Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 43(5); 2013 > Article
-
Original Article
- Effect of PLISSIT Model Sexual Health Enhancement Program for Women with Gynecologic Cancer and Their Husbands
- Ju-Hee Nho
-
Journal of Korean Academy of Nursing 2013;43(5):681-689.
DOI: https://doi.org/10.4040/jkan.2013.43.5.681
Published online: October 31, 2013
Department of Nursing, University of Ulsan, Ulsan, Korea.
- Address reprint requests to: Nho, Ju-Hee. Department of Nursing, University of Ulsan, 93 Daehakro, Nam-gu, Ulsan 680-749, Korea. Tel: +82-10-9703-7092, Fax: +82-259-1236, jhnho@ulsan.ac.kr
© 2013 Korean Society of Nursing Science
Abstract
-
Purpose
- The purpose of this study was to examine effects of the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISSIT) model sexual health enhancement program on, and development in, sexual function, sexual distress, marital intimacy, and subjective happiness of women with gynecologic cancer and their husbands.
-
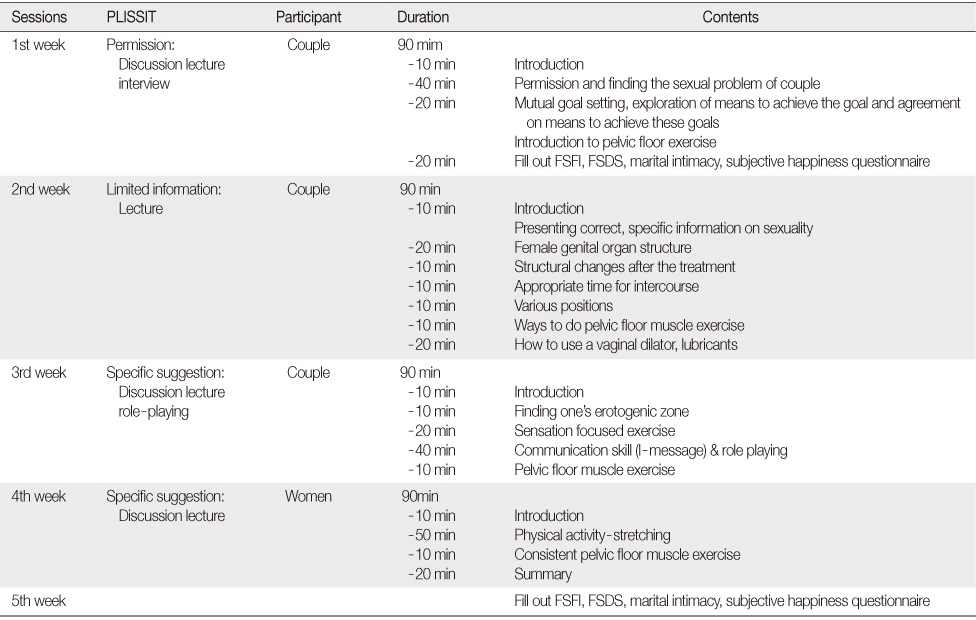
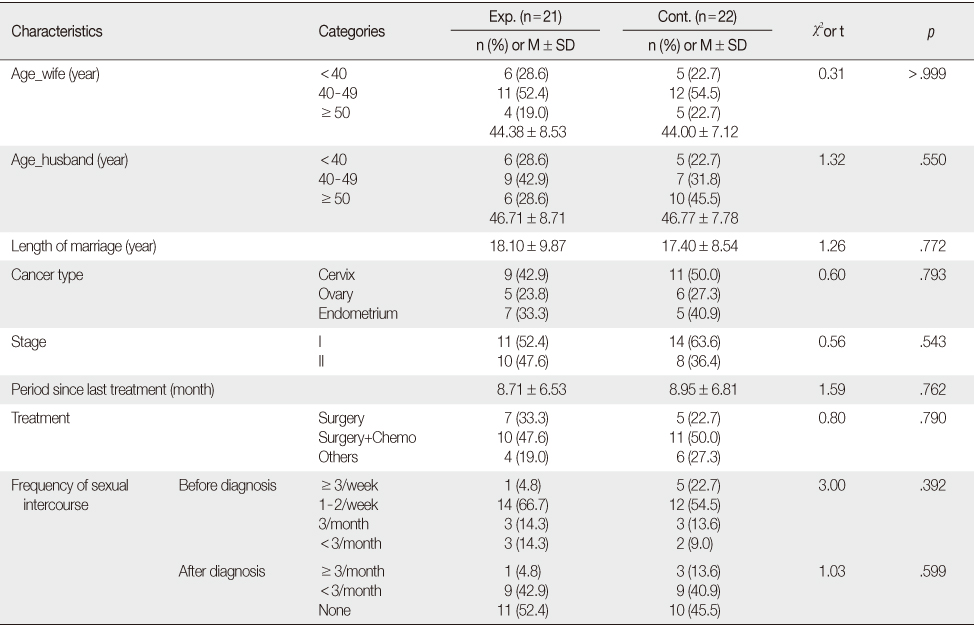
Methods
- The comprehensive program (4 session, 90 minutes per session) was developed based on the PLISSIT model. Participants were 43 couples, 21 assigned to the experimental group who attended the 4-week program, and 22 to the control group. Sexual function, sexual distress, marital intimacy, subjective happiness of the women, marital intimacy, subjective happiness of husbands were determined by a questionnaire that was completed by the participants before and after the program. The control group received the intervention post experiment. Chi-square test, t-test, Fisher's exact test were used to test the effectiveness of the program.
-
Results
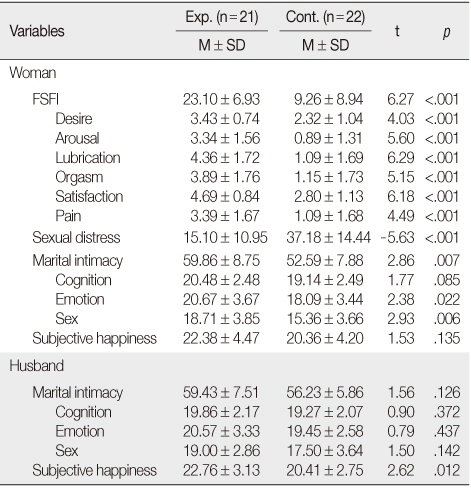
