Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 48(2); 2018 > Article
- Original Article Symptom Distress and Coping in Young Korean Breast Cancer Survivors: The Mediating Effects of Social Support and Resilience
- Ji Hyun Lee1, Hye Young Kim2,
-
Journal of Korean Academy of Nursing 2018;48(2):241-253.
DOI: https://doi.org/10.4040/jkan.2018.48.2.241
Published online: January 15, 2018
2College of Nursing · Research Institute of Nursing Science, Chonbuk National University, Jeonju,
-
Corresponding author:
Hye Young Kim,
Email: tcellkim@jbnu.ac.kr
Abstract
The purpose of this study was to test the mediating effect of social support and resilience on the relationship between symptom distress and coping in young Korean breast cancer survivors.
A purposive sample of 209 young breast-cancer survivors (mean age 39.9) was recruited for a cross-sectional survey, and the data were collected between June and October 2015. The instruments used in this study were the Memorial Symptom Assessment Scale-Short Form, the Multidimensional Scale of Perceived Social Support, 10-item Connor-Davidson Resilience Scale, and Cancer Coping Questionnaire. The collected data were then analyzed using the SPSS 23.0 and AMOS 23.0 programs.
Symptom distress was found to have a significant indirect effect on coping (beta=-.32,
Based on the results of this study, it can be suggested that in order to enhance young breast cancer survivors’ ability to cope with the distress they commonly feel, intervention methods that strengthen resilience and provide social support should be developed and made available to them.
Published online Apr 30, 2018.
https://doi.org/10.4040/jkan.2018.48.2.241
Symptom Distress and Coping in Young Korean Breast Cancer Survivors: The Mediating Effects of Social Support and Resilience
Abstract
Purpose
The purpose of this study was to test the mediating effect of social support and resilience on the relationship between symptom distress and coping in young Korean breast cancer survivors.
Methods
A purposive sample of 209 young breast-cancer survivors (mean age 39.9) was recruited for a cross-sectional survey, and the data were collected between June and October 2015. The instruments used in this study were the Memorial Symptom Assessment Scale-Short Form, the Multidimensional Scale of Perceived Social Support, 10-item Connor-Davidson Resilience Scale, and Cancer Coping Questionnaire. The collected data were then analyzed using the SPSS 23.0 and AMOS 23.0 programs.
Results
Symptom distress was found to have a significant indirect effect on coping (beta=−.32, p=.002), but not a significant direct effect (beta=.06, p=.577). Additionally, based on the values obtained for the squared multiple correlation, symptom distress, social support, and resilience were found to explain 46.4% of the total variance of coping.
Conclusion
Based on the results of this study, it can be suggested that in order to enhance young breast cancer survivors' ability to cope with the distress they commonly feel, intervention methods that strengthen resilience and provide social support should be developed and made available to them.
INTRODUCTION
Breast cancer is the most common type of cancer afflicting women worldwide, and in Korea, it is the second most prevalent form of cancer affecting females. For Western women, the risk of developing breast cancer increases with age, while in Korea, women in their 40s have the highest incidence of breast cancer. Further, patients below the age of 40 account for approximately 15.0% of the overall number of Korean patients with breast cancer, a percentage that is approximately three times greater than in Western society. Meanwhile, in 2012 it was reported that the mortality of breast cancer in Korea was the lowest among Organization for Economic Cooperation and Development member countries and that the five-year survival rate in the country for early-stage breast cancer with no metastasis was over 97.7% [1].
Young breast cancer survivors, those aged 45 or under [2, 3], show more severe levels of physical disability, anxiety, depressive symptoms, and sleep disorders, along with lower satisfaction in terms of their marriage and a greater fear of cancer recurrence, than older survivors [3]. These symptoms persist for over three years after diagnosis and even influence quality of life [3]. Furthermore, young breast cancer survivors have complained of a fear of premature menopause as a result of their treatment and of suffering from psychological distress due to the change their treatment brought to their role in the family [4]. The symptom distress these patients feel is usually quite severe and it should be noted that it persists after the completion of treatment [4, 5]. Another notable finding in this respect is that, after the completion of treatment, young breast cancer survivors require a higher level of social and psychological support to adapt to their health conditions than older breast cancer survivors do [6]. In this context, it is evident that effective coping strategies for addressing the issues faced by young breast cancer survivors at the individual level are required to improve their quality of life [7].
The Transactional Model of Stress and Coping developed by Lazarus & Folkman [8] emphasizes the process of dynamic interaction between individuals' awareness, cognition, and stress-coping strategies. They also state that stress events are not directly associated with maladjustment reactions and are actually adjusted by individuals' awareness of the stress event and the resources available to them to conduct effective coping [8, 9]. These resources affect the coping process and are assumed to be factors that mediate stress. The range of coping resources can be divided into two categories: social and psychological [8].
In regard to social resources, individuals seek social support when they require information or assistance to respond to or cope with a certain danger [8, 9]. In comparison to individuals with other conditions, breast cancer patients receive relatively more information support from medical personnel and emotional support from their family and friends. Further, those with low social support or a weak social network have been found to be less likely to receive proper help and support [10]. However, it is especially difficult for young breast cancer patients to find others experiencing the same situation, and this commonly causes them to feel isolated. By providing such patients with social support, such as informational and emotional support, and wider opportunities for information sharing, this greater level of social interaction, along with improved coping strategies, can enhance their quality of life [11].
