Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 43(4); 2013 > Article
-
Original Article
- Clinical Nurses’ Knowledge and Visual Differentiation Ability in Pressure Ulcer Classification System and Incontinence-associated Dermatitis
- Yun Jin Lee1, Seungmi Park2, Jung Yoon Kim3, Chul-Gyu Kim4, Sun Kyung Cha4
-
Journal of Korean Academy of Nursing 2013;43(4):526-535.
DOI: https://doi.org/10.4040/jkan.2013.43.4.526
Published online: August 12, 2013
1Department of Nursing, Severance Hospital, Seoul, Korea
2Department of Nursing, Hoseo University, Asan, Korea
3Department of Plastic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
4Department of Nursing, Cheongju University, Cheongju, Korea
1Department of Nursing, Severance Hospital, Seoul, Korea
2Department of Nursing, Hoseo University, Asan, Korea
3Department of Plastic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
4Department of Nursing, Cheongju University, Cheongju, Korea
- Address reprint requests to : Park, Seungmi Department of Nursing, Hoseo University, 79-20 Hoseo-ro, Sechul-ri, Baebang-eup, Asan 336-795, Korea Tel: +82-41-540-9533 Fax: +82-41-540-9558 E-mail: seungmipark@hoseo.edu
Copyright © 2013 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Purpose
- This study was done to compare clinical nurses’ knowledge and visual differentiation diagnostic ability for the pressure ulcer classification system (PUCS) and incontinence-associated dermatitis (IAD).
-
Methods
- A convenience sample of 602 nurses took the pressure ulcer classification system and incontinence-associated dermatitis knowledge test (PUCS & IAD KT) and completed the visual differentiation tool (VDT), consisting of 21 photographs with clinical information.
-
Results
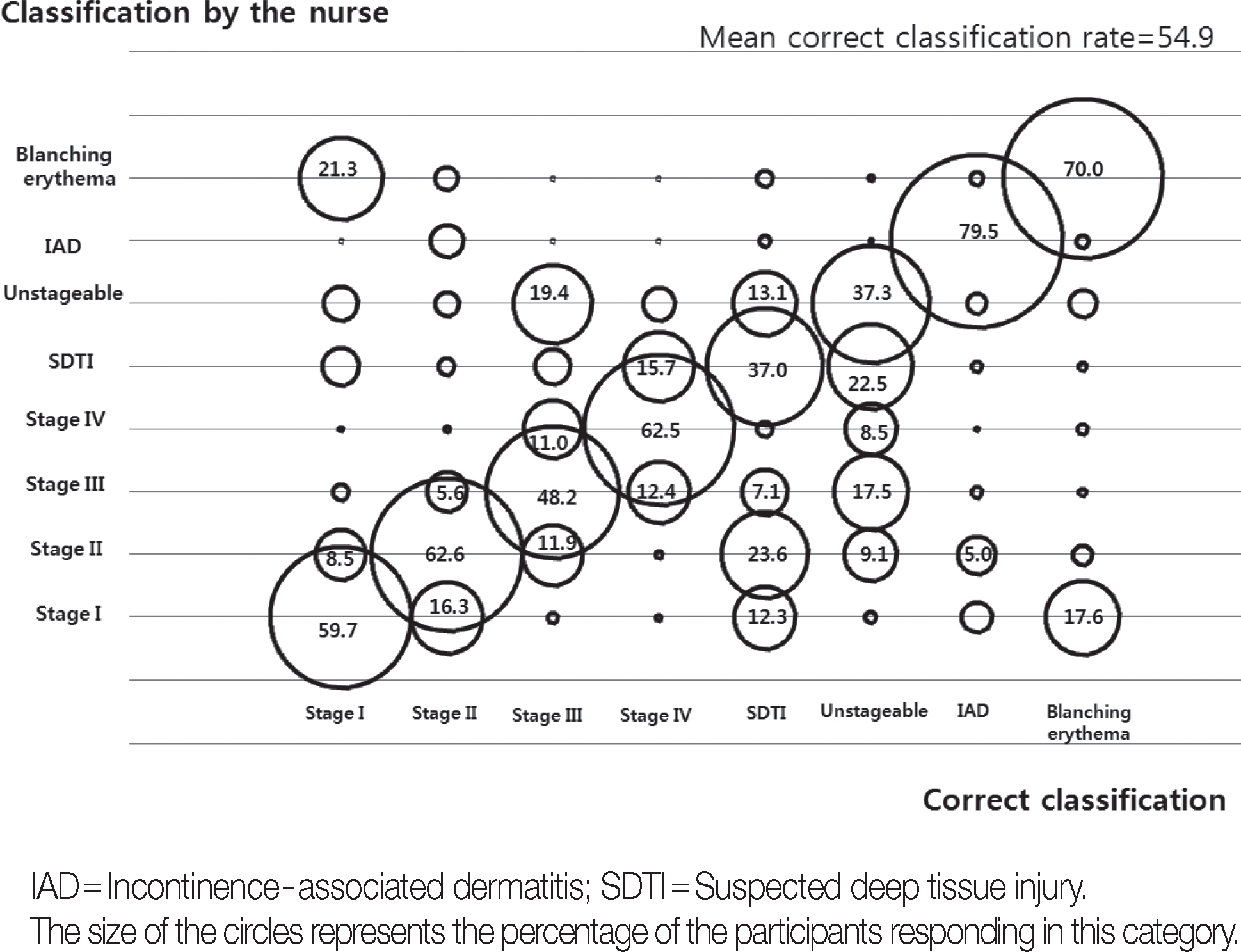
- The overall mean score for correct answers was 14.5 (± 3.2) in PUCS & IAD KT and 11.15 (± 4.9) in PUCS & IAD VDT. Incorrect responses were most common for statements related to stage III, IAD for PUCS & IAD KT, and suspected deep tissue injury (SDTI), un-stageable, and stage III for PUCS & IAD VDT. Significant correlations were found between PUCS & IAD KT and VDT (r= .48, p< .001). Factors affecting scores for PUCS & IAD VDT were PUCS & IAD KT, frequency of pressure ulcer, IAD management and participation in wound care education programs.
-
Conclusion
- Results indicate that nurses have an overall understanding of PUCS & IAD, but low visual differentiation ability regarding stage III, SDTI, and unstageable ulcers. Continuing education is needed to further improve knowledge and visual differentiation ability for PUCS & IAD.
| Characteristics | Categories | n (%) or M±SD |
PUCS & IAD KT |
PUCS & IAD VDT |
||||
|---|---|---|---|---|---|---|---|---|
| M±SD | t or F | p | M±SD | t or F | p | |||
| Age (year) | <30 | 304 (50.5) | 14.3±3.8 | 1.36 | .257 | 11.6±4.7 | 0.46 | .628 |
| 30-39 | 199 (33.1) | 14.5±3.6 | 11.6±5.3 | |||||
