Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 50(2); 2020 > Article
- Original Article Scale Development and Model Validation for the Process of Exercise Engagement for People with Prediabetes
- Shu-Chuan Chang, Hsiu-Chen Yeh, Yu-Lun Kuo
-
Journal of Korean Academy of Nursing 2020;50(2):298-312.
DOI: https://doi.org/10.4040/jkan.2020.50.2.298
Published online: April 30, 2020
2Department of Nursing, Tzu Chi University, Hualien, Taiwan
3Department of Nursing, Buddhist Tzu Chi General Hospital, Hualien, Taiwan
4Department of Nursing, Tzu Chi University of Science and Technology, Hualien, Taiwan
Abstract
Purpose
This study had two objectives: 1) to develop a scale for the process of exercise engagement (SPEE) for prediabetic individuals (PDIs); 2) to validate a structural model for the process of exercise engagement for PDIs.
Methods
A cross-sectional survey with simple random sampling was conducted from September 2013 to December 2015 (in Taiwan). A total of 310 PDIs were enrolled for scale development and model validation via item analysis, factor analyses, and structural equation modeling. The Kuo model was used as the basis for developing the Chinese version of the SPEE for PDIs.
Results
The SPEE contains five subscales with a total of twenty-one items that account for 54.9% to 65.9% of the total variance explained for assessing participants’ process of engagement during exercise. For Kuo model validation, the model measures indicated goodness of fit between the Kuo model and sample data. Analysis further revealed a direct effect between the creating health blueprints (CHB) stage and the spontaneous regular exercise (SRE) stage (b=.60).
Conclusion
The SPEE includes five subscales for assessing the psychological transition and behavioral expression at each stage of the process of exercise engagement for PDIs. The SPEE for people with prediabetes provides deeper insights into the factors of behavioral change stages that are required to initiate long-term health care outcomes and avoid developing diabetes. These insights are significant as they allow for patient- specific mapping and behavior modification to effect exercise.
Published online Apr 28, 2020.
https://doi.org/10.4040/jkan.2020.50.2.298
Scale Development and Model Validation for the Process of Exercise Engagement for People with Prediabetes
Abstract
Purpose
This study had two objectives: 1) to develop a scale for the process of exercise engagement (SPEE) for prediabetic individuals (PDIs); 2) to validate a structural model for the process of exercise engagement for PDIs.
Methods
A cross-sectional survey with simple random sampling was conducted from September 2013 to December 2015 (in Taiwan). A total of 310 PDIs were enrolled for scale development and model validation via item analysis, factor analyses, and structural equation modeling. The Kuo model was used as the basis for developing the Chinese version of the SPEE for PDIs.
Results
The SPEE contains five subscales with a total of twenty-one items that account for 54.9% to 65.9% of the total variance explained for assessing participants' process of engagement during exercise. For Kuo model validation, the model measures indicated goodness of fit between the Kuo model and sample data. Analysis further revealed a direct effect between the creating health blueprints (CHB) stage and the spontaneous regular exercise (SRE) stage (β=.60).
Conclusion
The SPEE includes five subscales for assessing the psychological transition and behavioral expression at each stage of the process of exercise engagement for PDIs. The SPEE for people with prediabetes provides deeper insights into the factors of behavioral change stages that are required to initiate long-term health care outcomes and avoid developing diabetes. These insights are significant as they allow for patient-specific mapping and behavior modification to effect exercise.
INTRODUCTION
The global population with prediabetes is increasing annually. The International Diabetes Federation has stated that 318 million people worldwide were estimated to have prediabetes in 2015, and this number is expected to reach 482 million by 2040 [1]. Prediabetes is a condition in which an individual's blood glucose exceeds the normal range, but he or she has not been diagnosed with diabetes. The criteria for a prediabetes diagnosis are fasting blood glucose levels between 100 and 125 mg/dl (known as impaired fasting glucose), 2-h postprandial plasma glucose between 140 and 199 mg/dl (known as impaired glucose tolerance), or hemoglobin A1c (HbA1c) between 5.7% and 6.5% [1]. Prediabetes is associated with a high risk of developing diabetes. If no active preventive approach is adopted during the prediabetic stage, prediabetes usually progresses to type 2 diabetes within an average of 3.6 years [2]. In one study, it was shown that annually in Taiwan, 3.2% of prediabetic individuals (PDIs) develop type 2 diabetes [3]. Prediabetes is also associated with increased risk of cardiovascular disease (14.8%), early stage nephropathy (17.7%), and retinopathy (7.9%) [4, 5, 6, 7]. Diabetes has a negative impact on patients and requires complicated, lifelong medical care. Diabetes not only impacts the patients but also their families and their associations within society.
For PDIs, lifestyle modification is the easiest way to prevent or delay the onset of diabetes. Studies have shown that healthy eating habits, regular exercise, and weight control lower the incidence of developing diabetes among prediabetics [8, 9, 10, 11]. Specifically, engaging in regular exercise is the most effective intervention for preventing diabetes. One study showed that while adopting a healthy diet can reduce diabetes incidence by 31.0%, regular exercise further reduces the incidence by 46.0% [12]. Another study indicated that PDIs engaging in regular exercise can reduce the risk of developing diabetes by between 30.0 and 69.0% compared to those who do not exercise [9, 10, 12]. Therefore, increasing physical activity among individuals with prediabetes should be prioritized to prevent the onset of diabetes.
Physical activity is associated with significant reductions in fasting glucose and HbA1c [13]. Physical activity is noted for: 1) reduced blood pressure, 2) reduced overall body fat, 3) reduced low-density lipoprotein cholesterol, 4) increased insulin sensitivity, 5) improved muscle strength, and 6) increased high-density lipoprotein cholesterol [14, 15]. Unfortunately, exercise is suboptimal among individuals with prediabetes in Taiwan for cultural reasons. Fewer than one-third of PDIs exercise routinely, and most of those who exercise do not do so for 150 minutes per week, which is the goal for effective diabetes prevention [16]. Furthermore, most of those who begin exercising after they recognize the importance of physical activity maintain their exercise routines for no more than six weeks [17]. Therefore, it is a major challenge for individuals with prediabetes to maintain consistent, lifelong exercise habits.
