Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 50(4); 2020 > Article
- Review Article Continuity of Care in Chronic Diseases: A Concept Analysis by Literature Review
- Jingjing Hu, Yuexia Wang, Xiaoxi Li
-
Journal of Korean Academy of Nursing 2020;50(4):513-522.
DOI: https://doi.org/10.4040/jkan.20079
Published online: August 31, 2020
2Department of Nursing, Henan Provincial People’s Hospital, People’s Hospital of Zhengzhou University, People’s Hospital of Henan University, Zhengzhou, China
Abstract
Purpose
This study aimed to utilize concept analysis to obtain a better understanding of the concept of “continuity of care” in chronic diseases.
Methods
The concept of continuity of care was analyzed using the Walker and Avant method. Covering literature in English from 1930 to 2018, the data sources included CINAHL Complete, Academic Search Complete, MEDLINE, PsyARTICLES, Health Source: Nursing/ Academic Edition, Google Scholar, Science Direct, and the Cochrane Library.
Results
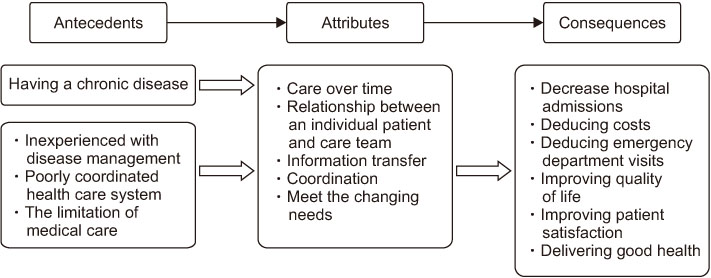
A comprehensive definition of concept of continuity of care was developed based on a systematic search and synthesis. The key defining attributes were identified as (a) care over time, (b) the relationship between an individual patient and a care team, (c) information transfer, (d) coordination, and (e) meeting changing needs.
The antecedents of continuity of care were having a chronic disease, inexperienced with disease management, a poorly coordinated healthcare system, and medical care limitations. The consequences of continuity of care were decreasing hospital admissions, reducing costs, reducing emergency room visits, improving the quality of life, improving patient satisfaction, and delivering good healthcare.
Conclusion
The thorough concept analysis provides insight into the nature of “continuity of care” in chronic diseases and also helps ground the concept in healthcare.
Published online Aug 31, 2020.
https://doi.org/10.4040/jkan.20079
Continuity of Care in Chronic Diseases: A Concept Analysis by Literature Review
Abstract
Purpose
This study aimed to utilize concept analysis to obtain a better understanding of the concept of “continuity of care” in chronic diseases.
Methods
The concept of continuity of care was analyzed using the Walker and Avant method. Covering literature in English from 1930 to 2018, the data sources included CINAHL Complete, Academic Search Complete, MEDLINE, PsyARTICLES, Health Source: Nursing/Academic Edition, Google Scholar, Science Direct, and the Cochrane Library.
Results
A comprehensive definition of concept of continuity of care was developed based on a systematic search and synthesis. The key defining attributes were identified as (a) care over time, (b) the relationship between an individual patient and a care team, (c) information transfer, (d) coordination, and (e) meeting changing needs. The antecedents of continuity of care were having a chronic disease, inexperienced with disease management, a poorly coordinated healthcare system, and medical care limitations. The consequences of continuity of care were decreasing hospital admissions, reducing costs, reducing emergency room visits, improving the quality of life, improving patient satisfaction, and delivering good healthcare.
Conclusion
The thorough concept analysis provides insight into the nature of “continuity of care” in chronic diseases and also helps ground the concept in healthcare.
INTRODUCTION
Worldwide, illness, disability, and death are mostly caused by chronic diseases such as cancer, type 2 diabetes, chronic lower respiratory conditions, and heart disease [1]. The increasing prevalence of chronic disease has given rise to both public health and economic threats, with estimated costs expected to reach approximately $7 trillion by 2025 [2]. Chronic diseases are a long-term problem. Caring for patients with chronic diseases has increasingly focused on the improvement of their quality of life (QoL) [3]. Improving the QoL among chronic disease patients has become a crucial problem, and primary care providers are usually tasked with improving the QoL of patients with chronic diseases. Continuity of care is considered a significant component of primary care that reduces the likelihood that older adults will experience serious illness. It needs a consistent experience in the healthcare system that involves focusing on the patients' needs, often leading to improved outcomes for patients with chronic diseases [4]. By establishing long-term relationships between physicians and chronic disease patients, improvements can be made in communication, understanding patients' medical histories, self-management, and disease monitoring [5]. It has been proven to improve chronic patients' QoL and has been recommended by the American Association for Continuity of Care [6, 7, 8].