- Post intervention results showed significant differences between the groups for sexual function, sexual distress, and marital intimacy in the women and for subjective happiness in the husbands.
-
Conclusion
- Results indicate that the sexual health enhancement program is effective in improving sexual function, lowering sexual distress, increasing marital intimacy, and subjective happiness in women with gynecologic cancer and their husbands.
This manuscript is a revision of the first author's doctoral dissertation from Seoul National University.
- 1. Anderson B, Anderson JE, Yi MY. Stretching. Seoul: Nexusbook; 2001.
- 2. Annon JS. Behavioural treatment of sexual problems: Brief therapy. Hagerstown, MD: Joanna Cotler Books; 1977.
- 3. Brotto LA, Heiman JR, Goff B, Greer B, Lentz GM, Swisher E, et al. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch Sex Behav. 2008;37(2):317–329. http://dx.doi.org/10.1007/s10508-007-9196-xArticlePubMedPDF
- 4. Chun N. A structural equation model on sexual function in women with gynecologic cancer. J Korean Acad Nurs. 2008;38(5):639–648. http://dx.doi.org/10.4040/jkan.2008.38.5.639ArticlePubMed
- 5. Chun N. Effectiveness of PLISSIT model sexual program on female sexual function for women with gynecologic cancer. J Korean Acad Nurs. 2011;41(4):471–480. http://dx.doi.org/10.4040/jkan.2011.41.4.471ArticlePubMed
- 6. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
- 7. Derogatis LR, Rosen R, Leiblum S, Burnett A, Heiman J. The female sexual distress scale (FSDS): Initial validation of a standardized scale for assessment of sexually related personal distress in women. J Sex Marital Ther. 2002;28(4):317–330.ArticlePubMed
- 8. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191.ArticlePubMedPDF
- 9. Han C, Kim HC, Kang SH, Moon DG, Kim JJ, Choi JY. Validity and reliability of Korean version of the female sexual distress scale (FSDS). Korean J Androl. 2004;22(2):68–74.
