Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 51(1); 2021 > Article
- Research Paper Sub-Health Status Survey and Influential Factor Analysis in Chinese during Coronavirus Disease 2019 Pandemic
- Yanbin Pan, Jianlong Yan, Wanxian Lu, Miaohang Shan
-
Journal of Korean Academy of Nursing 2021;51(1):5-14.
DOI: https://doi.org/10.4040/jkan.20241
Published online: February 28, 2021
2The First Clinical Medical College, Jinan University, Guangzhou, China
3Department of Cardiology, Shenzhen People’s Hospital, The Second Clinical Medical College of Jinan University, Shenzhen, China
Abstract
Purpose
This study aimed to investigate sub-health status (SHS) of people living in China during the Coronavirus disease 2019 (COVID-19) COVID-19 pandemic. COVID-19 is a severe acute respiratory syndrome coronavirus (SARS-CoV) infection-induced acute infectious disease, which is featured by universal susceptibility and strong infectivity, and SHS (a status of low quality health) refers to a status of low-quality health. COVID-19 has gradually developed into a global pandemic, making the public in a high stress situation in physiological, psychological and social states in the short term.
Methods
From March 6 to 11, 2020, a large-scale cross-sectional survey was conducted by convenient sampling, and SHS assessment scale was used in the questionnaire. The ordinal logistic regression analysis was used to identify the factors affecting SHS.
Results
In this study, 17,078 questionnaires were delivered with 16,820 effective questionnaires collected, and 10,715 subjects (63.7%) were found with SHS, with moderate SHS primarily. Physiological sub-scale scored the highest, followed by psychological and social sub-scales. Ordinal logistic regression analysis indicated that man, only-child, workers and farmers were risk factors of SHS. Protective factors of SHS included living in rural areas and townships, laid-off retirees and education degree.
Conclusion
It shows many people in China place in a poor health status during COVID-19 pandemic. It is necessary that relevant departments pay more attention to people with poor health such as men, only-child, urban people, workers and farmers, and groups with high education degree during and after pandemic stabilization.
Published online Feb 28, 2021.
https://doi.org/10.4040/jkan.20241
Sub-Health Status Survey and Influential Factor Analysis in Chinese during Coronavirus Disease 2019 Pandemic
Abstract
Purpose
This study aimed to investigate sub-health status (SHS) of people living in China during the Coronavirus disease 2019 (COVID-19) COVID-19 pandemic. COVID-19 is a severe acute respiratory syndrome coronavirus (SARS-CoV) infection-induced acute infectious disease, which is featured by universal susceptibility and strong infectivity, and SHS (a status of low quality health) refers to a status of low-quality health. COVID-19 has gradually developed into a global pandemic, making the public in a high stress situation in physiological, psychological and social states in the short term.
Methods
From March 6 to 11, 2020, a large-scale cross-sectional survey was conducted by convenient sampling, and SHS assessment scale was used in the questionnaire. The ordinal logistic regression analysis was used to identify the factors affecting SHS.
Results
In this study, 17,078 questionnaires were delivered with 16,820 effective questionnaires collected, and 10,715 subjects (63.7%) were found with SHS, with moderate SHS primarily. Physiological sub-scale scored the highest, followed by psychological and social sub-scales. Ordinal logistic regression analysis indicated that man, only-child, workers and farmers were risk factors of SHS. Protective factors of SHS included living in rural areas and townships, laid-off retirees and education degree.
Conclusion
It shows many people in China place in a poor health status during COVID-19 pandemic. It is necessary that relevant departments pay more attention to people with poor health such as men, only-child, urban people, workers and farmers, and groups with high education degree during and after pandemic stabilization.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a severe acute respiratory syndrome coronavirus (SARS-CoV) infection-induced pulmonary inflammation, which is manifested as fever, dry cough, and fatigue. Even worse, severe patients may experience acute respiratory distress syndrome, septic shock, coagulation disorder, and multiple organ failure in a rapid way [1]. COVID-19 is a public health emergency, the pandemic spread rapidly, affecting most parts of China, which also outbreaks and spreads in many overseas countries successively. Up to the date of this survey by questionnaire, 80,409 confirmed cases and 3,012 deaths have been reported in China; besides, there have been confirmed cases in at least 76 countries globally [2]. China has rapidly launched strong emergency measures, categorized it into class-B infectious (e.g., infectious atypical pneumonia and acquired immune deficiency syndrome [AIDS]) diseases and treated it as class-A (plague and cholera). However, COVID-19 is characterized by universal susceptibility and strong infectivity. The number of confirmed and suspected patients increases rapidly in a short period of time, which makes the public in a high level of physiological, psychological and social stress in the short term. Moreover, in order to prevent the spread and rebound of the pandemic and to block the route of virus transmission, plenty of Chinese are at home with restriction to their outdoor activities, having dinner, traveling, going back to school and returning to work, which inspires negative emotions (fear and anxiety) of the public. With respect to the above, it is necessary to investigate the subhealth status (SHS) of Chinese during the pandemic to understand the prevalence rate and related influential factors, so as to provide a reference for the subsequent nursing health guidance and intervention measures.
