-
Risk factors for the readmission of patients with diabetic ketoacidosis: a systematic review and meta-analysis
-
Hyerim Ji, Sun-Kyung Hwang
-
J Korean Acad Nurs 2025;55(4):634-650. Published online November 21, 2025
-
DOI: https://doi.org/10.4040/jkan.25072
-
-
 Abstract Abstract
 PDF PDF ePub ePub
- Purpose
This study aimed to identify risk factors associated with the readmission of patients with diabetic ketoacidosis (DKA) through a systematic review and meta-analysis.
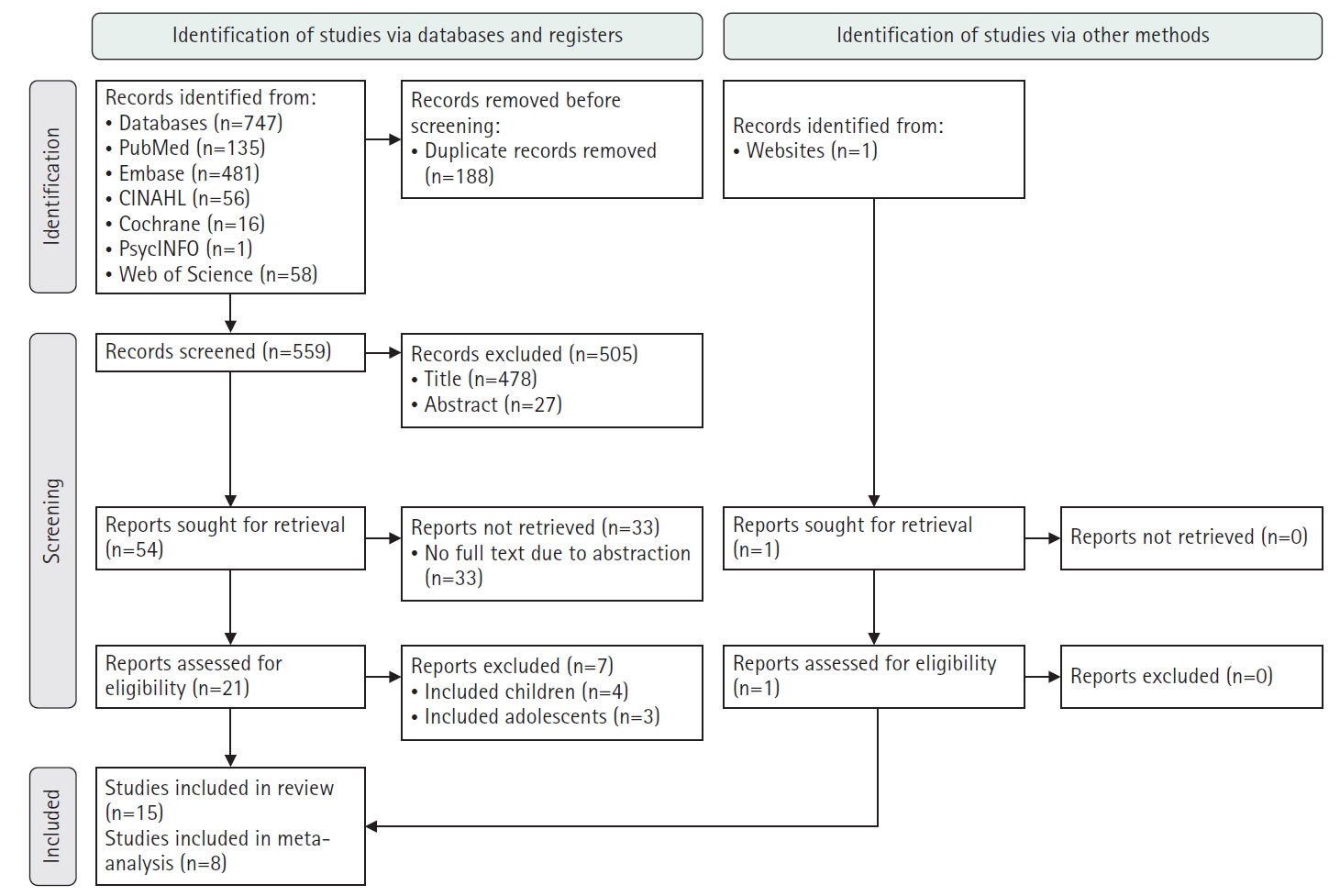
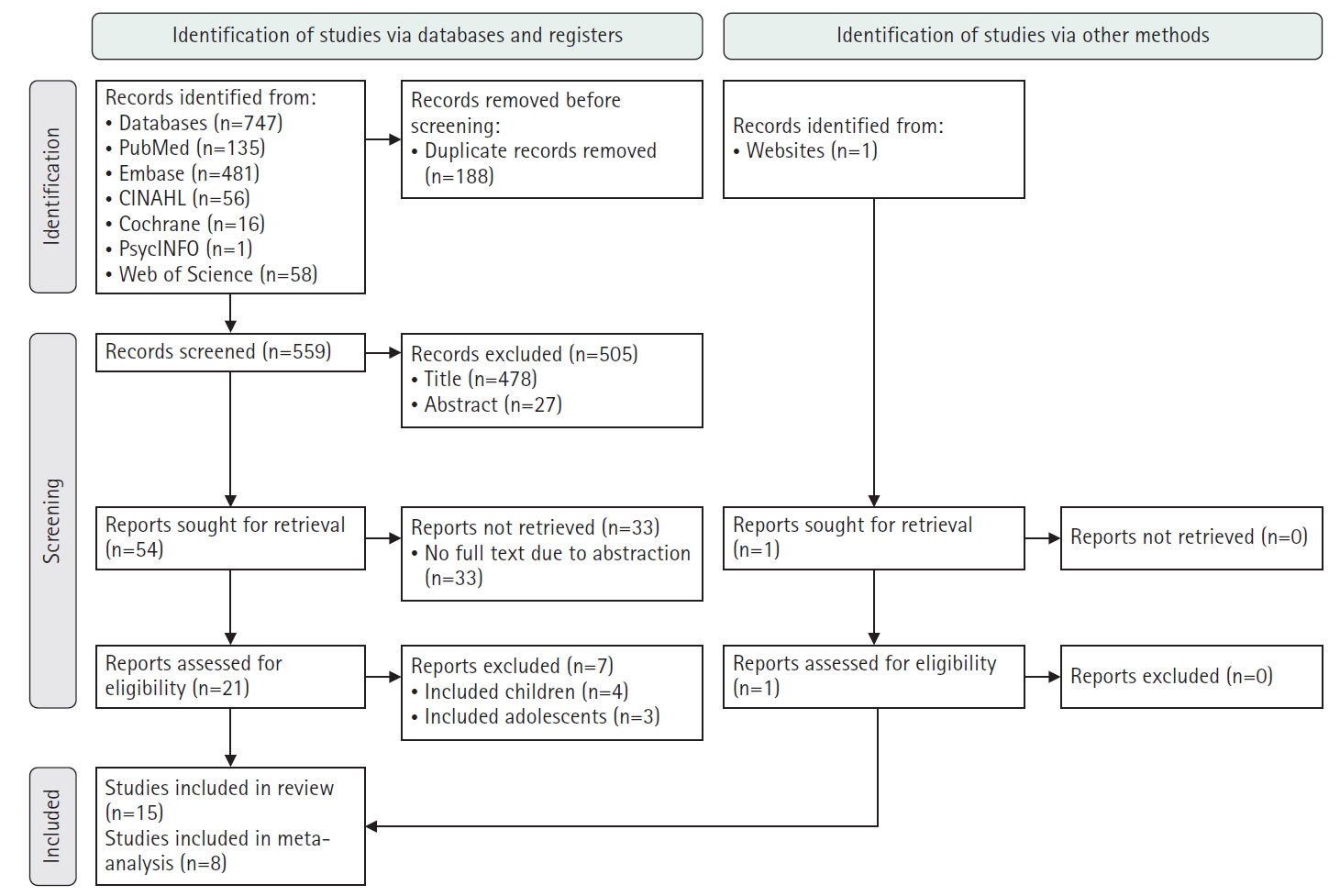
Methods
A systematic literature review was conducted in accordance with the PRISMA guidelines. Relevant studies were retrieved from international databases (PubMed, EMBASE, Cochrane Library, CINAHL, PsycINFO, and Web of Science) and Korean databases (RISS, KoreaMed, KMbase, KISS, and DBpia). Study quality was evaluated using the Newcastle-Ottawa Scale. Meta-analysis was performed using a random-effects model with the Hartung-Knapp-Sidik-Jonkman adjustment to account for the limited number of studies and heterogeneity.
Results
Fifteen studies were included in the review, and eight were eligible for meta-analysis. From the systematic review, 21 risk factors for DKA readmission were identified and categorized into five domains: demographic, socioeconomic, diabetes-related, comorbidity, and health-behavioral factors. In the meta-analysis, significant risk factors included low income, psychiatric disorders, and discharge against medical advice.
Conclusion
This study demonstrates that DKA readmissions result from the complex interplay of multiple clinical and social factors. By identifying these risk factors and suggesting risk-stratification criteria, the findings may support the development of tailored interventions, such as self-management education, integrated mental health care, structured discharge planning, and coordinated post-discharge follow-up.
