Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 41(6); 2011 > Article
-
Original Article
- Public Knowledge and Attitudes Regarding Antibiotic Use in South Korea
- So Sun Kim, Seongmi Moon, Eun Jung Kim
-
Journal of Korean Academy of Nursing 2011;41(6):742-749.
DOI: https://doi.org/10.4040/jkan.2011.41.6.742
Published online: December 31, 2011
1Professor, College of Nursing · Researcher, The Nursing Policy Research Institute, Yonsei University, Seoul, Korea.
2Assistant Professor, Department of Nursing, University of Ulsan, Ulsan, Korea.
3Full-time Lecturer, College of Nursing, Eulji University, Seongnam, Korea.
- Address reprint requests to: Kim, Eun Jung. College of Nursing, Eulji University, 212 Yangji-dong, Sujeong-gu, Seongnam 461-713, Korea. Tel: +82-31-740-7398 Fax: +82-31-740-7359, ejerkim@eulji.ac.kr
© 2011 Korean Society of Nursing Science
Figure & Data
REFERENCES
Citations

- Knowledge, Attitudes, and Practices Regarding Antibiotic Use Among the General Population in Kuwait: A Cross-Sectional Study
Moosa N Mohiyaldeen, Khaled J Alsamhan, Abdullah B AlRukaibi, Reem S AlSawwagh, Maram W AlZanki, Munirah Ebrahim, Zainab Abulhasan, Zainab Al Mousa, Abdullah Almajran
Cureus.2026;[Epub] CrossRef - Knowledge, perception, and behaviours related to antibiotic use and antimicrobial resistance in community-dwelling individuals in Hong Kong
Sze Lon Chloe Chui, Siu-Wai Lai, Pei-Yu Huang, Chi Ching Cherrie Pang, Chung Ki Anna Tsui, Hein Min Tun, Sinn Kay Olivia Chan, Peng Wu
Journal of Infection and Chemotherapy.2025; 31(3): 102583. CrossRef - Examining Mothers' Knowledge, Attitudes, and Behaviors Regarding Antibiotic Use According to Age and Educational Level
Ergin Kariptaş, Kıymet Kariptaş, Mahmut Erbey
Black Sea Journal of Health Science.2025; 8(6): 296. CrossRef - Study on knowledge, attitudes and behavioral practices of antimicrobial usage and resistance in animals and humans in Bahir Dar City, Northwest Ethiopia
Edom Mesafint, Yeabsira Wondwosen, Gashaw Getaneh Dagnaw, Abebe Tesfaye Gessese, Adugna Berju Molla, Bereket Dessalegn, Haileyesus Dejene
BMC Public Health.2024;[Epub] CrossRef - A Study of Awareness, Knowledge, Attitudes, and Practices Regarding Antibiotic Resistance
Anas Alhur, Lama Alghamdi, Fay Alqahtani, Milaf Alshammari, Halimah Hattany, Abdulrahman Akshah, Atyaf Al Ahmary, Rawan Aloqran, Ebtehal Olagi, Noura S Alshahrani, Reem Al-Qahtani, Joud Alqahtani, Lena Alghamdi, Abdullah Alharbi, Shahad Alshokani
Cureus.2024;[Epub] CrossRef - A study assessing public knowledge and behaviour of antibiotic use in Abu Dhabi and Dubai
Lana Maher Mohammad, Rana Mahmood Kamran, Syed Wasif Gillani
Journal of Pharmaceutical Health Services Research.2023; 14(3): 317. CrossRef - Antimicrobial stewardship: knowledge, perceptions, and factors associated with antibiotics misuse among consumer’s visiting the community pharmacies in a Nigeria Southwestern State
Wuraola Akande-Sholabi, Eunice Oyesiji
Journal of Pharmaceutical Policy and Practice.2023;[Epub] CrossRef - A stochastic model of antibiotic misuse, economy, and drug resistance: relating mutant extinction probability to socioeconomic and epidemiological factors
Bhawna Malik, Samit Bhattacharyya
Mathematical and Computer Modelling of Dynamical Systems.2023; 29(1): 236. CrossRef - The impacts of knowledge and attitude on behavior of antibiotic use for the common cold among the public and identifying the critical behavioral stage: based on an expanding KAP model
Qianning Wang, Yuanyang Wu, Dan Wang, Xiaoquan Lai, Li Tan, Qian Zhou, Lixia Duan, Rujiao Lin, Xi Wang, Feiyang Zheng, Tiantian Yu, Lu Wang, Si Fan, Yanting Wang, Xinping Zhang, Chenxi Liu