SHS is a low-quality status between disease and health in the aspects of the physical, mental and emotional performance of the subjects [3]. World Health Organization (WHO) defines SHS with no organic pathological changes but functional changes “the third state”, also known as “chronic fatigue syndrome” [4, 5]. In accordance with an early global survey, SHS accounted for 75% of the surveyed population, while healthy people only made up a relatively small share of 5% [6]. Relevant studies among China reported greatly varied prevalence of SHS in different occupational and age groups, ranging from about 34.3% to 92.7% [7, 8, 9, 10, 11]. The understanding of the concept of health is deepening in the public with the establishment of physio-psycho-society medical model. Domestic and foreign studies have explored the theory, connotation, concept of prevention and control, prevalence of different populations, influential factors, and intervention measures of SHS. However, there is no SHS survey on people during the pandemic of COVID-19.
With respect to the above, a large-scale convenient sampling in terms of SHS of people living in China was carried out in this study during the pandemic. The objectives of our study is to understand the physical, psychological and social SHS of people and relevant influential factors under the strict control of public health emergencies during such severe pandemic, such as restricting the crowd gathering, stopping work, closing business, suspending classes, strict traffic, sanitation and quarantine supervision. It is expected to provide basis for the prevention and implementation of relevant intervention measures following pandemic stabilization and the resumption of work, production and classes in the later stage.
METHODS
1. Study design
The present study was designed as a cross-sectional survey.
2. Objects of study and research method
On March 6 to 11, 2020, a convenient sampling was performed to investigate SHS of people living in China during the pandemic of COVID-19 through the “Questionnaire Star” (online questionnaire survey platform) [12]. The objects of the study were Chinese who were familiar with the use of mobile terminals and voluntarily participated in the survey. A total of 17,078 SHS questionnaires were collected, involving 32 provinces in China, mainly in Guangdong province. Original data of the questionnaires was exported from the back-end database of “Questionnaire Star” for further screening, with the deletion of questionnaires completed in a short time, questionnaires completed in the same internet protocol (IP) address (only one valid questionnaire retained for those submitted multiple times by an electronic terminal), and questionnaires with the same score selected for all items of the scale. Finally, 16,820 valid questionnaires were included, the effective recovery rate of the questionnaire = (actual number of returned questionnaires - number of invalid questionnaires) / actual number of returned questionnaires, and the effective recovery rate was 98.5%.
3. Study tools
1) General information questionnaire
The questionnaire was designed by the researcher team, including 17 basic data, such as gender, age, height, weight, ethnicity, native place, family residence, marital status, degree of education, political appearance, personal monthly salary, pandemic prevention role and so on.
2) Sub-health status assessment scale
In this study, Sub-health Measurement Scale version 1.0 (SHMS V1.0) was used as a general scale for SHS measurement, and the Cronbach's alpha and Kaiser-Meyer-Olkin of the questionnaire were .92 and .93, respectively [13]. Meanwhile, the reliability and validity of the questionnaire were also retested, which showed that the Cronbach's alpha was .88 and Kaiser-Meyer-Olkin Cronbach's was .95, exhibiting good reliability and validity of the scale. SHS assessment scale consisted of three sub-scales of physiological, psychological and social SHS, with 39 items in total. The international Likert 5-level scoring method was adopted as the scoring standard of the scale. Of the 39 items, forward score was adopted in 24 items, which was the same as the original score; 15 items used reverse score (6 points; the original score), and 4 items of SHS overall assessment were not involved in the score calculation. The sum of the scores of each sub-scale and total scale was the original gross score of sub-scale and total scale, respectively. For further understanding and comparison, the original gross score of the sub-scale and the total scale was converted to the hundred-mark system score according to the formula of dimension conversion score = (dimension original gross score - dimension theoretical minimum score) / (dimension theoretical maximum score - dimension theoretical minimum score) × 100. The theoretical minimum scores of physiological, psychological, social sub-scale, and the total scale of SHS were 70, 60, 45, and 175, respectively, and the theoretical minimum scores were 14, 12, 9, and 35, respectively. According to the grading results based on the conversion score of the total scale, it was classified into three stages: > 79 points as “healthy” status, ≥ 54 points and ≤ 79 points as “SHS”, and < 54 points as “disease” status. The SHS was, again, classified into three as: ≥ 54 and < 60 points as severe, ≥ 60 to < 72 points as moderate, ≥ 72 and ≤ 79 points as mild [13].
