Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 41(4); 2011 > Article
-
Original Article
- Effects and Adequacy of High-Fidelity Simulation-Based Training for Obstetrical Nursing
- Woo Sook Lee1, Miok Kim2
-
Journal of Korean Academy of Nursing 2011;41(4):433-443.
DOI: https://doi.org/10.4040/jkan.2011.41.4.433
Published online: August 12, 2011
1Associate Professor, Red Cross College of Nursing, Seoul, Korea
2Full-time Lecturer, Department of Nursing, Namseoul University, Cheonan, Korea
1Associate Professor, Red Cross College of Nursing, Seoul, Korea
2Full-time Lecturer, Department of Nursing, Namseoul University, Cheonan, Korea
- Address reprint requests to : Kim, Miok Department of Nursing, Namseoul University, 21 Maeju-ri, Seonghwan-eup, Seobuk-gu, Cheonan 331-707, Korea Tel: +82-41-580-2716 Fax. +82-41-580-2931 E-mail: aprilsea@hanmail.net
• Received: November 2, 2010 • Revised: November 4, 2010 • Accepted: August 4, 2011
Copyright © 2011 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Purpose
- Clinical training for nursing students is limited to rudimentary skills to avoid potential risks. Simulation-Based Training (SBT) can overcome the shortcomings of clinical training. We evaluated the educational effect of SBT for obstetrical nursing students using high-fidelity simulation courses.
-
Methods
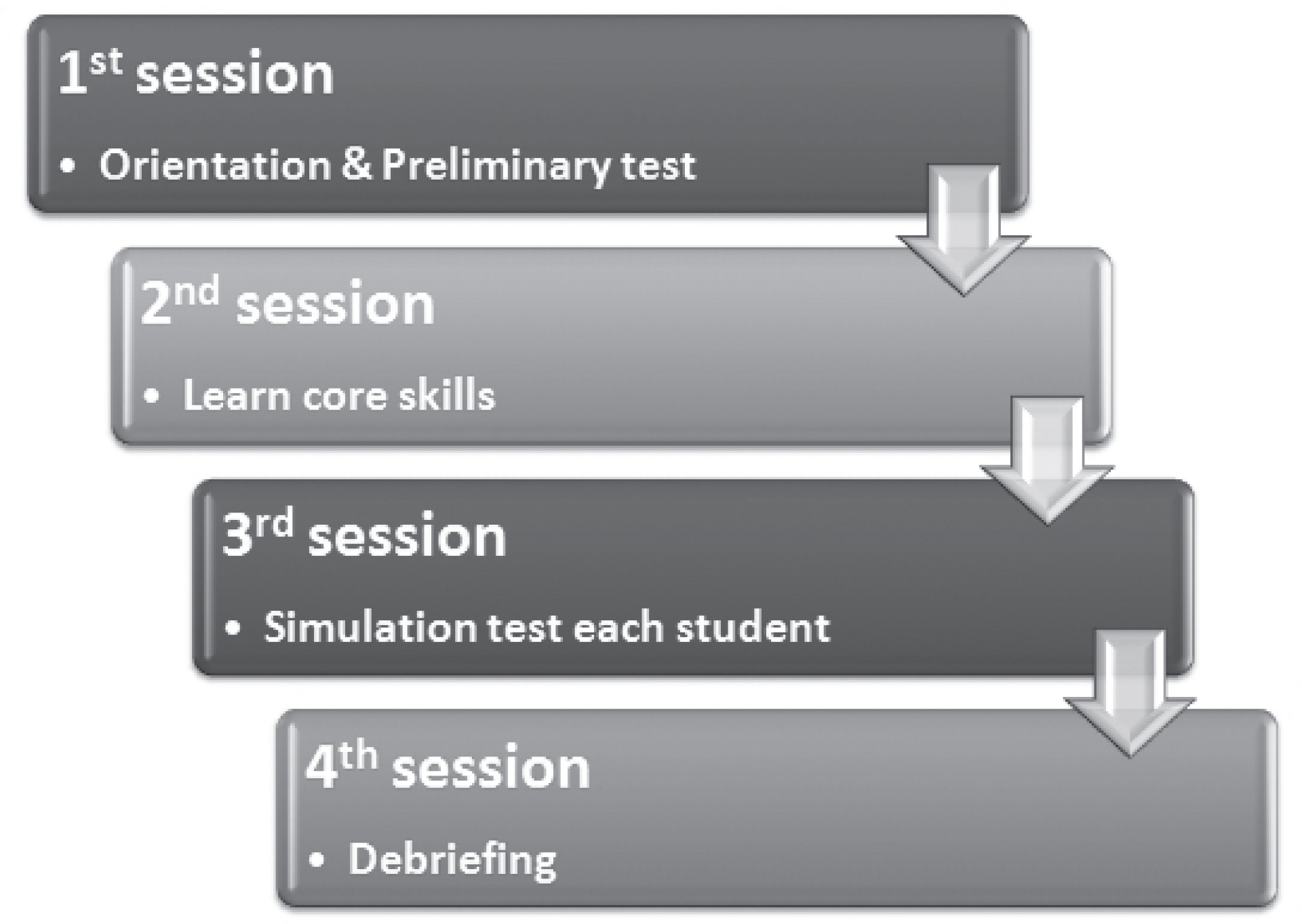
- We developed a simulation program for obstetrical nursing students to practice nursing skills that are necessary to provide quality care. The program consisted of four sessions. 1st: An orientation and a preliminary test. 2nd: Learning core skills required in obstetrical nursing. 3rd: Testing each student with scenario. 4th: Providing a debriefing session. At the beginning of the program, students were surveyed about their self-confidence in obstetrical nursing care, and at the end of the program, they were surveyed about the adequacy of SBT as well as self-confidence.
-
Results
- Students’ self-confidence showed a significant difference before and after simulation. Mean adequacy of SBT was 7.15±1.35 (out of 10). Most students became more interested in Women’s Health Nursing after SBT.
-
Conclusion