| ≥40 | 99 (16.4) | 15.0±3.0 | 11.1±4.8 | |||||
| 31.6±7.0 | ||||||||
| Gender* | Male | 13 (2.2) | 13.4±4.8 | −0.87 | .398 | 12.5±4.0 | 0.75 | .453 |
| Female | 572 (97.8) | 14.6±3.1 | 11.5±5.0 | |||||
| Education* | Diploma | 181 (30.2) | 14.7±3.0 | 0.85 | .430 | 11.6±4.6 | 0.07 | .933 |
| Bachelor | 328 (54.9) | 14.3±3.3 | 11.4±5.0 | |||||
| ≥Master | 89 (14.9) | 14.6±3.4 | 11.6±5.6 | |||||
| Position* | Staff nurse | 420 (70.8) | 14.2±3.2b | 5.66 | <.001 | 11.4±4.7a | 4.86 | <.001 |
| Charge nurse | 71 (12.0) | 14.7±3.0b | 10.5±5.1b | |||||
| Manager | 33 (5.6) | 14.6±2.8b | 12.2±4.3b | |||||
| CNS | 47 (7.9) | 16.4±2.8a | 14.3±5.6a | |||||
| Others | 22 (3.7) | 15.0±4.1b | 11.2±6.5b | |||||
| Career length (year) | <5 | 239 (39.7) | 14.1±3.5 | 2.80 | .061 | 11.6±4.5 | 2.23 | .107 |
| 5-9 | 160 (26.6) | 14.8±2.7 | 12.1±5.2 | |||||
| ≥10 | 203 (33.7) | 14.7±3.2 | 11.0±5.1 | |||||
| 8.1±6.6 | ||||||||
| Unit* | Surgical ward | 224 (37.7) | 14.5±3.3 | 0.03 | .991 | 11.1±5.3 | 1.34 | .261 |
| Medical ward | 130 (21.9) | 14.5±2.8 | 11.8±4.6 | |||||
| ICU | 115 (19.4) | 14.4±2.8 | 12.2±4.3 | |||||
| Others | 125 (21.0) | 14.5±3.6 | 11.6±5.1 | |||||
| Number of beds* | ≥1,000 | 249 (43.0) | 13.8±3.6b | 10.73 | <.001 | 11.1±4.9 | 1.48 | .228 |
| 500-999 | 286 (49.4) | 14.9±2.6a | 11.8±4.8 | |||||
| <500 | 54 (7.6) | 15.5±2.5a | 11.4±5.2 | |||||
| Frequency PU and | Never | 83 (13.9) | 12.4±4.0c | 17.30 | <.001 | 8.0±4.3c | 26.51 | <.001 |
| IAD management* | Sometimes | 182 (30.5) | 14.5±2.7b | 11.1±4.3b | ||||
| Often | 192 (32.2) | 14.8±3.0b | 12.1±4.9b | |||||
| Almost always | 140 (23.4) | 15.4±2.8a | 13.5±4.7a | |||||
| Participation of wound | Never | 181 (30.5) | 14.1±3.1b | 6.02 | <.001 | 10.0±4.7b | 15.01 | <.001 |
| care education | 1-2 | 347 (58.5) | 14.4±3.3b | 11.8±4.7b | ||||
| program* | 3-4 | 52 (8.8) | 16.1±2.4a | 14.6±4.9a | ||||
| ≥5 | 13 (2.2) | 15.9±2.3a | 14.1±6.1a | |||||
| Provider of PU | Doctor | 122 (21.9) | 14.6±3.4 | 1.49 | .217 | 10.6±4.8b | 3.62 | .013 |
| treatments* | Staff nurse | 168 (30.2) | 14.1±3.1 | 11.5±4.7b | ||||
| CNS | 224 (40.2) | 14.8±2.9 | 12.3±5.0a | |||||
| Others | 43 (7.7) | 14.8±3.3 | 10.9±5.3b | |||||
| Items | n (%) or M±SD |
|---|---|
| Stage I pressure ulcers are defined as intact skin with nonblanchable erythema on bony prominence. | 525 (87.2) |
| If there is perineal skin injury with erythema due to incontinence and no pressure, it is a pressure ulcer*. | 436 (72.4) |
| It is not a pressure ulcer if there are skin injuries with blanching erythema. | 356 (59.1) |
| Moisture associated skin damage such as urinary and fecal incontinence is related to the development of pressure ulcers. | 567 (94.2) |
| Pressures and/or shearing force increase the risk for pressure ulcers. | 581 (96.5) |
| Stage II pressure ulcers are intact skin with vesicles on pressure. | 420 (69.8) |
| The nose, ear, occiput, and malleolus do not have subcutaneous tissue and these ulcers cannot become stage III*. | 541 (89.9) |