First proposed in the late 1940s, the concept of continuity of care was used for hospitals to estimate the need for healthcare professionals [9]. In the 1950s, the focus shifted to a personal care provider—namely, the community nurse [10]. Then, in the 1970s, emphasis was placed on past and present care as well as coordination [11]. Multiple factors were considered to define continuity of care, including communication, ongoing relationships, flexibility, and patients' needs [12]. However, after the mid-1970s, continuity of care measurements gained attention, and continuity meant sustaining a relationship with the same physician [13]. Measurement instruments that emerged at that time included the Continuity of Care Index (COCI) [14], Sequential Continuity (SECON) index [15], and Usual Provider of Care (UPC) index [16]. Multivariate models began to appear again in the 1990s, and the definition of continuity of care became more concerned with patients' perspectives [17]. Continuity of care is a complex concept, and many types of continuities have been identified. Longitudinal continuity emphasizes the medical setting where patients can get the most care. Relational continuity concerns the sustained relationship between patient and provider. Meanwhile, informational continuity involves information transfer and following the patient [18]. Continuity of care can also cover communication between the patient and provider, personalized care, and high-efficiency discharge. It has been found that positive personal involvement is beneficial for continuity of care in patients with chronic diseases [19].
Due to the increasing number of group practices and the growth of the clients' movement, the definition of continuity of care has remained highly variable [20]. Although the concept of continuity of care has been identified many times, its overlap with related concepts, such as integrated care, care coordination, and patient-centered care, has not been thoroughly distinguished, and there is still confusion and ambiguity regarding its definition [21]. Hence, a concept analysis of continuity of care is greatly needed.
In this study, we aimed to obtain a better understanding of the term “continuity of care” in chronic diseases. An improved understanding could help create an operational definition and develop, as well as evaluate, continuity of care instruments to guide clinical practice. The findings of this work might also facilitate the use of continuity of care in the workplace to help chronic disease patients receive improved care.
METHODS
1. Study design
It is well known that the process of concept analysis informs theory development and promotes communication [22]. The method developed by Walker and Avant was selected for this concept analysis because it is universal and systematic [23]. Moreover, this method of concept analysis has been effectively used in the nursing field and has shown good performance [23]. There are eight steps as follows: Select a concept, determine the aim or purpose of the analysis, identify all uses of the concept, determine the defining attributes, construct a model case, construct other cases, identify antecedents and consequences, and define empirical referents. Furthermore, this method is a dynamic and repeated process rather than a step-by-step technique [23].
2. Research subjects
A systematic literature search was conducted as the foundation for this concept analysis. The search was performed using relevant databases such as CINAHL Complete, Academic Search Complete, MEDLINE, PsyARTICLES, Health Source: Nursing/Academic Edition, Google Scholar, Science Direct, and the Cochrane Library. Using Boolean operators and truncation, the key search terms were “continu* of care” OR “continu* care,” along with the search term “concept* analysis” OR “concept* definition.” Articles were included if they conformed to the following inclusion criteria: 1) full text, 2) scholarly (peer-reviewed) journals, 3) English language, and 4) publication between 1930~2018. Additionally, for a specific search, the first search term was limited to articles that listed the search term in the title, while the second term was presented in the full text.
