Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 46(1); 2016 > Article
-
Original Article
- Chemotherapy-related Cognitive Impairment and Quality of Life in People with Colon Cancer: The Mediating Effect of Psychological Distress
- Pok Ja Oh, Jeong Hye Kim
-
Journal of Korean Academy of Nursing 2016;46(1):19-28.
DOI: https://doi.org/10.4040/jkan.2016.46.1.19
Published online: February 29, 2016
1Department of Nursing, Sahmyook University, Seoul, Korea.
2Department of Clinical Nursing, University of Ulsan, Seoul, Korea.
- Address reprint requests to: Kim, Jeong Hye. Department of Clinical Nursing, University of Ulsan, 88 Olympic-ro 43 gil, Songpa-gu, Seoul 05505, Korea. Tel: +82-2-3010-5335, Fax: +82-2-3010-5332, kimjh@amc.seoul.kr
© 2016 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- The purpose of this study was to test the mediating effect of psychological distress in the relationship between chemotherapy related cognitive impairment (CRCI) and quality of life (QOL) in people with cancer.
-
Methods
- A purposive sample of 130 patients undergoing chemotherapy was recruited for the cross-sectional survey design. Data were collected from November 2014 to June 2015. The instruments were K-MMSE (Korean Mini-Mental State Examination), Everyday Cognition (ECog), Hospital Anxiety Depression Scale (HADS), and Functional Assessment of Cancer Therapy-General (FACT-G). Data were analyzed using descriptive statistics, correlation, and multiple regression using Baron and Kenny steps for mediation.
-
Results
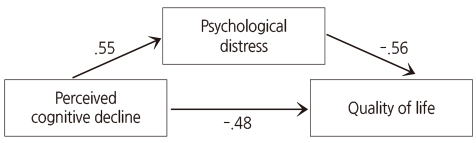
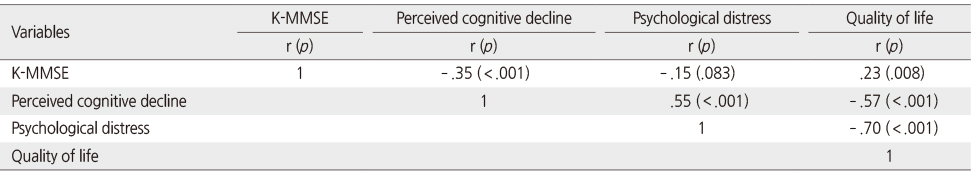
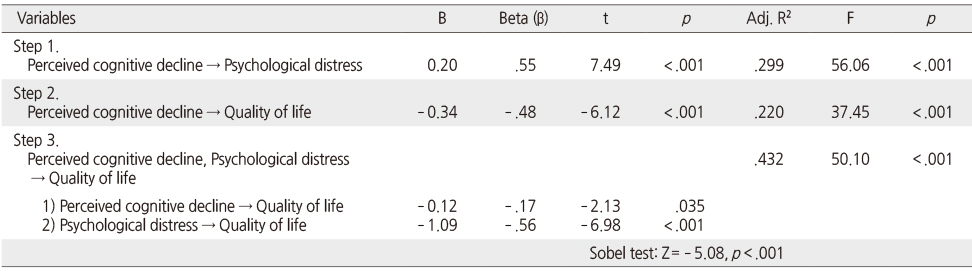
- The mean score for objective cognitive function was 27.95 and 69.32 for perceived cognitive decline. Overall quality of life was 91.74. The mean score was 17.52 for psychological distress. The prevalence was 56.2% for anxiety and 63.1% for depression, and 20.0% for CRCI. There were significant correlations among the variables, objective cognitive function and self-reported cognitive decline, psychological distress, and quality of life. Psychological distress was directly affected by CRCI. (R2=29%). QOL was directly affected by CRCI. Psychological distress and CRCI effected QOL (R2=43%). Psychological distress had a partial mediating effect (β= -.56, p <.001) in the relationship between self-reported cognitive decline and quality of life (Sobel test: Z= -5.08, p <.001).
-
Conclusion
- Based on the findings of this study, nursing intervention programs focusing on managing cognitive decline, and decreasing psychological distress are highly recommended to improve quality of life in cancer patients.
Acknowledgments
ACKNOWLEDGMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No.2014R1A1A2053517).
The authors declared no conflict of interest.
- 1. Ministry of Health & Welfare. Korea Central Cancer Registry. National Cancer Center. Annual report of cancer statistics in Korea in 2012. Seoul: Ministry of Health & Welfare; 2014.