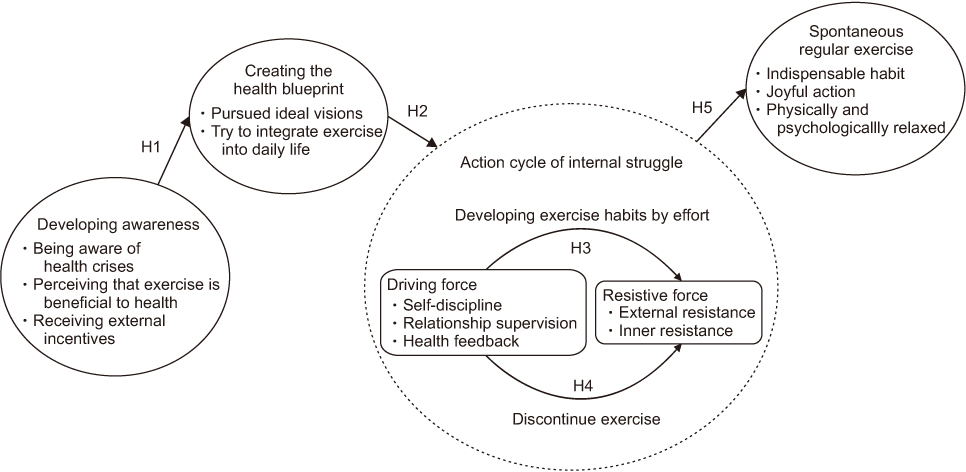
Based on previous qualitative research using grounded theory, the psychological status of PDIs' willingness to engage in exercise was modeled [18]. The Kuo model contains four stages: 1) developing awareness (DA) stage, 2) creating the health blueprint (CHB) stage, 3) action cycle of internal struggle (ACIS) stage, and 4) spontaneous regular exercise (SRE) stage. Furthermore, the ACIS stage contains two opposing forces: driving force (DF) and resistive force (RF) (Figure 1). Correctly assessing these two conflicting forces is critical for determining whether PDIs will enter the SRE stage.
According to the Kuo model, the DA stage is the key point in time at which PDIs may be strongly influenced to begin exercising. After progressing through the DA stage, PDIs enter the CHB stage and focus on self-determination with regard to their exercise goals. However, in the process, all such individuals must progress through the ACIS stage. When the self-discipline, relationship supervision, and health feedback of the DF are more powerful than the RF, the exercise behavior is maintained. In contrast, if the internal and external resistance of the RF are stronger than the DF, exercise behavior is interrupted. The RF and DF work against each other until the individual breaks the action cycle to enter the SRE stage. In this model, the stages of PDIs' exercise-engagement process are closely interlinked and interrelated.
The objective of the present study was to develop a scale and validate the model for the process of exercise engagement in PDIs from a quantitative perspective, as seen in Figure 1 [18]. Currently, several exercise behavior assessment scales such as the Exercise Self-Efficacy Scale (ESES) [19], the Sport Motivation Scale (SMS) [20], and the Trans-theoretical Model (TTM) [21] are available. Using the mentioned scales and theories to validate the model of the process of exercise engagement for PDIs has several constraints: 1) none of these theories or scales conduct investigations from the PDIs' perspective; 2) none of the scales cover the complete exercise-engagement process; and 3) none of the scales evaluate PDIs' psychological or emotional status at each stage of the exercise-engagement process.
The TTM and the Kuo model are fundamentally similar, while differences remain to be understood within the context of the disease as the region of interest and control from the perspective of the PDI. Behavioral modification from the individual's perspective to benefit from making specific changes is similar but slightly different between the TTM and the Kuo model. The Kuo model is specific for understanding and developing a predictive methodology to assess PDIs and their capacity to alter long-term health outcomes. Presently, scales that are suitable for investigating PDIs' exercise-engagement process remain lacking. To effectively resolve this shortcoming, this study developed a scale consisting of five subscales based on the five subcategories of the Kuo model (Figure 1). The scale was subsequently used to collect responses from PDIs to evaluate the interrelationships between DA, CHB, DF, RF, and SRE based on the following hypotheses:
Hypothesis 1 (H1): A relationship exists between DA and CHB, where DA will have a positive effect on CHB.
Hypothesis 2 (H2): A relationship exists between CHB and DF, where CHB will have a positive effect on DF.
Hypothesis 3 (H3) and Hypothesis 4 (H4): An inner conflict-based relationship exists between DF and RF, where the magnitudes of DF and RF may positively or negatively affect each other.
Hypothesis 5 (H5): A direct relationship exists between ACIS and SRE.
This study had two objectives: 1) to develop a scale for assessing the process of exercise engagement (SPEE) for PDIs, and 2) to validate the Kuo model for the process of exercise engagement for PDIs.
METHODS
1. Design and participants
A cross-sectional correlational survey with simple random sampling was conducted to validate the measurement scales and structural model. The participants were selected from a list of health checkups at a medical center in Hualien County in eastern Taiwan. The inclusion criteria consisted of: 1) elevated fasting blood glucose levels between 100 and 125 mg/dl, and 2) over 18 years of age. Exclusion criteria included: 1) previous diagnosis of type 1 or type 2 diabetes, 2) history of psychological illness, and 3) other serious illnesses (such as disability after stroke, liver disease, kidney disease, or cancer).