4. Statistical analysis
IBM SPSS ver. 22.0 software (IBM Corp., Armonk, NY, USA) was used for data entry and statistical analysis. Frequency, composition ratio and mean ± standard deviation were used for statistical description. Univariate analysis was performed to compare SHS of people with different characteristics by using χ2 test and rank-sum test. The ordinal Logistic regression analysis was used in multivariate analysis. p < .05 meant that the difference was statistically significant.
5. Ethical consideration
This study was approved by the medical ethics committee of the hospital (no. KY-2020-016). It should be noted that due to the severe COVID-19 pandemic in China at the beginning of 2020, the hospital verbally notified the approval of the ethical approval on March 1, 2020, and the approval document was delayed on April 1, 2020. In addition, before submitting the manuscript for review, the manuscript was also submitted to the hospital for re-approval according to hospital regulations.
RESULTS
1. Population characteristics of sub-health status
In this study, 17,078 questionnaires were delivered and 16,820 effective questionnaires were collected. Of the surveyed subjects, SHS was detected in 1,0715 people, 794 people were in disease state, and 5,311 people were in healthy state, accounting for 63.7%, 4.7%, and 31.6%, respectively. Meanwhile, of those detected in SHS, there were 1,141 (6.8%) people with mild SHS, 6,057 (36.0%) with moderate SHS and 3,517 (20.9%) with severe SHS. The average score and standard deviation of the three sub-scales of physiology, psychology and society and the total scale were 81.21 ± 11.23, 68.67 ± 12.71, 67.09 ± 17.48, and 73.28 ± 11.31, respectively. Physiological sub-scale showed the highest score, followed by psychological sub-scale, and the lowest society sub-scale.
2. General information of sub-health status