| There is no necrotic tissue on wound bed in patients with incontinence-associated dermatitis. | 283 (47.0) |
| Stable eschar on the heels serves as the body’s biological cover and should not be removed. | 302 (50.2) |
| Suspected deep tissue injury may further evolve and become covered by eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment. | 529 (87.9) |
| Unstageable pressure ulcers are wounds whose bases are covered by dead tissues composed of slough and/or eschar. | 513 (85.2) |
| Secondary cutaneous infection such as fungal infection may easily develop in patients with incontinence-associated dermatitis. | 582 (96.7) |
| Incidence of incontinence-associated dermatitis is higher in fecal incontinence than urinary incontinence. | 498 (82.7) |
| Suspected deep tissue injury appears as an area of purple or maroon discoloration in intact skin or as a blood-filled blister. | 540 (89.7) |
| It is stage II if there is no bony prominence but moisture associated skin damage with fecal incontinence*. | 389 (64.6) |
| A stage IV pressure ulcer is damage to muscle and bone. | 575 (95.5) |
| Necrotic tissue, undermining, and tunneling may exist in Stage III and Stage IV. | 566 (94.0) |
| A stage III pressure ulcer involves the fat tissue and fascia*. | 137 (22.8) |
| It is possible to label the ulcer as Stage II when Stage III is healing with granulation tissue*. | 386 (64.1) |
| Total number of correct answers | 8726 (76.3) |
| Total | 14.5±3.2 |
- Aydin A K &, Karadag . 2010;Assessment of nurses’ knowledge and practice in prevention and management of deep tissue injury and stage I pressure ulcer. Journal of Wound, Ostomy and Continence Nursing. 37(5):487–494. http://dx.doi.org/10.1097/WON.0b013e3181edec0bArticle
- Baumgarten M, Margolis D J, Localio A R, Kagan S H, Lowe R A, Kinosian B. . 2006;Pressure ulcers among elderly patients early in the hospital stay. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences. 61(7):749–754.Article
- Beeckman D, Schoonhoven L, Boucqué H, Van Maele G &, Defloor T. 2008;Pressure ulcers: E-learning to improve classification by nurses and nursing students. Journal of Clinical Nursing. 17(13):1697–1707.ArticlePubMed
- Beeckman D, Schoonhoven L, Fletcher J, Furtado K, Gunningberg L, Heyman H. . 2007;EPUAP classification system for pressure ulcers: European reliability study. Journal of Advanced Nursing. 60(6):682–691. http://dx.doi.org/10.1111/j.1365-2648.2007.04474.xArticlePubMed
- Bennett G, Dealey C &, Posnett J. 2004;The cost of pressure ulcers in the UK. Age and Ageing. 33(3):230–235. http://dx.doi.org/10.1093/ageing/afh086ArticlePubMed
- Defloor T &, Schoonhoven L. 2004;Inter-rater reliability of the EPUAP pressure ulcer classification system using photographs. Journal of Clinical Nursing. 13(8):952–959. http://dx.doi.org/10.1111/j.1365-2702.2004.00974.xArticlePubMed
