Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 55(1); 2025 > Article
-
Research Paper
- Effects of a nursing leadership program on self-leadership, interpersonal relationships, clinical performance, problem-solving abilities, and nursing professionalism among nursing students in South Korea: a quasi-experimental study
-
Sunmi Kim1
 , Young Ju Jeong2
, Young Ju Jeong2 , Hee Sun Kim3
, Hee Sun Kim3 , Seok Hee Jeong3
, Seok Hee Jeong3 , Eun Jee Lee3
, Eun Jee Lee3
-
Journal of Korean Academy of Nursing 2025;55(1):137-151.
DOI: https://doi.org/10.4040/jkan.24110
Published online: February 25, 2025
1College of Nursing, Woosuk University, Wanju, Korea
2Department of Nursing, Wonkwang Health Science University, Iksan, Korea
3College of Nursing, Research Institute of Nursing Science, Jeonbuk National University, Jeonju, Korea
- Corresponding author: Hee Sun Kim College of Nursing, Research Institute of Nursing Science, Jeonbuk National University, 567 Baekje-daero, Deokjin-gu, Jeonju 54896, Korea E-mail: joha0219@jbnu.ac.kr
- †This work was presented at 2023 Yonsei International Nursing Conference (2023 YINC), October 2023, Seoul, Republic of Korea.
© 2025 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License (http://creativecommons.org/licenses/by-nd/4.0) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- This study investigated the effects of a nursing leadership program on self-leadership, interpersonal relationships, clinical performance, problem-solving abilities, and nursing professionalism among nursing students in South Korea.
-
Methods
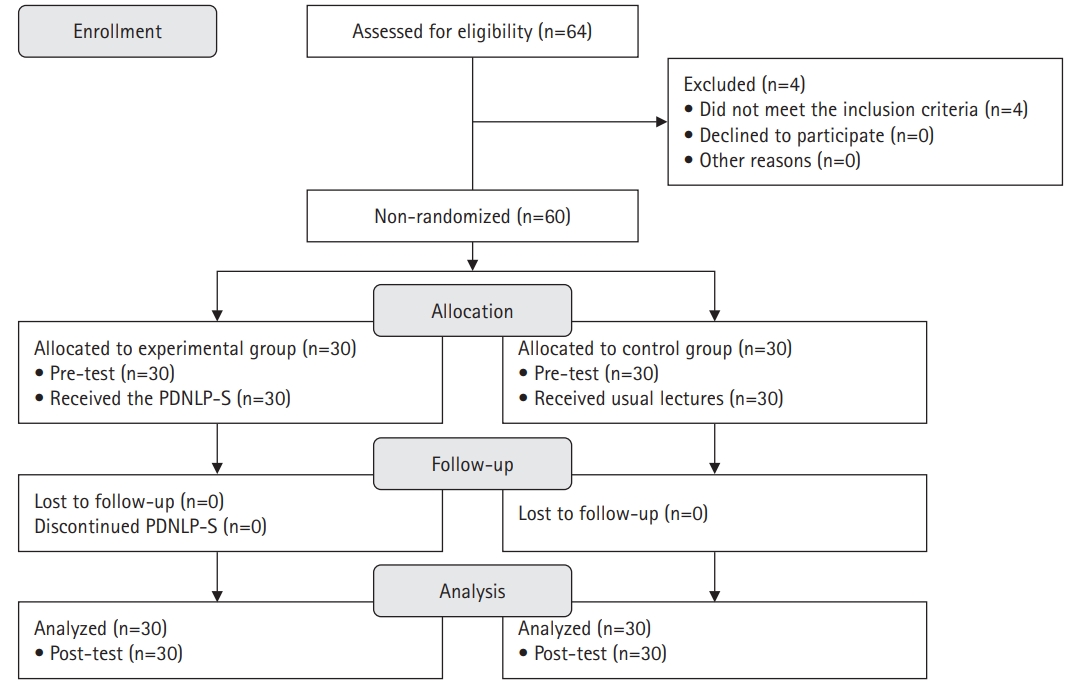
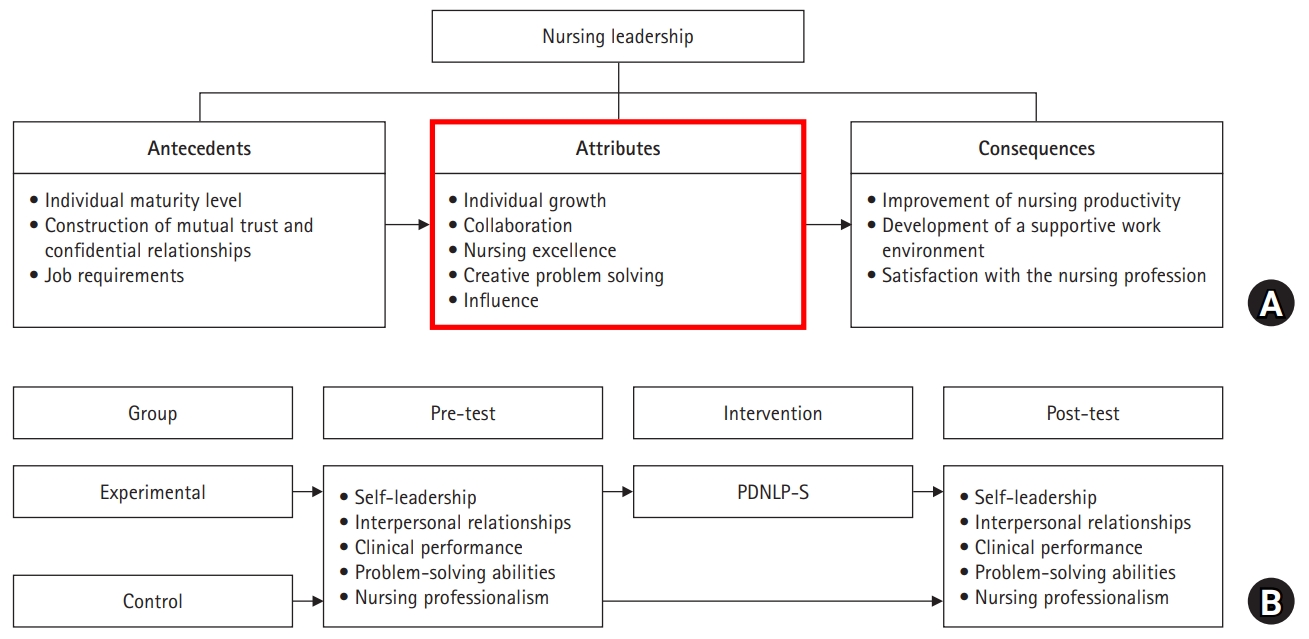