- 2. Gehring K, Roukema JA, Sitskoorn MM. Review of recent studies on interventions for cognitive deficits in patients with cancer. Expert Rev Anticancer Ther. 2012;12(2):255–269. ArticlePubMed
- 3. Schagen SB, Muller MJ, Boogerd W, Mellenbergh GJ, van Dam FS. Change in cognitive function after chemotherapy: A prospective longitudinal study in breast cancer patients. J Natl Cancer Inst. 2006;98(23):1742–1745. ArticlePubMed
- 4. Gilroy J. Basic neurology. 3rd ed. New York, NY: McGraw-Hill Professional Publishing; 2000.
- 5. de Ruiter MB, Reneman L, Boogerd W, Veltman DJ, Caan M, Douaud G, et al. Late effects of high-dose adjuvant chemotherapy on white and gray matter in breast cancer survivors: Converging results from multimodal magnetic resonance imaging. Human Brain Mapping. 2012;33(12):2971–2983. ArticlePubMed
- 6. Hutchinson AD, Hosking JR, Kichenadasse G, Mattiske JK, Wilson C. Objective and subjective cognitive impairment following chemotherapy for cancer: A systematic review. Cancer Treat Rev. 2012;38(7):926–934. ArticlePubMed
- 7. Hess LM, Insel KC. Chemotherapy-related change in cognitive function: A conceptual model. Oncol Nurs Forum. 2007;34(5):981–994. ArticlePubMed
- 8. Wefel JS, Kayl AE, Meyers CA. Neuropsychological dysfunction associated with cancer and cancer therapies: A conceptual review of an emerging target. Br J Cancer. 2004;90(9):1691–1696. ArticlePubMedPMCPDF
- 9. Jenkins V, Shilling V, Deutsch G, Bloomfield D, Morris R, Allan S, et al. A 3-year prospective study of the effects of adjuvant treatments on cognition in women with early stage breast cancer. Br J Cancer. 2006;94(6):828–834. ArticlePubMedPMCPDF
- 10. Pullens MJ, De Vries J, Roukema JA. Subjective cognitive dysfunction in breast cancer patients: A systematic review. Psychooncology. 2010;19(11):1127–1138. ArticlePubMed
- 11. National Cancer Information Center. Recommendations for distress management in cancer patients, version 1.0 [Internet]. Seoul, Ministry for Health, Welfare and Family Affairs. 2008;cited 2012 October 8. Available from: http://www.cancer.go.kr/2010/04/22/Recommendations_Distress_Management_version1.pdf
- 12. Pasquini M, Biondi M. Depression in cancer patients: A critical review. Clin Pract Epidemiol Ment Health. 2007;3:2ArticlePubMedPMC
- 13. Oh PJ, Jang ES. Effects of psychosocial interventions on cortisol and immune parameters in patients with cancer: A meta-analysis. J Korean Acad Nurs. 2014;44(4):446–457. ArticlePubMed
- 14. Lange M, Rigal O, Clarisse B, Giffard B, Sevin E, Barillet M, et al. Cognitive dysfunctions in elderly cancer patients: A new challenge for oncologists. Cancer Treat Rev. 2014;40(6):810–817. ArticlePubMed
- 15. Chung BY, Cho EJ. Correlates influencing cognitive impairment in breast cancer patients receiving chemotherapy. Asian Oncol Nurs. 2012;12(3):221–229. ArticlePDF
- 16. Park JH, Bae SH, Jung YS, Jung YM. Prevalence and characteristics of chemotherapy-related cognitive impairment in patients with breast cancer. J Korean Acad Nurs. 2015;45(1):118–128. ArticlePubMedPDF
- 17. Kaiser J, Bledowski C, Dietrich J. Neural correlates of chemotherapy-related cognitive impairment. Cortex. 2014;54:33–50. ArticlePubMed
- 18. Kang Y. A normative study of the Korean-Mini Mental State Examination (K-MMSE) in the elderly. Korean J Psychol. 2006;25(2):1–12.
- 19. Prabhu RS, Won M, Shaw EG, Hu C, Brachman DG, Buckner JC, et al. Effect of the addition of chemotherapy to radiotherapy on cognitive function in patients with low-grade glioma: Secondary analysis of RTOG 98-02. J Clin Oncol. 2014;32(6):535–541. ArticlePubMedPMC
- 20. Oh SM, Min KJ, Park DB. A study on the standardization of the hospital anxiety and depression scale for Koreans: A comparison of normal, depressed and anxious groups. J Korean Neuropsychiatr Assoc. 1999;38(2):289–296.