3. Data collection and analysis
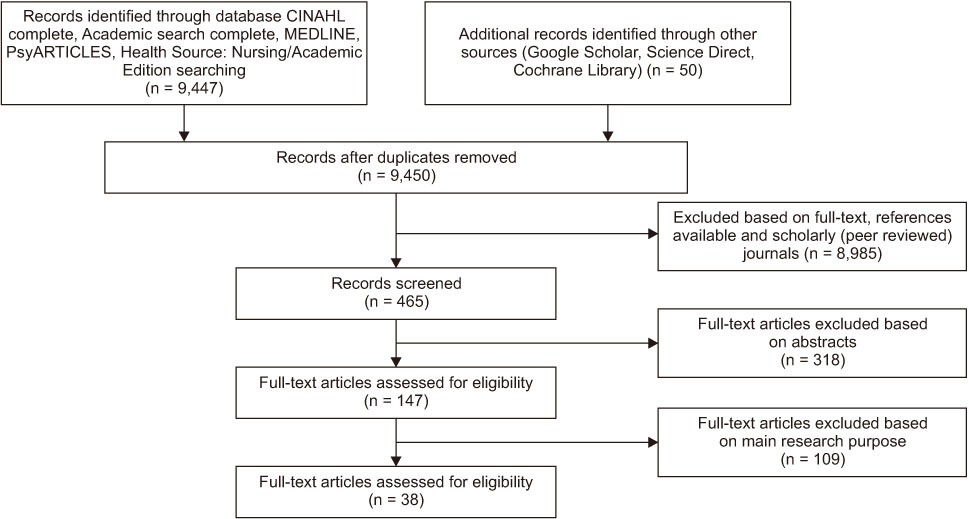
Aside from the relevant databases, some online dictionaries were used to find additional definitions of continuity of care. A total of 465 papers were identified in the search process. We removed duplicates and assessed time and language limitations. Also, we only included peer-reviewed works. Two researchers independently evaluated the abstracts and content of the included literature. Then, their evaluation results were compared. When they had different opinions, the two parties thoroughly discussed and analyzed the literature until they reached agreement. After examining the abstracts, 147 articles were included. Finally, 38 papers were included in the concept analysis (Figure 1) using the following exclusion criteria: (a) irrelevance to continuity of care related to chronic disease, and (b) irrelevance to the primary research purpose. The whole process was conducted by two researchers from June 20, 2018, to August 25, 2018.
Figure 1
Flowchart of the data selection process.
RESULTS
1. Definitions of continuity of care
The McGraw-Hill Concise Dictionary of Modern Medicine defines continuity of care as “uninterrupted healthcare for a condition from the time of first contact to the point of resolution or long-term maintenance” [24]. The Farlex Partner Medical Dictionary defines continuity of care as “the desired goal of a model of care in which the same generalist physician serves as advisor, advocate, and friend as the patient moves through the various stages of medical care” [25].
According to the American Academy of Family Physicians, continuity of care is concerned with quality of care over time [26]. This is the process by which a patient and his or her physician-led care team are cooperatively involved in ongoing healthcare management, with the shared goal of high-quality, cost-effective medical care. However, continuity of care in nursing focuses on the “transformation” of information and “communication” with nurses, as well as the “coordination” of care over time to maintain a personalized approach that can meet patients' changing needs [27]. Based on carefully examining these various definitions, we can assert that continuity of care is a continuous process of mutual medical assistance that involves healthcare management, cooperation, and an ongoing relationship.
2. Uses of the concept
Continuity of care was first formally described in 1947 as a planned exchange of information between a hospital and other nursing agencies that considered the patient and his or her life as a whole, shifting the focus from the disease to the patient [9]. Moreover, it has been a widely used term in the health discipline, nursing, and measurement [17]. Continuity in primary care is described as an uninterrupted relationship between patient and provider intended to improve quality of life [5]. Continuity of care emphasizes the “flexibility” and “coordination” of service as well as “stability” and “contact” over time in the relationship between the patient and provider in mental health. To meet patients' multiple and changing needs, a care team is more beneficial than a single provider [28]. Regarding disease management, continuity of care is described as services delivered by health professionals in “a coherent, logical, and timely fashion” through multiple healthcare settings [29].
3. Defining attributes
Walker and Avant [23] suggested that defining attributes is the core part of concept analysis, which mainly identifies characteristics that appear repeatedly and distinguishes the concept from other similar concepts. Continuity of care has five defining attributes that are seen in the process of healthcare delivery: care over time, the relationship between the patient and care team, information transfer, coordination, and meeting changing needs.
1) Care over time
Care over time is a longitudinal or chronological dimension, as well as an essential part of continuity. The time frame, which differentiates continuity of care from other concepts, may be short or long [17]. Continuity has often been used to describe “longitudinality,” which refers to establishing a long-term relationship with providers [30]. Continuity of care includes a period of time during which care is delivered by a healthcare team, and it emphasizes the ability to provide support over time [27, 31]. Continuity of care involves not only a relationship but also trust or dependence in care.