The study sample size was determined according to the following two criteria: (1) Stevens [22] suggested that five subjects should be allocated for each item of scale. (2) Gorsuch [23] and Thompson [24] suggested that at least 100 and 200 subjects are required for exploratory factor analysis (EFA) and structural equation modeling (SEM), respectively. As the initial version of the SPEE included forty-seven items (Appendix 1), a total of 235 (5×47=235) subjects were required according to Criterion 1. In order to fulfill Criterion 2 (100 subjects for EFA and 200 subjects for SEM) simultaneously, a total of 300 subjects were required. A simple random sampling technique was employed for randomly selecting PDIs from the list of health checkups over the previous three years. Based on an estimated participation rate of 65%, 465 PDIs were randomly selected for invitation to engage in the study. A total of 310 participants were recruited for the study where (n=110) for EFA and (n=200) for SEM analysis. The study was conducted from September 2013 to December 2015.
2. Data collection
After the research approval was granted by the institutional review board, the research institution made available a list of people with fasting blood glucose levels between 100 and 125 mg/dl as measured in health examinations over the past three years. Those who did not meet the inclusion criteria or whose phone number and address on the list were incorrect were eliminated from consideration, and subsequently, sampled randomly an estimated number of eligible individuals. A fasting blood glucose tracking notification was mailed to 450 eligible people, and 310 chose to participate (final participation rate of 68.9%). Potential participants were contacted via telephone and home visit and were sent multiple notifications inviting them to join this study. Participants were invited to the hospital for free blood glucose testing and a diabetes prevention health education seminar. In some instances, the researcher provided health education on an individual basis at the participants' homes. Participant recruitment continued until the required sample size was obtained.
3. Measures and variables
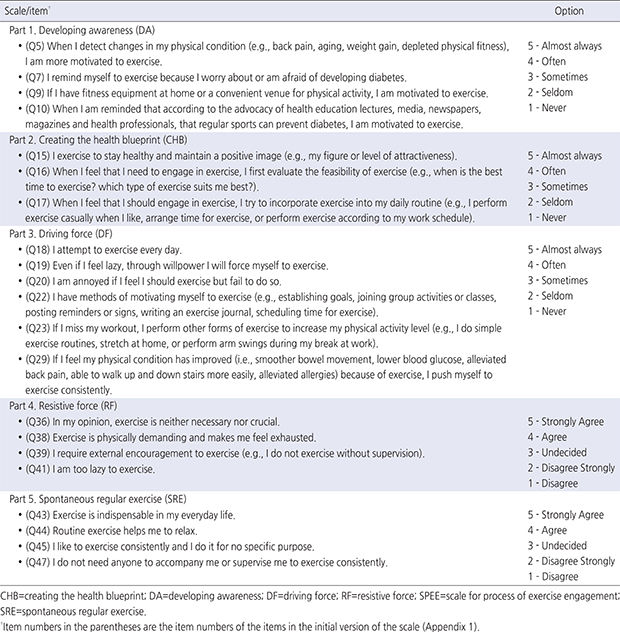
The Chinese version of the SPEE developed for use in this study is based on the Kuo model for the process of exercise engagement in PDIs in Taiwan (Figure 1) [18]. The scale includes five subscales for quantifying the PDIs' statuses in each of the five stages during the process. The subscales include: 1) the DA stage, 2) CHB stage, 3) DF stage, 4) RF stage, and 5) SRE stage. The scale's content validity was assessed by five experts to ensure its appropriateness. The resulting content validity index [25] of the five subscales ranged from 0.78 to 0.79, demonstrating the SPEE's acceptable content validity.
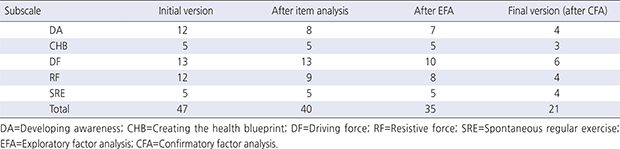
Preliminary testing was conducted for assessing the suitability of the SPEE. A total of thirty PDIs were asked about their understanding of the contents of the scale. Cronbach's α of .63~.94 for the five subscales showed good internal consistency of the initial version of the SPEE. Minor modifications were made to the scale based on their feedback. Appendix 2 summarizes the number of items in the SPEE at each stage of development. The final version of the scale with a total of twenty-one items is provided in Appendix 3.
The score ranges were 4~20, 3~15, 6~30, 4~20, and 4~20 for the DA, CHB, DF, RF, and SRE subscales, respectively. Each item was scored from 1 (never for the DA, CHB, and DF subscales; disagree for the RF and SRE subscales) to 5 (almost always for the DA, CHB, and DF subscales; strongly agree for the RF and SRE subscales). Higher scores on the DA, CHB, DF, and SRE subscales represented higher levels of motivation for those stages, whereas a higher score on the RF subscale represented a greater resistance to exercise.
Questionnaires were administered either at the hospital or the participant's home. Researchers were made available to answer any questions that the participant may have had. The average time for completing the questionnaire was approximately thirty minutes. Participants could opt for either location at their discretion and convenience. The questionnaires were in Traditional Chinese, and all participants were literate. The completed questionnaires were managed by the research team and remain confidential.
4. Ethical considerations
This study was approved by the institutional research board (Number IRB 101-69) and the research institute. The research objectives and procedure were explained to each participant before the start of the study. Participants were enrolled in the study after providing informed, written consent and right of withdrawal at any time was open to their discretion. Participants' identifying information, i.e., name, phone number, and address, were kept private and confidential in a secure data base that could only be accessed by the interviewing researchers. The research team assured confidentiality with all data accessed.
5. Data analysis
The Chi-square test was conducted to compare the demographic variables of the study sample for item analysis/EFA with the study sample for confirmatory factor analysis (CFA)/SEM. A p<.05 was considered statistically significant.