- A quasi-experimental study was conducted. The Practice-Driven Nursing Leadership Program for Students (PDNLP-S) was developed based on the ADDIE model (analysis, design, development, implementation, and evaluation). This quasi-experimental study design included 60 nursing students. The experimental group (n=30) participated in the PDNLP-S for 120-minute sessions over 5 weeks, while the control group (n=30) received usual lectures. The PDNLP-S included lectures, discussions, and individual and group activities to cultivate core nursing leadership competencies such as individual growth, collaboration, nursing excellence, creative problem-solving, and influence. Data were analyzed using descriptive statistics, the Mann-Whitney U-test, and the independent t-test with IBM SPSS Windows ver. 26.0.
-
Results
- The experimental group demonstrated significant improvements in self-leadership (t=3.28, p=.001), interpersonal relationships (t=3.07, p=.002), clinical performance (U=268.50, p=.004), and problem-solving abilities (t=2.20, p=.017) compared to the control group. No significant difference was observed in nursing professionalism (t=0.50, p=.311).
-
Conclusion
- This study demonstrates that the PDNLP-S improved nursing students’ self-leadership, interpersonal relationships, clinical performance, and problem-solving abilities. The PDNLP-S can play a significant role in cultivating future nurse leaders by enhancing these nursing leadership competencies among nursing students.
Introduction
Methods
1) Demographic questionnaire
2) Self-leadership
3) Interpersonal relationships
4) Clinical performance
5) Problem-solving ability
6) Nursing professionalism
Results
Discussion
Conclusion
-
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
-
Acknowledgements
None.
-
Data Sharing Statement
Please contact the corresponding author for data availability.