- Defloor T, Schoonhoven L, Katrien V, Weststrate J &, Myny D. 2006;Reliability of the European Pressure Ulcer Advisory Panel classification system. Journal of Advanced Nursing. 54(2):189–198. http://dx.doi.org/10.1111/j.1365-2648.2006.03801.xArticlePubMedPDF
- Fader M, Clarke-O'Neill S, Cook D, Dean G, Brooks R, Cottenden A. . 2003.Management of night-time urinary incontinence in residential settings for older people: An investigation into the effects of different pad changing regimes on skin health. Journal of Clinical Nursing. 12(3): p. 374–386.ArticlePubMed
- Finlay K, Smith J, Abrams S &, Evangelista M. 2004;The impact of nursing education on pressure ulcer prevention. Journal of Wound, Ostomy and Continence Nursing. 31(3S):S3–S4.Article
- Gray M. 2010;Optimal management of incontinence-associated dermatitis in the elderly. American Journal of Clinical Dermatology. 11(3):201–210. http://dx.doi.org/10.2165/11311010-000000000-00000ArticlePubMed
- Honaker J S, Forston M R, Davis E A, Wiesner M M &, Morgan J A. 2013;Effects of non contact low-frequency ultrasound on healing of suspected deep tissue injury: A retrospective analysis. International Wound Journal. 10(1):65–72. http://dx.doi.org/10.1111/j.1742-481X.201200944xArticlePubMed
- Hopkins A, Dealey C, Bale S, Defloor T &, Worboys F. 2006;Patient stories of living with a pressure ulcer. Journal of Advanced Nursing. 56(4):345–353. http://dx.doi.org/10.1111/j.1365-2648.2006.04007.xArticlePubMed
- Jin Y S. 2009;Knowledge, performance, and awareness of importance on pressure ulcer care among nurses at a general hospital. Unpublished master’s thesis, Yonsei University, Seoul.
- Kelly J &, Isted M. 2011;Assessing nurses’ ability to classify pressure ulcers correctly. Nursing Standard. 26(7):62–64, 66 passim.Article
- Kim H Y. 2003;The knowledge of pressure ulcer and the nursing intervention of nurse in hospital. Unpublished master's thesis, Dong-A University, Busan.
- Kim K S, Kim J A, Kim M S, Kim Y J, Kim E S, Park K O. . 2009;Development of performance measures based on the nursing process for prevention and management of pressure ulcers, falls and pain. Journal of Korean Clinical Nursing Research. 15(1):133–147.
- Korean Association of Wound Ostomy Continence Nurses. 2011.Clinical guideline for pressure ulcer. Seoul: Fornurse.
- Kwon E O, Eom I H, Chang S J, Shim M Y &, Lee S H. 2012;Accuracy of nurses’ assessments of pressure ulcers in hospitalized patients. Journal of Korean Clinical Nursing Research. 18(1):29–38.
- Lee E J &, Yang S O. 2011;Clinical knowledge and actual performance of pressure ulcer care by hospital nurses. Journal of Korean Clinical Nursing Research. 17(2):251–261.
- Lee M O. 2000;Knowledge level of pressure ulcer among hospital nurses. Journal of Korean Academy of Adult Nursing. 12(4):619–628.
- Lee Y J, Kim J Y &, Lee T W. 2011;Inter-rater reliability of the pressure ulcer classification system. Korean Wound Management Society. 7(2):75–80.
