Search
- Page Path
- HOME > Search
- The effects of a lifestyle intervention for men in infertile couples in South Korea: a non-randomized controlled trial
- Yun Mi Kim, Ju-Hee Nho
- J Korean Acad Nurs 2025;55(2):191-204. Published online April 16, 2025
- DOI: https://doi.org/10.4040/jkan.24104
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to evaluate the effects of an interaction model of client health behavior (IMCHB)-based lifestyle intervention on health-promoting behaviors, infertility stress, fertility-related quality of life, and semen quality in men in infertile couples.
Methods
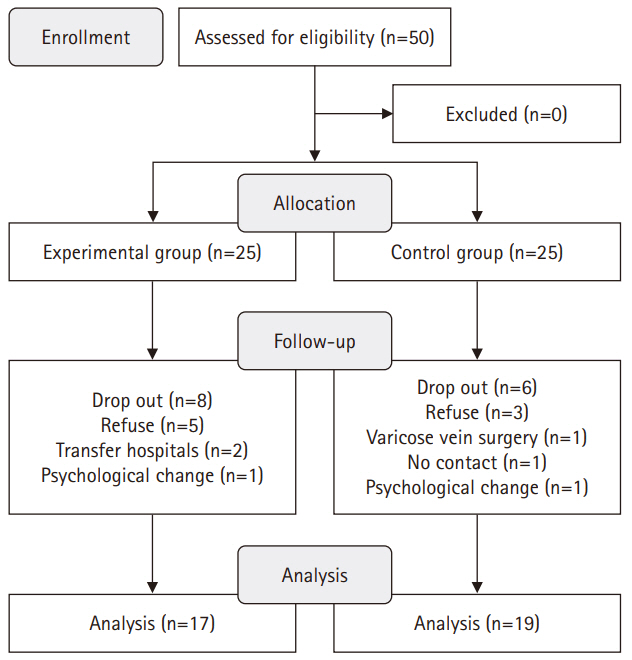
This study used a quasi-experimental, non-equivalent control group, pretest-posttest design, with participants divided into an experimental group (n=17) and a control group (n=19). The 16-session, 8-week intervention included components such as reproductive health education, physical activity, nutritional management, and stress management. Data collection occurred between July 1, 2021 and September 27, 2022. The outcomes measured included health-promoting behaviors, infertility stress, fertility-related quality of life, and sperm quality (volume, total motility, immobility, concentration, and normal morphology).
Results
The experimental group showed significant improvements in health-promoting behaviors (z=–2.27, p=.023) and reductions in infertility stress (t=–2.40, p=.022) compared to the control group. Total sperm motility (F=4.39, p=.045) and normal morphology (z=2.86, p=.017) were also significantly higher in the experimental group than in the control group.
Conclusion
The IMCHB-based lifestyle intervention significantly increased health-promoting behaviors, reduced infertility stress, and improved key sperm parameters, indicating its effectiveness in supporting the reproductive health of men in infertile couples. -
Citations
Citations to this article as recorded by- Psychological Stress and Male Infertility: Oxidative Stress as the Common Downstream Pathway
Aris Kaltsas, Stamatis Papaharitou, Fotios Dimitriadis, Michael Chrisofos, Nikolaos Sofikitis
Biomedicines.2026; 14(2): 259. CrossRef
- Psychological Stress and Male Infertility: Oxidative Stress as the Common Downstream Pathway
- 3,534 View
- 132 Download
- 1 Crossref

- Experience of Mothers with Babies by in Vitro Fertilization
- Myung Sun Yi, So Woo Lee, Myoung Ae Choe, Keum Soon Kim, Yun Mi Kim
- Journal of Korean Academy of Nursing 2001;31(1):55-67. Published online March 29, 2017
- DOI: https://doi.org/10.4040/jkan.2001.31.1.55
-
 Abstract
Abstract
 PDF
PDF A phenomenological study was conducted to investigate the experiences of mothers pregnant via in vitro fertilization (IVF). Sample of nine mothers participated. Ten theme clusters emerged when the formulated meanings were organized into categories. During the infertility period, the participants were subject to self- depreciation, envy, anxiety, and depression. It changed their priorities in life from a job-oriented life to one where having a baby was the most important thing. After trying numerous alternative therapies, IVF became their last hope in having a baby. Since the success rate for IVF is low (only 20-30%), the participants for the treatment were overwhelmed with uncertainty, and it led to further anxiety, depression and despair. Success of pregnancy gave them extreme satisfaction, but they became very cautious in their day-to-day life because of their fear of abortion and early delivery. Some were even worried about the side effect of IVF during the pregnancy. Finally, the delivery of the baby gave them relief from the obligation of having a baby. Women did not have any difficulties in rearing a "test tube baby" except in the case of twins. Most women had no ethical difficulty in having a baby by IVF. However they did not wish this information to be revealed to other people. They again turned to IVF to have a son(s) when the resultory child(s) was a daughter(s). This is because of the strong preference for sons in Korean society.