-
Author Contributions
Conceptualization or/and Methodology: SK, YJJ, HSK, SHJ, EJL. Data curation or/and Analysis: SK, YJJ. Funding acquisition: HSK. Investigation: SK, YJJ. Project administration or/and Supervision: HSK, SHJ. Resources or/and Software: SK, YJJ. Validation: SK, YJJ, HSK, SHJ, EJL. Visualization: SK, YJJ, HSK, SHJ, EJL. Writing: original draft or/and Review & Editing: SK, YJJ, HSK, SHJ, EJL. Final approval of the manuscript: all authors.
Article Information
- 1. Northouse PG. Leadership: theory and practice. 7th ed. SAGE Publications; 2016.
- 2. Booher L, Yates E, Claus S, Haight K, Burchill CN. Leadership self-perception of clinical nurses at the bedside: a qualitative descriptive study. J Clin Nurs. 2021;30(11-12):1573-1583. https://doi.org/10.1111/jocn.15705ArticlePubMed
- 3. Kim JS, Kim YM, Jang KS, Kim BN, Jeong SH. Concept analysis of nursing leadership. J Korean Acad Nurs Adm. 2015;21(5):575-586. https://doi.org/10.11111/jkana.2015.21.5.575Article
- 4. Aqtash S, Alnusair H, Brownie S, Alnjadat R, Fonbuena M, Perinchery S. Evaluation of the impact of an education program on self-reported leadership and management competence among nurse managers. SAGE Open Nurs. 2022;8:23779608221106450. https://doi.org/10.1177/23779608221106450ArticlePubMedPMC
- 5. Kim J, Kim MA, Lee SJ, Kim EJ. Effects of leadership program on self-leadership and self-esteem in nursing students. J Korean Data Anal Soc [Internet]. 2015 [cited 2023 Aug 30];17(1B):575-586. Available from: https://www.dbpia.co.kr/Journal/articleDetail?nodeId=NODE08964828
- 6. Brown A, Crookes P, Dewing J. Clinical leadership in pre-registration nursing programmes: an international literature review. Contemp Nurse. 2015;51(1):39-55. https://doi.org/10.1080/10376178.2015.1095055ArticlePubMed
- 7. Miles JM, Scott ES. A new leadership development model for nursing education. J Prof Nurs. 2019;35(1):5-11. https://doi.org/10.1016/j.profnurs.2018.09.009ArticlePubMed
- 8. Cummings GG, Lee S, Tate K, Penconek T, Micaroni SP, Paananen T, et al. The essentials of nursing leadership: a systematic review of factors and educational interventions influencing nursing leadership. Int J Nurs Stud. 2021;115:103842. https://doi.org/10.1016/j.ijnurstu.2020.103842ArticlePubMed
- 9. American Association of Colleges of Nursing. The essentials: core competencies for professional nursing education [Internet]. American Association of Colleges of Nursing; 2021 [cited 2024 Dec 30]. Available from: https://www.aacnnursing.org/Essentials/Download-Order
- 10. Korean Accreditation Board of Nursing Education. Standard book for accreditation board of nursing education [Internet]. Korean Accreditation Board of Nursing Education; 2017 [cited 2024 Dec 30]. Available from: http://www.kabone.or.kr/eng/edu/accreditation.do
- 11. Démeh W, Rosengren K. The visualisation of clinical leadership in the content of nursing education: a qualitative study of nursing students’ experiences. Nurse Educ Today. 2015;35(7):888-893. https://doi.org/10.1016/j.nedt.2015.02.020ArticlePubMed
- 12. Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2010;47(3):363-385. https://doi.org/10.1016/j.ijnurstu.2009.08.006ArticlePubMed
- 13. Harley J. Developing self-awareness for effective nurse leadership. Nurs Manag (Harrow). 2024 May 22 [Epub]. https://doi.org/10.7748/nm.2024.e2124ArticlePubMed
- 14. Kaiser L, Conrad S, Neugebauer EA, Pietsch B, Pieper D. Interprofessional collaboration and patient-reported outcomes in inpatient care: a systematic review. Syst Rev. 2022;11(1):169. https://doi.org/10.1186/s13643-022-02027-xArticlePubMedPMC
- 15. Jang KS, Lee MH, Kim BN, Kim YM, Kim EA, Kim JS, et al. Practice-driven nursing leadership. Hakjisa Medical; 2018.