- Nixon J, Thorpe H, Barrow H, Phillips A, Andrea Nelson E, Mason S A. . 2005;Reliability of pressure ulcer classification and diagnosis. Journal of Advanced Nursing. 50(6):613–623. http://dx.doi.org/10.11 11/j.1365-2648.2005.03439.xArticlePubMed
- Pedley G E. 2004;Comparison of pressure ulcer grading scales: A study of clinical utility and inter-rater reliability. International Journal of Nursing Studies. 41(2):129–140.ArticlePubMed
- Richbourg L, Smith J &, Dunzweiler S. 2011;Suspected deep tissue injury evaluated by North Carolina WOC nurses: A descriptive study. Journal of Wound, Ostomy and Continence Nursing. 38(6):655–660. http://dx.doi.org/10.1097/WON.0b013e31823429e7
- Russell L. 2002;Pressure ulcer classification: The systems and the pitfalls. British Journal of Nursing. 11(12 Suppl):S49–S50, S52, S54-S47 passim.ArticlePubMed
- Shea J D. 1975;Pressure sores: Classification and management. Clinical Orthopaedics and Related Research. (112):89–100.Article
- Suddaby E C, Barnett S &, Facteau L. 2005;Skin breakdown in acute care pediatrics. Pediatric Nursing. 31(2):132–138. 148. PubMed
- Vanderwee K, Clark M, Dealey C, Gunningberg L &, Defloor T. 2007;Pressure ulcer prevalence in Europe: A pilot study. Journal of Evaluation in Clinical Practice. 13(2):227–235. http://dx.doi.org/10.1111/j.1365-2753.2006.00684.xArticlePubMed
- Whittington K T &, Briones R. 2004;National Prevalence and Incidence Study: 6-year sequential acute care data. Advances in Skin & Wound Care. 17(9):490–494.Article
- Yang N Y &, Moon S Y. 2009;Perceived importance, educational needs, knowledge and performance concerning pressure ulcer care by clinical nurses. Journal of Korean Academy of Adult Nursing. 21(1):95–104.
- Young Z F, Evans A &, Davis J. 2003;Nosocomial pressure ulcer prevention: A successful project. Journal of Nursing Administration. 33(7-8):380–383.PubMed
REFERENCES
Figure & Data
REFERENCES
Citations

- Effectiveness of immersive teaching strategies on pressure injury: Impact on nurses' knowledge, attitudes and self-efficacy – A partially randomized participant preference (PRPP) controlled trial
Wen-Yi Chao, Yu-Lin Wu, Mei-Yu Hsu, Chien-Lun Chu
Nurse Education in Practice.2025; 82: 104237. CrossRef - Senior Baccalaureate Nursing Students’ Knowledge and Visual Differentiation Ability for the Pressure Injury Classification System and Incontinence-associated Dermatitis
Eunyoung Cho, Yune Kyong Kim, Yun Jin Lee, Youn Sun Hwang
Journal of Korean Academy of Fundamentals of Nursing.2024; 31(2): 191. CrossRef - Big Data Analysis on Consumer Perception of Pressure Injuries: Text Mining and Semantic Network Analysis
Kyung Hee Park, Jinho Lee, Soon Chul Kwon, Jaeseung Kim
Journal of Wound Management and Research.2024; 20(3): 251. CrossRef - Knowledge and Visual Differentiation Ability of the Pressure Injury Classification System and Incontinence-Associated Dermatitis among Hospital Nurses: A Descriptive Study
Seungmi Park, Eun Jung Kim, Son Ja Lee, Eun Jeong Kim, Ji Yeon Lee, Jung Eun Hong
Healthcare.2024; 12(2): 145. CrossRef - Investigation of factors associated with pressure ulcer in patients receiving home care services via path analysis
Selma Durmuş Sarıkahya