BMC Public Health.2023;[Epub] CrossRef - Antibiotics administration without prescription in Bangladesh
Humayun Kabir, Md Kamrul Hasan, Nahida Akter, Dr Hamim Tassdik, Dr Md Fakrul Islam, Dr Hasina Jannat, Ariful Haque Tutul, Ojifa Akter, Rawshan Ara, Muhammad Didarul Islam, Sohel Mahmud, Masuda Akter, Dipak Kumar Mitra
IJID Regions.2023; 7: 11. CrossRef - Rational use of antimicrobials: a nationwide cross-sectional survey among people of Pakistan
Sitaram Khadka, Furqan K. Hashmi, Gopal K. Yadav, Sabitri Lamichhane, Santoshi Giri, Fatima Tariq, Sabahat Amin, Warda Zaheer, Kiran Akram, Ifra Asghar, Kainat Zahra, Faiza Bajwa, Noor Ul-ain, Muhammad A.J. Adnan
International Journal of Surgery: Global Health.2023; 6(1): e103. CrossRef - Prevalence and impacts of self-medication in a disadvantaged setting: the importance of multi-dimensional health interventions
Cuong Tat Nguyen, Hien Thu Nguyen, Laurent Boyer, Pascal Auquier, Guillaume Fond, Khanh Nam Do, Anh Kim Dang, Huyen Phuc Do, Carl A. Latkin, Roger C. M. Ho, Cyrus S. H. Ho
Frontiers in Public Health.2023;[Epub] CrossRef - Antibiyotik Kullanımına Yönelik Bilgi ve Tutumların İncelenmesi
Ayhan DURMUŞ, Cemal SEZER
Journal of Innovative Healthcare Practices.2023; 4(1): 64. CrossRef - Development and Psychometric Evaluation of the Antibiotic Knowledge and Consumption Tool (AKCT)
Sanah Hasan, Hana Sulieman, Husam Babi, Samir Bloukh
Antibiotics.2022; 11(12): 1744. CrossRef - Socio-Demographic Factors Associated with Antibiotics and Antibiotic Resistance Knowledge and Practices in Vietnam: A Cross-Sectional Survey
Khanh Nguyen Di, Sun Tee Tay, Sasheela Sri La Sri Ponnampalavanar, Duy Toan Pham, Li Ping Wong
Antibiotics.2022; 11(4): 471. CrossRef - Knowledge and perceptions of outpatients regarding upper respiratory tract infections and awareness of an Antibiotics Smart Use campaign in Thailand
Pacharaporn Phueanpinit, Nongchanok Siriwattanasakul, Penpit Tichakorn, Siranan Klanbut
Journal of Pharmacy Practice and Research.2022; 52(4): 294. CrossRef - Knowledge, Attitudes and Practices Regarding Antibiotic Use and Antibiotic Resistance: A Latent Class Analysis of a Romanian Population
Elena Narcisa Pogurschi, Carmen Daniela Petcu, Alexandru Eugeniu Mizeranschi, Corina Aurelia Zugravu, Daniela Cirnatu, Ioan Pet, Oana-Mărgărita Ghimpețeanu
International Journal of Environmental Research and Public Health.2022; 19(12): 7263. CrossRef - The Predictors Influencing the Rational Use of Antibiotics Among Public Sector: A Community-Based Survey in Thailand
Thaw Zin Lin, Isareethika Jayasvasti, Sariyamon Tiraphat, Supa Pengpid, Manisthawadee Jayasvasti, Phetlada Borriharn
Drug, Healthcare and Patient Safety.2022; Volume 14: 27. CrossRef - Antibiotic prescription for acute upper respiratory tract infections: Understanding patient and physician contributions via patients’ migration
Woohyeon Kim, Euna Han
Social Science & Medicine.2022; 314: 115466. CrossRef - Public knowledge, attitude, and practice regarding antibiotics use in Punjab, Pakistan: a cross-sectional study
Ali Hassan Gillani, Jie Chang, Fahmida Aslam, Amna Saeed, Sundus Shukar, Farhat Khanum, Ammar Jairoun, Alison Nicholson, Mohamed Izham Mohamed Ibrahim, Yu Fang
Expert Review of Anti-infective Therapy.2021; 19(3): 399. CrossRef - Assessing the Syrian Population’s Knowledge, Attitudes, and Practices Regarding Antibiotic Usage
Abdallah Altorkmani, Mhd Amin Alzabibi, Mosa Shibani, Hlma Ismail, Bisher Sawaf, Nizar Daher, Ahmad Al-Moujahed
Avicenna Journal of Medicine.2021; 11(03): 132. CrossRef - Use of antimicrobials and antimicrobial resistance in Nepal: a nationwide survey