The following steps were performed for the development of the SPEE based on the Kuo model (Figure 1):
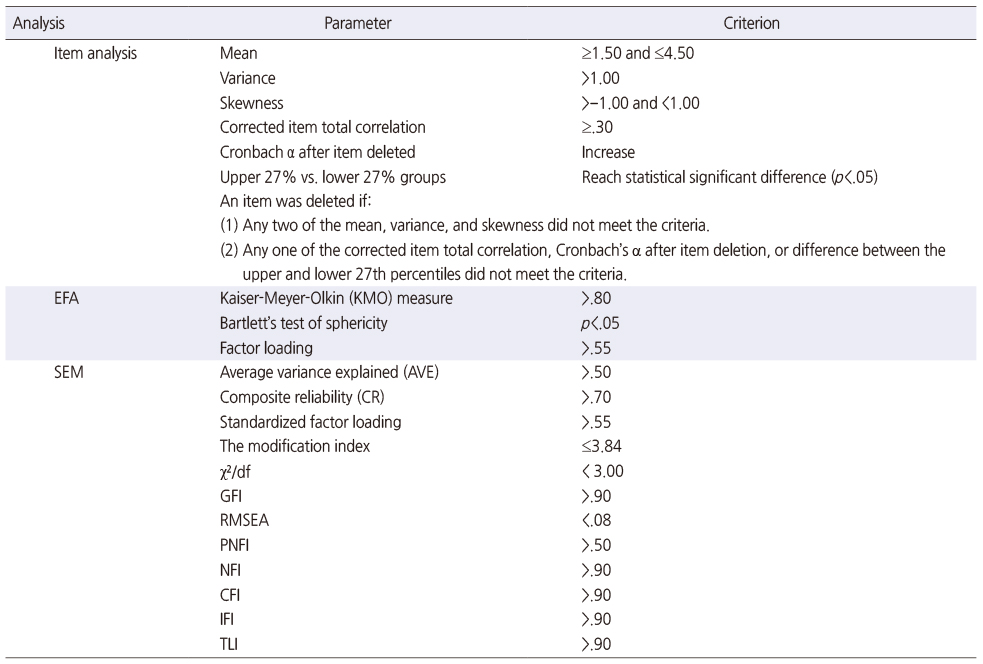
• Step 1: Item analysis was implemented to exclude unqualified items with low discrimination ability and internal consistency. Within each subscale, the mean, variance, skewness, corrected item total correlation [26], Cronbach's α coefficient after item deletion, and difference between lower 27% and upper 27% groups were evaluated.
• Step 2: EFA with maximum likelihood estimation was adopted for exploring latent structures with further item reduction in each subscale. First, the Kaiser-Meyer-Olkin (KMO) measure and Bartlett's test of sphericity were calculated and performed to evaluate sample adequacy for EFA. Parallel analysis [27] method was then used to decide the number of factors in each subscale. Only the factors with a derived eigenvalue by EFA greater than the corresponding values by parallel method were retained. Considering the sample size of 110 for EFA, the items with a factor loading of less than 0.55 [28] were also deleted due to low correlation with explored factors.
• Step 3: The SEM technique combining CFA and path analysis was conducted to validate measurement specificity of the subscales as well as the Kuo model (Figure 1). Through CFA, the scales' reliability and validity obtained from EFA were confirmed. Reliability and convergent validity of the factors were acceptable only if the corresponding composite reliability (CR) and average variance extracted (AVE) were greater than .70 and .50, respectively. Items were deleted due to lack of convergent validity if the derived factor loading by CFA was less than 0.55. The path coefficients were estimated via path analysis to evaluate the relationships of the DA, CHB, DF, RF, and SRE stages. The model's goodness of fit was evaluated based on χ2/df, goodness-of-fit index (GFI), comparative fit index (CFI), root mean square error of approximation (RMSEA), parsimonious normed fit index (PNFI), normed fit index (NFI), incremental fit index (IFI), and Tucker–Lewis index (TLI) [29].
The parameters with the corresponding criteria for the scale and model are summarized in Table 1. The scale with items and the Kuo model were considered suitable if they met the corresponding criteria. All analyses were performed using IBM SPSS Statistics 21.0 and AMOS 21.0 for Windows (SPSS, Chicago, IL) software.
Table 1
Evaluation Criteria for Reliability and Validity of Scales and Fit of Model
RESULTS
1. Demographics of the sampled participants
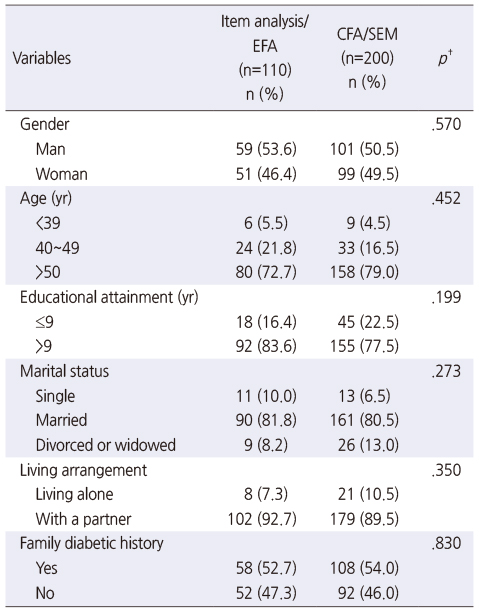
Of the total 310 valid questionnaires, 110 were collected using the initial version of the scale (Appendix 1) and analyzed using item analysis and EFA. The remaining 200 were subsequently collected for scale and model validation with SEM by using the revised and updated version based on the results of item analysis and EFA. The two respondent groups had similar demographic characteristics and did not differ significantly (all p>.05), as shown in Table 2. Slightly over half of the respondents were men, and most were aged 50 or older (>70%), well educated (>75% had >9 years of educational experience), married (>80%), and living with a partner (>89%). In addition, more than half of the entire PDI group had family histories of diabetes.