-
Citations
Citations to this article as recorded by- Development of an Uncertainty Scale for Infertile Women
Miok Kim, Sue Kim
Korean Journal of Women Health Nursing.2010; 16(4): 370. CrossRef
- Development of an Uncertainty Scale for Infertile Women
- 732 View
- 0 Download
- 1 Crossref

- Factors Related to Nurse Staffing Levels in Tertiary and General Hospitals
- Yun Mi Kim, Kyung Ja June, Sung Hyun Cho
- Journal of Korean Academy of Nursing 2005;35(8):1493-1499. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.8.1493
-
 Abstract
Abstract
 PDF
PDF Background Adequate staffing is necessary to meet patient care needs and provide safe, quality nursing care. In November 1999, the Korean government implemented a new staffing policy that differentiates nursing fees for inpatients based on nurse-to-bed ratios. The purpose was to prevent hospitals from delegating nursing care to family members of patients or paid caregivers, and ultimately deteriorating the quality of nursing care services.
Purpose To examine nurse staffing levels and related factors including hospital, nursing and medical staff, and financial characteristics.
Methods A cross-sectional design was employed using two administrative databases, Medical Care Institution Database and Medical Claims Data for May 1-31, 2002. Nurse staffing was graded from 1 to 6, based on grading criteria of nurse-to-bed ratios provided by the policy. The study sample consisted of 42 tertiary and 186 general acute care hospitals.
Results None of tertiary or general hospitals gained the highest nurse staffing of Grade 1 (i.e., less than 2 beds per nurse in tertiary hospitals; less than 2.5 beds per nurse in general hospitals). Two thirds of the general hospitals had the lowest staffing of Grade 6 (i.e., 4 or more beds per nurse in tertiary hospitals; 4.5 or more beds per nurse in general hospitals). Tertiary hospitals were better staffed than general hospitals, and private hospitals had higher staffing levels compared to public hospitals. Large-sized general hospitals located in metropolitan areas had higher staffing than other general hospitals. Occupancy rate was positively related to nurse staffing. A negative relationship between nursing assistant and nurse staffing was found in general hospitals. A greater number of physician specialists were associated with better nurse staffing.
Conclusions The staffing policy needs to be evaluated and modified to make it more effective in leading hospitals to increase nurse staffing.