Komal Raj Rijal, Megha Raj Banjara, Binod Dhungel, Samarpan Kafle, Kedar Gautam, Bindu Ghimire, Prabina Ghimire, Samriddh Dhungel, Nabaraj Adhikari, Upendra Thapa Shrestha, Dev Ram Sunuwar, Bipin Adhikari, Prakash Ghimire
Scientific Reports.2021;[Epub] CrossRef - Knowledge, attitude, and practices related to antibiotic use and resistance among the general public of coastal south Karnataka, India – A cross-sectional survey
Khyati Bhardwaj, Suchitra Shenoy M, Shrikala Baliga, B. Unnikrishnan, B. Shantharam Baliga
Clinical Epidemiology and Global Health.2021; 11: 100717. CrossRef - Self-medication Behavior with antibiotics: a national cross-sectional survey in Sri Lanka
Shukry Zawahir, Sarath Lekamwasam, Kjell H. Halvorsen, Grenville Rose, Parisa Aslani
Expert Review of Anti-infective Therapy.2021; 19(10): 1341. CrossRef - Knowledge and Attitude of Antibiotic Use among Public in Rural Area of Cempaka, Banjarbaru, South Kalimantan
Nurul Mardiati, Rahmayanti Fitriah, Nadia Wahyu Artati, Wika Tiarawati, Muhammad Zaini
Borneo Journal of Pharmacy.2021; 4(3): 238. CrossRef - public-knowledge-and-attitudes-towards-antibiotics-usage-in-perlis-a-cross-sectional-study
>Ahmad Syahmi Ahmad Zaini, >Jihan Diyana Maidin, >Mumtaz Mohamad Ghausillah, >Norhaffizawati Othman
Malaysian Journal of Pharmacy.2021; 7(2): 32. CrossRef - Antibiotic Use and Resistance Knowledge: Awareness Among the General Public in Jazan, Saudi Arabia
Abdulaziz Jali, Alshomokh Hakami, Najwa Dahas, Mashael Mahnashi, Afnan Siddiq, Halimah Alsomaili, Abdulaziz H Alhazmi
Cureus.2021;[Epub] CrossRef - Public Health Literacy, Knowledge, and Awareness Regarding Antibiotic Use and Antimicrobial Resistance during the COVID-19 Pandemic: A Cross-Sectional Study
Suhaib M. Muflih, Sayer Al-Azzam, Reema A. Karasneh, Barbara R. Conway, Mamoon A. Aldeyab
Antibiotics.2021; 10(9): 1107. CrossRef - Knowledge, Perception, and Belief on Antibiotic Use in The Community of Panyabungan, Mandailing Natal District, Indonesia
R.A. Syahputra, Khairunnisa Khairunnisa, Urip Harahap
Research Journal of Pharmacy and Technology.2021; : 6549. CrossRef - Antibiotic Self-Medication and Antibiotic Resistance: Multilevel Regression Analysis of Repeat Cross-Sectional Survey Data in Europe
Alistair Anderson
REGION.2021; 8(2): 121. CrossRef - Predicting sustainable consumption of package-free bath products among students in higher education institutions
Alvin Patrick M. Valentin
International Journal of Sustainability in Higher Education.2021; 22(7): 1753. CrossRef - Understanding parental self-medication with antibiotics among parents of different nationalities: a cross-sectional study
Zhongliang Zhou, Dantong Zhao, Huarui Zhang, Chi Shen, Dan Cao, Guanping Liu, Liang Zhu, Yu Fang
Global Health Research and Policy.2021;[Epub] CrossRef - Antibiotics dispensing between legal idealism and implementation: Closing the implementation gap between local regulation and practice
Ammar Abdulrahman Jairoun, Sabaa Saleh Al-Hemyari, Maimona Jairoun
Research in Social and Administrative Pharmacy.2020; 16(9): 1328. CrossRef - A Descriptive Study Using an Intercept Survey
Barbara Pieper, Joanne Sobeck, Linda Kaljee, Thomas N. Templin
Journal of Wound, Ostomy & Continence Nursing.2020; 47(1): 20. CrossRef - First-year pharmacy students’ prior knowledge correlates with study progress and reveals different dynamics of misconceptions
Ilona Södervik, Leena Hanski, Nina Katajavuori
Pharmacy Education.2020; 20: 94. CrossRef - Serbian students’ knowledge, attitudes and behaviour towards antibiotic use: is there room for improvement?