A total of 16,820 Chinese were enrolled in the study finally, including 6,676 men (39.7%) and 10,144 women (60.3%). The age of the people ranged from 9 to 61 years old (21.4 ± 3.96), of which 40 people (0.2%) aged < 18 years old, 15,687 (93.3%) of between 18~44 years old, 132 (0.8%) of between 45~59 years old, and 6 (0.04%) of > 60 years old. Furthermore, there were 6,105 people (36.3%) living in rural areas, 1,976 (11.7%) in county towns, 2,920 (17.4%) in townships, and 5,819 (34.6%) in urban areas. In terms of the degree of education, there were 29 students (0.2%) in primary school or below, 75 (0.4%) in junior high school, 486 (2.9%) in senior high school or technical secondary school, 16,100 (95.7%) in junior college or undergraduate course, 112 (0.7%) in master's degree, and 18 (0.1%) with doctor's degree or above.
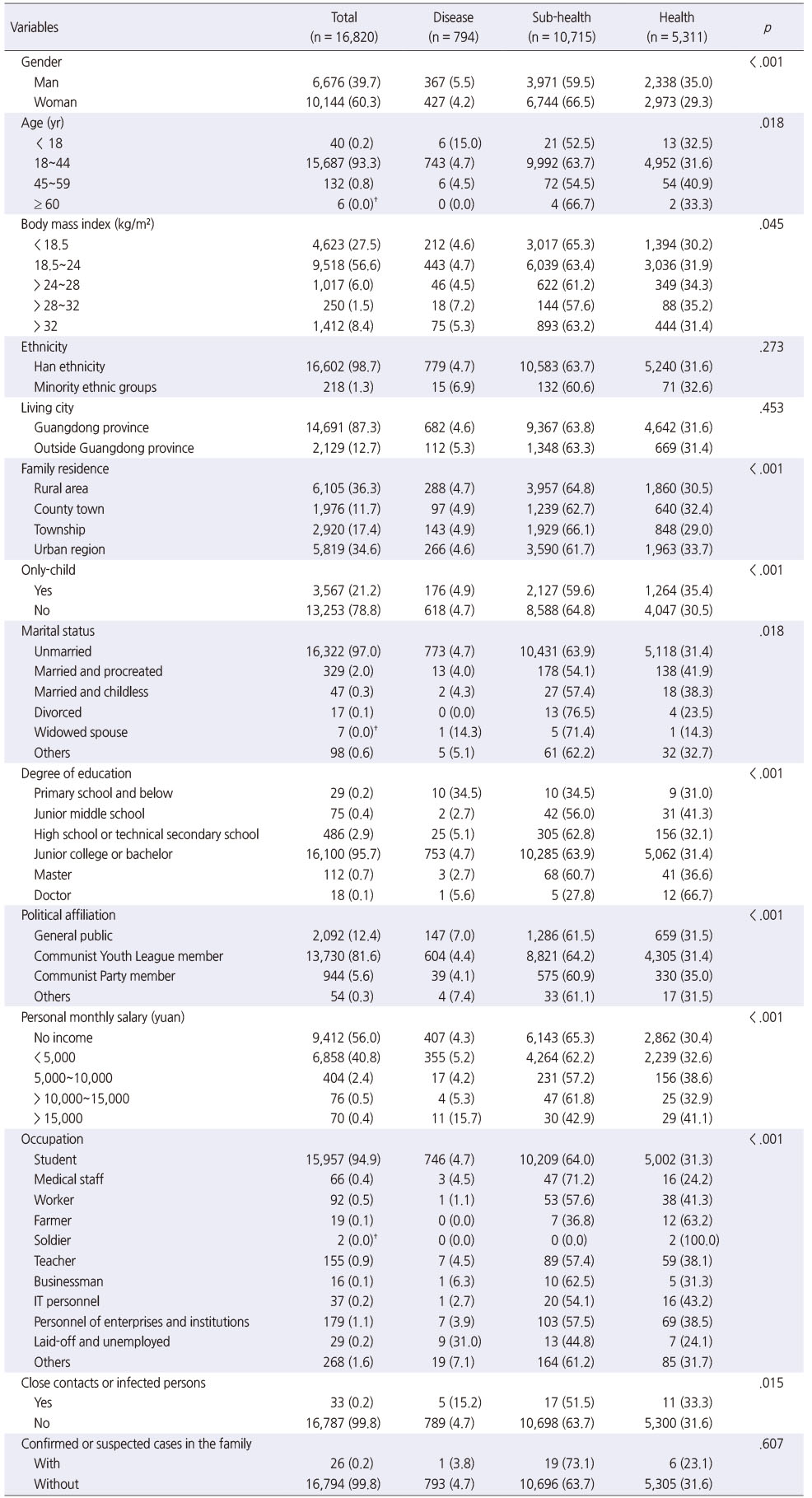
3. Univariate analysis on sub-health status
The results of analysis revealed that there were statistically significant differences in gender, age, body mass index (BMI), family residence, only-child status, marital status, degree of education, political affiliation, personal monthly salary, occupation, close contacts or infected persons. While no statistical significance was detected in ethnicity, living city, and confirmed or suspected cases in the family (Table 1).
Table 1
Disease, Sub-health and Health Status by General Characteristics
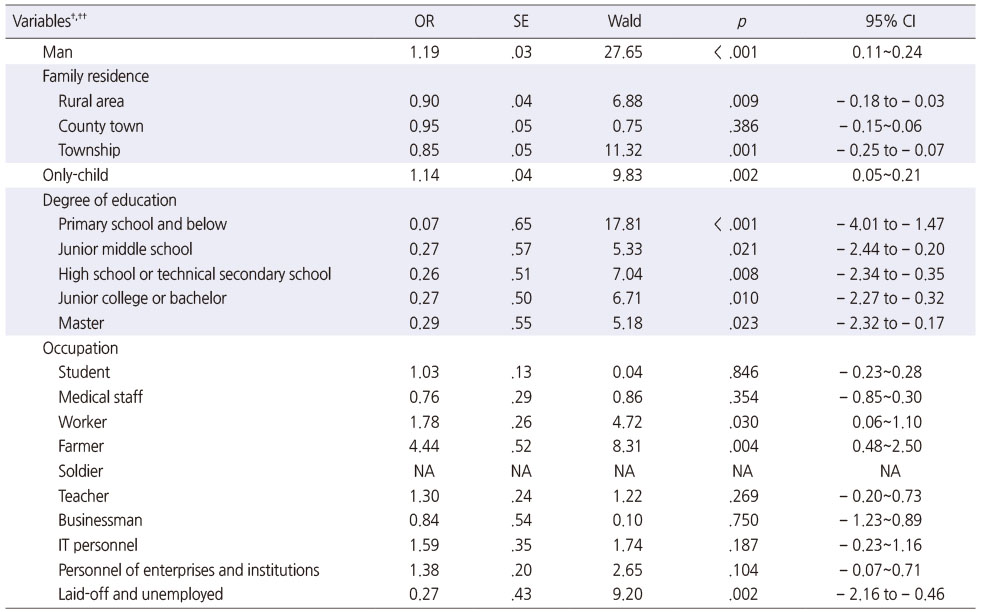
4. Multivariate analysis on sub-health status
The ordinal multi-classification Logistic regression model was constructed by involving gender, age, BMI, ethnicity, living city, family residence, only-child status, marital status, degree of education, political affiliation, personal monthly salary, occupation, close contacts or infected persons, and confirmed or suspected cases in the family as the independent variables. Corresponding results indicated that there was statistical significance in gender, family residence, only-child, degree of education, and occupation (p < .05). Furthermore, age, close contacts or infected persons, confirmed or suspected cases in the family, and other independent variables with statistical significance (p < .05) were included again in the ordinal multi-classification logistic regression model for further analysis. Finally, it was discovered that health status was related to gender, family residence, only-child, degree of education, and occupation (p < .05).