- The results from evaluating the effects of simulation-based obstetrical nursing training show that SBT provides invaluable clinical experience for obstetrical nursing students by overcoming the lack of actual clinical involvement in clinical training programs.
Table 1.General Characteristics of Participants (N=138)
Table 2.Self-confidence about Clinical Practices for Obstetric Nursing (N=138
Table 3.Adequacy of Simulation-based Training (N=138
- Alinier G, Hunt W &, Gordon R. 2004;Determining the value of simulation in nurse education: Study design and initial results. Nurse Education in Practice. 4:200–207. doi:10.1016/S1471(03)00066-0.ArticlePubMed
- Baillie L &, Curzio J. 2009;Students’ and facilitators’ perceptions of simulation in practice learning. Nurse Education in Practice. 9:297–306. doi: 10.1016/j.nepr.2008.08.007.ArticlePubMed
- Beaubien J M &, Baker D P. 2004;The use of simulation for training teamwork skills in health care: How low can you go? Quality & Safety in Health Care. 13:i51–i56.Article
- Choi J Y, Jang K S, Choi S H &, Hong M S. 2008;Validity and reliability of a clinical performance examination using standardized patients. Journal of Korean Academy of Nursing. 38:83–91. doi:10.4040/jkan.2008.38.1.83.ArticlePubMed
- Cohen J. 1988.Statistical power analysis for the behavioral sciences. 2nd ed.Hillsdale, NJ: Erlbaum.Article
- Deering S, Brown J, Hodor J &, Satin A J. 2006;Simulation training and resident performance of singleton vaginal breech delivery. Obstetrics & Gynecology. 107:86–89.Article
- Ellis D, Crafts J F, Hunt L P, Read M, Fox R &, James M. 2008;Hospital, simulation center, and teamwork training for eclampsia management: A randomized controlled trial. American Journal of Obstetrics and Gynecology. 111:723–731.
- Eom M R, Kim H S, Kim E K &, Seong K. 2010;Effects of teaching method using standardized patients on nursing competence in subcutaneous injection, self-directed learning readiness, and problem solving ability. Journal of Korean Academy of Nursing. 40:151–160. doi:10.4040/ jkan.2010.40.2.151.ArticlePubMed
- Fanning R M &, Gaba D M. 2007;The role of debriefing in simulation-based training. Society for Simulation in Healthcare. 2:115–125.