Olga Horvat, Ana Tomas, Milica Paut Kusturica, Dragica Bukumiric, Bojan Blagojevic, Zorana Kovacevic
International Journal of Public Health.2020; 65(8): 1257. CrossRef - Perceptions of Responsibility for Antibiotic Resistance: Implications for Stewardship Campaigns
A. K. Worthington, E. L. MacGeorge, K. A. Foley
Journal of Health Communication.2020; 25(9): 703. CrossRef - A scoping review on the influential cognitive constructs informing public AMR behavior compliance and the attribution of personal responsibility
Hayley Fletcher-Miles, John Gammon
American Journal of Infection Control.2020; 48(11): 1381. CrossRef - Surveys of knowledge and awareness of antibiotic use and antimicrobial resistance in general population: A systematic review
Hathairat Kosiyaporn, Sunicha Chanvatik, Tibet Issaramalai, Wanwisa Kaewkhankhaeng, Anond Kulthanmanusorn, Nithiwat Saengruang, Woranan Witthayapipopsakul, Shaheda Viriyathorn, Supapat Kirivan, Watinee Kunpeuk, Rapeepong Suphanchaimat, Angkana Lekagul, Vi
PLOS ONE.2020; 15(1): e0227973. CrossRef - Knowledge, attitudes and practices regarding antimicrobial use and resistance among communities of Ilala, Kilosa and Kibaha districts of Tanzania
Calvin Sindato, Leonard E. G. Mboera, Bugwesa Z. Katale, Gasto Frumence, Sharadhuli Kimera, Taane G. Clark, Helena Legido-Quigley, Stephen E. Mshana, Mark M. Rweyemamu, Mecky Matee
Antimicrobial Resistance & Infection Control.2020;[Epub] CrossRef Knowledge and Beliefs of Health Care Professionals Towards Antimicrobial Resistance in Hiwot Fana Specialized University Hospital, in Harar, Ethiopia
Zufan Gebrehiwot, Yohannes Tadiwos
Infection and Drug Resistance.2020; Volume 13: 2027. CrossRef- Analysing incompliant attitudes towards antibiotic prescription completion in the UK
Alistair Anderson
Journal of Antimicrobial Chemotherapy.2020; 75(3): 756. CrossRef - Antibiotic use and resistance: an unprecedented assessment of university students’ knowledge, attitude and practices (KAP) in Lebanon
Samer Sakr, Ali Ghaddar, Bassam Hamam, Imtithal Sheet
BMC Public Health.2020;[Epub] CrossRef - Development and nationwide application of an antibiotic knowledge scale
Dandan Li, Heping Yang, Yanhong Gong, Yuxin Zhao, Lei Qiu, Na Sun, Xiaoxv Yin
Preventive Medicine.2020; 141: 106262. CrossRef - Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal
Anant Nepal, Delia Hendrie, Suzanne Robinson, Linda A. Selvey
BMC Public Health.2019;[Epub] CrossRef - Knowledge and attitude towards antibiotic use within consumers in Alkharj, Saudi Arabia
Saleh Abdullah Alqarni, Mohammed Abdulbari