Returning to the abovementioned categorization of coping resources, it should be noted that in regard to psychological resources, resilience is important. Resilience is categorized as positive belief, and it concerns one's ability to overcome emotional hardship when faced with challenges and to quickly and efficiently recover from negative experiences [12, 13]. By enhancing resilience, young breast cancer survivors can alleviate the negative impacts of the various physical, psychological, and social issues they experience after the completion of treatment, and it can also help them establish positive coping behaviors. Therefore, it is clearly important to predict the variables associated with coping resources for young breast cancer survivors and to comprehensively examine their influence, as these resources can have an impact on the success of these patients' coping.
To perform this, we reviewed previous literature in an attempt to gain an understanding of the relationship between symptom distress (perceived stress) and coping in young breast cancer survivors, focusing on studies that have applied Lazarus & Folkman's theory [8]. However, many studies merely reported associations between coping resources or their fragmentary effects [14, 15, 16]. Moreover, in a study on the indirect effects of coping resources (social support and optimism) on the relationship between symptom experience and coping in patients with early breast cancer [17], structural correlation between individual variables were identified. However, despite the fact that the severity of symptoms experienced varies in different age groups (young or old) [2, 3] and the level of coping resources required by the subjects also varies [11], the study identified the causal relationships without considering age groups, which presents the limitation of not being able to identify the relationships between perceived stress, coping resources, and coping in young breast cancer survivors.
Considering the above, this study was conducted with the purpose of identifying the structural correlation between factors that influence the coping process of young breast cancer survivors. To achieve this, these influential factors were applied to the stress-coping theory. Consequently, in order to determine the effectiveness and impact of appropriate channels, a model, which could contribute to could contribute to the identification of practical and effective nursing interventions to improve coping strategies for young breast cancer survivors, was established and verified.
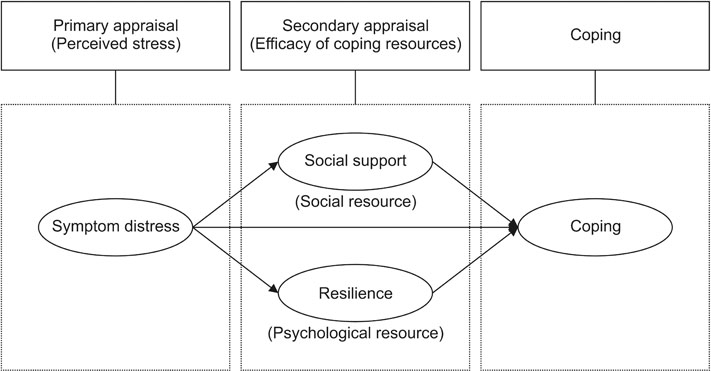
1. Theoretical framework and hypothetical model
The theoretical framework of this study is Lazarus and Folkman's stress-coping theory [8] featuring the key concepts of stress, appraisal, and coping. When an individual is diagnosed with breast cancer, their cognitive appraisal of the stress event can generate stress. They then evaluate the stress through primary appraisal, which determines if the event or situation poses a threat to their physical and/or psychological health, and, once stress is initially generated, symptom distress can persist, even after diagnosis and the completion of the overall treatment process [3, 4, 5]. It is for this reason that symptom distress has been established as the primary appraisal in this study.
Secondary appraisal relates to when coping resources available to patients are identified and applied to alleviate the degree of stress. As young breast cancer survivors generally find it extremely difficult to make decisions concerning their health [13], they must make use of resources provided from the outside, such as necessary support, information, and feedback [18]. Considering this, in our study social support was set as one of the coping resources used during secondary appraisal. Furthermore, resilience, which is positive belief and is required to overcome uncertainty about and fear of cancer [8, 12, 13, 18], was also set as one of the coping resources used during the secondary appraisals of young breast cancer survivors.
Based on Lazarus & Folkman's theory [8], a path was established in which symptom distress affected social support [16, 19] and resilience [13, 16], and another path was established in which symptom distress affected coping [16]. In addition, further paths were established in which social support [17] and resilience affected coping [16] (Figure 1).
Figure 1
Lazarus & Folkman's stress-coping theory and hypothetical model.
METHODS
1. Study design
Based on a structural model, this study was conducted to suggest a hypothetical model for coping through consideration of the theoretical framework of Lazarus & Folkman's theory [8], previous studies, and literature.
2. Study subjects and data collection
The pilot study was conducted from June 9 to July 14, 2015, with the participation of 20 young breast cancer survivors who met the inclusion criteria of the main study in order to identify any potential difficulties in the translation, such as words that are complicated or difficult to understand. These participants were recruited from C National University H Hospital's cancer center in J city. Prior to conducting the pilot study, five nursing professors, one doctor from a breast-endocrine surgery department, and one nurse engaged in a review of the content validity of the measuring instruments and items [20]. The average time taken by the pilot study respondents to complete the self-reported questionnaire was approximately 17 minutes.
The data collection period for the main study extended from July 15 until October 30, 2015, and data were collected from the outpatient breast cancer center at W University Hospital and C National University H Hospital in Korea. Three trained interviewers collected data, and the inter-evaluator reliability was .90. The specifics of the subject inclusion criteria were as follows: females aged between 20 and 45; diagnosed with stage 1, 2, or 3 primary breast cancer; at least six months post treatment (surgery, chemotherapy, radiotherapy); capable of understanding the study purpose and responding to the survey; and who provided written consent for participation. The exclusion criteria were as follows: subjects with recurrence of breast cancer, and concomitant mental disease or other concomitant chronic diseases such as cardiac, renal, and pulmonary disease.
