Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 39(2); 2009 > Article
-
Original Article
- Hospital Nurses' Knowledge and Compliance on Multidrug-resistant Organism Infection Control Guideline
- Jiyeon Kang, Jinwan Cho, Yujung Kim, Dong-Hee Kim, Jiyoung Lee, Hey-Kyung Park, Sung-Hee Jung, Eun-Nam Lee
-
Journal of Korean Academy of Nursing 2009;39(2):186-197.
DOI: https://doi.org/10.4040/jkan.2009.39.2.186
Published online: April 28, 2009
1Assistant Professor, Department of Nursing, Dong-A University, Busan, Korea.
2Nurse, Dong-A University Medical Center, Busan, Korea.
3Full-time Lecturer, Department of Nursing, Namseoul University, Cheonan, Korea.
4Professor, Department of Nursing, Dong-A University, Busan, Korea.
- Address reprint requests to: Kang, Jiyeon. Department of Nursing, Dong-A University, 1 Dongdaesin-dong 3ga, Seo-gu, Busan 602-714, Korea. Tel: 82-51-240-2871, Fax: 82-51-240-1947, jykang@dau.ac.kr
Copyright © 2009 Korean Society of Nursing Science
Abstract
-
Purpose
- This study was done to investigate nurses' knowledge of, and compliance with the multidrug-resistant organism (MDRO) infection control guidelines.
-
Methods
- A survey questionnaire was developed based on the institutional and national guidelines and was administered to a convenience sample of 306 nurses in a university hospital.
-
Results
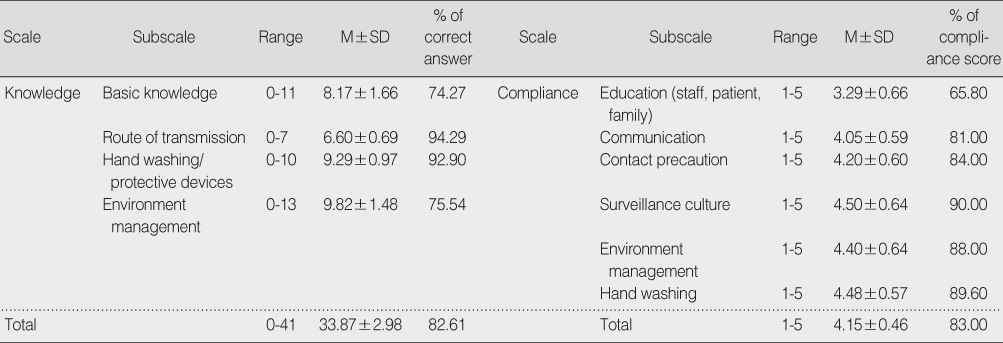
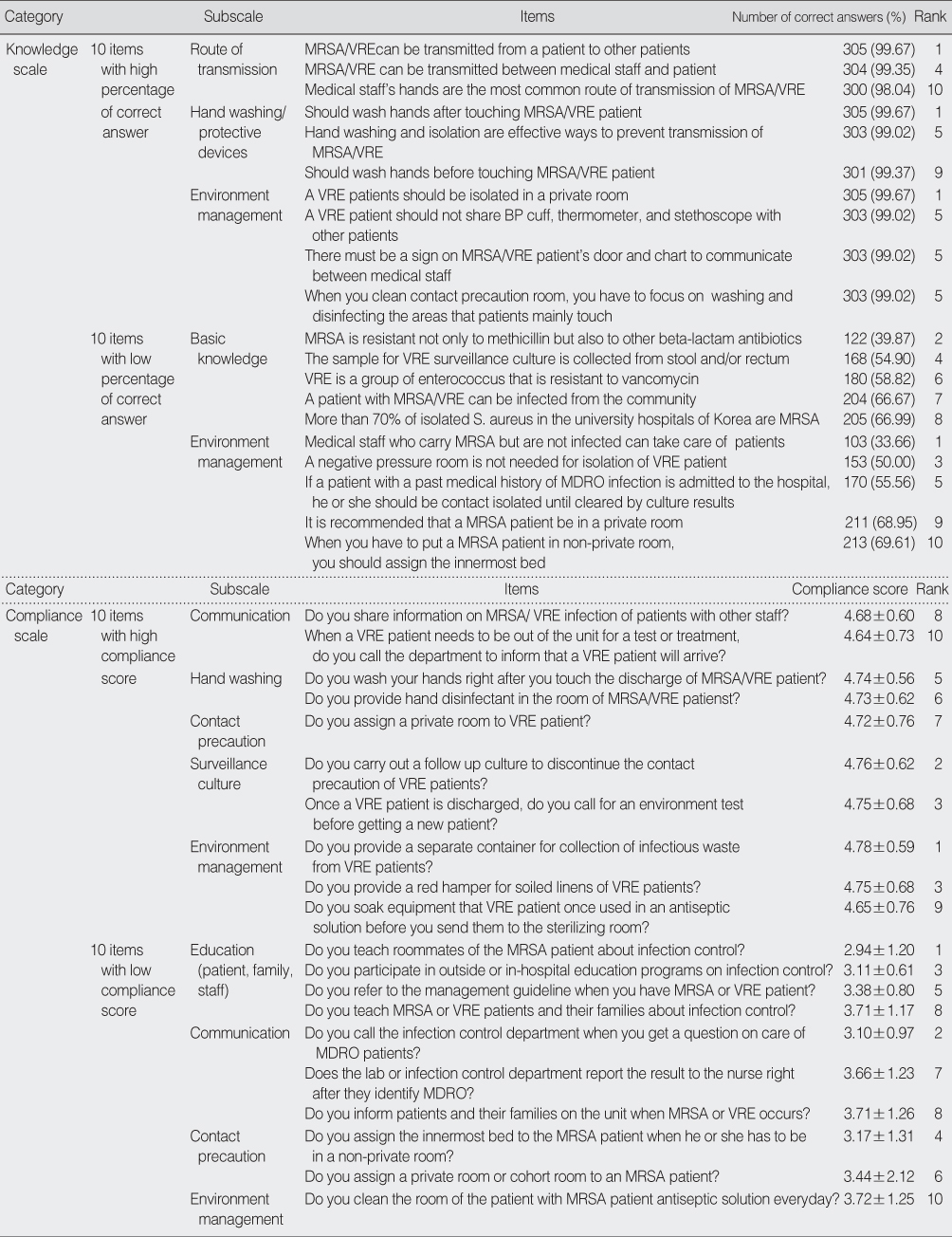
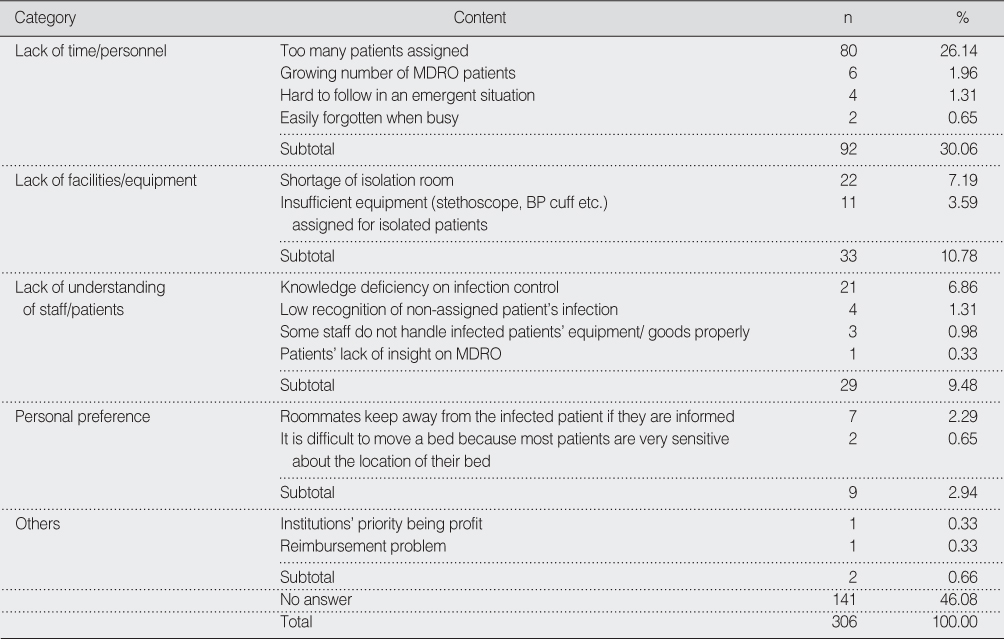
- The mean score for knowledge was 33.87 (percentage of correct answers: 82.61%). The percentages of correct answers for basic concepts, route of transmission, hand washing/protective devices and environment management were 74.27%, 94.29%, 92.90% and 75.54% respectively. The mean compliance score was 4.15 (range: 1-5). The compliance scores for education, communication, contact precaution, disinfection, surveillance culture, and hand washing were 3.29, 4.05, 4.20, 4.50, 4.40 and 4.48 respectively. Nurses indicated "lack of time (30.06%)", "lack of means (10.78%)" and "lack of knowledge (9.48%)" as reasons for noncompliance.