The results of ordinal logistic regression analysis showed that the probability of SHS and disease state in men was 1.19 (95% confidence interval [CI], 0.11~0.24; p < .001) times higher than that in women. The incidence of SHS and disease in Chinese living in rural areas and townships were 0.90 (95% CI, −0.18 to −0.03; p = .009) and 0.85 (95% CI, −0.25 to −0.07; p = .001) times of that in urban areas, respectively. The only-child was 1.14 (95% CI, 0.05~0.21; p = .002) times more likely to have SHS and disease than the non-only-child. The probability of SHS and disease of people with education degree of primary school and below, junior high school, senior high school or technical secondary school, junior college or bachelor degree and master degree was 0.07 (95% CI, −4.01 to −1.47; p < .001), 0.27 (95% CI, −2.44 to −0.20; p = .021), 0.26 (95% CI, −2.34 to −0.35; p = .008), 0.27 (95% CI, −2.27 to −0.32; p = .010) and 0.29 (95% CI, −2.32 to −0.17; p = .023) times of that of doctoral degree respectively. In terms of different occupations, workers and farmers were risk factors for SHS and disease (odds ratio [OR] = 1.78 and 4.44, respectively), while laid-off retiree was a protective factor (OR = 0.27) (Table 2).
Table 2
Multivariate Analysis on Sub-Health Status
DISCUSSION
1. Sub-health status of people during the pandemic of COVID-19
In this study, the prevalence of SHS was 63.7%, with moderate SHS (36.0%) primarily, suggesting a slightly lower prevalence than that of early large-scale international and domestic studies, but still at a high level. WHO's global survey in the early 21st century has shown that about 75% of people are in SHS [6]. Meanwhile, China's Early Survey of 2002 International Symposium on Sub-health Academic Achievements also pointed out that about 70% of the population were in SHS [14]. Fan et al. [15] carried out a large-scale survey on the health status of 8,417 people in 19 universities in 2002, and also found that 69.17% of the respondents were in SHS, and 1/3 of which were in severe SHS. The prevalence rate of SHS in this study decreased compared with the past large-scale study. It may be attributed to researchers' exploration of SHS etiology and symptomatology, renewal of health concept, analysis of relevant influential factors, diagnosis and treatment by using combined traditional Chinese and Western medicine, and implementation of effective intervention measures. In addition, this study was completed in the form of an online survey owing to the influence of the pandemic, showing a selection bias of the objects of study, mainly young people. Maybe relatively healthy participants are online. It is speculated that this is another reason why the prevalence of SHS in this study was not higher than the previous early studies.
Despite a decrease in the prevalence of SHS of people during the pandemic of COVID-19 in this study than that of earlier studies, compared with the recent studies before the outbreak of the pandemic, it is still at a high level, suggesting an unfavorable health status. For example, by surveying 3,431 Chinese in four communities, Liu et al. [16] found that the prevalence rate of SHS was 35.1%. Meanwhile, Zhang et al. [17] conducted a survey by enrolling 5,125 Chinese to investigate the SHS and influential factors in the community, and found that the population with SHS accounted for 31.1% of the total respondents. Compared with the recent studies prior to the outbreak of the pandemic, the higher prevalence of SHS in the present study may be explained by the absence of consensus on the exact cause of SHS, standardized diagnostic standards, perfect prevention and treatment methods, and treatment specificity [18]. On the other hand, outburst of the pandemic also constitutes an important factor for the high prevalence of SHS, which makes the physical and mental health of people in a high stress situation within a short period of time.