Table 2
Participant Demographics
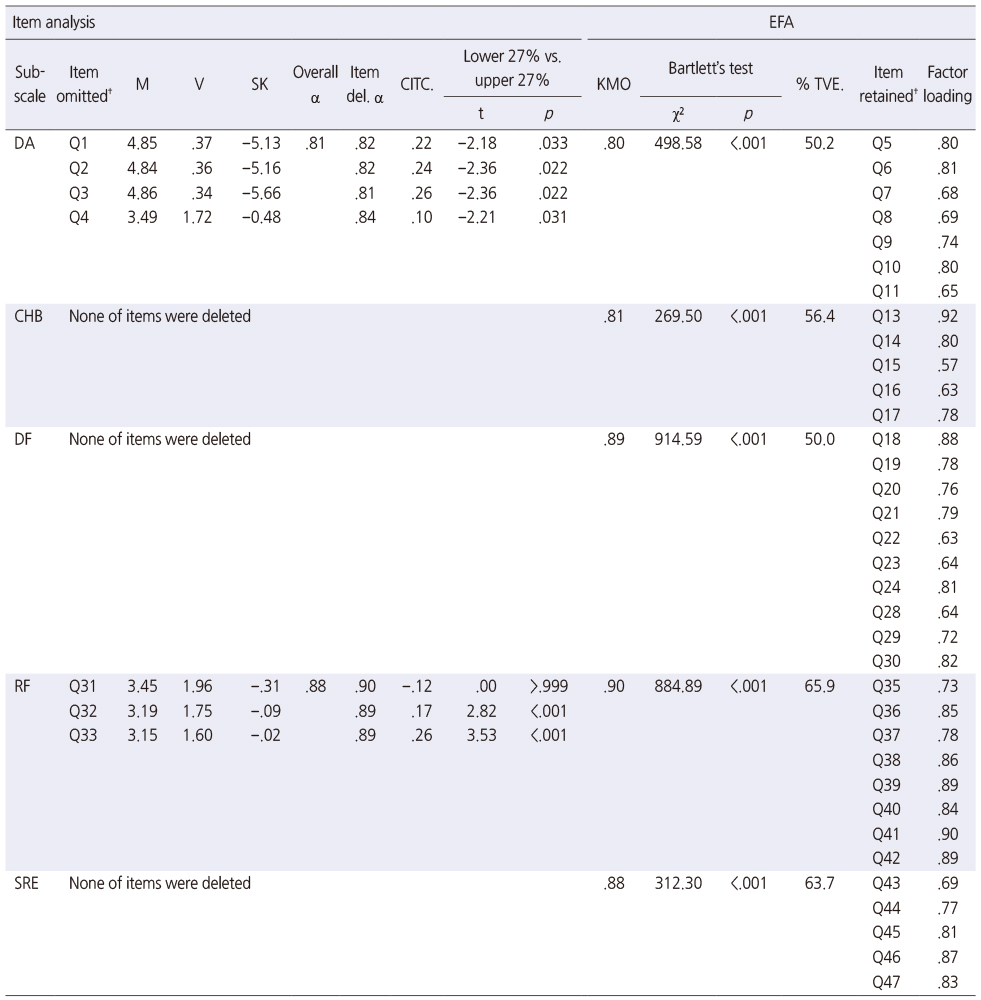
2. Reliability and exploration of the scale
The items omitted by item analysis due to low discrimination ability and internal consistency based on the criteria in Table 1 are shown in Table 3. An item was deleted if: 1) any two of the mean, variance, and skewness did not meet the criteria; 2) any one of the corrected item total correlation, Cronbach's α after item deletion, or difference between the upper and lower 27th percentiles did not meet the deletion criteria. Consequently, items Q1~Q4 (item numbers in the initial version of the scale, Appendix 1) in the DA subscale and items Q31~Q33 in the RF subscale were omitted. However, the EFA data in Table 3 shows the items retained based on the EFA results and the corresponding criteria in Table 1. The values of the KMO measure (.80~.90) and p<.001 of Bartlett's test revealed that the questionnaire data was adequate for EFA. Items Q12, Q25~Q27, and Q34 were omitted, as their factor loading was lower than .55. After implementing EFA, one factor was retained in each of the five SPEE subscales. The corresponding percentages of total variance explained ranged from 50.0% to 65.9%, demonstrating the subscales' acceptable ability to assess variability in the participants' responses after reduction and extraction following EFA [30].
Table 3
Item Analysis and Exploratory Factor Analysis
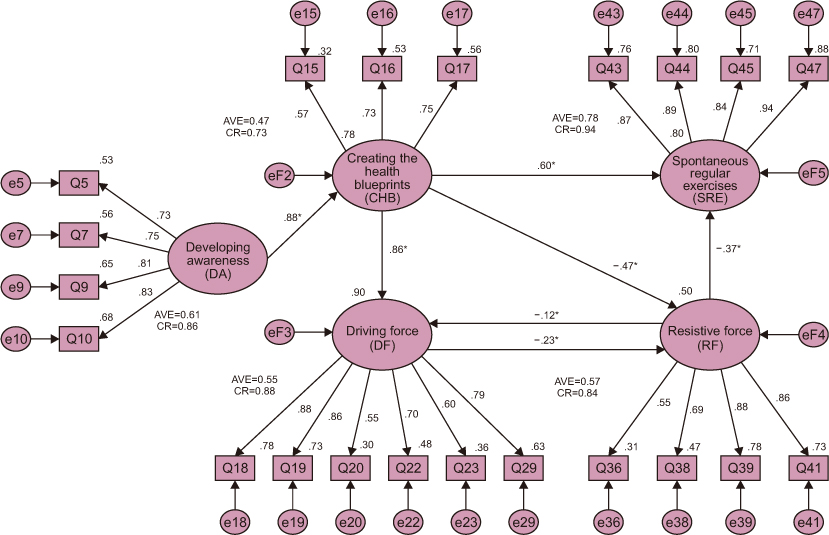
3. Validation of the scale and conceptual model
SEM was conducted to evaluate the validity of the measurement model of the subscales and structure of the Kuo model (Figure 1). The final SEM model with the path coefficients (standardized regression coefficients) presented in Figure 2. As shown in Figure 2, the final version of the five subscales was further reduced to 4, 3, 6, 4, and 4 items for the DA, CHB, DF, RF, and SRE subscales, respectively. Specific items were eliminated based on the modification index of SEM (Table 1). A CR of .73~.94, standardized factor loading of .55~.90, and AVE of 0.57~0.78 demonstrated acceptable convergent validity in each subscale. Only the AVE of .47 for the CHB subscale was slightly lower than .50.