- 10. Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2003;56(4):937–949.ArticlePubMed
- 11. Juraskova I, Butow P, Robertson R, Sharpe L, McLeod C, Hacker N. Post-treatment sexual adjustment following cervical and endometrial cancer: A qualitative insight. Psychooncology. 2003;12(3):267–279. http://dx.doi.org/10.1002/pon.639ArticlePubMed
- 12. Kalaitzi C, Papadopoulos VP, Michas K, Vlasis K, Skandalakis P, Filippou D. Combined brief psychosexual intervention after mastectomy: Effects on sexuality, body image, and psychological well-being. J Surg Oncol. 2007;96(3):235–240. http://dx.doi.org/10.1002/jso.20811ArticlePubMed
- 13. Katz A. Breaking the silence on cancer and sexuality: A handbook for healthcare providers. Pittsburgh, PA: Oncology Nursing Society; 2007.
- 14. Katz A. Woman cancer sex. Pittsburgh, PA: Hygeia Media; 2009.
- 15. King IM. A theory for nursing: Systems, concepts, process. New York, NY: Wiley; 1981.
- 16. Laumann EO, Paik A, Glasser DB, Kang JH, Wang T, Levinson B, et al. A cross-national study of subjective sexual well-being among older women and men: Findings from the global study of sexual attitudes and behaviors. Arch Sex Behav. 2006;35(2):145–161. http://dx.doi.org/10.1007/s10508-005-9005-3ArticlePubMedPDF
- 17. Lee KH. A measure of marital intimacy. J Korean Home Econ Assoc. 1995;33(4):235–249.
- 18. Lim JS. The relationships of a self-enhancement bias, life events and subjective well-being in old-adults. Seoul, Ewha Womans University. 2004;Unpublished master's thesis.
- 19. Lyubomirsky S, Lepper HS. A measure of subjective happiness: Preliminary reliability and construct validation. Soc Indic Res. 1999;46(2):137–155.ArticlePDF
- 20. Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K. Couples' support-related communication, psychological distress, and relationship satisfaction among women with early stagebreast cancer. J Consult Clin Psychol. 2004;72(4):660–670. http://dx.doi.org/10.1037/0022-006x.72.4.660ArticlePubMed
- 21. Masters WH, Johnson VE. Human sexual inadequacy. Boston, MA: Little, Brown; 1970.