In addition, in terms of SHS scale score, physiological sub-scale showed the highest score, followed by psychological sub-scale, and the lowest society sub-scale. In other words, social dimension showed the worst health state, followed by the psychology, and the best the physiology. Some scholars have demonstrated that the outstanding performance of social SHS is the dislocation of roles and maladjustment, while that of psychological SHS is panic, anxiety, emotional disorder and thought disorder of unknown reasons [19]. For current COVID-19 pandemic in China, strict control measures have been taken, such as restricting the crowd gathering, stopping work, closing business, suspending classes, strict traffic, sanitation, and quarantine supervision. It has a great impact on the social activities, working modes as well as learning and living environment of people living in China, resulting in a poor social dimension. Furthermore, COVID-19 has a general susceptibility, rapid spread through respiratory droplets, close contact and aerosols, and can still not be treated effectively; besides, there is a shortage of prevention materials at the early stage of the pandemic [20, 21]. These conditions have caused certain panic and anxiety to the psychology of people, resulting in an unideal psychological health condition. Simultaneously, the government, schools and work units have made rapid response to the pandemic, such as overall arrangement of contactless distribution to ensure the daily needs of Chinese, online teaching with micro-lecture and massive open online courses, and online telecommuting through Internet media. Meanwhile, in order to solve the special psychological problems during the pandemic, the development of online application program was also optimized by the hospital for network consultation and remote psychological intervention. However, there is still a need for continuous social support, psychological counseling, humanistic care, as well as community health, mental health and community nursing related to preventive health care for different groups by relevant units after pandemic stabilization and resumption of work, production and classes in the later stage.
2. Factors related to sub-health status of people during the pandemic of COVID-19
In accordance with the results of multivariate analysis, gender was one of the influential factors during the pandemic of COVID-19. Men were 1.19 times more likely to have SHS and disease status in relative to women, which suggests a higher risk of developing SHS. At present, there is no definite conclusion with respect to the impact of gender on SHS, with inconsistent results. Prior studies indicated that the average score of SHS in men was higher than that in women, that was, the probability of SHS of women was higher than that of men [22, 23]. However, men were also reported to be the risk factor of SHS, and its probability of SHS was higher than that of women [24], which was consistent with the results of this study. As for the high possibility of SHS in men during the COVID-19 pandemic, it is speculated that men are less likely to talk and receive less social and emotional support than women. It may also be explained by the reason that men bear more family and social responsibilities, and the delayed resumption of work and production during the COVID-19 pandemic results in greater economic, physical and mental pressure of men. However, considering that the impact of gender on SHS is still controversial, the results in this study need to be recognized cautiously, and more high-quality and multi-center studies are required for further exploration and verification.
Furthermore, our study also found that people living in rural areas and townships were the protective factors of SHS (OR = 0.90 and 0.85, respectively). In other words, people living in cities have higher risk to develop SHS and disease status, while people living in rural areas or townships are less likely to have SHS and disease status. During the COVID-19 pandemic, people actively abide by the national control measures, avoid crowd gathering activities under the correct guidance of relevant departments, and have home quarantine consciously. However, compared with rural areas and townships, urban regions are featured by scarce land resources that result in high population density and narrow space, which increase the risk of COVID-19 pandemic spreading. In this way, the relative degree of spatial free activities is low in order to prevent the spread of the pandemic. In addition, there is higher market dependence of urban food supply, whereas the rural areas can achieve self-sufficiency to a large extent. The above factors may all have an impact on the physical, physiological and social health of Chinese, leading to the difference in the prevalence of SHS.
Meanwhile, compared with the non-only-child, the only-child was 1.14 times more likely to have SHS and disease than the non-only-child. It indicated a higher possibility of SHS in the only-child group, which was consistent with previous results [25, 26]. It is speculated that the only-child has no brothers and sisters, and control measures such as home quarantine during the pandemic of COVID-19 have an obvious negative impact on their social interaction as well as psychological and emotional support, hence leading to a greater possibility of SHS [27].
In addition, the degree of education was a protective factor of SHS. Compared with population with doctor's degree or above, the population with primary school or below, junior high school, senior high school or technical secondary school, junior college or bachelor's degree and master's degree was less likely to have SHS and disease state. Besides, although the degree of education was a protective factor of SHS, the overall protective effect was weakening from primary school to master's degree. It may be related to the reason that population with higher degree of education and heavier academic tasks may experience more problems related to graduation destination and employment [28]. Moreover, it is supposed that population with higher degree of education need to take on more important social roles and tasks [29]. However, due to the small sample size of doctors surveyed, the results of the effect of the degree of education on the occurrence of SHS need to be interpreted cautiously on the basis of accumulated studies.
