutrition; IQR=Interquartile range; GRV=Gastric residual volume; GNRI=Geriatric nutritional risk index.
*The algorithm for formula selection (
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