- Feltz D L. 1988;Self-confidence and sports performance. Exercise and Sport Sciences Reviews. 16:151–166. doi:10.1249/00003677-198800160-00016.Article
- Gardner R &, Raemer D B. 2008;Simulation in obstetrics and gynecology. Obstetrics and Gynecology Clinics of North America. 35:97–127. doi: 10.1016/j.ogc.2007.12.008.ArticlePubMed
- Goffman D, Heo H, Chazotte C, Merkatz I &, Bernstein P S. 2008;Using simulation training to improve shoulder dystocia documentation. Obstetrics & Gynecology. 112:1284–1287.Article
- Hertel J P &, Millis B J. 2002.Using simulations to promote learning in higher education: An introduction. Sterling VA: Stylus.
- Jude D C, Gilbert C G &, Magrane D. 2006;Simulation training in the obstetrics and gynecology clerkship. American Journal of Obstetrics and Gynecology. 195:1489–1492. doi:10.1016/j.ajog.2006.05.003.ArticlePubMed
- Lasater K. 2007;High-fidelity simulation and the development of clinical judgement: Students’ experiences. Journal of Nursing Education. 46.
- Maslovitz S, Barkai G, Lessing J, Ziv A &, Many A. 2007;Recurrent obstetric management mistakes identified by simulation. Obstetrics & Gynecology. 109:1295–1300.Article
- McCaughey C S &, Traynor M K. 2010;The role of simulation in nurse education. Nurse Education Today. 30:827–832. doi:10.1016/j.nedt.2010.03.005.ArticlePubMed
- McIntosh J B, Alexander M, Veitch L &, May N. 1997;Evaluation of Nursing Times. 93:46–48.
- Mikkelsen J, Reime M H &, Harris A K. 2008;Nursing students’ learning of managing cross-infection scenario-based simulation training versus study groups. Nurse Education Today. 28:664–671. doi:10.1016/ j.nedt.2007.11.003.ArticlePubMed
- Mole L J &, McLafferty I H. 2004;Evaluating a simulated ward exercise for third year student nurses. Nurse Education in Practice. 4:91–99. doi: 10.1016/S1471(03)00031-3.ArticlePubMed
- Moule P, Wilford A, Sales R &, Locker L. 2008;Student experiences and mentor views of the use of simulation for learning. Nurse Education Today. 28:790–797. doi:10.1016/j.nedt.2008.03.007.ArticlePubMed
- Park H, Lee J, Hwang H, Lee J, Choi Y, Kim H. . 2003;The agreement of checklist recordings between faculties and standardized patients in an objective structured clinical examination (OSCE). Korean Journal of Medical Education. 15:141–150.Article
- Park J H, Jung E, Ko J K &, Yoo H B. 2008;Delivery training for undergraduate medical students using birth simulator. Korean Journal of Obstetrics and Gynecology. 51:950–956.
- Park S I. 1998.Teory and practice of the teaching-learning method (II). Paju: Kyoyookbook.
- Pittini R, Oepkes D, Macrury K, Reznick R, Beyene J &, Windrim R. 2002;Teaching invasive perinatal procedures: Assessment of a high fidelity simulator-based curriculum. Ultrasound in Obstetrics and Gynecology. 19:478–483. doi:10.1046/j.1469-0705.2002.00701.x.ArticlePubMedPDF
- Siassakos D, Draycott T, Brien K, Kenyon C, Bartlett C &, Fox R. 2010;Exploratory randomized controlled trial of hybrid obstetric simulation training for undergraduate students. Te Journal of the Society for Simulation in Healthcare. 5:193–198. doi:10.1097/SIH.0b013e3181d3ee0b.Article