-
Conclusion
- While most educational programs have focused on hand washing or use of protective devices to prevent transmission of MDRO in acute care settings, hospital nurses' knowledge of the basic concepts of MDRO and environmental management has remained insufficient. Nurses are relatively non-compliant to the guidelines in the areas of education (staff, patient, family) and communication. Comprehensive educational programs are needed to decrease hospital infection rates and to improve the health of patients.
- 1. Blok H, Troelstra A, Kamp-Hopmans TE, Gigengack-Baars AC, Vandenbroucke-Grauls CM, Weersink AJ, et al. Role of health care workers in outbreaks of methicillin-resistant Staphylococcus aureus: A 10-year evaluation from a Dutch university hospital. Infection Control and Hospital Epidemiology. 2003;24:679–685.ArticlePubMed
- 2. Cheong H, Song J, Eom J, Kim W, Choi S, Choi J, et al. Colonization rate, risk factor for acquisition and genetic diversity of Vancomycin-resistant enterococci (VRE) isolated from rectal culture of patients in intensive care units from ten large hospitals in Korea. Korean Journal of Infectious Disease. 2002;34:276–284.
- 3. Clancy M, Graepler A, Wilson M, Douglas I, Johnson J, Price CS. Active screening in high risk units is an effective and cost-avoidant method to reduce the rate of MRSA infection in the hospital. Infection Control and Hospital Epidemiology. 2006;27:1009–1017.PubMed
- 4. DiazGranados CA, Zimmer SM, Klein M, Jernigan JA. Comparison of mortality associated with vancomycin-resistant and vancomycin-susceptible enterococcal bloodstream infections: A meta-analysis. Clinical Infectious Diseases. 2005;41:327–333.ArticlePubMed
- 5. Dong-A University Medical Center. Guideline for prevention and management of infection. 2008;Busan, Author.
- 6. Easton PM, Sarma A, Williams FL, Marwick CA, Phillips G, Nathwani D. Infection control and management of MRSA: Assessing the knowledge of staff in an acute hospital setting. Journal of Hospital Infection. 2007;66:29–33.ArticlePubMed
- 7. Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clinical Infectious Diseases. 2003;36:592–598.ArticlePubMed
- 8. Farr B. Doing the right thing (and figuring out what that is). Infection Control and Hospital Epidemiology. 2006;27:999–1003.ArticlePubMed
- 9. Jeong J, Choe M. The effect of hand washing improving programs on the adherence of hand washing and nosocomial infection. Korean Journal of Nosocomial Infection Control. 2004;9:117–129.
- 10. Jung M, Yoon S. Analysis on the transmission paths of vancomycin resistant enterococci infection in a health care environment in Korea. Journal of Korean Society of Living Environment System. 2003;10:125–130.
- 11. Kim JK, Kim CH, Han SY, Byun HW, Park WJ, Woo HJ, et al. Clinical characteristics in patients with vancomycin-resistant enterococci colonization or infection during 5 years in a private general hospital. Korean Journal of Critical Care Medicine. 2005;20:54–62.