- 21. Kim H, Yoo HJ, Kim YJ, Han OS, Lee KH, Lee JH, et al. Development and validation of Korean functional assessment cancer therapy-general (FACT-G). Korean J Clin Psychol. 2003;22(1):215–229.
- 22. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Person Soc Psychol. 1986;51(6):1173–1182.Article
- 23. Pereira J, Hanson J, Bruera E. The frequency and clinical course of cognitive impairment in patients with terminal cancer. Cancer. 1997;79(4):835–842.ArticlePubMed
- 24. Park JH, Bae SH. A meta-analysis of chemotherapy related cognitive impairment in patients with breast cancer. J Korean Acad Nurs. 2012;42(5):644–658. ArticlePubMed
- 25. Meyers CA, Wefel JS. The use of the mini-mental state examination to assess cognitive functioning in cancer trials: No ifs, ands, buts, or sensitivity. J Clin Oncol. 2003;21(19):3557–3558. ArticlePubMed
- 26. Hall KE, Isaac CL, Harris P. Memory complaints in epilepsy: An accurate reflection of memory impairment or an indicator of poor adjustment? A review of the literature. Clin Psychol Rev. 2009;29(4):354–367. ArticlePubMed
- 27. Hutter N, Vogel B, Alexander T, Baumeister H, Helmes A, Bengel J. Are depression and anxiety determinants or indicators of quality of life in breast cancer patients? Psycho Health Med. 2013;18(4):412–419. Article
- 28. Baek Y. The correlation among symptoms, anxiety, depression and quality of life in patients with colorectal cancer undergoing chemotherapy [master's thesis]. Seoul, Seoul National University. 2013.
- 29. Park JH, Jun EY, Kang MY, Joung YS, Kim GS. Symptom experience and quality of life in breast cancer survivors. J Korean Acad Nurs. 2009;39(5):613–621. ArticlePubMed
REFERENCES
Mediating effect of psychological distress in the relationship between perceived cognitive decline and quality of life.
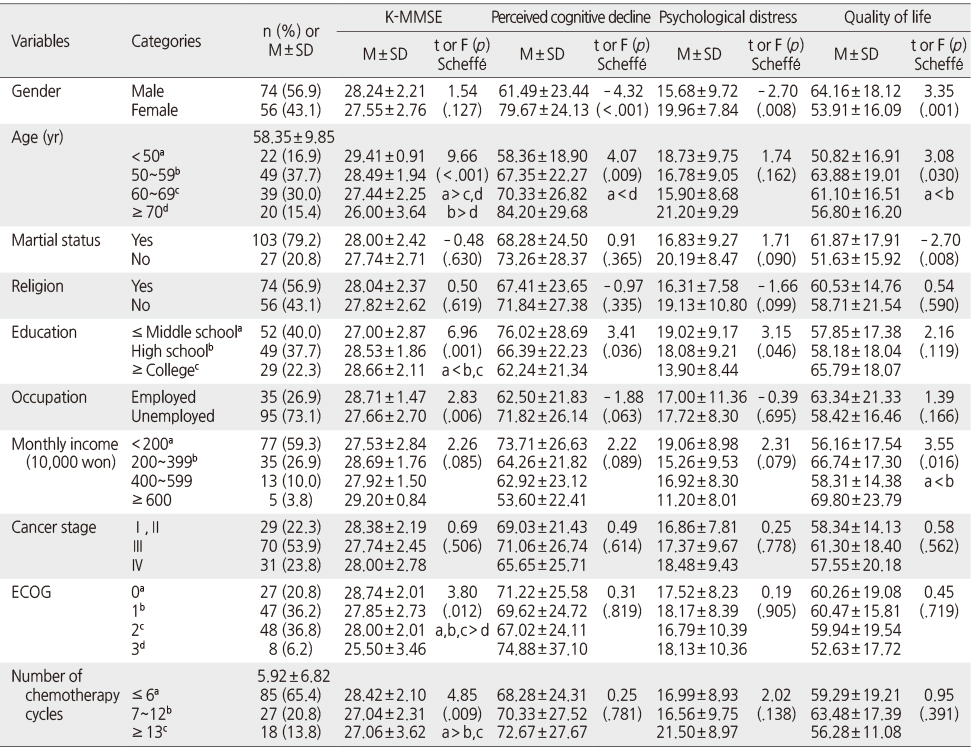
Cognitive Function, Psychological Distress, and Quality of Life according to General Characteristics of Participants (N =130)
Descriptive Statistics of K-MMSE Scores, Perceived Cognitive Decline, Psychological Distress, and Quality of Life (N =130)
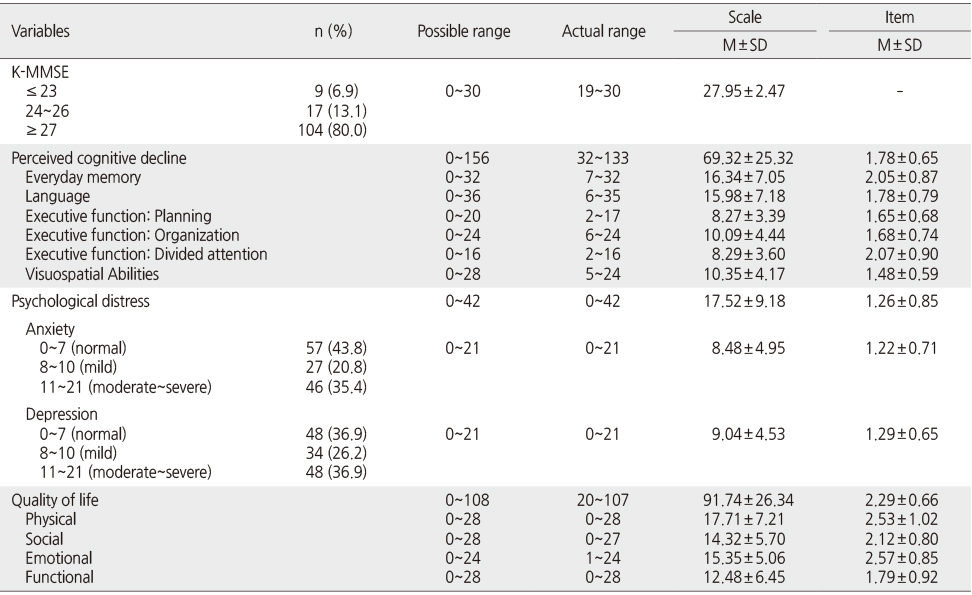
Figure & Data
REFERENCES
Citations

- Association of Physical Activity with Dementia Risk in Cancer Survivors: A Korean Nationwide Cohort Study
Su Kyoung Lee, Minji Han, Sangwoo Park, Sun Jae Park, Jihun Song, Hye Jun Kim, Jaewon Kim, Hyeokjong Lee, Hyun-Young Shin, Kyae Hyung Kim, Sang Min Park
Cancer Research and Treatment.2026; 58(1): 48. CrossRef - Self-disclosure in Adult Patients With Cancer
Hyungran Lee, Younhee Jeong