Journal of Tissue Viability.2024; 33(2): 152. CrossRef - Evaluating Intensive Care Nurses’ Knowledge of Incontinence-Associated Dermatitis: A Multicenter Cross-sectional Study
Meryem Kılıç, Asiye Tuncay, Sümeyra Benan Çakır
Advances in Skin & Wound Care.2024; 37(9): 1. CrossRef - Development and Effectiveness of a Clinical Decision Support System for Pressure Ulcer Prevention Care Using Machine Learning
Myoung Soo Kim, Jung Mi Ryu, Byung Kwan Choi
CIN: Computers, Informatics, Nursing.2023; 41(4): 236. CrossRef - The ability of critical care nurses to identify pressure injury and incontinence‐associated dermatitis: A multicentre cross‐sectional survey
Huan Liu, Aiping Du, Yongming Tian, Mingrong Gao, Shuming Ji, Jie Mi, Xiaoping Shao, Debin Huang, Xiaoyi Cao
Nursing Open.2023; 10(3): 1556. CrossRef - Effects of Attitude, Barriers/Facilitators, and Visual Differentiation on Oral Mucosa Pressure Ulcer Prevention Performance Intention
Min Kyeong Kang, Myoung Soo Kim
Healthcare.2021; 9(1): 76. CrossRef - The Effect of Pressure Injury Training for Nurses: A Systematic Review and Meta-analysis
Gaeun Kim, Mikyung Park, Kyungwon Kim
Advances in Skin & Wound Care.2020; 33(3): 1. CrossRef - The Interrater Agreement for the Assessment of Pressure Ulcer Risk Using the Braden Scale and the Classification of Pressure Ulcers by Nurses in A Medium-Sized Hospital
Hyung-Ju Na, Sung-Hee Yoo, Young-Ran Kwon, Min-Jeng Ahn
Korean Journal of Adult Nursing.2020; 32(1): 35. CrossRef - Development and Utilization of a Clinical Decision Support System Contents for Pressure Ulcer Prevention Care
Myoung Soo Kim, Jung Mi Ryu
Journal of Health Informatics and Statistics.2020; 45(4): 365. CrossRef - Canonical Correlation between Knowledge-Barriers/Facilitators for Pressure Ulcer Prevention Nursing Variables and Attitude-Performance Variables
Myoung Soo Kim, Jung Mi Ryu
Journal of Health Informatics and Statistics.2019; 44(3): 227. CrossRef - The use of sub-epidermal moisture measurement in predicting blanching erythema in jaundice patients
Seungmi Park, Chul-Gyu Kim, Ji Woon Ko
Journal of Wound Care.2018; 27(5): 342. CrossRef - Effects of home-visit nursing services on hospitalization in the elderly with pressure ulcers: a longitudinal study
Hyo Jung Lee, Yeong Jun Ju, Eun-Cheol Park, Juyeong Kim, Sang Gyu Lee
European Journal of Public Health.2017; 27(5): 822. CrossRef - Effects of pressure ulcer classification system education programme on knowledge and visual differential diagnostic ability of pressure ulcer classification and incontinence‐associated dermatitis for clinical nurses in Korea
Yun Jin Lee, Jung Yoon Kim
International Wound Journal.2016; 13(S1): 26. CrossRef - A Phenomenological Study on Illness Experience of Patients with Pressure Ulcer
Misoo Yoo, Myungsun Yi
Korean Journal of Adult Nursing.2015; 27(5): 515. CrossRef - Effects of Pressure Ulcer Classification System Education Program on Knowledge and Visual Discrimination Ability of Pressure Ulcer Classification and Incontinence-Associated Dermatitis for Hospital Nurses
Yun Jin Lee, Seungmi Park
Journal of Korean Biological Nursing Science.2014; 16(4): 342. CrossRef
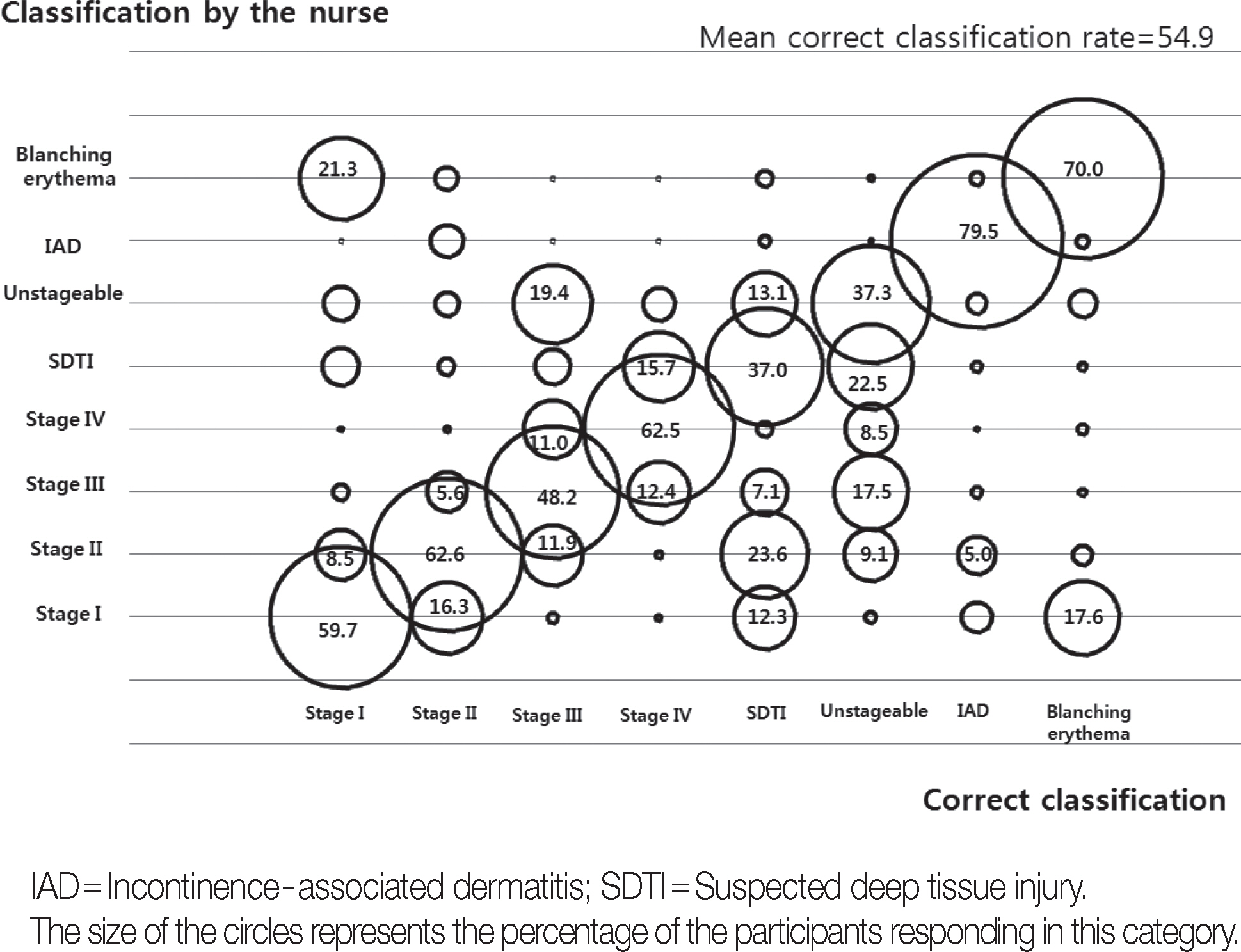
Figure 1.