- 12. Kim K, Cha K, Lee J, Yoo S, Choi O, Wie S, et al. Knowledge and performance of infection control guidelines. Korean Journal of Nosocomial Infection Control. 2004;9:139–150.
- 13. Kim M, Jeong C. The level of the awareness and the compliance on the nosocomial infection control among clinical nurses in the hospital. Korean Journal of Nosocomial Infection Control. 2002;7:133–141.
- 14. Kim NC, Choi KO. Effects on nurses' hand washing behavior and reduction of respiratory isolation rate of MRSA of the hand washing education. Journal of Korean Academy of Adult Nursing. 2002;14:26–33.
- 15. Kim SO, Cho SH. A study on clinical nurses level of perception of importance, performance and satisfaction in the control of nosocomial infection. Journal of Korean Academy of Nursing. 1997;27:765–776.ArticlePDF
- 16. Kim YH, Jeon SS, Jeong IS, Chang CH, Kim JH, Huh JA. The effect of hand washing improving program and MRSA carrier screening program on the MRSA infection rates in an intensive care unit. Journal of Korean Acade my of Nursing. 2003;33:686–692.ArticlePDF
- 17. Klevens RM, Edwards JR, Tenover FC, McDonald LC, Horan T, Gaynes R, et al. Changes in the epidemiology of MRSA in intensive care unit in US hospitals, 1992-2003. Clinical Infectious Diseases. 2006;42:389–391.ArticlePubMed
- 18. Ministry for Health and Welfare. Guideline for prevention and management of hospital infection. 2005;Seoul, Author.
- 19. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of staphylococcus aureus and enterococcus. Infection Control and Hospital Epidemiology. 2003;24:362–386.PubMed
- 20. National Health Insurance Corporation. Regulations about National Health Insurance Payment for medical treatment. 2008;Seoul, Author. (Rev. July 11, 2008).
- 21. NNIS. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2003. American Journal of Infection Control. 2003;31:481–498.ArticlePubMed
- 22. Office of Profession. Mandated training related to infection control. 2008;Retrieved July 2, 2008. from http://www.op.nysed.gov/icmemo.htm.
- 23. Oh H. National survey on nurses' knowledge of infection control in general hospitals and analysis of variables to impact on their knowledge. Korean Journal of Nosocomial Infection Control. 2005;10:78–86.
- 24. Ott M, Shen J, Sherwood S. Evidenced-based practice for control of methicillin-resistant Staphylococcus aureus. AORN Journal. 2005;81:361–372.PubMed
- 25. Sax H, Perneger T, Hugonnet S, Herrault P, Chraiti MN, Pittet D. Knowledge of standard and isolation precautions in a large teaching hospital. Infection Control and Hospital Epidemiology. 2005;26:298–304.ArticlePubMed
- 26. Shitrit P, Gottsman BS, Katzir M, Kilman A, Ben-Nissan Y, Chowers M. Active surveillance for MRSA decreases the incidence of MRSA bacteremia. Infection Control and Hospital Epidemiology. 2006;27:1004–1008.PubMed
- 27. Siegal J, Rhinehart E, Jackson M, Chiarello L. HICPAC. Management of multidrug-resistant organisms in healthcare settings, 2006. 2006;Retrieved April 2, 2007. from http://www.cdc.gov/ncidod/dhqp/pdf/ar/mdroGuideline2006.pdf.