- Vu N V, Barrows H S, March M L, Verhulst S J, Colliver J A &, Travis T. 1992;Six years of comprehensive, clinical, performance-based assessment using standardized patients at the Southern Illinois University School of Medicine. Academic Medicine. 67:42–50. doi:10.1097/00001888-199201000-00009.ArticlePubMed
- Wilford A &, Doyle T J. 2006;Integrating simulation training into the nursing curriculum. British Journal of Nursing. 15:604–607.ArticlePubMed
- Yoo M S, Yoo L Y, Park Y O &, Son Y J. 2002;Comparison of students’ clinical competency in different instructional methods for fundamentals of nursing practicum. Journal of Korean Academy of Nursing. 32:327–335.ArticlePDF
- Ziv A, Small S D &, Wolpe P R. 2000;Patient safety and simulation-based medical education. Medical Teacher. 22:489–495. doi:10.1080/01421590050110777.ArticlePubMed
REFERENCES
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Critical thinking, communication, decision-making confidence, and practicum stress among nursing students in maternal nursing practicum: A structural equation model
Yu-Yun Hsu, Tram Thi Bich Nguyen, Ching-Hsueh Yeh, Shiow-Meei Tsai, Yi-Chien Tsai
Nurse Education Today.2025; 153: 106815. CrossRef - Improving clinical reasoning competency and communication skills using virtual simulation-based learning focused on a pathophysiological approach in Korea: a quasi-experimental study
Sung Hae Kim, Yoona Choi
Journal of Korean Biological Nursing Science.2024; 26(4): 363. CrossRef - Trends in Acupuncture Training Research: Focus on Practical Phantom Models
Jung Eun Jang, Yeon Sun Lee, Woo Seok Jang, Won Suk Sung, Eun-Jung Kim, Seung Deok Lee, Kyung Ho Kim, Chan Yung Jung
Journal of Acupuncture Research.2022; 39(2): 77. CrossRef - Development and application of a mobile-based multimedia nursing competency evaluation system for nursing students: A mixed-method randomized controlled study
Soyoung Jang, Eunyoung E. Suh
Nurse Education in Practice.2022; 64: 103458. CrossRef - Nursing simulation practicum for delivery care: A scoping review
Chiyoung Cha, Sookyung Jeong
Nurse Education Today.2022; 114: 105391. CrossRef - Analysis of the effect of an artificial intelligence chatbot educational program on non-face-to-face classes: a quasi-experimental study
Jeong-Won Han, Junhee Park, Hanna Lee
BMC Medical Education.2022;[Epub] CrossRef - HEMŞİRELİK EĞİTİMİ VE OTANTİK ÖĞRENME
Ayşe METİN, Özen KULAKAÇ
Samsun Sağlık Bilimleri Dergisi.2021; 6(1): 35. CrossRef - The effects of a maternal nursing competency reinforcement program on nursing students’ problem-solving ability, emotional intelligence, self-directed learning ability, and maternal nursing performance in Korea: a randomized controlled trial
Sun-Hee Kim, Bo Gyeong Lee
Korean Journal of Women Health Nursing.2021; 27(3): 230. CrossRef - Development and Evaluation of a Simulated Conflict Management Program on Inter-Professional Communication Skills
Yeonjae Jo
Stress.2020; 28(3): 167. CrossRef - Experiences of Arab male nursing students during high fidelity maternity simulation training
Savithri Raman, Leodoro J. Labrague, Judie Arulappan, Omar Ali Mohammed Al‐Zaabi, Jansi Natarajan, Sophia Cyril Vincent