| Characteristics | Categories | n (%) or M±SD | PUCS & IAD KT |
PUCS & IAD VDT |
||||
|---|---|---|---|---|---|---|---|---|
| M±SD | t or F | p | M±SD | t or F | p | |||
| Age (year) | <30 | 304 (50.5) | 14.3±3.8 | 1.36 | .257 | 11.6±4.7 | 0.46 | .628 |
| 30-39 | 199 (33.1) | 14.5±3.6 | 11.6±5.3 | |||||
| ≥40 | 99 (16.4) | 15.0±3.0 | 11.1±4.8 | |||||
| 31.6±7.0 | ||||||||
| Gender |
Male | 13 (2.2) | 13.4±4.8 | −0.87 | .398 | 12.5±4.0 | 0.75 | .453 |
| Female | 572 (97.8) | 14.6±3.1 | 11.5±5.0 | |||||
| Education |
Diploma | 181 (30.2) | 14.7±3.0 | 0.85 | .430 | 11.6±4.6 | 0.07 | .933 |
| Bachelor | 328 (54.9) | 14.3±3.3 | 11.4±5.0 | |||||
| ≥Master | 89 (14.9) | 14.6±3.4 | 11.6±5.6 | |||||
| Position |
Staff nurse | 420 (70.8) | 14.2±3.2b | 5.66 | <.001 | 11.4±4.7a | 4.86 | <.001 |
| Charge nurse | 71 (12.0) | 14.7±3.0b | 10.5±5.1b | |||||
| Manager | 33 (5.6) | 14.6±2.8b | 12.2±4.3b | |||||
| CNS | 47 (7.9) | 16.4±2.8a | 14.3±5.6a | |||||
| Others | 22 (3.7) | 15.0±4.1b | 11.2±6.5b | |||||
| Career length (year) | <5 | 239 (39.7) | 14.1±3.5 | 2.80 | .061 | 11.6±4.5 | 2.23 | .107 |
| 5-9 | 160 (26.6) | 14.8±2.7 | 12.1±5.2 | |||||
| ≥10 | 203 (33.7) | 14.7±3.2 | 11.0±5.1 | |||||
| 8.1±6.6 | ||||||||
| Unit |
Surgical ward | 224 (37.7) | 14.5±3.3 | 0.03 | .991 | 11.1±5.3 | 1.34 | .261 |
| Medical ward | 130 (21.9) | 14.5±2.8 | 11.8±4.6 | |||||
| ICU | 115 (19.4) | 14.4±2.8 | 12.2±4.3 | |||||
| Others | 125 (21.0) | 14.5±3.6 | 11.6±5.1 | |||||
| Number of beds |
≥1,000 | 249 (43.0) | 13.8±3.6b | 10.73 | <.001 | 11.1±4.9 | 1.48 | .228 |
| 500-999 | 286 (49.4) | 14.9±2.6a | 11.8±4.8 | |||||
| <500 | 54 (7.6) | 15.5±2.5a | 11.4±5.2 | |||||
| Frequency PU and | Never | 83 (13.9) | 12.4±4.0c | 17.30 | <.001 | 8.0±4.3c | 26.51 | <.001 |
| IAD management |
Sometimes | 182 (30.5) | 14.5±2.7b | 11.1±4.3b | ||||
| Often | 192 (32.2) | 14.8±3.0b | 12.1±4.9b | |||||
| Almost always | 140 (23.4) | 15.4±2.8a | 13.5±4.7a | |||||
| Participation of wound | Never | 181 (30.5) | 14.1±3.1b | 6.02 | <.001 | 10.0±4.7b | 15.01 | <.001 |
| care education | 1-2 | 347 (58.5) | 14.4±3.3b | 11.8±4.7b | ||||
| program |
3-4 | 52 (8.8) | 16.1±2.4a | 14.6±4.9a | ||||
| ≥5 | 13 (2.2) | 15.9±2.3a | 14.1±6.1a | |||||
| Provider of PU | Doctor | 122 (21.9) | 14.6±3.4 | 1.49 | .217 | 10.6±4.8b | 3.62 | .013 |
| treatments |
Staff nurse | 168 (30.2) | 14.1±3.1 | 11.5±4.7b | ||||
| CNS | 224 (40.2) | 14.8±2.9 | 12.3±5.0a | |||||
| Others | 43 (7.7) | 14.8±3.3 | 10.9±5.3b | |||||
| Items | n (%) or M±SD |
|---|---|
| Stage I pressure ulcers are defined as intact skin with nonblanchable erythema on bony prominence. | 525 (87.2) |
| If there is perineal skin injury with erythema due to incontinence and no pressure, it is a pressure ulcer |
436 (72.4) |
| It is not a pressure ulcer if there are skin injuries with blanching erythema. | 356 (59.1) |
| Moisture associated skin damage such as urinary and fecal incontinence is related to the development of pressure ulcers. | 567 (94.2) |