-
Citations
Citations to this article as recorded by- High-Volume Hospital Had Lower Mortality of Severe Intracerebral Hemorrhage Patients
Sang-Won Park, James Jisu Han, Nam Hun Heo, Eun Chae Lee, Dong-Hun Lee, Ji Young Lee, Boung Chul Lee, Young Wha Lim, Gui Ok Kim, Jae Sang Oh
Journal of Korean Neurosurgical Society.2024; 67(6): 622. CrossRef - Relationship between the legal nurse staffing standard and patient survival after perioperative cardiac arrest: A cross-sectional analysis of Korean administrative data
Yunmi Kim, Jiyun Kim, Soon Ae Shin
International Journal of Nursing Studies.2019; 89: 104. CrossRef - Job Analysis of the Nursing Unit Managers of Women's Hospital Using DACUM Analysis
Kyoung-Suk Son, Kyung Sook Cho
Korean Journal of Women Health Nursing.2019; 25(3): 239. CrossRef - Determinants of Registered Nurse Skill Mix & Staffing Level in Korea
Su-Jin Cho, Jinhyun Kim
Journal of Korean Academy of Nursing Administration.2014; 20(1): 10. CrossRef - Structure of Nurse Labor Market and Determinants of Hospital Nurse Staffing Levels
Bohyun Park, Sukyung Seo, Taejin Lee
Journal of Korean Academy of Nursing.2013; 43(1): 39. CrossRef - Nurse staffing, quality of nursing care and nurse job outcomes in intensive care units
Sung‐Hyun Cho, Kyung Ja June, Yun Mi Kim, Yong Ae Cho, Cheong Suk Yoo, Sung‐Cheol Yun, Young Hee Sung
Journal of Clinical Nursing.2009; 18(12): 1729. CrossRef - Nurse Staffing and Patient Mortality in Intensive Care Units
Sung-Hyun Cho, Jeong Hae Hwang, Jaiyong Kim
Nursing Research.2008; 57(5): 322. CrossRef - Impact of nurse staffing level on emergency department market share
Jee-In Hwang, Hyejung Chang
Health Care Management Review.2007; 32(3): 245. CrossRef
- High-Volume Hospital Had Lower Mortality of Severe Intracerebral Hemorrhage Patients
- 1,142 View
- 2 Download
- 8 Crossref

- Estimation of Nursing Costs Based on Nurse Visit Time for Long-Term Care Services
- Eun-Kyung Kim, Yun Mi Kim, Myung Ae Kim
- J Korean Acad Nurs 2010;40(3):349-358. Published online June 30, 2010
- DOI: https://doi.org/10.4040/jkan.2010.40.3.349
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to estimate nursing costs and to establish appropriate nursing fees for long-term care services for community elders.
Methods Seven nurses participated in data collection related to visiting time by nurses for 1,100 elders. Data on material costs and management costs were collected from 5 visiting nursing agencies. The nursing costs were classified into 3 groups based on the nurse's visit time under the current reimbursement system of long-term care insurance.
Results The average nursing cost per minute was 246 won. The material costs were 3,214 won, management costs, 10,707 won, transportation costs, 7,605 won, and capital costs, 5,635 won per visit. As a result, the average cost of nursing services per visit by classification of nursing time were 41,036 won (care time <30 min), 46,005 won (care time 30-59 min), and 57,321 won (care time over 60 min).
Conclusion The results of the study indicate that the fees for nurse visits currently being charged for long-term care insurance should be increased. Also these results will contribute to baseline data for establishing appropriate nursing fees for long-term care services to maintain quality nursing and management in visiting nursing agencies.