Saudi Pharmaceutical Journal.2019; 27(1): 106. CrossRef - Knowledge, attitude and practice (KAP) survey regarding antibiotic use among pilgrims attending the 2015 Hajj mass gathering
Saber Yezli, Yara Yassin, Abdulaziz Mushi, Fuad Maashi, Nibras Aljabri, Gamal Mohamed, Kingsley Bieh, Awam Awam, Badriah Alotaibi
Travel Medicine and Infectious Disease.2019; 28: 52. CrossRef - Low-income community knowledge, attitudes and perceptions regarding antibiotics and antibiotic resistance in Jelutong District, Penang, Malaysia: a qualitative study
Lyna Irawati, Alian A. Alrasheedy, Mohamed Azmi Hassali, Fahad Saleem
BMC Public Health.2019;[Epub] CrossRef - Exposure assessment of the consumers living in Mount Lebanon directorate to antibiotics through medication and red meat intake: A cross-sectional study
Christelle Bou-Mitri, Paula Hage Boutros, Joelle Makhlouf, Maya Abou Jaoudeh, Najwa El Gerges, Jessy El Hayek Fares, Elie Bou Yazbeck, Hussein Hassan
Veterinary World.2019; 12(9): 1395. CrossRef - Knowledge and Expectations on Antibiotic Use among Older Adults in Malaysia: A Cross-Sectional Survey
Lai San Kong, Farida Islahudin, Leelavathi Muthupalaniappen, Wei Wen Chong
Geriatrics.2019; 4(4): 61. CrossRef - Assessment of Farmers’ Knowledge, Attitudes and Practices on Antibiotics and Antimicrobial Resistance
Yasin Ozturk, Senol Celik, Emre Sahin, Mehmet Nuri Acik, Burhan Cetinkaya
Animals.2019; 9(9): 653. CrossRef - Public Awareness about Antibiotic Use and Resistance among Residents in Highland Areas of Vietnam
Thuy Van Ha, An Mai Thi Nguyen, Ha Song Thi Nguyen
BioMed Research International.2019; 2019: 1. CrossRef - Public Knowledge and Attitudes Towards Antibiotics Use and Resistance in Baghdad, Iraq: A Survey Conducted in Outpatient Department of University Teaching Hospital
Berq J. Hadi Al-Yasseri, Nibras A. Hussain
The Open Public Health Journal.2019; 12(1): 567. CrossRef - Online health information and public knowledge, attitudes, and behaviours regarding antibiotics in the UK: Multiple regression analysis of Wellcome Monitor and Eurobarometer Data
Alistair Anderson, Italo Francesco Angelillo
PLOS ONE.2018; 13(10): e0204878. CrossRef - Reduced antibiotic prescription rates following physician-targeted interventions in a dental practice
Hyesung Kim, Jeong Kyu Oh, Myeng Ki Kim, Kwanghak Bae, Hyungkil Choi
Acta Odontologica Scandinavica.2018; 76(3): 204. CrossRef - Factors affecting the rate of antibiotic prescription in dental practices
Hyesung Kim, Myeng Ki Kim, Hyungkil Choi
Journal of Korean Academy of Oral Health.2017; 41(1): 28. CrossRef - Is the level of knowledge a predictor of rational antibiotic use in Serbia?