- 22. Nho JH, Park YS. Descriptive study on sexuality for women with gynecological cancer. Korean J Women Health Nurs. 2012;18(1):17–27. http://dx.doi.org/10.4069/kjwhn.2012.18.1.17ArticlePubMed
- 23. Park JS, Lee YE. Effects of integrated menopause management program for middle aged woman. Korean J Women Health Nurs. 2011;17(1):10–20. http://dx.doi.org/10.4069/kjwhn.2011.17.1.10ArticlePubMed
- 24. Park YS, Cho IS, Kim YM. A survey of urban middle-aged women's sexual function and sexual distress. Korean J Women Health Nurs. 2007;13(4):254–261.ArticlePDF
- 25. Rivalta M, Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, Grande M, et al. Biofeedback, electrical stimulation, pelvic floor muscle exercises, and vaginal cones: A combined rehabilitative approach for sexual dysfunction associated with urinary incontinence. J Sex Med. 2009;6(6):1674–1677. http://dx.doi.org/10.1111/j.1743-6109.2009.01238.xArticlePubMedPDF
- 26. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. http://dx.doi.org/10.1080/009262300278597ArticlePubMed
- 27. Scott JL, Halford WK, Ward BG. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol. 2004;72(6):1122–1135. http://dx.doi.org/10.1037/0022-006x.72.6.1122ArticlePubMed
REFERENCES
Figure & Data
REFERENCES
Citations

- The Effect of Sexual Education Program on Sexual Function and Genital Self-image, Sexual Quality of Life among Primiparous Women
Athar Rasekh Jahromi, Hanie Jafari, Parvin Adedi, Mojgan Javadnoori, Solmaz Mohammadi, Vahid Rahmanian, Safieh Jamali
Current Womens Health Reviews.2025;[Epub] CrossRef - Effects of a sexual health enhancement program for women with breast cancer: A quasi-experimental study
Hye Sook Kim, Chaewon Yun
European Journal of Oncology Nursing.2025; 76: 102852. CrossRef - Factors Influencing Quality of Life in Pregnant Women With Preterm Labor
So Jin Lee, Ju-Hee Nho, Eun Jee Lee, Dong Hyun Lee
Journal of Korean Maternal and Child Health.2025; 29(2): 87. CrossRef - The effectiveness of couple-based interventions on the marital outcomes of women with genital and breast cancer and their partners: a systematic review and meta-analysis
Hamideh Zahedi, Zohreh Alizadeh-Dibazari, Mojgan Mirghafourvand, Mohammad Hasan Sahebihagh, Mina Hosseinzadeh
BMC Cancer.2024;[Epub] CrossRef - Feasibility and effectiveness of communication tools for addressing intimacy and sexuality in patients with cancer: a systematic review
Susanne A. M. Arends, Carlijn E. van Rossum, Corien M. Eeltink, Jantien E. Robertus, Linda J. Schoonmade, Anneke L. Francke, Irene P. Jongerden
Supportive Care in Cancer.2024;[Epub] CrossRef - The Effect of Sexual Counseling Based on PLISSIT and EX-PLISSIT Models on Sexual Function, Satisfaction, and Quality of Life: A Systematic Review and Meta-Analysis
Sevil Cicek Ozdemir, Aliye Dogan Gangal, Ayten Senturk Erenel
Archives of Sexual Behavior.2024; 53(9): 3485. CrossRef - The Effect of Sexual Counseling Based on EX‑PLISSIT Model on Improving the Sexual Function of Married Women with Systemic Lupus Erythematosus: A Randomized Controlled Trial
Maryam Shami, Ali Montazeri, Seyedeh Tahereh Faezi, Zahra Behboodi Moghadam
Sexuality and Disability.2023; 41(2): 451. CrossRef - The Effect of Post-Operative Sexual Counseling Carried out with PLISSIT Model on Sexual Function and Sexual Satisfaction in Gynecologic Cancers
Çiğdem BİLGE, Ergül ASLAN
Clinical and Experimental Health Sciences.2023; 13(3): 623. CrossRef - The effect of a psycho-educational intervention on sexuality of women with acute coronary syndromes: a randomized controlled trial
Fatemeh Soleimaninejad, Razieh Lotfi, Mehdi Mousavi, Majid Taghizadeh, Kourosh Kabir