-
Citations
Citations to this article as recorded by- Plan for Invigoration of Visiting Nursing Center in Long-Term Care Insurance for the Elderly - Through SWOT Analysis -
Do Hwa Byeon
Journal of Korean Public Health Nursing.2015; 29(2): 203. CrossRef - Activity-Based Costing Analysis of Nursing Activities in General Hospital Wards
Ho-Soon Yoon, Jinhyun Kim
Journal of Korean Academy of Nursing Administration.2013; 19(4): 449. CrossRef - Trends in Home-visit Nursing Care by Agencies' Characteristics under the National Long-term Care Insurance System
Jung Suk Lee, Rah Il Hwang, Eun Jeong Han
Journal of Korean Academy of Community Health Nursing.2012; 23(4): 415. CrossRef - Korean and United States: Comparison of Costs of Nursing Interventions
Sung-Jung Hong, Eun-Joo Lee
Korean Journal of Adult Nursing.2012; 24(4): 358. CrossRef - The Characteristics and Service Utilization of Home Nursing Care Beneficiaries Under the Korean Long Term Care Insurance
Jung-Suk Lee, Eun-Jeong Han, Im-Ok Kang
Journal of Korean Academy of Community Health Nursing.2011; 22(1): 33. CrossRef
- Plan for Invigoration of Visiting Nursing Center in Long-Term Care Insurance for the Elderly - Through SWOT Analysis -
- 1,870 View
- 1 Download
- 5 Crossref

- Variations in Nurse Staffing in Adult and Neonatal Intensive Care Units
- Sung Hyun Cho, Jeong Hae Hwang, Yun Mi Kim, Jae Sun Kim
- Journal of Korean Academy of Nursing 2006;36(5):691-700. Published online August 31, 2006
- DOI: https://doi.org/10.4040/jkan.2006.36.5.691
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to analyze variations in unit staffing and recommend policies to improve nursing staffing levels in intensive care units (ICUs).
Method A cross-sectional study design was used, employing survey data from the Health Insurance Review Agency conducted from June-July, 2003. Unitstaffing was measured using two indicators; bed-to-nurse (B/N) ratio (number of beds per nurse), and patient-to-nurse (P/N)ratio (number of average daily patients per nurse). Staffing levels were compared according to hospital and ICU characteristics.
Result A total of 414 institutions were operating 569 adult and 86 neonatal ICUs. Tertiary hospitals (n=42) had the lowest mean B/N (0.82) and P/N (0.76) ratios in adult ICUs, followed by general hospitals (B/N: 1.34, P/N: 0.97). Those ratios indicated that a nurse took care of 3 to 5 patients per shift. Neonatal ICUs had worse staffing and had greater variations in staffing ratios than adult ICUs. About 17% of adult and 26% of neonatal ICUs were staffed only by adjunct nurses who had responsibility for a general ward as well as the ICU.
Conclusion Stratification of nurse staffing levels and differentiation of ICU utilization fees based on staffing grades are recommended as a policy tool to improve nurse staffing in ICUs.
-
Citations
Citations to this article as recorded by- Development of a competency for professional oral hygiene care of endotracheally-intubated patients in the intensive care unit: development and validity evidence
Eun-Sil Choi, Hie-Jin Noh, Won-Gyun Chung, So-Jung Mun
BMC Health Services Research.2021;[Epub] CrossRef - Associated Factors with Performance of Infection Control for the Prevention of Ventilator-associated Pneumonia among Some Intensive Care Unit Nurses
Hyeon Hwa Lee, Mi Ah Han, Jong Park, Seong Woo Choi
Journal of Health Informatics and Statistics.2018; 43(1): 1. CrossRef - Influencing Factors on Nursing Practices for Healthcare-associated Infections Control in Intensive Care Unit
Soon Ok Kim, Jin Suk Ra
Korean Journal of Healthcare-Associated Infection Control and Prevention.2018; 23(2): 39. CrossRef - The Study of Preceptor Nurses’ Occupational Stress and Burden
Joohee Han, Eun Kwang Yoo
Korean Journal of Stress Research.2018; 26(1): 38. CrossRef - Financial Projection of the Nursing Fee Differentiation Policy Improvement Proposal in the National Health Insurance: Using a Break-even Analysis Model for the Optimal Nursing Fee
Sungjae Kim, Jinhyun Kim
Journal of Korean Academy of Nursing Administration.2013; 19(5): 565. CrossRef - Nurse Staffing and Patient Mortality in Intensive Care Units
Sung-Hyun Cho, Jeong Hae Hwang, Jaiyong Kim
Nursing Research.2008; 57(5): 322. CrossRef
- Development of a competency for professional oral hygiene care of endotracheally-intubated patients in the intensive care unit: development and validity evidence
- 967 View
- 6 Download
- 6 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