- 28. van Gemerg-Pijnen J, Hendrix MG, van der Palen J, Schellens PJ. Performance of methicillin-resistant Staphylococcus aureus protocols in Dutch hospitals. American Journal of Infection Control. 2005;33:377–384.ArticlePubMed
- 29. Woolf S. Practice guidelines: A new reality in medicine: III. Impact on patient care. Archives in Internal Medicine. 1993;153:2646–2655.Article
- 30. Yoon HS. A survey on the performance of surgical hand scrubs. Journal of Korean Academy of Nursing. 1996;26:591–604.ArticlePDF
REFERENCES
Figure & Data
REFERENCES
Citations

- Development and Evaluation of Infection Control Nursing Simulation Education Program for Nurses in a NICU
Min-hee Cho, Sunghee Kim
Journal of Korea Society for Simulation in Nursing.2024; 12(2): 1. CrossRef - The Effect on COVID-19 Infection Control Practice of Nurses who Work in Working Sites with Negative Pressure Isolation Rooms
Min Ji Park, Yun Mi Lee
Journal of Korean Critical Care Nursing.2022; 15(1): 35. CrossRef - Comparison of Knowledge, Attitude and Function of Nurses with Nursing Students about Hospital-Acquired Infection (HAI) Control in Sarab`s Imam Khomeini Medical Education Center at 2020
Y Lotfi, A bahadori, A Sadighi, S Fazlizadeh, M Hajizade, Y Zehtabiyan
Journal of Health and Care.2022; 24(1): 17. CrossRef - Knowledge, Attitudes, and Practices of NICU Doctors and Nurses Toward Prevention and Control of Nosocomial Infection With Multidrug Resistant Organism
Jinyan Zhou, Shuohui Chen
Frontiers in Pediatrics.2022;[Epub] CrossRef - Interprofessional perceptions of emotional, social, and ethical effects of multidrug-resistant organisms: A qualitative study
Stefan Bushuven, Markus Dettenkofer, Andreas Dietz, Stefanie Bushuven, Petra Dierenbach, Julia Inthorn, Matthias Beiner, Thorsten Langer, Vijayaprasad Gopichandran
PLOS ONE.2021; 16(2): e0246820. CrossRef - It Is Time to Address the Isolation Policy for Patients Colonized with Vancomycin-resistant Enterococci
Euijin Chang, Hong Bin Kim
Korean J healthc assoc Infect Control Prev.2021; 26(1): 16. CrossRef - Factors Influencing Compliance in Intravenous Practice for Infection Prevention among Nurses in Small and Medium Hospitals
Sung Ae Choi, Sun Young Jeong
Journal of Korean Academy of Fundamentals of Nursing.2020; 27(4): 344. CrossRef - Knowledge and Practice of Middle East Respiratory Syndrome Isolation Precaution among Hospital Nurses
Sunju Kim, Rhayun Song
Journal of Korean Academy of Fundamentals of Nursing.2018; 25(1): 46. CrossRef - Associated Factors with Performance of Infection Control for the Prevention of Ventilator-associated Pneumonia among Some Intensive Care Unit Nurses
Hyeon Hwa Lee, Mi Ah Han, Jong Park, Seong Woo Choi
Journal of Health Informatics and Statistics.2018; 43(1): 1. CrossRef - Knowledge and Compliance Level of the Multi-drug resistant Organisms of ICU nurses
Joung-A Shon, Jin Hee Park
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(7): 280. CrossRef - Factors Influencing Performance of MultiDrug-Resistant Organisms Infection Control in Nurses of General Hospital*