Among the 3,892 patients who visited the two hospitals during the data collection period, 330 met the inclusion criteria and were prospectively listed as study subjects. However, only 220 participated in the survey. Of the 220 respondents, six did not complete the survey owing to personal circumstances, while five were found to have given insincere responses and were excluded. Thus, a total of 209 survey responses were used for the analysis in this study. There was no absolute standard for determining the sample size of the structural equation model. However, it was determined based on Hair et al.'s argument [21] that if the data sample size is 150~200, to satisfy the multivariate normality, it is appropriate to use maximum likelihood estimation, which is a prediction method frequently used in structural equation modeling.
3. Ethical considerations
Approval was obtained from the Institutional Review Board(IRB) of both W University Hospital (IRB No. WKUH 201506-HR-045) and C National University H Hospital (IRB No. CNUHH-2015-090). After reading the informed consent form and giving written consent, submission of the completed questionnaires implied that participants consented to participate in this study.
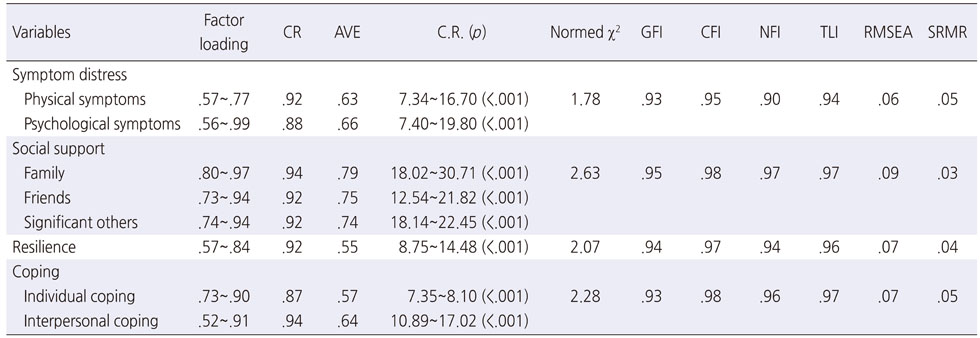
4. Study instruments
In this study, all tools were used after approval from the original developer via email. The measuring tool for symptom distress was used after approval of Korean translation. And the measuring tools for social support, coping, and resilience were used after approval from the developer of the Korean version. All measuring tools were subject to confirmatory factor analysis (CFA), which was conducted in order to verify their construct validity. For convergent validity, which verifies how well a construct is measured by observed variables, the standards were as follows: a minimum of .50 standardized factor loadings from latent variable to observed variable; .70 or greater construct reliability (CR); .50 or greater average variance extracted (AVE); >1.965 critical ratio (C.R.); and p<.05 or greater [22]. Further, to verify reliability, Cronbach's alpha was calculated. Normed χ2 was set as 3 or lower, while the goodness-of-fit index (GFI), comparative fit index (CFI), normed fit index (NFI), and Tucker-Lewis index (TLI) were all .90 or greater. Meanwhile, the root mean square error of approximation (RMSEA) was .08 or lower and the standardized root mean residual (SRMR) was .05 or lower [21, 22].
1) Symptom distress
Symptom distress was measured by the Memorial Symptom Assessment Scale-Short Form (MSAS-SF), which was developed by Chang et al. [23] using cultural adaptation processes suggested by the World Health Organization [24]. To facilitate its use in our study, a bilingual nursing professor translated the MSAS-SF from English to Korean and produced a preliminary draft. The draft then underwent a process of convergence by two nursing professors, which involved discussions regarding differences between it and the original. The translated draft was then back-translated into English by an English expert, and a subsequent comparison of the original and back-translated MSAS-SF yielded no substantial differences. The validity of each item was designed to be assessed on a scale ranging from 4 (strongly agree) to 1 (strongly disagree), after which the content validity index (CVI) of each item was calculated. As a result, the CVI of all 30 items was above 80.0% [20].
The tool consisted of a total of 34 items: 28 items relating to physical symptom distress, two additional items for which respondents were asked to provide subjective essay-type answers concerning other physical distress symptoms, and four items relating to psychological symptom distress. These contents were verified by a group of experts in terms of validity, and a total of 32 items were included in the final tool, with the two items concerning essay-type answers being excluded. Next, a score ranging from 0 (not painful at all) to 4 (very painful) on a five-point Likert scale was allocated to each item, meaning the total score for the questionnaire could range between 0 and 128. Considering the design of the questionnaire, a higher score represented more severe physical and psychological symptom distress. Finally, at the time of development, Cronbach's alpha in regard to the internal reliability of the tool was .82 for physical symptom distress and .76 for psychological symptom distress [23].
The CFA result for the measuring tool used to test symptom distress showed that it did not satisfy the criteria, as five items (4, 13, 15, 22, and 24) were confirmed to have a factor loading of .50 or lower. After these five items had been removed, CFA was conducted once again, and the result was as follows: factor loading of .56~.99 for symptom distress measuring tools, CR of .92 for physical symptom distress, CR of .88 for psychological symptom distress, AVE of .63 for physical symptom distress, AVE of .66 for psychological symptom distress, and C.R. of 7.34~19.80 (p<.001). The model suitability was found to be of an adequate level, with normed χ2=1.78 GFI=.93, CFI=.95, NFI=.90, TLI=.94, RMSEA=.06, and SRMR=.05. Further, Cronbach's alpha for internal reliability was .90 for physical symptom distress and .83 for psychological symptom distress (Table 1).