2) Relationship between patient and care team
The relationship between a patient and care team has evolved from one patient, one provider to one patient, multiple providers; it now emphasizes the relationship between one person and his or her care team [28, 31]. This shift reflects the increasing specialization in clinical care [29]. For patients with chronic diseases, relational continuity—which concerns the relationship between a patient and care team—is based on mutual trust and responsibility [32].
3) Information transfer
Information transfer serves to guarantee continuity of care in hospitals and nursing homes through the development of information systems. More massive transfer infrastructures are being developed to meet the increasing needs of older patients and to maintain continuity of care [31]. Reliable, accurate and timely information-transmission systems and positive medical staff can promote improved continuity of care [33].
4) Coordination
Coordination, which means bringing all people involved in an activity together in an organized way, is the core component of continuity of care. With coordination, the process of service delivery is uninterrupted; without coordination, patients will receive suboptimal care [27, 34]. Moreover, coordination emphasizes cohesion, smoothness, and connectedness, which will enhance the relationship between a service user and providers [28].
5) Meeting changing needs
Meet changing needs is an essential goal of continuity of care. In complex and competitive environments, patients' needs constantly change, especially among those with chronic diseases such as COPD, mental disorders, and coronary artery disease [28, 29, 32]. Meeting patients' multiple needs can improve quality of life and reduce hospital admissions and medical costs [32].
4. Operational definition
In chronic disease contexts, continuity of care is a process that involves care over time. To meet patients' changing needs, continuity of care emphasizes information transfer and relationship coordination between patients and their care teams in ongoing healthcare management.
5. Model case construction
Tom is a seventy-year-old male who has suffered from COPD for 20 years. Last month he caught a cold that induced an acute exacerbation of COPD. Then, he was sent to a hospital and discharged a week later, but his pulmonary function became worse than before. His physician talked to him about his condition and wanted to build continuous care (care over time) with him to help him manage his chronic disease. He understood his condition and poor self-control and was therefore glad to accept the physician's suggestions. Then, his medical information was transferred to the community clinic by the hospital (information transfer). At the community, Tom was assisted by a care team that consisted of three nurses and one doctor. Every week, Tom would receive telephone care, which mainly involved symptom assessment, continuous health education, and emotional support. Every two weeks, he would receive a home visit from a community nurse for the same purpose (relationship between patient and care team). Tom listened to the suggestions and positively engaged with them. Cooperation between the community and the hospital also helped Tom get optimal care (coordination). Moreover, if he had any requests, the care team would record them and try to accommodate them (meeting changing needs). Ultimately, Tom had fewer hospital admissions and lower healthcare costs, as well as an improved quality of life.
6. Contrary case construction
Jack is a sixty-year-old male who lives alone and has been suffering from diabetes for 15 years. Every year, he must make three or four hospital visits. Last month, he went to the hospital again. When he was discharged, his physician only prescribed some medicine for him (failed care over time). Because of poor self-management, he usually forgot to take the oral hypoglycemic or insulin. When he went to the nearest community clinic experiencing discomfort, he had to spend more time there because the doctors were not familiar with his condition (failed coordination) and did not have his medical information (failed information transfer). When he was back at home, he did not receive telephone calls or home visits from his physician (failed relationship between patient and care team). Moreover, when he had questions and called the hospital, they told him to consult an outpatient service (failure to meet changing needs). As a result, he had few opportunities to communicate with professionals unless he returned to the hospital, and he lived in poor physical condition.
7. Antecedents
Events that occur before the concept are antecedents [23]. The antecedents of the concept of continuity of care can be divided into two parts. From the patient's perspective, they include 1) having a chronic disease and 2) inexperienced with disease management. From the perspective of those who deliver healthcare, the antecedents are 3) a poorly coordinated healthcare system and 4) the limitations of medical care.
Having a chronic disease is an important reason for not easily participating in treatment. The prevalence of chronic disease and the possibility of long-term treatment underscore the importance of continuity of care [6]. In health service delivery systems, the biggest challenge concerns how to improve healthcare for people with chronic health conditions. Providing uninterrupted healthcare service—known as continuity or coordination of care—is a key part of the issue [35]. Hustoft et al. [31] reported that people with chronic diseases are inexperienced and lack disease-management skills; therefore, they need long-term guidance from health professionals. Hussey et al. [36] found that poor coordination and complex care are common in healthcare systems, resulting in suboptimal care for patients experiencing chronic disease. Wagner et al. [37] emphasized that when medical care is limited, it cannot meet the changing needs of chronic disease patients. All of these are factors related to the emergence of continuity of care.