Nursing Forum.2020; 55(2): 92. CrossRef - Effects of integrative simulation practice on nursing knowledge, critical thinking, problem-solving ability, and immersion in problem-based learning among nursing students
Young A Song
Korean Journal of Women Health Nursing.2020; 26(1): 61. CrossRef - Simülasyon Uygulamasının Kadın Sağlığı Ve Hastalıkları Hemşireliği Dersi Eğitimine Etkisine İlişkin Öğrenci Görüşlerinin Belirlenmesi
Esra Arslan Gürcüoğlu, Mehtap Uzun Aksoy, Sıdıka Pelit Aksu, Ayten Şentürk Erenel
Kocaeli Üniversitesi Sağlık Bilimleri Dergisi.2019; 5(1): 42. CrossRef - A Comparative Study on Learning Outcomes according to the Integration Sequences of S-PBL in Nursing Students: Randomized Crossover Design
So Young Yun, Ja Yun Choi
Journal of Korean Academy of Nursing.2019; 49(1): 92. CrossRef - Effect of simulation-based training method on the psychological health promotion in operating room students during the educational internship
Gholamreza Mohammadi, Maedeh Tourdeh, Abbasali Ebrahimian
Journal of Education and Health Promotion.2019;[Epub] CrossRef - Effect of Practical Delivery-nursing Simulation Education on Team-based Learning on the Nursing Knowledge, Self-efficacy, and Clinical Competence of Nursing Students
Sun Hee Lee
Korean Journal of Women Health Nursing.2018; 24(2): 150. CrossRef - Policy issues in simulation-based nursing education and technology development
Hyunbong Park, Soyoung Yu
Health Policy and Technology.2018; 7(3): 318. CrossRef - Development and Effects of Simulation Practice Program about Family centered Delivery Care
Seung Hee Yang, Sehoon Hong
Korean Journal of Women Health Nursing.2017; 23(1): 52. CrossRef - The Factor Influencing Problem Solving Ability of Nursing Students in Nursing Simulation Learning
Gyoo-Yeong CHO
JOURNAL OF FISHRIES AND MARINE SCIENCES EDUCATION.2017; 29(4): 1083. CrossRef - Effect of Step-Based Prebriefing Activities on Flow and Clinical Competency of Nursing Students in Simulation-Based Education
Young-Ju Kim, Gie-Ok Noh, Young-Soon Im
Clinical Simulation in Nursing.2017; 13(11): 544. CrossRef - Transforming Magnetic Resonance Imaging Education through Simulation-Based Training
Wiam Elshami, Mohamed Abuzaid
Journal of Medical Imaging and Radiation Sciences.2017; 48(2): 151. CrossRef - Development and Effects of Simulation Program for Fall Management
Mi Yu, Jong Kyung Kim, Se Young Kim, Sung Hyun Cho, Myung Ja Kim, GyeongAe Seomun
Journal of Korean Academy of Nursing Administration.2017; 23(5): 548. CrossRef - Effects of Maternity Nursing Simulation using High-fidelity Patient Simulator for Undergraduate Nursing Students
Ahrin Kim
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(3): 177. CrossRef - Persistence of Integrated Nursing Simulation Program Effectiveness*
Sun-Kyoung Lee, Sun-Hee Kim, Sun-Nam Park
Journal of Korean Academy of Fundamentals of Nursing.2016; 23(3): 283. CrossRef - Influence of Nursing Students’ Anxiety during Simulation Training on Personal Satisfaction of Simulation, Self-efficacy, Clinical Competence
Mi Young Kim, Soohyun Park, Jongsoon Won
Journal of Korean Academy of Fundamentals of Nursing.2016; 23(4): 411. CrossRef - Effects of a Simulation-based High-risk neonatal Care Education on Learning Satisfaction, Class Participation, Learning Motivation and Clinical Competency in Nursing Students