Besides, workers and farmers were risk factors of SHS in different occupational groups (OR = 1.78). During the COVID-19 pandemic period, there was a delayed resumption of work and production, and some agricultural products were unsalable, workers and farmers were hence faced with greater economic pressure, which led to a higher possibility of SHS. While the laid-off retirees were the protective factors of sub-health, which may be explained by the reason that such population has basic life guarantee after retirement, and the life pressure is relatively small, hence showing a lower detection rate of SHS.
There are some limitations in this study. Firstly, this study was a cross-sectional study, which can explore the correlation between related factors and SHS, but it is not enough to clarify their causal relationship. Case control study or cohort study can be carried out in future to explore the causal relationship and the closeness between related factors and SHS. Secondly, there existed selection bias in the enrolled subjects in this study, with young people aged 18 to 44 years old as the primary objects of study, and with a low proportion of population aged over 60 years old. It may be that the questionnaire survey in this study was conducted through Internet media during the COVID-19 pandemic period. The elderly are generally not good at using electronic products, resulting in a small sample size of this age range and biased population. Thirdly, despite a relatively larger sample size in this study, SHS exhibits an intimate association with social environment, economic culture, psychology and physique. Different groups have certain specificity and high dispersion. Therefore, more high-quality research is required to explore SHS of different groups. Fourthly, SHS assessment scale used in this study was the authoritative domestic general scale with high reliability and validity. However, connotation of SHS is constantly expanding at present. It is proposed that SHS involves not only physical, psychological and social aspects, but also moral aspect. In this regard, relevant assessment scale shall be improved in the subsequent study in combination with systematic study on SHS.
CONCLUSION
SHS is bi-directional in the sense, which can develop to disease state and turn to health state. And effective intervention plays a positive role in its transformation to health state [30]. Our study suggests a relatively high prevalence rate of SHS during the COVID-19 pandemic; besides, men, only-child, urban people, workers and farmers, and groups with different education degree are the influential factors of SHS. Therefore, relevant departments should pay attention to the impact and influence of COVID-19 pandemic on the people's physical, psychological and social health. Community nursing and health shall emphasize the prevention and intervention of influential factors related to SHS during and after the pandemic, and promote active transformation of people' physical, psychological and social health.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Pan Y & Lu W.
Data curation or/and Analysis: Pan Y & Yan J & Shan M.
Funding acquisition: None.
Investigation: Yan J & Lu W & Shan M.
Project administration or/and Supervision: Pan Y & Lu W.
Resources or/and Software: Yan J.
Validation: Pan Y & Yan J.
Visualization: Pan Y & Yan J.
Writing original draft or/and Review & Editing: Pan Y & Yan J & Lu W.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
References
-
National Health Commission of the People's Republic of China. March 4: Daily briefing on novel coronavirus cases [Internet]. Beijing: National Health Commission of the People's Republic of China; c2020 [cited 2020 May 1].Available from: http://www.nhc.gov.cn/xcs/yqtb/202003/6e02433f7786402d8ea162fb5b80b5a0.shtml.
-
-
Cui WY. In: Investigation on the level of health quotient and subhealth status of undergraduate nursing students in school [master's thesis]. Changchun: Changchun University of Chinese Medicine; 2019. pp. 1-59.
-
-
Fu SL. In: A new perspective on health in the 21st century. Shanghai: Shanghai science and technology education press; 2000. pp. 1-20.
-
-
Lai QY, Chen CJ, Jiao RY, Jing CX, Xie JW. [On the relationship between the sub-health family and work stress of female university teachers in Guangzhou]. Henan Journal of Preventive Medicine 2020;31(3):171–174. [doi: 10.13515/j.cnki.hnjpm.1006-8414.2020.03.003]Chinese.
-
-
Chang H, Bao L, Zhou Q, Chu W. [Level and influencing factors of occupational stress and sub-health of the pharmaceutical marketers in Northeast China]. Journal of Hygiene Research 2020;49(1):70–74. [doi: 10.19813/j.cnki.weishengyanjiu.2020.01.012]Chinese.
-
-
Chou YJ, Meng TC, Zhang HJ. [Research on college students' sub-health status and its influencing factors]. Technology Wind 2019;18:199–202. [doi: 10.13515/j.cnki.hnjpm.1006-8414.2020.03.003]Chinese.