Table 1
Confirmatory Factor Analysis of the Research Measurements
2) Social support
Social support was measured by the Multidimensional Scale of Perceived Social Support (MSPSS), which was developed by Zimet et al. [25] and translated by Shin & Lee [26]. This tool consisted of a total of 12 items, with 4 items relating to family support, friends' support, and significant others' support, respectively. Each item was evaluated using a seven-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), giving a total score of between 12 and 84. The construction of the tool meant that higher scores represented higher awareness of social support. At the time of development, Cronbach's alpha concerning the internal reliability of the tool was .91 for family support, .87 for friends' support, and .85 for significant others' support [25].
Meanwhile, the CFA result for the measuring tool for social support was as follows: factor loading of .73~.97; CR of .94 for family support, .92 for friends' support, and .92 for significant others' support; AVE of .79 for family support, .75 for friends' support, and .74 for significant others' support; and C.R. of 12.54~30.71 (p<.001). The model suitability was of adequate level, with normed χ2=2.63 GFI=.95, CFI=.98, NFI=.97, TLI=.97, RMSEA=.09, and SRMR=.03. Further, Cronbach's alpha for internal reliability was .94 for family support, .91 for friends' support, and .93 for significant others' support (Table 1).
3) Resilience
Resilience was measured by the Korean version of the Connor-Davidson Resilience Scale (CD-RISC), which was developed by Connor & Davidson [27]. This tool featured a subsection consisting of 10 items, and each item was evaluated using a five-point Likert scale ranging from 1 (never) to 5 (always), giving a total score of between 10 and 50; the higher the score, the higher the participant's resilience. At the time of development, Cronbach's alpha concerning the internal reliability of the tool was found to be .85 [27].
Further, the CFA result of the measuring tool for resilience was as follows: factor loading of .57~.84; CR of .92; AVE of .55; and C.R. of 8.75~14.48 (p<.001). Additionally, the model suitability was of adequate level, with normed χ2=2.07 GFI=.94, CFI=.97, NFI=.94, TLI=.96, RMSEA=.07, and SRMR=.04. Cronbach's alpha for internal reliability was .92 (Table 1).
4) Coping
Coping was measured by the Korean Form of Cancer Coping Questionnaire (K-CCQ), which was originally developed by Moorey et al. [28], with the Korean form being validated by Kim et al. [29]. This tool consisted of a total of 23 items, with 14 items relating to individual coping and nine items concerning interpersonal coping. Each item was evaluated using a four-point Likert scale ranging from 1 (never) to 4 (very often), with a total score ranging from 23 to 92; the higher the score, the better the subject was coping. At the time of development, Cronbach's alpha concerning the internal reliability of the tool was found to be .87 for individual coping and .80 for interpersonal coping [28].
In the first CFA of the study, six items (1, 2, 3, 4, 6, and 7) were found to have a factor loading of .50 or lower and, consequently, did not satisfy the structural concept; hence, they were removed. The second CFA result for the measuring tool for coping was as follows: factor loading of .52~.91; individual coping of .87; interpersonal coping of .94; AVE of .57 for individual coping and .64 for interpersonal coping; and C.R. of 7.35~17.02 (p<.001). The model suitability was of an adequate level, with normed χ2=2.28 GFI=.93, CFI=.98, NFI=.96, TLI=.97, RMSEA=.07, and SRMR=.05. Cronbach's alpha for internal reliability was .87 for individual coping and .95 for interpersonal coping (Table 1).
5. Data analysis method
The collected data were analyzed using SPSS 23.0 for Windows and IBM SPSS AMOS 23.0. The general and disease-related characteristics of the participants were subject to descriptive statistics, and Cronbach's alpha values were calculated to verify the reliability of the measuring tools. Further, skewness and kurtosis were measured to verify the normality of samples, and the multicollinearity of the sample was analyzed using tolerance, variance inflation factor (VIF), and Pearson's correlation coefficient. Additionally, CFA was conducted to confirm the validity of the latent variable, while factor loading, CR, AVE, and C.R. were calculated for each subfactor that constituted an individual factor. Absolute fix indices including χ2(p), normed χ2, GFI, CFI, NFI, TLI, RMSEA, and SRMR were calculated to assess the suitability of the data for the hypothetical model. To verify the significance of direct, indirect, and total effects between influential factors concerning coping, bootstrapping was used, and the number of bootbootstrap samples was set to 2,000. When there were multiple mediating variables in a multiple mediator model, phantom variables were used to verify the difference between the two indirect effects related to specific variables [22]. Finally, when establishing the model, in cases where there was a single observed variable in the structural equation in the study, the factor loading was set to 1 and measurement error variance was set to 0.