Soon-Gu Kim
Journal of the Korea Academia-Industrial cooperation Society.2015; 16(10): 6807. CrossRef - First experiences of high‐fidelity simulation training in junior nursing students inKorea
Suk Jeong Lee, Sang Suk Kim, Young‐Mi Park
Japan Journal of Nursing Science.2015; 12(3): 222. CrossRef - Effects of Case-Based Learning on Clinical Decision Making and Nursing Performance in Undergraduate Nursing Students*
Mi-Eun Jeong, Hyoung-Sook Park
Journal of Korean Academy of Fundamentals of Nursing.2015; 22(3): 308. CrossRef - Reliability and Validity of the Clinical Judgment Rubric on Simulation Practice with a Post-operative Rehabilitation Case
Hye Kyung Oh
The Korean Journal of Rehabilitation Nursing.2015; 18(2): 145. CrossRef - Development and Effects of Integrated Simulation Program (Maternal-Child) for Nursing Students
Hyun Jung Park, Sun Hee Lee
Child Health Nursing Research.2015; 21(4): 293. CrossRef - The needs and effects of convergence-based simulation practice for obstetrical nursing
Hyun-Ju Chae
Journal of Digital Convergence.2015; 13(9): 377. CrossRef - Perceived Confidence in Practice of Core Basic Nursing Skills of New Graduate Nurses
Yeon-Ha Kim, Seon Young Hwang, Ae-Young Lee
The Journal of Korean Academic Society of Nursing Education.2014; 20(1): 37. CrossRef - Current Status of Women's Health Nursing Practicum and Direction
Jeung-Im Kim, Heesun Kang, Somi Park, Sukhee Ahn
Korean Journal of Women Health Nursing.2014; 20(2): 173. CrossRef - Factors Affecting the Satisfaction of Simulation Education about Emergency Delivery for Paramedic Students
Mi-Lye Baek
Fire Science and Engineering.2014; 28(5): 98. CrossRef - Effect of a simulation-based program for post-operative care of emergency patients
Min-Jeong Chae, Soon-Hee Choi, Jeoung-Suk Kim
The Korean Journal of Emergency Medical Services.2014; 18(3): 91. CrossRef - The Effects of Simulation-Based Training, Underwent Before or After the Clinical Practice for the Nursing Students
Jung Ok Lee
The Journal of Korean Academic Society of Nursing Education.2014; 20(2): 203. CrossRef - Effects of Preceptorship on Nursing Students' Clinical Competency, Stress of Clinical Practice, and Practice Satisfaction in Clinical Practice
Sung-Jung Hong, Eunhee Kim
Journal of the Korea Academia-Industrial cooperation Society.2014; 15(10): 6204. CrossRef - Effects of High-fidelity Simulation-based Education on Nursing Care for Patients with Acute Chest Pain
Sang-Young Han
Journal of the Korea Academia-Industrial cooperation Society.2014; 15(3): 1515. CrossRef - Effect of Simulation-based Practice by applying Problem based Learning on Problem Solving Process, Self-confidence in Clinical Performance and Nursing Competence
Young A Song
Korean Journal of Women Health Nursing.2014; 20(4): 246. CrossRef - Development and Effects of a Simulation-based Education Program for Newborn Emergency Care
So Young Yoo
Journal of Korean Academy of Nursing.2013; 43(4): 468. CrossRef - Development and Evaluation of Simulation-Based Training for Obstetrical Nursing Using Human Patient Simulators