Figure 2
SEM=Structural equation modeling; DA=Developing awareness; CHB=Creating the health blueprint; DF=Driving force; RF=Resistive force; SRE=Spontaneous regular exercise; AVE=Average variance explained; CR=Composite reliability; GFI=Goodness-of-fit index; RMSEA=Root mean square error of approximation; PNFI=Parsimonious normed fit index; NFI=Normed fit index; CFI=Comparative fit index; IFI=Incremental fit index; TLI=Tucker-Lewis index. *p<.05. †Item numbers in the figure are the item numbers of the items in the initial version of the scale (Appendix 1).
Structural equation modeling model.
χ2/df=2.08, GFI=.85, RMSEA=.07, PNFI=.77, NFI=.88, CFI=.93, IFI=.93, TLI=.92.
The analysis of the Kuo model included the measure of model fit χ2/df=2.08, GFI=.85, RMSEA=.07, PNFI=.77, NFI=.88, CFI=.93, IFI=.93, and TLI=.92, which indicated good fit between the Kuo model and the sample data (Figure 2). The exceptions were GFI and NFI, which were both slightly lower than .90. The standardized regression coefficients of DA on CHB, CHB on DF, DF on RF, and RF on DF were all statistically significant and supported H1, H2, H3, and H4 of the Kuo model (Figure 1). The standardized regression coefficients of DA to CHB (β=.88) and CHB to DF (β=.86) exhibited strong positive effects, whereas the coefficients of DF to RF (β=−.23) and RF to DF (β=−.12) exhibited negative effects. H5 for progression from the ACIS stage to the SRE stage was supported by the significant direct effect of RF on SRE (β=−.37). This revealed that SRE was directly motivated by a decline in RF. However, the DF effected SRE actions indirectly through the mediation effect of RF (β=−.23 of DF on RF). The conceptual process outlined by Kuo et al. [18] did not mention the effect of the CHB stage on the SRE stage. However, the results of this study revealed that the CHB stage also directly affected the SRE stage (β=.60).
DISCUSSION
The development of the SPEE for PDIs provides the medical profession with a convenient instrument to assess the psychological probability that a PDI will implement exercise. The SPEE is a 5-point scale containing 21 items, comprising DA (4 items), CHB (3 items), DF (6 items), RF (4 items), and SRE (4 items) (Appendix 3). This scale is the first exercise-engagement scale designed for PDIs and the first to assess the psychological milieu and behavioral outcome at each stage of the exercise-engagement process. The development process of the SPEE differs from other scales in several key manners: The hypoglycemia problem-solving scale developed by Wu et al. [31] for people with diabetes mellitus was constructed based on the original SPSI and its Chinese version, unlike the SPEE, which relied on the Kuo model foundation. Ebrahimi et al. [32] developed the Diabetes Adjustment Assessment Scale (DAAS) based on their qualitative study but without a conceptual model infrastructure. The DAAS is focused on patients diagnosed with type 2 diabetes and their adjustment to disease onset, not PDIs.
The DA and CHB subscales can be used to explore the levels of PDIs' self-awareness in terms of the importance of physical activity and psychological barriers to exercise. The concept is similar to Lin and Chi's SMS [20], which explores the factors that motivate an individual to engage in exercise. The main focus is interest in exercise, desire to learn a new sport, improved health, and sense of accomplishment. However, the SMS is designed for general public assessment and not for individuals with specific potential chronic health care needs. The DA subscale of the present study is designed to assess the perspective from the PDIs' point of view. Recognition of health risks is the cause or motivation, and the choice to engage in exercise is the effect, which leads to improved health and a reduction diabetes outcomes. Comparatively, the SMS adopted a broader perspective while covering more dimensions to determine the reasons that individuals engage in exercise.
The DF and RF subscales are similar to the ESES [19] in that both explore the factors that promote or hinder exercise habits among individuals. As with the SMS, the ESES focuses on the general population and not a specific at-risk subgroup. Both scales explore the counteracting effect between positive and negative factors that influence the choice to engage in exercise behavior. Further distinguishing the ESES from the SPEE, the DF and RF subscales are more effective at exploring PDIs' psychological and emotional status during the internal struggle stage. The psychological and emotional status in DF assesses willpower, self-blame, self-motivation, and consistency with regard to exercise. The SPEE is different from the ESES, where the focus explored positive motivations: 1) sense of happiness, 2) improved health, 3) enhanced muscle strength, and 4) bone density. However, the ESES failed to examine motivations to continue exercise over the long term. By comparison, the RF subscale explored: 1) denial, 2) difficulty, 3) sedentary passiveness, and 4) laziness, which are not assessed in the ESES.
The validation of the SPEE is consistent with the Kuo model of the process of exercise engagement in PDIs (Figure 1). The DA stage and its impact on PDIs is of greatest importance and strongly effects the CHB stage. Data showed a direct effect of the DA stage on the CHB stage. This is highly predictive of PDIs' potential to achieve exercise goals that will mediate or eliminate the onset of diabetes, as PDIs may choose to further educate themselves on the dangers of diabetes. The CHB stage motivates the SRE stage not only directly but also indirectly through the DF and RF stages. Furthermore, the effect of the SRE stage on the DF stage is positive, while it is negative on the RF stage. PDIs are able to empower themselves through education via the hospital or other means, which explains the effects on the DF and RF. The DF and RF stages are negatively and significantly correlated. For PDIs, the more acute the DA stage, the greater their motivation is for engaging in exercise and the smoother their entrance is into the CHB stage. DA stage acuteness does not influence the DF; as such, it may be proposed that during the DA stage, the type of education is extremely important. Once PDIs have crossed the CHB threshold and engaged in exercise, they enter the internal struggle cycle between DF and RF. This influences their exercise behaviors, which enhance or exacerbate their probability for developing diabetes. During the exercise-engagement process, DF and RF counteract each other; however, when a higher DF is present, PDIs more readily enter the SRE stage. In essence, PDIs must first reduce their RF to successfully enter the SRE stage. Therefore, although the RF is a mediating variable in this model, it is critical for determining whether PDIs will develop long-lasting exercise habits.