Jeonglim Ryu, Yu Kyung Ko
Journal of Korean Academy of Fundamentals of Nursing.2016; 23(2): 149. CrossRef - Effect of Education on Infection Control for Multidrug Resistant Organism on Infection Control by NICU Nurses
Jihee Lim, Kyung-Sook Bang
Child Health Nursing Research.2016; 22(3): 172. CrossRef - Factors related to the Management of MultiDrug-Resistant Organisms among Intensive Care Unit Nurses: An Application of the Health Belief Model*
Suyoung Kim, Chiyoung Cha
Journal of Korean Academy of Fundamentals of Nursing.2015; 22(3): 268. CrossRef - The Factors Influencing Compliance of Multidrug-resistant Organism Infection Control in Intensive Care Units Nurses
Ji Hee Kim, Kyung Hee Lim
Korean Journal of Adult Nursing.2015; 27(3): 325. CrossRef - Recognition and Performance Level of Hospital Infection Control in Nurses of Long-term Care Hospital
Ha-Yun Jung, Yun-Kyung Jung
The Korean Journal of Health Service Management.2013; 7(4): 131. CrossRef - Effects of Infection Control Education for Families of VRE Patients
Jung Seo, Ji-Yeon Kang
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(2): 212. CrossRef - Development and Evaluation of a Web-based Education Program for Nursing Students on Control of Vancomycin-resistant Enterococcus Infection
Ju Gong, Ji-Yeon Kang
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(1): 122. CrossRef - Knowledge and Compliance Level of the Multidrug-resistant Organisms of Nursing Students
Kyung-Mi Kim, Og-Son Kim, Mi-Yang Jeon
Journal of Korean Biological Nursing Science.2012; 14(1): 8. CrossRef - Status of and Factors Influencing Vaccination against the Pandemic (H1N1) 2009 Virus among University Students from the Fields of Nursing and Allied Health
Og Son Kim
Journal of Korean Academy of Nursing.2011; 41(3): 403. CrossRef
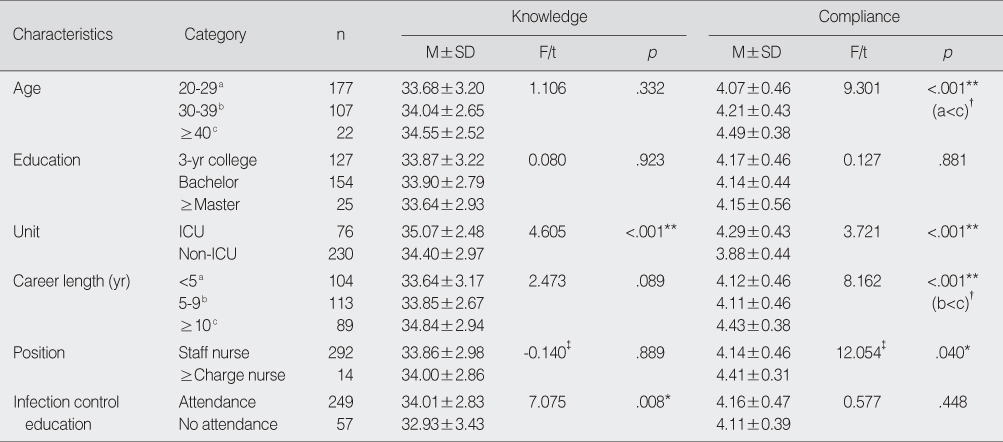
Knowledge and Compliance by General Characteristics (N=306)
*p<.05; **p<.001; †Scheffe's test; ‡Z of Mann Whitney U test.
ICU=intensive care unit; Non-ICU included medical, surgical, pediatric, obstetric/gynecology unit.
Knowledge & Compliance Scores on Multidrug-resistant Organism Infection Control Guidelines (N=306)
Top 10 High-ranking and Bottom 10 Low-ranking Items of Knowledge and Compliance Scales (N=306)
MRSA=Methicillin-resistant Staphylococcus aureus; MDRO=multidrug-resistant organism; VRE=Vancomycin-resistant enterococcus; BP=blood pressure.
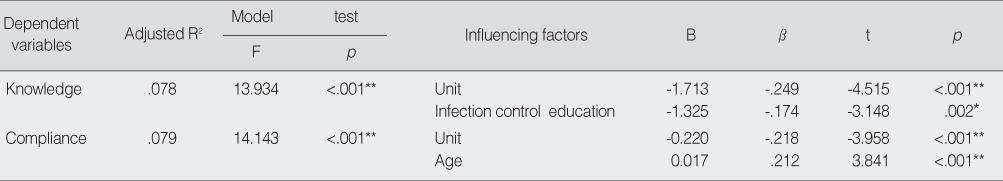
Stepwise Multiple Regression for Knowledge and Compliance
*p<.05; **p<.001.
Reasons for Noncompliance (N=306)
MDRO=multidrug-resistant organism.
* ICU=intensive care unit; Non-ICU included medical, surgical, pediatric, obstetric/gynecology unit.
MRSA=Methicillin-resistant Staphylococcus aureus; MDRO=multidrug-resistant organism; VRE=Vancomycin-resistant enterococcus; BP=blood pressure.
*
MDRO=multidrug-resistant organism.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