-
-
Liu C, Wang J, Su XL. [Investigation on health status of medical staff in a tertiary hospital]. China Health Standard Management 2019;10(16):10–12. [doi: 10.3969/j.issn.1674-9316.2019.16.005]Chinese.
-
-
Chen JY, Yang LB, Jiang PP, Sun XM, Yu KQ, Li F, et al. [Associations between health-promoting lifestyle and suboptimal health status in Guangdong: A cross sectional study]. Journal of Southern Medical University 2016;36(4):538–543.Chinese.
-
-
Gao H, Wang RQ, Huo JP. [The application of questionnaire “Wen Juan Xing” platform in female climacteric clinic]. Chinese Journal of Family Planning & Gynecotokology 2020;12(6):65–68. [doi: 10.3969/j.issn.1674-4020.2020.06.16]Chinese.
-
-
Xu J, Feng LY, Luo R, Qiu JC, Zhang JH, Zhao XS, et al. [Assessment of the reliability and validity of the Sub-health Measurement Scale Version1.0]. Journal of Southern Medical University 2011;31(1):33–38.Chinese.
-
-
Yan BH, Ding GY. [Advances in the epidemiology of sub-health]. Modern Preventive Medicine 2005;32(5):465–466. 477.Chinese.
-
-
Fan CX, Wang SY, Zhu L, Xiao YJ, Ma SB. [Study on the prevalence and risk factors of “subhealth” status in college and university staff in Guangdong province]. Chinese Journal of Epidemiology 2003;24(9):774–777. [doi: 10.3760/j.issn:0254-6450.2003.09.007]Chinese.
-
-
Liu L, Wang DP, Li YH, Xia YJ. [The logistic regression analysis on influencing factors of sub-health status of community population]. Inner Mongolia Medical Journal 2017;49(6):648–651. [doi: 10.16096/J.cnki.nmgyxzz.2017.49.06.003]Chinese.
-
-
Zhang XH, Zou YL, Feng YM. [Investigation of sub-health status and its influencing factors of community inhabitants]. Guide of China Medicine 2015;13(6):1–4. [doi: 10.15912/j.cnki.gocm.2015.06.001]Chinese.
-
-
Zhu WD, Xu SS, Zhang YL, Wang L, Chen XL. [Research progress of sub-health status and countermeasures]. Nursing Practice and Research 2013;10(13):114–115. [doi: 10.3969/j.issn.1672-9676.2013.13.070]Chinese.
-
-
Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Research 2020;293:113382 [doi: 10.1016/j.psychres.2020.113382]
-
-
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine 2020;382(18):1708–1720. [doi: 10.1056/NEJMoa2002032]
-
-
Zhang XY. In: The study of how Baduanjin intervene the nurses sub-health condition [master's thesis]. Changchun: Changchun University of Chinese Medicine; 2017. pp. 1-45.
-
-
Wang X, He YM. Sub-health status in male and female Chinese populations. Chinese Journal of Public Health 2012;28(1):15–16.
-
-
Wang HQ, Jin Y, Hu XB, Zhang FG, Tang J. Sub-health status of urban people in five occupational groups and its influential factors in Gansu Province. Chinese General Practice 2012;15(10):1167–1169.
-
-
Li JQ, Wu R, Liu Q, Wang H. [Influencing factor related to sub-health in adolescents: A systematic review]. Chinese Journal of Evidence-Based Medicine 2013;13(3):251–258. [doi: 10.7507/1672-2531.20130044]Chinese.
-
-
Zhou X, Xiao YM, Wang C, Zhu J. Sub-health status and its influential factors among university students in Nanchang city. Chinese Journal of Public Health 2012;28(10):1364–1366.
-
-
Wang J, Luo CM, Chen Y, Deng X, Jiang XL, Yang GY. [The study on the characteristics of interpersonal relationship in clinical practice nurses]. Chinese Nursing Management 2017;17(3):355–359.Chinese.
-
-
Li YH, Wang Q, He YX, Zhang TH, Chen J, Liu H, et al. [Investigation and analysis of sub-health status of college students]. World Latest Medicine Information 2019;19(42):312–313. [doi: 10.19613/j.cnki.1671-3141.2019.42.193]Chinese.
-
-
Zhou W, Xu RY, Li Y, Wei L, Yuan JM, Yang T, et al. [Characteristics of mental sub-health state population]. Guangdong Medical Journal 2011;32(10):1326–1330. [doi: 10.3969/j.issn.1001-9448.2011.10.043]Chinese.
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