RESULTS
1. General and disease-related characteristics of subjects
The study population consisted of 209 subjects between 21 and 44 years, with the highest number of subjects found in the 40~44 age group (n=134, 64.1%). The mean age was 39.90±4.12 years. A total of 169 subjects (80.9%) had spouses, while the number of children appeared in the order of two children (n=107, 51.2%), no child (n=44, 21.1%), one child (n=37, 17.7%), and more than three children (n=21, 10.0%). A total of 97 subjects (46.4%) were employed, while 122 subjects (58.4%) had a religion, with Christianity (n=56, 26.8%) being the most common. Meanwhile, monthly household income appeared in the order of ≥3 million won (n=129, 61.7%), 2~2.99 million won (n=41, 19.6%), and <2 million won (n=39, 18.7%).
With respect to the disease-related characteristics of the subjects, the most common cancer stage was stage 1 (n=102, 48.8%), followed by stage 2 (n=81, 38.8%) and stage 3 (n=26, 12.4%). For duration since cancer diagnosis, 153 subjects (73.2%) reported 13~59 months and 33 subjects (15.8%) reported <12 months. For age at the time of diagnosis, the most common response was 30~39 years (n=110, 52.6%), followed by 4 0~44 years (n=85, 40.7%) and <29 years (n=14, 6.7%). The most common surgical method was breast conserving surgery (n=137, 65.6%), followed by mastectomy (n=51, 24.4%) and mastectomy with reconstruction (n=21, 10.0%). The most common treatment method was combined chemotherapy and radiotherapy after surgery (n=112, 53.6%), followed by radiotherapy after surgery (n=54, 25.8%), surgery only (n=27, 12.9%), and chemotherapy after surgery (n=16, 7.7%). A total of 104 subjects (49.8%) reported that they received hormonal therapy, while 195 reported (93.3%) that they did not receive any immunotherapy.
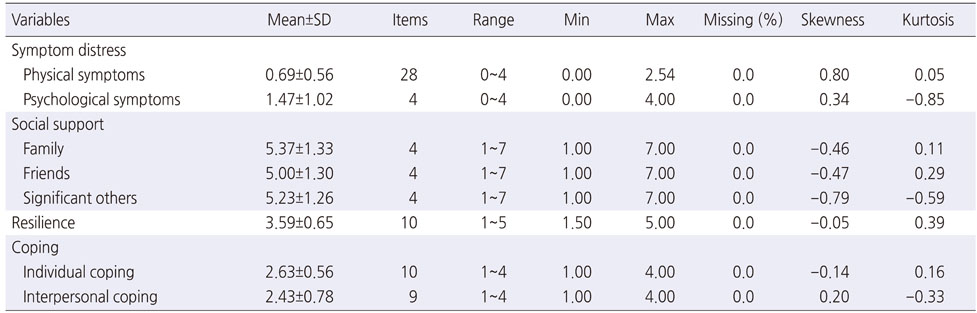
2. Descriptive statistics and normality verification of study variables
According to the descriptive statistics of the study variables, the scores of the two subfactors of symptom distress were as follows: with a grade point average of four (full score), 0.69±0.56 for physical symptom distress, and 1.47±1.02 for psychological symptom distress. Next, for perceived social support, the scores of the subfactors were as follows: with a grade point average of seven (full score), 5.37±1.33 for family support, 5.00±1.30 for friends' support, and 5.23±1.26 for significant other's support. The score for resilience was 3.59±0.65 with a grade point average of five (full score), while among the subfactors for coping, the score for individual coping was 2.63±0.56 and interpersonal coping was 2.43±0.78, out of a full score of four points.
In all observed variables in the study, the absolute value of skewness ranged from 0.05 to 0.80 and the absolute value of kurtosis ranged from 0.05 to 0.85, showing that they did not deviate from the hypothesis of normal distribution (Table 2).
Table 2
Descriptive Statistics of the Research Variables (N=209)
3. Verification of multi-collinearity between variables
The verification result showed a tolerance of .74~.89, a VIF of 1.13~1.36, and that the range of significant correlation values between variables was −.33~.72, confirming suitable multi-collinearity between the observed variables.
4. Measurement model analysis
The measurement model suitability was confirmed to be adequate and to have adequately reflected the concept, with χ2=37.03 (p<.001), normed χ2=2.47, GFI=.98, CFI=.96, NFI=.94, TLI=.92, RMSEA=.08, and SRMR=.05. In the analysis of the measurement model, the standardized coefficients of latent and observed variables by pathway were confirmed to be .61~.90, and all were found to be statistically significant at the level of p<.001.
5. Verification of hypothetical model's suitability
The overall suitability of the hypothetical model established in the study was χ2=29.45 (p<.001), normed χ2χ2=1.96, GFI=.97, CFI=.97, NFI=.95, TLI=.95, RMSEA=.07, and SRMR=.07.
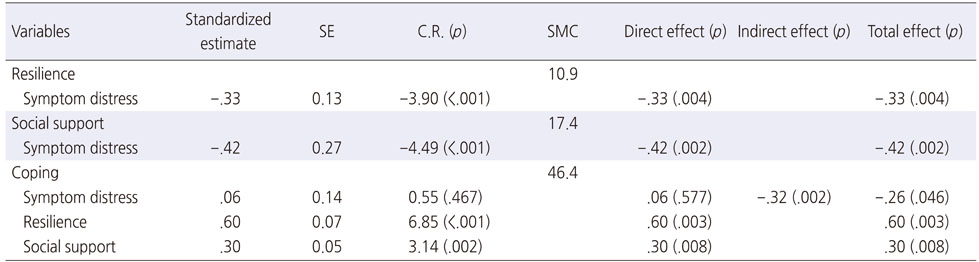
6. Parameter estimation of the final model
Symptom distress showed statistically significant pathways for resilience (β=−.33, p=.004) and social support (β=−.42, p=.002), with the explanatory power of each pathway set as 10.9% and 17.4%, respectively. Further, coping showed significant pathways for social support (β=.30, p=.008) and resilience (β=.60, p=.003), but no significant pathway was identified with symptom distress. The explanatory power of these variables was 46.4% (Table 3).