MIOK KIM, MINHO SHIN
CIN: Computers, Informatics, Nursing.2013; 31(2): 76. CrossRef - Systematic Review of Korean Studies on Simulation within Nursing Education
Jung-Hee Kim, In-Hee Park, Sujin Shin
The Journal of Korean Academic Society of Nursing Education.2013; 19(3): 307. CrossRef - Development and Applicability Evaluation of an Emergent Care Management Simulation Practicum for Nursing Students
Hea Kung Hur, SoMi Park, Yoon Hee Shin, Young Mi Lim, GiYon Kim, Ki Kyong Kim, Hyang Ok Choi, Ji Hea Choi
The Journal of Korean Academic Society of Nursing Education.2013; 19(2): 228. CrossRef - Outcomes and Satisfaction of Simulation-based Learning in Nursing of Patient with UGI Bleeding
Eon-Na Ryoo, Yeon Suk Park, Eun-Ho Ha
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(3): 1274. CrossRef - Effects of Simulation-based Education on Communication Skill and Clinical Competence in Maternity Nursing Practicum
Hye Young Kim, Eun Ko, Eun Sook Lee
Korean Journal of Women Health Nursing.2012; 18(4): 312. CrossRef - Effects of Clinical Practice and Simulation-Based Practice for Obstetrical Nursing
Sun-Ae Kim, Sun-Kyung Lee, Hyun Ju Chae
Korean Journal of Women Health Nursing.2012; 18(3): 180. CrossRef
Effects and Adequacy of High-Fidelity Simulation-Based Training for Obstetrical Nursing
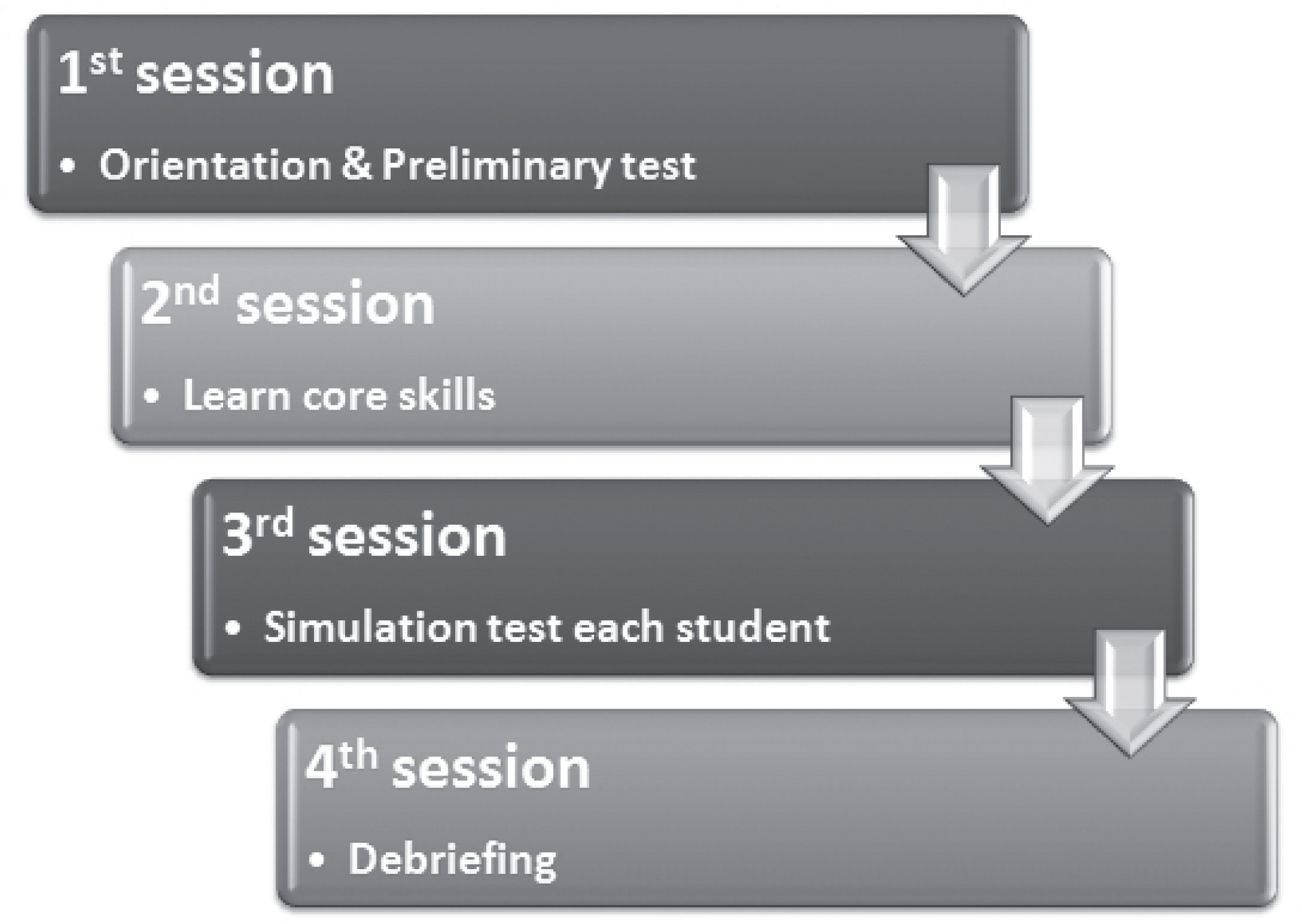
Figure 1. Running process of the simulation-based training.
Figure 1.
Effects and Adequacy of High-Fidelity Simulation-Based Training for Obstetrical Nursing
| Variables | Mean±SD | n (%) |
|---|---|---|
| Age (yr) | 21.3±2.7 | |
| Gender | ||
| Female | 125 (90.6) | |
| Male | 13 (9.4) | |
| Simulation experience | ||
| Yes | 106 (76.8) | |
| No | 31 (22.4) | |
| Satisfaction with the obstetric clinical experience | ||
| Very high | 22 (15.9) | |
| High | 41 (29.7) | |
| Middle | 34 (24.6) | |
| Low | 31 (22.5) | |
| Very Low | 10 (7.2) | |
| Sub-domain | Items | Before simulation |
After simulation |
p |
|---|---|---|---|---|
| Mean±SD | Mean±SD | |||
| Knowledge about clinical situation | Preparation of clients for Leopold’s maneuver | 3.17±0.90 | 3.80±0.75 | <.001 |
| Correct understanding of the relationship between uterine contraction and fetal heart rates | 2.87±0.85 | 3.46±0.92 | <.001 | |
| Correct interpretation of fetal monitoring results | 2.46±0.83 | 3.09±0.94 | <.001 | |
| Thorough understanding of process of labor | 3.01±0.83 | 3.25±0.82 | .003 | |
| Understanding of the clients reaction during labor | 2.98±0.81 | 3.30±0.90 | <.001 | |
| Thorough understanding of postpartum changes (Height of fundus, etc.) | 3.41±0.86 | 3.70±0.77 | .001 | |
| Sub-total | 2.98±0.63 | 3.43±0.64 | <.001 | |
| Precise assessment | Appropriate assessment of clients (physical examination, pain assessment, etc.) | 2.92±0.76 | 3.32±0.85 | <.001 |
| Appropriate intervention | Proper performance for each step of Leopold’s maneuver | 3.06±0.94 | 3.70±0.83 | <.001 |
| Check fetal heart rate at correct location and correct interpretation | 3.01±0.86 | 3.67±0.84 | <.001 | |
| Clear explanation to client about clients’ medical status | 2.67±0.82 | 3.30±0.78 | <.001 | |
| Right position change for the condition of the client | 3.02±0.88 | 3.68±0.86 | <.001 | |