8. Consequences
Consequences are events that occur as outcomes of the concept [23]. The consequences of continuity of care have two beneficiaries: patients and care providers. For patients, 1) decreased hospital admissions, 2) reduced costs, and 3) reduced emergency room visits are the immediate consequences of continuity of care. As continuity of care increases, there is a significantly lower likelihood of hospital admissions, along with lowered healthcare costs and fewer emergency room visits. Thus, developing long-term relationships between physicians and patients may improve future health outcomes [32, 38]. In addition, 4) improving quality of life is another necessary consequence. Continuity of care can have a positive influence on patients with long-term chronic conditions [39]. Hypertensive patients involved in continuity of care have an improved living status compared to non-continuity of care patients [40].
For care providers, patient satisfaction is a vital consequence of continuity of care. Clinicians should maintain long-term continuity of care as a means of 5) improving patient satisfaction. Discontinuous care can lead to poor health outcomes. Conversely, keeping sustained and trusting relationships with primary care providers can improve patient satisfaction [41]. 6) Delivering good healthcare is also a vital consequence. Continuity of care is a key element of providing better healthcare. Moreover, a high level of continuity of care can deliver good healthcare in terms of both the process and the outcomes [39]. Figure 2 presents a conceptual diagram consisting of antecedents, attributes, and consequences.
Figure 2
Concept diagram of “continuity of care”.
9. Defining empirical referents
Empirical referents are “classes or categories of actual phenomena that by their existence or presence demonstrate the occurrence of the concept itself” [23]. Several empirical referents of continuity of care have been developed in the literature. Although continuity of care can be measured from the provider's perspective [7], it is mostly measured from the patient's perspective. For example, the COCI mainly describes the dispersion aspect, which consists of the number of providers and visits [32]. The UPC index measures the density of visits with the same provider [42]. The SECON index describes the sequence aspect, which refers to the patterns of patient visits [43]. Finally, the Modified Continuity Index (MCI) and the Modified Modified Continuity Index (MMCI) measure the concentration of care with providers [44]. These indices are convenient and easy to acquire; however, there has been increasing criticism of them in recent years. For example, they fail to consider the content of visits and whether care providers' efforts are consistent with those of patients [30].
Though it is challenging to develop a perfect instrument to measure all attributes of continuity of care, the modified questionnaire of Continuity of Care between Care Levels (CCAENA©), which includes seven items measuring relational continuity, four items measuring informational continuity, and three items measuring managerial continuity, might be the most suitable method [30]. The initial validation of the CCAENA questionnaire was performed in Spain, and it showed high face and content validity, as well as appropriate construct validity [45]. Its validity and reliability were again verified by Aller et al. [46] with a random sample of 1,500 patients. Meanwhile, to analyze the perception of continuity of care in patients with chronic diseases, Vialoni et al. [47] conducted a cross-sectional study that applied the CCAENA questionnaire in six countries with 4,881 samples. A high level of continuity of care was found among primary doctors as compared to secondary care doctors.
DISCUSSION
This study used concept analysis to obtain a better understanding of “continuity of care” with regard to chronic diseases. The findings indicated that continuity of care refers to a process that involves information transfer and relationship coordination between patients and their care teams during their ongoing healthcare management. Compared to previous studies of similar concepts, such as coordination of care, integration of care and patient-centered care, continuity of care was found to have unique value, even though these are all patient-centered concepts [21]. Coordination of care concerns cooperation between different care providers. Integration of care, meanwhile, includes the sharing of responsibilities and care organization in addition to communication and cooperation. Finally, patient-centered care concerns shared decision-making and patient involvement [21]. Thus, the coordination and integration of care do not include the importance of the personal care team. A personal relationship between a patient and care team will facilitate patient-centered care but is not a necessary element.