The findings of this study suggest that whether PDIs initially engage in exercise depends on the impact of the DA stage and, subsequently, whether exercise habits are established. Attaining the SRE stage is dependent to the extent that the RF is reduced, as increasing the DF is not useful. Providing PDIs with physical activity-related health education with the purpose of motivating regular exercise behaviors is crucial. The priority is to increase their awareness of the importance of exercise, followed with solutions and supporting strategies to eliminate factors that prevent regular exercise. In doing so, it is possible to reduce the effect of the RF.
The single difference between the study results and the Kuo model (Figure 1) is the direct and significant (β=.60) effect of the CHB stage on the SRE stage. As PDIs enter the CHB stage, they may enter the SRE stage directly, bypassing the DF and RF stages. The findings of this study strongly support the Kuo model and are consistent with Self-Determination Theory. This theory states that human behaviors are generated from intrinsic motivation, and the expression of these behaviors is subject to the influence of extrinsic factors [33]. Therefore, when providing relevant clinical health education, medical staff will best serve PDIs by developing awareness, specifically by helping PDIs to plan health blueprints. If PDIs perceive a positive outcome for behavioral change, the exercise intervention may be more effective.
Several factors may influence the transferability of the SPEE and the findings of this study. Due to time constraints, this study could not assess the long-term benefits of exercise and the predictive capacity of the SPEE. As a result of limited research budget and time, the research was confined to one geographic location. Another confounding factor is that the level of participants' education was consistently high, as the government of Taiwan has an enforced state education policy that has been in existence for the last 50 years. It is known that level of education influences behavioral modification.
In order to enhance the transferability of the SPEE, further studies should focus on: 1) psychological status of exercise for PDIs, 2) behavioral expression at various stages of the exercise-engagement process, and 3) contributing factors to the formation of long-term exercise habits. This research would have benefited greatly with the inclusion of a quantitative approach to assess changes in glucose levels as participants became engaged in exercise to reduce the long-term liability of developing diabetes.
Although the sample size of 110 in EFA of the current study met the minimum requirement suggested by Gorsuch [23] and Thompson [24]. However, the sample size of 235 based on the rule of five subjects for each item is the more preferable guideline for scale development [22]. Lack of enough power due to less sample size might be a limitation of the current study. Therefore, a further study with larger sample is suggested to conduct for providing stronger evidence to validate the developed scale and model.
CONCLUSION
This study is the first to develop a scale that includes the five subscales of DA, CHB, DF, RF, and SRE for assessing the psychological transition and behavioral expression at each stage of the process of exercise engagement for PDIs. The Kuo model for the process of exercise engagement of PDIs is valid and has a goodness of fit. Higher scores on the DA, CHB, DF, and SRE for people with prediabetes provides deeper insights into the behavioral change stages required to initiate extended long-term health care outcomes in order to avoid developing diabetes. These insights are significant as they allow for patient-specific mapping of their DF and RF and the factors affecting their transition to the SRE stage. The use of SPEE within the clinical setting may prove useful in developing tailored exercise strategies that may lead to a reduction in the rate of diabetes onset in PDIs.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Kuo YL & Chang SC.
Data curation or/and Analysis: Kuo YL.
Funding acquisition: Kuo YL.
Investigation: Kuo YL & Yeh HC.
Project administration or/and Supervision: Kuo YL.
Resources or/and Software: Chang SC & Yeh HC.
Validation: Kuo YL.
Visualization: Kuo YL.
Writing original draft or/and Review & editing: Kuo YL & Chang SC.
ACKNOWLEDGEMENTS
Thanks for Hualien Tzu Chi Hospital for assistance in collecting the data.
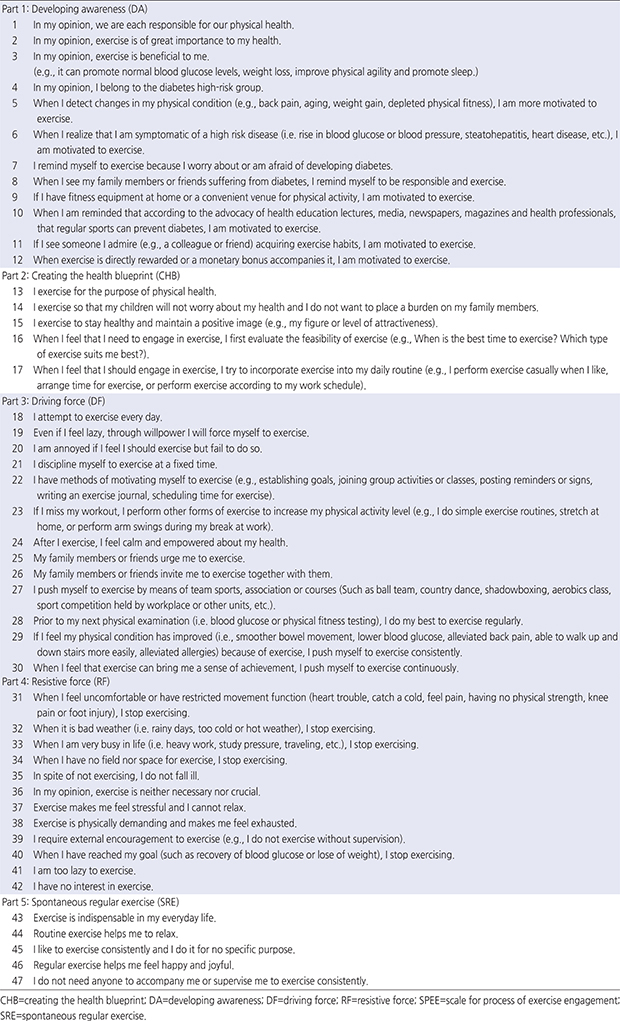
Appendix 1
Initial Version of the Scale for Process of Exercise Engagement (SPEE)
Appendix 2
Number of Items of the SPEE Scale at Each Stage of Analysis
Appendix 3
Final Version of Scale for Process of Exercise Engagement (SPEE)
References
-
International Diabetes Federation (IDF). IDF diabetes atlas (seventh edition) [Internet]. Brussels: IDF; c2015 [cited 2019 Jan 13].Available from: https://diabetesatlas.org/upload/resources/previous/files/7/IDF%20Diabetes%20Atlas%207th.pdf.