Cancer Nursing.2025; 48(4): 289. CrossRef - NYHA classification deterioration and quality of life in heart failure inpatients: A chain mediation analysis of cognitive impairment and depression
Jin Yang, You Pu, Mingjun He, Tianyi Wang, Ting Ye, Yunman Huang, Yunfeng Di, Xianqin Zhang, Zheng Yang
Heart & Lung.2025; 73: 95. CrossRef - Disease Perception, Stigma, Distress, Physical Symptom Experience and Quality of Life in Colorectal Cancer Patients Undergoing Chemotherapy: A Cross-Sectional Study
Eun-Hee Lee, Dongwon Choi
Journal of Korean Academy of Fundamentals of Nursing.2024; 31(4): 494. CrossRef - Aldehyde dehydrogenase 2 polymorphism is associated with chemotherapy‐related cognitive impairment in patients with breast cancer who receive chemotherapy
Senbang Yao, Wen Li, Shaochun Liu, Yinlian Cai, Qianqian Zhang, Lingxue Tang, Sheng Yu, Yanyan Jing, Xiangxiang Yin, Huaidong Cheng
Cancer Medicine.2023; 12(5): 5209. CrossRef - Factors Associated with Self-reported Memory Problems of Adult Cancer Survivors Based on the Korea National Health and Nutrition Examination Survey 2019
Sangjin Ko
Journal of Health Informatics and Statistics.2023; 48(1): 51. CrossRef - Colon Cancer Survivorship in Patients Who Have Received Adjuvant Chemotherapy
Meghana Kesireddy, Laura Tenner
Clinical Colorectal Cancer.2023; 22(4): 361. CrossRef - Predictors of cognitive impairment in patients undergoing ileostomy for colorectal cancer: a retrospective analysis
Jing Xu, Yuelan Yang, Die Hu
PeerJ.2023; 11: e15405. CrossRef - Symptom Experience, Social Support, and Quality of Life in Patients with Hematologic Malignancies Undergoing Chemotherapy
Ga Eun Kim, Ju-Eun Song, Mi-Ae You, Jin-Hee Park
Asian Oncology Nursing.2022; 22(1): 29. CrossRef - Effect of Ambulatory Chemotherapy (Portable Infusion Pump Use) Video Education on Knowledge, Self-efficacy and Anxiety of Colorectal Cancer Patients
Eun Hee Choi, Eun Young Park, Young A Park, You Hee Son, Myung Jin Jang
Asian Oncology Nursing.2022; 22(3): 193. CrossRef - A pilot retrospective study of comprehensive nursing care on psychological disorder in colorectal cancer undergoing chemotherapy
Zhou-Yi Zhang, Rui Wang, Li Zhang, Ming-Li Gu, Xiu-E Guan
Medicine.2022; 101(28): e29707. CrossRef - The Experience of Chemotherapy Related Cognitive Impairment in Patients with Cancer
Pok Ja Oh, Ji Hyun Kim
Asian Oncology Nursing.2022; 22(1): 1. CrossRef - The Mediating Effect of Depression on the Relationship between Cognitive Function and the Activities of Daily Living in Post-stroke Patient
Ji Eun Kim, Hwee Wee
Journal of Korean Academy of psychiatric and Mental Health Nursing.2021; 30(4): 309. CrossRef - A serial multiple mediator model of sense of coherence, coping strategies, depression, and quality of life among gynecologic cancer patients undergoing chemotherapy