| Pressures and/or shearing force increase the risk for pressure ulcers. | 581 (96.5) |
| Stage II pressure ulcers are intact skin with vesicles on pressure. | 420 (69.8) |
| The nose, ear, occiput, and malleolus do not have subcutaneous tissue and these ulcers cannot become stage III |
541 (89.9) |
| There is no necrotic tissue on wound bed in patients with incontinence-associated dermatitis. | 283 (47.0) |
| Stable eschar on the heels serves as the body’s biological cover and should not be removed. | 302 (50.2) |
| Suspected deep tissue injury may further evolve and become covered by eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment. | 529 (87.9) |
| Unstageable pressure ulcers are wounds whose bases are covered by dead tissues composed of slough and/or eschar. | 513 (85.2) |
| Secondary cutaneous infection such as fungal infection may easily develop in patients with incontinence-associated dermatitis. | 582 (96.7) |
| Incidence of incontinence-associated dermatitis is higher in fecal incontinence than urinary incontinence. | 498 (82.7) |
| Suspected deep tissue injury appears as an area of purple or maroon discoloration in intact skin or as a blood-filled blister. | 540 (89.7) |
| It is stage II if there is no bony prominence but moisture associated skin damage with fecal incontinence |
389 (64.6) |
| A stage IV pressure ulcer is damage to muscle and bone. | 575 (95.5) |
| Necrotic tissue, undermining, and tunneling may exist in Stage III and Stage IV. | 566 (94.0) |
| A stage III pressure ulcer involves the fat tissue and fascia |
137 (22.8) |
| It is possible to label the ulcer as Stage II when Stage III is healing with granulation tissue |
386 (64.1) |
| Total number of correct answers | 8726 (76.3) |
| Total | 14.5±3.2 |
| Variables | Pressure ulcer classification system and incontinence-associated dermatitis visual differentiation tool |
|---|---|
| r (p) | |
| Pressure ulcer classification system and incontinence-associated dermatitis knowledge test | .48 (<.001) |
| Dependent variables | Independent variables | ß | SE | t or F | p | Partial R2 | Model R2 |
|---|---|---|---|---|---|---|---|
| PUCS, IAD, & VDT | Intercept | −1.04 | 0.79 | −1.43 | .154 | ||
| Knowledge of PUCS and IAD | 0.54 | 0.04 | 13.76 | <.001 | .30 | .30 | |
| Frequency PU and IAD management | 0.97 | 0.17 | 5.45 | <.001 | .04 | .34 | |
| Participation of wound care education program | 1.19 | 0.28 | 4.33 | <.001 | .02 | .36 | |
| Model | 108.31 | <.001 |
PUCS=Pressure ulcer classification system; IAD=Incontinence-associated dermatitis; KT=Knowledge test; VDT=Visual differentiation tool; CNS=Clinical nurse specialist; ICU=Intensive care unit; PU=Pressure ulcer; a, b, c=Duncan multiple range test grouping. Except for non-response.
Opposite coding.
PUCS=Pressure ulcer classification system; IAD=Incontinence-associated dermatitis; VDT=Visual differentiation tool; PU=Pressure ulcer.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