- 16. Kohnen D, De Witte H, Schaufeli WB, Dello S, Bruyneel L, Sermeus W. Engaging leadership and nurse well-being: the role of the work environment and work motivation-a cross-sectional study. Hum Resour Health. 2024;22(1):8. https://doi.org/10.1186/s12960-023-00886-6ArticlePubMedPMC
- 17. Neck CP, Manz CC, Houghton JD. Self-leadership: the definitive guide to personal excellence. 2nd ed. Sage Publications; 2019.
- 18. Ntshingila N, Downing C, Hastings-Tolsma M. A concept analysis of self-leadership: the “bleeding edge” in nursing leadership. Nurs Forum. 2021;56(2):404-412. https://doi.org/10.1111/nuf.12551ArticlePubMed
- 19. Kowalski MO, Basile C, Bersick E, Cole DA, McClure DE, Weaver SH. What do nurses need to practice effectively in the hospital environment?: an integrative review with implications for nurse leaders. Worldviews Evid Based Nurs. 2020;17(1):60-70. https://doi.org/10.1111/wvn.12401ArticlePubMed
- 20. Leonard JC, Whiteman K, Stephens K, Henry C, Swanson-Biearman B. Improving communication and collaboration skills in graduate nurses: an evidence-based approach. Online J Issues Nurs. 2022;27(2):Man03. https://doi.org/10.3912/OJIN.Vol27No02Man03Article
- 21. Ariga RA, Aurelia R, Anak Ampun PT, Hutabarat CP, Panjaitan FB. Enhancing nursing excellence: exploring the relationship between nurse deployment and performance. Int J Environ Res Public Health. 2024;21(10):1309. https://doi.org/10.3390/ijerph21101309ArticlePubMedPMC
- 22. Nachtergaele S, De Roo N, Allart J, De Vriendt P, Embo M, Cornelis E. Exploring influencing factors to clinical leadership development: a qualitative study with healthcare professionals in Flemish nursing homes. BMC Health Serv Res. 2024;24(1):1169. https://doi.org/10.1186/s12913-024-11613-9ArticlePubMedPMC
- 23. Choi MS. A study on the relationship between teaching effectiveness of clinical nursing education and clinical competency in nursing students [master’s thesis]. Seoul: Ewha Woman’s University; 2005.
- 24. Nabizadeh-Gharghozar Z, Alavi NM, Ajorpaz NM. Clinical competence in nursing: a hybrid concept analysis. Nurse Educ Today. 2021;97:104728. https://doi.org/10.1016/j.nedt.2020.104728ArticlePubMed
- 25. Lee WS, Park SH, Choi EY. Development of a Korean problem solving process inventory for adults. J Korean Acad Fundam Nurs [Internet]. 2008 [cited 2024 Dec 30];15(4):548-557. Available from: https://j.kafn.or.kr/upload/pdf/jkafn-15-4-548.pdf
- 26. Guibert-Lacasa C; Vázquez-Calatayud M. Nurses’ clinical leadership in the hospital setting: a systematic review. J Nurs Manag. 2022;30(4):913-925. https://doi.org/10.1111/jonm.13570ArticlePubMedPMC
- 27. Yeun EJ, Kwon YM, Ahn OH. Development of a nursing professional values scale. J Korean Acad Nurs. 2005;35(6):1091-1100. https://doi.org/10.4040/jkan.2005.35.6.1091ArticlePubMed
- 28. He X, Mao Y, Cao H, Li L, Wu Y, Yang H. Factors influencing the development of nursing professionalism: a descriptive qualitative study. BMC Nurs. 2024;23(1):283. https://doi.org/10.1186/s12912-024-01945-6ArticlePubMedPMC
- 29. Jung KS, Oh EJ. The effects of nursing professionalism, nurse’s image on self-leadership in nursing students. J Korean Acad Ind Coop Soc. 2021;22(10):66-75. https://doi.org/10.5762/KAIS.2021.22.10.66Article
- 30. Hajizadeh A, Zamanzadeh V, Kakemam E, Bahreini R, Khodayari-Zarnaq R. Factors influencing nurses participation in the health policy-making process: a systematic review. BMC Nurs. 2021;20(1):128. https://doi.org/10.1186/s12912-021-00648-6ArticlePubMedPMC