| Appropriate breathing technique according to the clients’ status | 2.78±0.87 | 3.58±0.84 | <.001 | |
| Nursing interventions for anxiety | 3.15±0.91 | 3.60±0.85 | <.001 | |
| Client education for postpartum management | 3.28±0.86 | 3.64±0.78 | <.001 | |
| Proper comfort care for clients | 3.25±0.78 | 3.60±0.89 | <.001 | |
| Privacy protection for the client in all the possible situations | 3.88±0.82 | 3.76±0.97 | .208 | |
| Correct judgement and report on clients’ condition | 2.27±0.79 | 3.21±0.81 | <.001 | |
| Providing nursing care calmly | 3.07±0.78 | 3.33±0.92 | .003 | |
| Sub-total | 3.08±0.60 | 3.55±0.60 | <.001 | |
| Prioritization | Priority nursing care plan according to clients’ condition | 2.68±1.06 | 3.16±0.90 | <.001 |
| Appropriate communication | Appropriate communication with clients and colleagues | 3.28±0.71 | 3.53±0.83 | .001 |
| Total | 3.03±0.58 | 3.48±0.60 | <.001 |
| Sub-domain | Items | Mean±SD |
|---|---|---|
| Relevance of the simulation learning process | ||
| Simulation-based training increased confidence in nursing | 7.31±1.74 | |
| Simulations were realistic | 7.38±1.84 | |
| Simulation helped to establish nursing goals for clients | 7.27±1.74 | |
| Simulation-based training increased students’ interest in women’s health nursing | 8.33±1.26 | |
| Simulation-based training may help nursing practice in the future | 8.01±1.90 | |
| Total | 7.17±1.38 | |
| Adequacy of simulation-based training in each session | ||
| Orientation & Preliminary test | Orientation helped in understanding the simulation program | 7.09±1.91 |
| The goal of the simulation program was made clear | 7.44±1.84 | |
| The simulation scenarios were easily understood | 6.79±1.72 | |
| 7.10±1.52 | ||
| Learning core skills | Open Lab was properly used for simulation preparation | 6.30±2.39 |
| Simulation test | Students could confirm abnormal status of clients through simulation | 7.01±1.68 |
| Students could prioritize nursing interventions during the simulation | 6.49±1.73 | |
| Students knew what should be done to resolve clients’ problems | 6.32±1.79 | |
| Students could perform correct procedure for nursing skills | 6.30±1.76 | |
| 6.52±1.48 | ||
| Debriefing | Constructive feedback was given after simulation | 7.75±1.78 |
| Debriefing helped the student identify his or her strength | 7.29±1.85 | |
| Debriefing helped to identify the weakness of the student | 8.12±1.71 | |
| 7.72±1.55 | ||
| Total | 6.99±1.36 | |
| Relevance of the simulation learning environment | ||
| The installation and equipment of the simulation program were appropriate | 7.95±1.83 | |
| The duration of the simulation tests were appropriate | 7.61±1.81 | |
| The simulation tests were interesting enough to hold students’ attentio | 7.53±1.95 | |
| Appropriate nursing information was provided during the simulation program | 7.33±1.67 | |
| Total | 7.60±1.60 | |
| Total | 7.15±1.35 | |
Table 1. General Characteristics of Participants (N=138)
Table 2. Self-confidence about Clinical Practices for Obstetric Nursing (N=138
Table 3. Adequacy of Simulation-based Training (N=138
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