Olga J. Horvat, Ana D. Tomas, Milica M. Paut Kusturica, Alisa V. Savkov, Dragica U. Bukumirić, Zdenko S. Tomić, Ana J. Sabo, Yeng-Tseng Wang
PLOS ONE.2017; 12(7): e0180799. CrossRef - Knowledge, Attitude and Practice of Self-Medication with Antibiotics Among Nursing Students
Sevgul Donmez, Kivanc Gungor, Pinar Gov
International Journal of Pharmacology.2017; 14(1): 136. CrossRef - Knowledge of antibiotics and antibiotic resistance in patients followed by family physicians
A. Robert, Y. Nguyen, O. Bajolet, B. Vuillemin, B. Defoin, V. Vernet-Garnier, M. Drame, F. Bani-Sadr
Médecine et Maladies Infectieuses.2017; 47(2): 142. CrossRef - From Visiting a Physician to Expecting Antibiotics: Korean Perspectives and Practices toward Respiratory Tract Infections
Leila Freidoony, Chun-Bae Kim, Hamid Haghani, Myung-Bae Park, Sei-Jin Chang, Sang-Ha Kim, Sang Baek Koh
Journal of Korean Medical Science.2017; 32(2): 278. CrossRef - Community knowledge and attitudes on antibiotic use in Moshi Urban, Northern Tanzania: Findings from a cross sectional study
Mbwambo Goodluck, Emidi Basiliana, R. Mgabo Maseke, Nimrod Sigall Geofrey, C. Kajeguka Debora
African Journal of Microbiology Research.2017; 11(25): 1018. CrossRef - Association between public knowledge regarding antibiotics and self-medication with antibiotics in Teling Atas Community Health Center, East Indonesia
Kurniawan Kurniawan, Jimmy Posangi, Nancy Rampengan
Medical Journal of Indonesia.2017; 26(1): 62. CrossRef - Knowledge and Attitudes towards Antibiotic Use and Resistance - A Latent Class Analysis of a Swedish Population-Based Sample
Martina Vallin, Maria Polyzoi, Gaetano Marrone, Senia Rosales-Klintz, Karin Tegmark Wisell, Cecilia Stålsby Lundborg, Patrick Butaye
PLOS ONE.2016; 11(4): e0152160. CrossRef - Knowledge, attitudes and practices towards antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore
Darius Shaw Teng Pan, Joyce Huixin Huang, Magdalene Hui Min Lee, Yue Yu, Mark I-Cheng Chen, Ee Hui Goh, Lili Jiang, Joash Wen Chen Chong, Yee Sin Leo, Tau Hong Lee, Chia Siong Wong, Victor Weng Keong Loh, Adrian Zhongxian Poh, Tat Yean Tham, Wei Mon Wong,
BMC Family Practice.2016;[Epub] CrossRef - Active educational intervention as a tool to improve safe and appropriate use of antibiotics
Mayadah B. Shehadeh, Ghadeer A.R.Y. Suaifan, Eman A. Hammad