Table 3
Parameter Statistics for the Final Model and the Direct, Indirect, and Total Effect of the Final Model (N=209)
7. Effects analysis of the final model
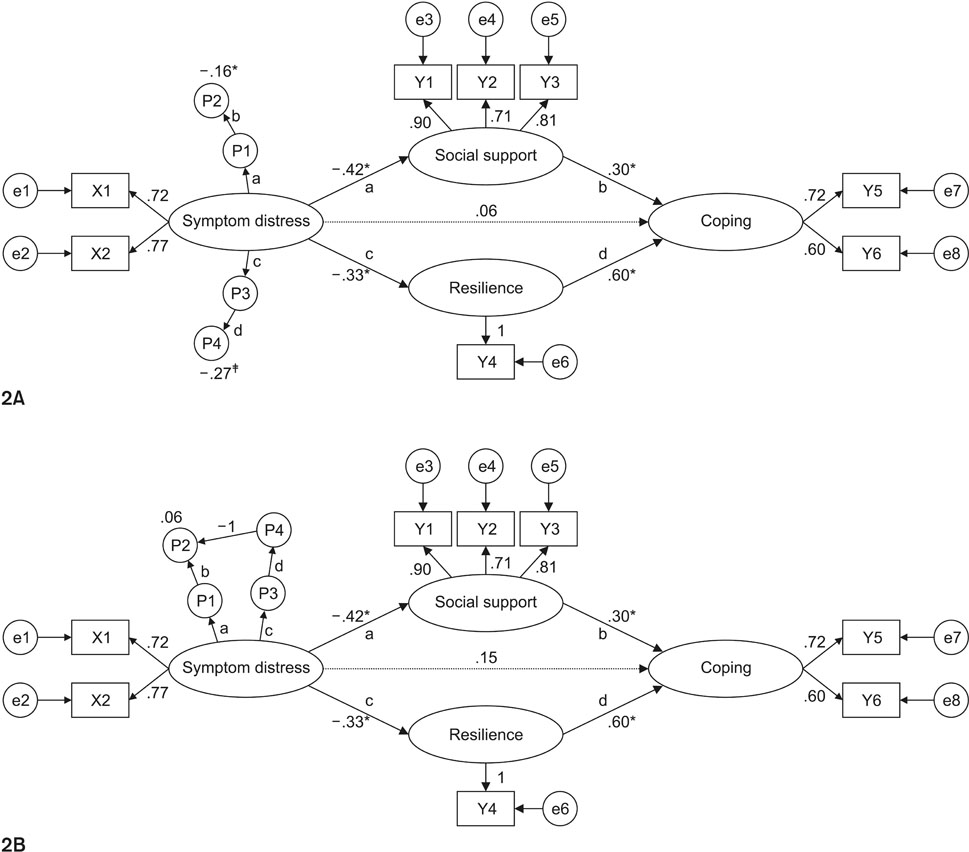
The direct, indirect, and total effects of the exogenous variables of the hypothetical model on endogenous variables were analyzed and the results showed that symptom distress had significant direct and total effects on social support and resilience. Meanwhile, for coping, social support and resilience had a significant direct effect, and the total effect was also statistically significant. Further, symptom distress had a significant indirect effect (β=−.32, p=.002) on coping through social support and resilience (Table 3). In regard to the multiple mediator model, in cases where multiple indirect effects were present, phantom variables were used to estimate specific indirect effects related to certain variables; the pathway of “symptom distress”→“social support”→“coping” was expressed as the phantom variable of “P1”→“P2” and the pathway of “symptom distress”→“resilience”→“coping” was expressed as the phantom variable of “P3”→“P4.” The indirect effect P2, which had effects on the pathway of “symptom distress”→“social support”→“coping,” was −.16 (p=.009), and the indirect effect P4, which had effects on the pathway of “symptom distress”→“resilience”→“coping,” was −.27 (p=.001), indicating it to be significant. However, the difference in the scales between the two indirect effects (P4 and P2) was observed to be statistically insignificant (p=.534) (Figure 2).
Figure 2
Differential verification after analysis of multiple mediator model using phantom variable. (A) Specific indirect effects in multi-mediation model, including phantom variables. (B) Verification of the difference between two indirect effects in a multi-mediation model involving phantom variables.
DISCUSSION
Young breast cancer survivors more frequently complain of psychological distress, depressive symptoms, fatigue, and issues relating to attention and sexual function than their older counterparts, and multiple studies have reported that such symptom distress may play a critical role in undermining such patients' health-related quality of life [3]. Thus, efficient use of coping resources (social support and resilience) in stress situations [8], such as when experiencing symptom distress, would strengthen young breast cancer survivors' coping capabilities, and ultimately have beneficial effects on their mental health and psychosocial adjustment. Considering this, this study investigated the direct and indirect effects of influential factors on the coping process of young breast cancer survivors by applying Lazarus & Folkman's stress-coping theory [8].