Given the increasing number of patients with chronic diseases as well as economic threats, continuity of care has become even more necessary. For chronic disease patients, care over time involves a long period of care that is delivered by a healthcare team [27]. It involves not only relationships but also trust or dependence on care. Developing long-term relationships between nurses and patients may improve future health outcomes [32, 38]. The relationship between an individual patient and his or her care team is a significant attribute of continuity of care. Regarding interpersonal relations, the focus has shifted from relationships in the hospital to those in a broader nursing area. Home visits and telephone education are more commonly used to build relationships between nurses and patients. These interventions are also continuity of care-related approaches. Moreover, accurate, timely, and reliable information-transmission systems can promote improved continuity of care for chronic disease patients [33]. As the core component of continuity of care, coordination can provide uninterrupted service for people with chronic diseases [27, 34]. Finally, to improve quality of life and reduce hospital admissions and medical costs for chronic disease patients, it is necessary to meet the changing needs of patients [32].
The strength of this concept analysis is that it is the first conceptual definition to explore the continuity of care in chronic diseases. It also creates an operational definition and develops or evaluates the instruments of continuity of care to guide clinical practice. Lastly, it may also facilitate the use of continuity of care in healthcare workplaces, which may help more chronic disease patients receive better care.
A limitation of the review in this study is that it covers only papers written in English. This restriction might, therefore, limit the resulting insights and perspectives. A methodological limitation is that the findings from this method can be subjective, because different researchers may have different opinions regarding the literature and ultimately report different results.
Compared to previous studies, the important new findings of this study include an operational definition and a perfect instrument for continuity of care. Moreover, this study can provide a practical framework for researchers, policymakers, and health professionals that will facilitate a better understanding of and communication about continuity of care in chronic disease contexts. In addition, the thorough concept analysis present here could provide insight into the nature of continuity of care in relation to chronic diseases and help ground the concept in healthcare.
CONCLUSION
The results of this concept analysis indicated that continuity of care involved care over time. To meet patients' changing needs, continuity of care emphasized information transfer and relationship coordination between patients and their care teams in their ongoing healthcare management.
The chronic disease patients needed continuity of care when they were inexperienced with disease management. In addition, a poorly coordinated healthcare system and the limited medical care were highly related to the emergence of continuity of care.
The implementation of measures to ensure continuity of care in chronic disease could improve quality of life and patient satisfaction, reduce costs, hospital admissions and emergency room visits, and deliver good healthcare. Besides, the modified Questionnaire of Continuity between Care Levels (CCAENA) might be the most suitable instrument to measure all attributes of continuity of care.
This study's findings will facilitate an in-depth understanding and communication in healthcare, as well as guide better nursing practice and patient care.
This manuscript is a revision of the first author's master's thesis from Institute of Technology, Tralee. Year of 2017.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Hu J & Wang Y & Li X.
Data curation or/and Analysis: Hu J & Wang Y & Li X.
Funding acquisition: None.
Investigation: None.
Project administration or/and Supervision: Hu J.
Resources or/and Software: None.
Validation: Hu J.
Visualization: Hu J & Li X.
Writing original draft or/and Review & editing: Hu J & Wang Y & Li X.
ACKNOWLEDGEMENTS
I would like to acknowledge the support of Nursing Department, Henan Provincial People's Hospital and IT Tralee Nursing Faculty.
References
-
World Health Organization (WHO). Chronic disease and health promotion [Internet]. Geneva: WHO; c2016 [cited 2019 Feb 2].Available from: http://www.who.int/chp/en/.
-
-
World Health Organization (WHO). Global action plan for the prevention and control of NCDs 2013-2020 [Internet]. Geneva: WHO; c2013 [cited 2019 Feb 2].Available from: http://www.who.int/nmh/events/ncd_
action_ plan/en/.
-
-
Kizhakkeveettil A, Whedon J, Schmalzl L, Hurwitz EL. Yoga for quality of life in individuals with chronic disease: A systematic review. Alternative Therapies in Health & Medicine 2019;25(1):36–43.
-
-
van Servellen G, Fongwa M, Mockus D'Errico E. Continuity of care and quality care outcomes for people experiencing chronic conditions: A literature review. Nursing & Health Sciences 2006;8(3):185–195. [doi: 10.1111/j.1442-2018.2006.00278.x]
-
-
Björkelund C, Maun A, Murante AM, Hoffman K, De Maeseneer J, Farkas-Pall Z. Impact of continuity on quality of primary care: From the perspective of citizens' preferences and multimorbidity - position paper of the European Forum for Primary Care. Quality in Primary Care 2013;21(3):193–204.
-
-
National Organization for Rare Disorders (NORD). American Association for Continuity of Care [Internet]. Danbury: NORD; c2019 [cited 2019 Feb 2].