Hee Sun Kim, Ju-Hee Nho, Joo-Hyun Nam
European Journal of Oncology Nursing.2021; 54: 102014. CrossRef - Impact of changes in perceived attentional function on postsurgical health-related quality of life in breast cancer patients awaiting adjuvant treatment
Mi Sook Jung, Moira A. Visovatti, Eun Hee Sohn, Hwa-Seung Yoo, Mijung Kim, Je Ryong Kim, Jin Sun Lee
Health and Quality of Life Outcomes.2020;[Epub] CrossRef - Factors influencing quality of life in patients with multiple myeloma
Hee-Young Kang, Eun-Young Choi
Contemporary Nurse.2019; 55(2-3): 109. CrossRef - The role of depression in the relationship between cognitive decline and quality of life among breast cancer patients
Jin-Hee Park, Yong Sik Jung, Young-Mi Jung, Sun Hyoung Bae
Supportive Care in Cancer.2019; 27(7): 2707. CrossRef - A Longitudinal Path Analysis of Symptom, Fatigue and Quality of life in Patients with Colorectal Cancer during Chemotherapy
Eun Hee Kim, Soon Rim Suh
Journal of Health Informatics and Statistics.2018; 43(3): 200. CrossRef - Factors Affecting Cognitive Function in Patients with Stomach Cancer
Yeoung Ji Yu, Seung Hee Ahn, Yong Ae Cho, Eunjung Ryu, Eun-Ju Kim
Asian Oncology Nursing.2018; 18(4): 241. CrossRef - Serum lipid changes following the onset of depressive symptoms in postmenopausal women
Jane E. Persons, Jennifer G. Robinson, Martha E. Payne, Jess G. Fiedorowicz
Psychiatry Research.2017; 247: 282. CrossRef - Development of the Cognitive Function Scale for Breast Cancer Patients
Bok Yae Chung, Eun Hee Choi, Gyung Duck Kim, Kyung Hae Kim, Hye Sun Byun
Asian Oncology Nursing.2017; 17(1): 12. CrossRef
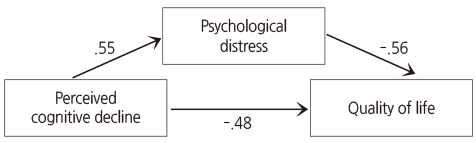
Figure 1
Cognitive Function, Psychological Distress, and Quality of Life according to General Characteristics of Participants (N =130)
ECOG=Eastern cooperative oncology group; K-MMSE=Korean mini–mental state examination.
Descriptive Statistics of K-MMSE Scores, Perceived Cognitive Decline, Psychological Distress, and Quality of Life (N =130)
K-MMSE=Korean mini–mental state examination.
Correlations among K-MMSE Scores, Perceived Cognitive Decline, Psychological Distress, and Quality of Life (N =130)
K-MMSE=Korean mini–mental state examination.
Mediating Effect of Psychological Distress in the Relationship between Perceived Cognitive Decline and Quality of Life (N =130)
ECOG=Eastern cooperative oncology group; K-MMSE=Korean mini–mental state examination.
K-MMSE=Korean mini–mental state examination.
K-MMSE=Korean mini–mental state examination.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