Sexual and Relationship Therapy.2023; 38(2): 277. CrossRef - Sexual health outcomes of PLISSIT-based counseling versus grouped sexuality education among Iranian women with breast cancer: A randomized clinical trial
Effat Merghati Khoei, Rhoghieh Kharaghani, Elham Shakibazadeh, Soghrat Faghihzadeh, Noura Aghajani, Jeffrey E. Korte, Mina Esmkhani
Sexual and Relationship Therapy.2022; 37(4): 557. CrossRef - Effects of the Better Model Based Counseling on Sexuality of Women with Breast Cancer
Zeynep Ozkan Olcer, Umran Oskay
International Journal of Sexual Health.2022; 34(1): 41. CrossRef - The effect of PLISSIT based counseling model on sexual function, quality of life, and sexual distress in women surviving breast cancer: a single-group pretest–posttest trial
Zohreh Keshavarz, Elham Karimi, Samira Golezar, Giti Ozgoli, Maliheh Nasiri
BMC Women's Health.2021;[Epub] CrossRef - Development and Evaluation of a Sexual Health Improvement Program for Women with Gynecologic Cancer
Soon Yang Jang
Asian Oncology Nursing.2021; 21(3): 163. CrossRef - Effects of Nurse-Led Intervention Programs Based on Goal Attainment Theory: A Systematic Review and Meta-Analysis
Bom-Mi Park
Healthcare.2021; 9(6): 699. CrossRef - The Effect of the PLISSIT Model on Sexual Functions: A Systematic Review
Serap KIRICI, Emel EGE
Bandırma Onyedi Eylül Üniversitesi Sağlık Bilimleri ve Araştırmaları Dergisi.2021; 3(3): 199. CrossRef - Sexual Health Outcomes of PLISSIT-based Counseling versus Grouped Sexuality
Education among Iranian Women with Breast Cancer: A Randomized Clinical Trial
Medical & Clinical Research.2019;[Epub] CrossRef - PLISSIT Interventions and Sexual Functioning: Useful Tools for Social Work in Palliative Care?
Michael R. Bennett
Journal of Social Work in End-of-Life & Palliative Care.2019; 15(4): 157. CrossRef - Effect of a Web-Based Sexual Health Enhancement Program for Women with Gynecologic Cancer and Their Husbands
Ju-Hee Nho, Yeon Hee Kim, Hye-Ji Kook
International Journal of Sexual Health.2019; 31(1): 50. CrossRef - Oncology Nurses' Knowledge Regarding Fertility Preservation for Patients with Cancer
Miok Kim, Ju-Hee Nho, Aeran Lee
Korean Journal of Adult Nursing.2019; 31(3): 315. CrossRef - The Influence of Ex-PLISSIT (Extended Permission, Limited Information, Specific Suggestions, Intensive Therapy) Model on Intimacy and Sexuality of Married Women with Multiple Sclerosis
Fatemeh Daneshfar, Zahra Behboodi-Moghadam, Zohreh Khakbazan, Seyed Massood Nabavi, Nahid Dehghan Nayeri, Sogand Ghasemzadeh, Ali Montazeri
Sexuality and Disability.2017; 35(4): 399. CrossRef - Development of a Web-based Sexual Health Program for Women Undergoing Treatment for Gynecologic Cancer and Their Partners
Ju-Hee Nho
Korean Journal of Women Health Nursing.2016; 22(2): 104. CrossRef - The effectiveness of the Permission, Limited Information, Specific suggestions, Intensive Therapy (PLISSIT) model based sexual counseling on the sexual function of women with Multiple Sclerosis who are sexually active
Zohreh Khakbazan, Fatemeh. Daneshfar, Zahra Behboodi-Moghadam, Seyed Massood Nabavi, Sogand Ghasemzadeh, Abbas Mehran
Multiple Sclerosis and Related Disorders.2016; 8: 113. CrossRef - Comments on female sexual dysfunction with cervical cancer in Republic of Korea
Gyeong-Eun Heo, Tae-Hee Kim, Hae-Hyeog Lee, Jun-Mo Kim
Archives of Gynecology and Obstetrics.2016; 294(1): 209. CrossRef - Reply to letter to the editor by J.-M. Kim et al. on "Sexual function and quality of life in women with cervical cancer before radiotherapy: a pilot study" by Grion et al.