Our model suitability test showed adequate results, indicating that it was suitable for predicting the coping processes of such survivors. In this study, young breast cancer survivors' symptom distress, social support, and resilience were found to explain 46.4% of the total variance of coping. Symptom distress was found to have no direct effects on coping but was confirmed to have indirect effects through social support and resilience as complete mediating variables, with no difference in the level of indirect effects. As the physical and psychological symptom distress of young breast cancer survivors can only be alleviated through the application of coping resources relating to social support and resilience, our results confirm that mediation of such coping resources can have beneficial effects on the coping of these survivors.
Applying Lazarus & Folkman's stress-coping theory [8], this study established a body of nursing knowledge concerning the coping of young breast-cancer survivors. This was achieved by forming a basis for describing the causal pathway of such cancer survivors' coping processes. According to Lazarus & Folkman [8], coping resources can be considered mediating factors for stress and coping strategies, and they are also especially important for perceiving difficult situations in a positive manner. The results of this study show that the indirect effects of social support (coping resources provided from the outside) and resilience (individuals' psychological coping resources) on symptom distress (perceived stress) and coping are statistically significant; therefore, this study has empirically verified the concept of Lazarus and Folkman's theory [8].
In this study, the direct effects of social support and resilience on the symptom distress of young breast cancer survivors were confirmed and, consistent with the findings of previous studies [13, 16, 19], we substantiated the effects perceived stress has on coping resources [8]. Even after the completion of their cancer treatment, young breast cancer survivors still experience stress events—symptom distress—more frequently than do older survivors [3, 4, 5]. This suggests that, in order to reduce various forms of physical and mental symptom distress, including premature menopause and fear of experiencing various physical symptoms such as sexual dysfunction, poor body image, and cancer relapse [3], and to enhance social support and resilience in young breast cancer survivors, measures such as systematic inspections for symptom distress, development of guidelines for symptom distress management, development and operation of symptom distress alleviation programs, provision of information and education on regularly occurring health issues, and telephone counseling should be implemented.
The symptom distress scores in this study were generally low, which is inconsistent with the findings of a previous study in which young breast cancer survivors showed higher symptom distress than old survivors [3]. This may be attributable to the fact that the subjects of the present study were breast cancer survivors who had completed their treatment over six months previously. Another possible reason for this finding is that the symptom distress instrument used in this study had originally been developed for all cancer patients [23], and not strictly for breast cancer patients, which means that it is possible that some of the symptoms experienced by breast cancer patients were not included. Thus, additional studies should be conducted using instruments that thoroughly reflect the symptoms of young breast cancer survivors.
Social support, a coping resource, was confirmed to have direct effects on the coping of young breast cancer survivors. This study supports the result of another study [19], which suggested that a higher coping score means that the respondent receives greater social support. This study confirmed that social support is a useful coping resource that can strengthen individuals' problem-solving abilities and enable them to effectively cope with stress situations; further, it showed that support from family, friends, and significant others are key factors that affect coping in young breast cancer survivors. Considering that the survival rate of young breast cancer patients is higher among those who have heightened social support post-cancer diagnosis than among those who maintain the same amount of contact with friends and family as before breast cancer treatment [11], it is clearly highly important to develop individualized intervention strategies for such patients, who are in more serious need of psychosocial help than are older breast cancer survivors, with the aim of increasing social support. This should be performed with the goal of transforming various difficult situations into more positive ones. Further, appropriate social support should be provided for young breast cancer survivors, who will generally be required to visit outpatient clinics for the foreseeable future in order to receive follow-up care, by investigating the kind of resource network each patient requires. For individuals with good support from family and friends, the emotional support they receive from these areas should be reinforced, and medical professionals should also provide assistance in terms of disease-related information and decision making. Moreover, individuals who perceive themselves to have low support from friends and family should be provided with a comprehensive social support program that comprises systems for both continuous follow-up care from medical personnel and for the acquiring of assistance from community social organizations. In particular, it can be supposed that developing a system that provides young breast cancer survivors with the required social support through their social networks would also provide them with the social resources they require.
However, the results of this study were different from the results of Kim & So [17], which reported that social support does not mediate the relationship between symptom experience and coping in early breast cancer patients. Young breast cancer patients (<50 years old) are more likely than older breast cancer patients (≥50 years old) to want emotional support from professional counselors, while also showing higher demand for appropriate social support services [6, 30]. In the study by Kim & So [17], the study population consisted of a relatively high percentage—approximately 70.0%—of older women aged ≥50 years, and as a result, social support may not have affected coping.
It should also be noted that social support scores were generally high in this study, which is inconsistent with a previous study's finding that young breast cancer survivors have higher demands regarding social support than do old breast cancer survivors [5]; this latter finding is similar to another finding: that young women with breast cancer who actively participate in breast cancer treatment have higher social support [11]. One reason for the difference between these findings and our own may be that the participants of this study were breast cancer survivors who had completed aggressive treatment at least six months previously. Further, the social support instrument used in this study measures individuals' perceived support from family, friends, and significant others, which suggests that South Korea's family-centered culture and breast cancer support group activities may have affected the outcomes. Thus, further studies to clarify this point are required.
Resilience, which is another coping resource, was shown to have direct effects on coping, and this result was consistent with that of a previous study that demonstrated a positive correlation between resilience and coping [17]. Considering this and our own results, we surmise that developing and implementing resilience-enhancing nursing intervention programs for young breast cancer survivors improves their coping capabilities, thereby improving their adaptation to distress and psychosocial problems that would negatively affect them for the foreseeable future.