Saudi Pharmaceutical Journal.2016; 24(5): 611. CrossRef - Public Knowledge and Attitudes Regarding the Use of Antibiotics and Resistance: Findings from a Cross‐Sectional Study Among Palestinian Adults
A. Abu Taha, A. H. Abu‐Zaydeh, R. A. Ardah, S. W. Al‐Jabi, W. M. Sweileh, R. Awang, S. H. Zyoud
Zoonoses and Public Health.2016; 63(6): 449. CrossRef - Antibiotic misuse among children with diarrhea in China: results from a national survey
Ruili Li, Feng Xiao, Xiaoguo Zheng, Huimin Yang, Lihong Wang, Delu Yin, Tao Yin, Qianqian Xin, Bowen Chen
PeerJ.2016; 4: e2668. CrossRef - Removal characteristics and mechanism of antibiotics using constructed wetlands
Yeong-Joo Choi, Lee-Hyung Kim, Kyung-Duk Zoh
Ecological Engineering.2016; 91: 85. CrossRef - General population's knowledge and attitudes about antibiotics: a systematic review and meta-analysis
Maria R. Gualano, Renata Gili, Giacomo Scaioli, Fabrizio Bert, Roberta Siliquini
Pharmacoepidemiology and Drug Safety.2015; 24(1): 2. CrossRef - Antibiotic use and resistance: a cross-sectional study exploring knowledge and attitudes among school and institution personnel in Tbilisi, Republic of Georgia
Ketevan Kandelaki, Cecilia Stålsby Lundborg, Gaetano Marrone
BMC Research Notes.2015;[Epub] CrossRef - Antibiotic Use: A Cross-Sectional Survey Assessing the Knowledge, Attitudes and Practices amongst Students of a School of Medicine in Italy
Giacomo Scaioli, Maria R. Gualano, Renata Gili, Simona Masucci, Fabrizio Bert, Roberta Siliquini, Lamberto Manzoli
PLOS ONE.2015; 10(4): e0122476. CrossRef - Knowledge, attitudes and perceptions regarding antibiotic use and self-medication: a cross-sectional study among Australian Chinese migrants
Jie Hu, Zhiqiang Wang
Healthcare infection.2015; 20(1): 23. CrossRef - Public Knowledge, Beliefs and Behavior on Antibiotic Use and Self-Medication in Lithuania
Eglė Pavydė, Vincentas Veikutis, Asta Mačiulienė, Vytautas Mačiulis, Kęstutis Petrikonis, Edgaras Stankevičius
International Journal of Environmental Research and Public Health.2015; 12(6): 7002. CrossRef - Knowledge, Attitude and Practice towards Antibiotic Use among the Public in Kuwait
Abdelmoneim Ismail Awad, Esraa Abdulwahid Aboud, Andrew C Singer
PLOS ONE.2015; 10(2): e0117910. CrossRef - Assessing the Lebanese population for their knowledge, attitudes and practices of antibiotic usage