-
-
Joint Committee of the NLNE and NOPHN on the Integration of the Social and Health Aspects of Nursing in the Basic Curriculum; Subcommittee to Study the Hospital Referral of Patients for Continuity of Nursing Care. Carn I, Frost H. Hospital referral of patients for continuity of nursing care. The American journal of nursing 1947;47(11):761–764. [doi: 10.2307/3457729]
-
-
Farrisey RM. Continuity of nursing care and referral systems. American Journal of Public Health & the Nation's Health 1954;44(4):449–454. [doi: 10.2105/ajph.44.4.449]
-
-
Breslau N, Reeb KG. Continuity of care in a university-based practice. Journal of Medical Education 1975;50(10):965–969. [doi: 10.1097/00001888-197510000-00006]
-
-
Spruill CT, Heaton A. The challenge of continuity of care: Evolution of a nursing care model in NICU. Newborn & Infant Nursing Reviews 2015;15(2):72–76. [doi: 10.1053/j.nainr.2015.04.005]
-
-
Walker LO, Avant KC. In: Strategies for theory construction in nursing. 5th ed. Boston (MA): Prentice Hall; 2011.
-
-
McGraw-Hill Concise Dictionary of Modern Medicine. Continuity of care [Internet]. New York: McGraw-Hill; c2002 [cited 2019 Feb 2].Available from: https://medical-
dictionary.thefreedictionary.com/continuity+of+care.
-
-
Farlex Partner Medical Dictionary. Continuity of care [Internet]. Huntingdon Valley: Farlex, Inc.; c2012 [cited 2019 Feb 2].Available from: https://medical-
dictionary.thefreedictionary.com/continuity+of+care.
-
-
American Academy of Family Physicians (AAFP). Continuity of care, definition of [Internet]. Leawood: AAFP; c2015 [cited 2019 Feb 2].Available from: https://www.aafp.org/about/policies/all/definition-
care.html.
-
-
Giuliano C, Parmenter BJ, Baker MK, Mitchell BL, Williams AD, Lyndon K, et al. Cardiac rehabilitation for patients with coronary artery disease: A practical guide to enhance patient outcomes through continuity of care. Clinical Medicine Insights. Cardiology 2017;11:1179546817710028 [doi: 10.1177/1179546817710028]
-
-
Hustoft M, Biringer E, Gjesdal S, Abmus J, Hetlevik Ø. Relational coordination in interprofessional teams and its effect on patient-reported benefit and continuity of care: A prospective cohort study from rehabilitation centres in Western Norway. BMC Health Services Research 2018;18(1):719. [doi: 10.1186/s12913-018-3536-5]
-
-
Perdok H, Verhoeven CJ, van Dillen J, Schuitmaker TJ, Hoogendoorn K, Colli J, et al. Continuity of care is an important and distinct aspect of childbirth experience: Findings of a survey evaluating experienced continuity of care, experienced quality of care and women's perception of labor. BMC Pregnancy and Childbirth 2018;18(1):13. [doi: 10.1186/s12884-017-1615-y]
-
-
Hetlevik Ø, Hustoft M, Uijen A, Abmus J, Gjesdal S. Patient perspectives on continuity of care: Adaption and preliminary psychometric assessment of a Norwegian version of the Nijmegen Continuity Questionnaire (NCQ-N). BMC Health Services Research 2017;17(1):760. [doi: 10.1186/s12913-017-2706-1]
-
-
Gleason JL, Beck KH. Examining associations between relocation, continuity of care, and patient satisfaction in military spouses. Military Medicine 2017;182(5-6):e1657–e1664. [doi: 10.7205/MILMED-D-16-00191]
-
-
Ellis J, Zeng C, Steiner J, Shoup JA, McQuillan D, Bayliss E. D2-5: Interpersonal continuity of care and utilization among multimorbid seniors in an integrated healthcare system. Clinical Medicine & Research 2014;12(1-2):86. [doi: 10.3121/cmr.2014.1250.d2-5]
-
-
Vitaloni M, Vargas I, Vázquez ML, Ollé L, Unger JP, Mogollón A, et al. Users perception of relational continuity of care in six Latin America countries healthcare networks. European Journal of Public Health 2017;27 Suppl 3:ckx187.187 [doi: 10.1093/eurpub/ckx187.187]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