-
-
Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing diabetes prevention study: A 20-year follow-up study. The Lancet 2008;371(9626):1783–1789. [doi: 10.1016/S0140-6736(08)60766-7]
-
-
Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: A high-risk state for diabetes development. Lancet 2012;379(9833):2279–2290. [doi: 10.1016/S0140-6736(12)60283-9]
-
-
Plantinga LC, Crews DC, Coresh J, Miller ER 3rd, Saran R, Yee J, et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or prediabetes. Clinical Journal of American Society of Nephrology 2010;5(4):673–682. [doi: 10.2215/CJN.07891109]
-
-
Diabetes Prevention Program Research Group. The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the diabetes prevention program. Diabetic Medicine 2007;24(2):137–144. [doi: 10.1111/j.1464-5491.2007.02043.x]
-
-
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow-up of the Finnish diabetes prevention study. The Lancet 2006;368(9548):1673–1679. [doi: 10.1016/S0140-6736(06)69701-8]
-
-
Lindström J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish diabetes prevention study (DPS): Lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 2003;26(12):3230–3236. [doi: 10.2337/diacare.26.12.3230]
-
-
The Diabetes Prevention Program (DPP) Research Group. The diabetes prevention program (DPP): Description of lifestyle intervention. Diabetes Care 2002;25(12):2165–2171. [doi: 10.2337/diacare.25.12.2165]
-
-
Pedley CF, Case LD, Blackwell CS, Katula JA, Vitolins MZ. The 24-month metabolic benefits of the healthy living partnerships to prevent diabetes: A community-based translational study. Diabetes & Metabolic Syndrome 2018;12(3):215–220. [doi: 10.1016/j.dsx.2017.09.011]
-
-
Sato Y, Nagasaki M, Kubota M, Uno T, Nakai N. Clinical aspects of physical exercise for diabetes/metabolic syndrome. Diabetes Research and Clinical Practice 2007;77 3 Suppl:S87–S91. [doi: 10.1016/j.diabres.2007.01.039]
-
-
Bai YL, Wang LM, Hung SY, Chiou CP. [Exercise benefits for health of elderly diabetics]. Journal of Taiwan Nephrology Nurses Association 2012;11(3):1–7.Chinese.
-
-
Kuo YL, Chang SC, Chang M, Wang YW, Yeh SC. [The effects of multi-approach health education on people with pre-diabetes]. Journal of Evidence-Based Nursing 2008;4(4):297–306. [doi: 10.6225/JEBN.4.4.297]Chinese.
-
-
Chang SC, Hayter M, Yeh HC, Hsieh TC, Kuo YL. The effectiveness of different health education strategies in people with pre-diabetes: A randomized controlled trial. Journal of Health Science 2016;6(2):22–29. [doi: 10.5923/j.health.20160602.02]
-
-
Lin CY, Chi LK. [Development of the sport motivation scale: Analysis of reliability and validity]. Bulletin of Sport and Exercise Psychology of Taiwan 2003;(2):15–32.Chinese.
-
-
Stevens J. In: Applied multivariate statistics for the social sciences. 4th ed. Mahwah (NJ): Lawrence Erlbaum Associates; 2002. pp. 203-204.
-
-
Gorsuch RL. In: Factor analysis. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1983. pp. 109-110.
-
-
Thompson B. In: Exploratory and confirmatory factor analysis: Understanding concepts and applications. Washington, D.C.: American Psychological Association; 2004. pp. 273-275.
-
-
Davis LL. Instrument review: Getting the most from a panel of experts. Applied Nursing Research 1992;5(4):194–197. [doi: 10.1016/S0897-1897(05)80008-4]
-
-
Ferketich S. Focus on psychometrics. Aspects of item analysis. Research in Nursing & Health 1991;14(2):165–168. [doi: 10.1002/nur.4770140211]
-
-
Lautenschlager GJ, Lance CE, Flaherty VL. Parallel analysis criteria: Revised equations for estimating the latent roots of random data correlation matrices. Educational and Psychological Measurement 1989;49(2):339–345. [doi: 10.1177/0013164489492006]
-
-
Hair JF, Black WC, Babin BJ, Anderson RE. In: Multivariate data analysis. Harlow: Pearson Education Limited; 2014. pp. 115.
-
-
Hooper D, Coughlan J, Mullen M. Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods 2008;6(1):53–60. [doi: 10.21427/D7CF7R]
-
-
Lattin JM, Carroll JD, Green PE. In: Analyzing multivariate data. Pacific Grove (CA): Thomson Brooks/Cole; 2003. pp. 351-352.
-
-
Ebrahimi H, Karimi Moonaghi H, Asghari Jafarabadi M, Namdar Areshtanab H, Jouybari L. Development and preliminary validation of diabetes adjustment assessment scale (DAAS): A new measure of adjustment with type 2 diabetes. Journal of Caring Sciences 2016;5(2):145–152. [doi: 10.15171/jcs.2016.015]
-
-
Deci EL, Ryan RM. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry 2000;11(4):227–268. [doi: 10.1207/S15327965PLI1104_01]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