The present study confirmed the direct, indirect, and total effects of variables, along with identifying the correlations between them, through the application of covariance structure analysis, which was conducted to verify the predictive model created concerning the coping of young breast cancer survivors. Further, the complete mediating effects of social support and resilience were verified by identifying the pathway from symptom distress to coping. It is also recommended that the effect of mediation strategies be maximized, as this can facilitate the development of various programs that can be applied in cancer nursing practice, as well as more effective nursing practices. In particular, a 12-week stress management and resilience training (SMART) program has been reported to significantly improve the resilience, perceived stress, and quality of life of breast cancer patients [31]; moreover, the implementation of a four-module breast cancer e-support program has also been reported to be effective in enhancing individuals' symptom distress, social support, depression and anxiety, and quality of life [32]. Hence, the SMART and breast cancer e-support programs may be effective in relieving symptom distress and enhancing social support and resilience in young breast cancer patients, thereby helping them implement effective coping skills.
Despite the abovementioned findings, this study has the following limitations. First, as we established a structural model based on data collected from participants who satisfied specific criteria, it may not be possible to extend the results of the study to all young breast cancer survivors. In addition, this study has a second limitation that it has not been able to establish a structural model, including all mediating factors that may influence the coping of young breast cancer survivors. Finally, this was only a cross-sectional study. Thus, longitudinal research is recommended to confirm the causal path of this study's findings. Thus, longitudinal research is recommended to confirm the causal path of this study's findings.
CONCLUSION
In this study, the mediating effect of coping resources on the relationship between perceived stress and coping was identified. Such findings demonstrate that to improve the coping capacity of young breast cancer survivors suffering from severe physical and psychological symptom distress, there is a need for social resources that provide supportive care, helping build health together with family, friends, and health professionals, as well as psychological resources that allow for positive views about the disease. In other words, providing individually customized nursing intervention to young breast cancer survivors through continued assessment of their resilience and social support can contribute to improving coping ability and the health outcomes of the subjects.
This manuscript is a revision of the first author's doctoral dissertation from Chonbuk National University.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
References
-
Korean Breast Cancer Society. Breast cancer facts & figures 2016 [Internet]. Seoul: Korean Breast Cancer Society; c2017 [cited 2017 Apr 15].Available from: http://www.kbcs.or.kr./sub02/sub04.html.
-
-
Khalili N, Farajzadegan Z, Mokarian F, Bahrami F. Coping strategies, quality of life and pain in women with breast cancer. Iran J Nurs Midwifery Res 2013;18(2):105–111.
-
-
Lazarus RS, Folkman S. In: Kim JH, editor. Stress, appraisal, and coping. 1st Engl. Ed. Seoul: DaeKwang Moon Hwa Sa Publishing Co.; 1991. pp. 46-206.
-
-
Jung DW. In: Psychosocial stress. Paju: Korean Studies Information; 2010. pp. 25-163..
-
-
Fradelos EC, Papathanasiou IV, Veneti A, Daglas A, Christodoulou E, Zyga S, et al. Psychological distress and resilience in women diagnosed with breast cancer in Greece. Asian Pac J Cancer Prev 2017;18(9):2545–2550. [doi: 10.22034/APJCP.2017.18.9.2545]
-
-
Yoo GJ, Sudhakar A, Le MN, Levine EG. Exploring coping strategies among young Asian American women breast cancer survivors. J Cancer Educ 2015;32(1):43–50. [doi: 10.1007/s13187-015-0917-x]
-
-
Kang JY, Suh EE. The influence of stress, spousal support, and resilience on the ways of coping among women with breast cancer. Asian Oncol Nurs 2015;15(1):1–8. [doi: 10.5388/aon.2015.15.1.1]
-
-
Moyer A, Salovey P. Predictors of social support and psychological distress in women with breast cancer. Korean J Health Psychol 1999;4(2):177–191. [doi: 10.1177/135910539900400212]
-
-
Hair JF, Black WC, Babin BJ, Anderson RE. In: Multivariate data analysis. 7th ed. Upper Saddle River (NJ): Pearson Prentice Hall; 2010. pp. 578-581.
-
-
Bae BR. In: Structural equation modeling with Amos 21: Principles and practice. Seoul: Chungram publishing Co.; 2014. pp. 322-447.
-
-
World Health Organization. Process of translation and adaptation of instruments [Internet]. Geneva: World Health Organization; c2015 [cited 2015 Apr 20].Available from: http://www.who.int/substance_
abuse/research_ tools/translation/en/.
-
-
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess 1988;52(1):30–41. [doi: 10.1207/s15327752jpa5201_2]
-
-
Shin JS, Lee YB. The effects of social supports on psychosocial well-being of the unemployed. Korean J Soc Welf 1999;37:241–269.
-
-
Kim JN, Kwon JH, Kim SY, Yu BH, Hur JW, Kim BS, et al. Validation of Korean-cancer coping questionnaire (K-CCQ). Korean J Health Psychol 2004;9(2):395–414.
-
-
Zhu J, Ebert L, Liu X, Chan SW. A mobile application of breast cancer e-support program versus routine care in the treatment of Chinese women with breast cancer undergoing chemotherapy: Study protocol for a randomized controlled trial. BMC Cancer 2017;17(1):291. [doi: 10.1186/s12885-017-3276-7]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