-
A Structural Equation Modeling on Premenstrual Syndrome in Adolescent Girls
-
Jung-hee Jeon, Sun-kyung Hwang
-
J Korean Acad Nurs 2014;44(6):660-671. Published online December 31, 2014
-
DOI: https://doi.org/10.4040/jkan.2014.44.6.660
-
-
 Abstract Abstract
 PDF PDF
-
Purpose
The aims of this study were to construct a hypothetical structural model which explains the premenstrual syndrome (PMS) in adolescent girls and to test the fitness with collected data.
Methods
The participants were 1,087 adolescent girls from 3 high schools and 5 middle schools in B city. Data were collected from July 3 to October 15, 2012 using self-reported questionnaires and were analyzed using PASW 18.0 and AMOS 16.0 programs.
Results
The overall fitness indices of hypothetical model were good (χ2 =1555, p<.001), χ2/df=4.40, SRMR=.04, GFI=.91, RMSEA=.05, NFI=.90, TLI=.91, CFI=.92, AIC=1717). Out of 16 paths, 12 were statistically significant. Daily hassles had the greatest impact on PMS in the adolescent girls in this model. In addition, PMS in adolescent girls was directly affected by menarche age, Body Mass Index (BMI), amount of menstruation, test anxiety, social support, menstrual attitude and femininity but not by academic stress. This model explained 27% of the variance in PMS in adolescent girls.
Conclusion
The findings from this study suggest that nursing interventions to reduce PMS in adolescent girls should address their daily hassles, test anxiety, menstrual attitude and BMI. Also, social support from their parents, friends, and teachers needs to be increased.
-
Citations
Citations to this article as recorded by  - Premenstrual Sendrom ile Algılanan Stres ve Gece Yeme Sendromu İlişkisi
Rabia Kahvacı, Keziban Amanak
Bilecik Şeyh Edebali Üniversitesi Sağlık Bilimleri Fakültesi Dergisi.2024; 2(2): 102. CrossRef - Factors influencing health-related quality of life in adolescent girls: a path analysis using a multi-mediation model
Hyunjeong Shin, Songi Jeon, Inhae Cho
Health and Quality of Life Outcomes.2022;[Epub] CrossRef - According to Some Variables in Girls A High School Determining the Premenstrual Syndrome Violence and Perceped Stress Level
Nuriye ERBAŞ, Nermin ALTUNBAŞ
Acibadem Universitesi Saglik Bilimleri Dergisi.2021;[Epub] CrossRef - The Influence of Female University Students' Life Style, Women's Health Characteristics, and Endocrine Disrupting Chemicals on Menstrual Symptoms
Bo Gyeong Lee, Nam Hee Kim
Journal of The Korean Society of Maternal and Child Health.2021; 25(2): 88. CrossRef - Do depression, fatigue, and body esteem influence premenstrual symptoms in nursing students?
Eun Joo Lee, Seung Kyoung Yang
Korean Journal of Women Health Nursing.2020; 26(3): 231. CrossRef - Secondary Data Analysis on the Factors Influencing Premenstrual Symptoms of Shift Work Nurses: Focused on the Sleep and Occupational Stress
Jihyun Baek, Smi Choi-Kwon
Journal of Korean Academy of Nursing.2020; 50(4): 631. CrossRef - Effects of Sleep Pattern, Stress, Menstrual Attitude, and Behavior That Reduces Exposure to Endocrine Disrupting Chemicals on Premenstrual Syndrome in Adolescents
Hye Jin Kim, So Young Choi, Haeyoung Min
Korean Journal of Women Health Nursing.2019; 25(4): 423. CrossRef - Factors Influencing Functional Health of Patients with Chronic Insomnia based on Theory of Unpleasant Symptoms
Eun Kyoung Han, Sunah Kim, In-Young Yoon
Korean Journal of Adult Nursing.2019; 31(2): 165. CrossRef - Relationship between Menstrual Distress and Sleep Disturbance in Middle-school Girls
Se Yeong Park, SoMi Park
Korean Journal of Women Health Nursing.2018; 24(4): 392. CrossRef - Development and psychometric validation of the Menstrual Health Instrument (MHI) for adolescents in Korea
Hyunjeong Shin, Young-Joo Park, Inhae Cho
Health Care for Women International.2018; 39(10): 1090. CrossRef - A Structural Model for Premenstrual Coping in University Students: Based on Biopsychosocial Model
Myung-Ock Chae, Hae Ok Jeon, Ahrin Kim
Journal of Korean Academy of Nursing.2017; 47(2): 257. CrossRef
-
1,199
View
-
10
Download
-
11
Crossref
|