R. C. Grion, Luiz Francisco Baccaro, A. F. Vaz, L. Costa-Paiva, D. M. Conde, A. M. Pinto-Neto
Archives of Gynecology and Obstetrics.2016; 294(1): 211. CrossRef - Interventions for sexual dysfunction following treatments for cancer in women
Bridget Candy, Yuan Chi, Lisa Graham-Wisener, Louise Jones, Michael King, Anne Lanceley, Victoria Vickerstaff, Adrian Tookman
Cochrane Database of Systematic Reviews.2016;[Epub] CrossRef - Effects of Lifestyle Intervention on Fatigue, Nutritional Status and Quality of Life in Patients with Gynecologic Cancer
Hyunjin An, Ju-Hee Nho, Sunyoung Yoo, Hyunmin Kim, Minji Nho, Hojeong Yoo
Journal of Korean Academy of Nursing.2015; 45(6): 812. CrossRef
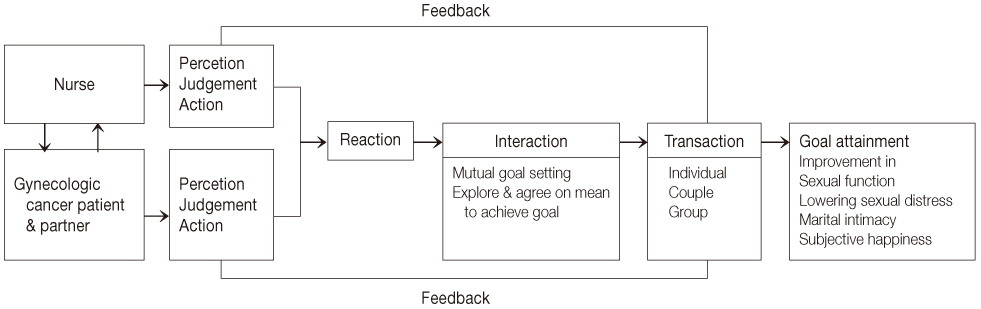
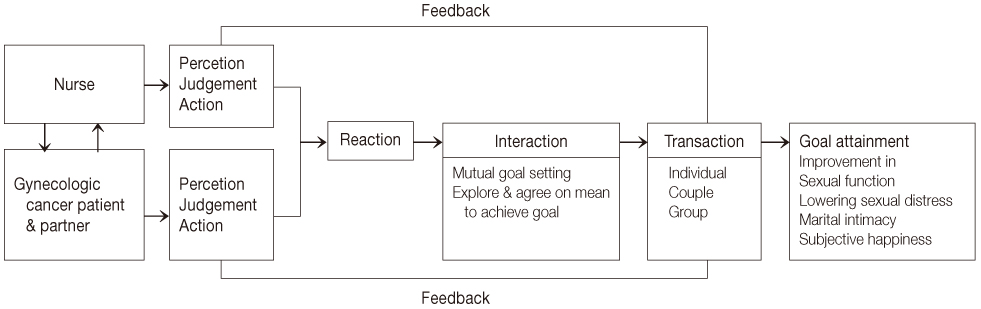
Figure 1
Sexual Health Enhancement Program
FSFI=Female sexual function index; FSDS=Female sexual distress scale.
Baseline Characteristics of Participants (N=43)
Exp.=Experimental group; Cont.=Control group.
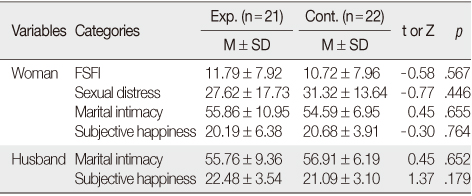
Homogeneity Test for FSFI, Sexual Distress, Marital Intimacy and Subjective Happiness (N=43)
Exp.=Experimental group; Cont.=Control group; FSFI=Female sexual function index.
Effectiveness of Sexual Health Enhancement Program (N=43)
Exp.=Experimental group; Cont.=Control group; FSFI=Female sexual function index.
FSFI=Female sexual function index; FSDS=Female sexual distress scale.
Exp.=Experimental group; Cont.=Control group.
Exp.=Experimental group; Cont.=Control group; FSFI=Female sexual function index.
Exp.=Experimental group; Cont.=Control group; FSFI=Female sexual function index.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