Tarek H. Mouhieddine, Zeinab Olleik, Muhieddine M. Itani, Soumayah Kawtharani, Hussein Nassar, Rached Hassoun, Zeinab Houmani, Zeinab El Zein, Ramy Fakih, Ibrahim K. Mortada, Youssef Mohsen, Zeina Kanafani, Hani Tamim
Journal of Infection and Public Health.2015; 8(1): 20. CrossRef - Perceptions and Use of Antimicrobials Among Staff of a University Community in Southwestern Nigeria
Esther O. Asekun-Olarinmoye, Patience O. Akinwusi, Wasiu O. Adebimpe, Akinlolu G. Omisore, Michaeline A. Isawumi, Mustapha B. Hassan, Olugbenga A. Olowe, Olufunmi B. Makanjuola, Omoniyi M. Abiodun, Janet O. Olaitan, Peter B. Olaitan, Christopher O. Alebio
Sage Open.2014;[Epub] CrossRef - Determinants of an effective antibiotic campaign: Lessons from Hong Kong
Mei Lin Ho, Benjamin John Cowling, Wing Hong Seto, Lai Chin Wong, Tin Yau Wong
Journal of Global Antimicrobial Resistance.2014; 2(4): 334. CrossRef - Exploring antibiotic use and practices in a Malaysian community
Omotayo Fatokun
International Journal of Clinical Pharmacy.2014; 36(3): 564. CrossRef - Assessing the Impact of a School Intervention to Promote Students’ Knowledge and Practices on Correct Antibiotic Use
Maria-Manuel Azevedo, Céline Pinheiro, John Yaphe, Fátima Baltazar
International Journal of Environmental Research and Public Health.2013; 10(7): 2920. CrossRef
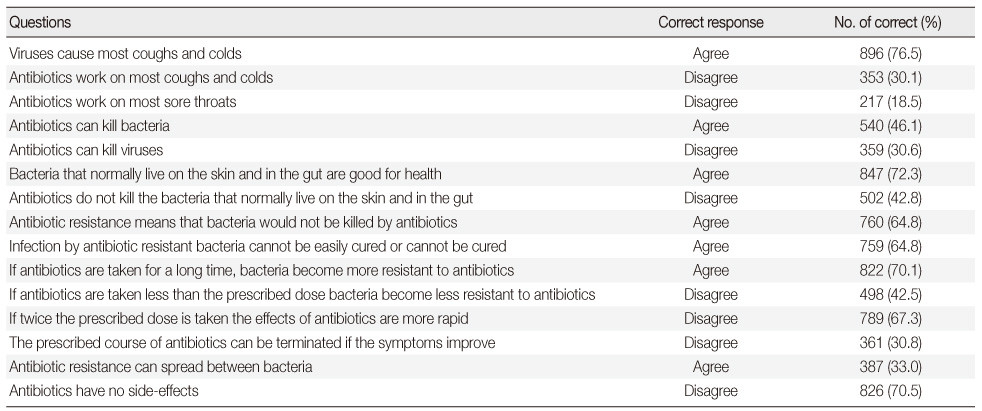
Responses to Questions regarding Knowledge of Antibiotic Use
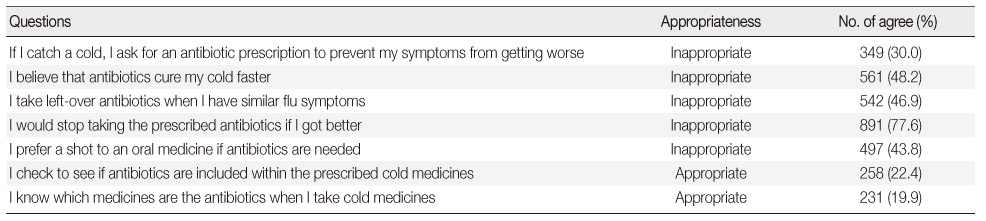
Responses to Questions regarding Attitudes toward Antibiotic Use
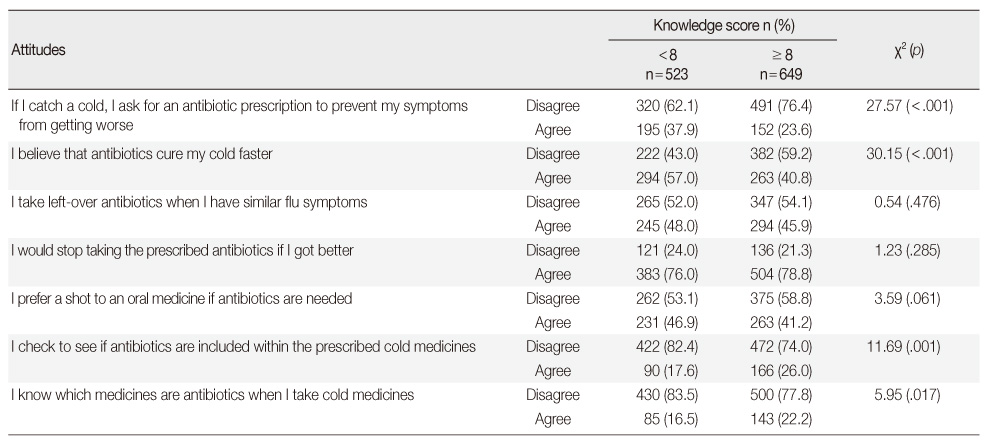
Association between Knowledge of and Attitudes toward Antibiotic Use
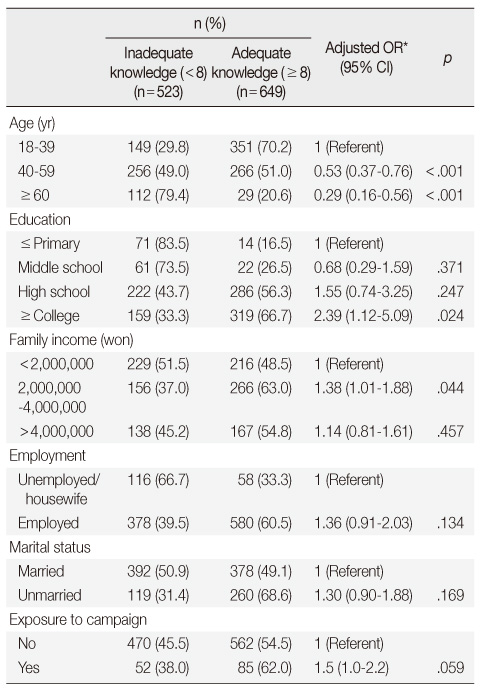
Factors Significantly Associated with Public Knowledge of Antibiotic Use
*Odds ratio adjusted for other significant factors; Obtained with a step-wise multiple logistic regression analysis.
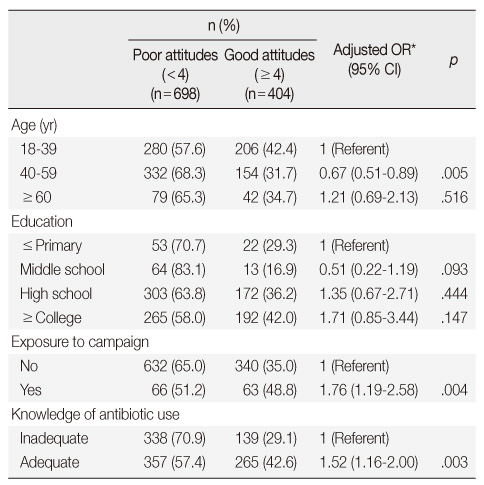
Factors Significantly Associated with Public Attitudes Toward Antibiotic Use
*Odds ratio adjusted for other significant factors; Obtained with a step-wise multiple logistic regression analysis.
*Odds ratio adjusted for other significant factors; Obtained with a step-wise multiple logistic regression analysis.
*Odds ratio adjusted for other significant factors; Obtained with a step-wise multiple logistic regression analysis.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