- 31. Välimäki M, Hu S, Lantta T, Hipp K, Varpula J, Chen J, et al. The impact of evidence-based nursing leadership in healthcare settings: a mixed methods systematic review. BMC Nurs. 2024;23(1):452. https://doi.org/10.1186/s12912-024-02096-4ArticlePubMedPMC
- 32. Williamson GR, Kane A, Evans S, Attrill L, Cook F, Nash K. Student nurses as a future general practice nursing workforce: implementing collaborative learning in practice: implications for placement learning and patient access: a mixed methods study. BMC Nurs. 2023;22(1):326. https://doi.org/10.1186/s12912-023-01501-8ArticlePubMedPMC
- 33. Bae SH, Park JS. Development and evaluation of extracurricular coaching programs for improving communication skills and leadership among nursing students. J Korean Acad Soc Nurs Educ. 2015;21(2):202-214. https://doi.org/10.5977/jkasne.2015.21.2.202Article
- 34. Kim KH. The effects of action learning on self-leadership and class satisfaction in nursing students. J Learn Cent Curric Instr. 2019;19(23):1221-1236. https://doi.org/10.22251/jlcci.2019.19.23.1221Article
- 35. Huston CJ. Leadership roles and management function in nursing: theory and application. 11th ed. Lippincott Williams & Wilkins; 2023.
- 36. James AH, Watkins D, Carrier J. Perceptions and experiences of leadership in undergraduate nurse education: a narrative inquiry. Nurse Educ Today. 2022;111:105313. https://doi.org/10.1016/j.nedt.2022.105313ArticlePubMed
- 37. Statistical power analyses using G*Power 3. 1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149-1160. https://doi.org/10.3758/BRM.41.4.1149ArticlePubMed
- 38. Dick W. A model for the systematic design of instruction. In: Tennyson RD, Schott F, Seel NM, Dijkstra S, editors. Instructional design: international perspectives: theory, research, and models. Routledge; 2013. p. 361-370.
- 39. Houghton JD, Neck CP. The revised self‐leadership questionnaire: testing a hierarchical factor structure for self‐leadership. J Manag Psychol. 2002;17(8):672-691. https://doi.org/10.1108/02683940210450484Article
- 40. Buhrmester D, Furman W, Wittenberg MT, Reis HT. Five domains of interpersonal competence in peer relationships. J Pers Soc Psychol. 1988;55(6):991-1008. https://doi.org/10.1037//0022-3514.55.6.991ArticlePubMed
- 41. Han N, Lee DG. Validation of the Korean version of the Interpersonal Competence Questionnaire in Korean college students. Korean J Couns Psychother [Internet]. 2010 [cited 2024 Dec 30];22(1):137-156. https://www.kci.go.kr/kciportal/ci/sereArticleSearch/ciSereArtiView.kci?sereArticleSearchBean.artiId=ART001422199
- 42. Lee WH, Kim CJ, Yoo JS, Hur HK, Kim KS, Lim SM. Development of a clinical competency measurement tool for students. J Nurs Sci. 1991;13:17-29.
- 43. Han SS, Kim MH, Yun EK. Factors affecting nursing professionalism. J Korean Acad Soc Nurs Educ. 2008;14(1):73-79. https://doi.org/10.5977/JKASNE.2008.14.1.073Article
- 44. Park JH. The effect of self-leadership program for nursing students on empowerment, self-directed learning, and happiness. J Korea Acad Ind Coop Soc. 2019;20(7):61-67. https://doi.org/10.5762/KAIS.2019.20.7.61Article
- 45. Wakefield MK, Williams DR, Le Menestrel S, Flaubert JL; National Academies of Sciences, Engineering, and Medicine. The future of nursing 2020-2030: charting a path to achieve health equity. National Academies Press; 2021. https://doi.org/10.17226/25982
- 46. Ni YX, Wu D, Bao Y, Li JP, You GY. Nurses’ perceptions of career growth: a qualitative descriptive study. J Adv Nurs. 2022;78(11):3795-3805. https://doi.org/10.1111/jan.15376ArticlePubMed
- 47. Ma X, Yang Y, Wang X, Zang Y. An integrative review: developing and measuring creativity in nursing. Nurse Educ Today. 2018;62:1-8. https://doi.org/10.1016/j.nedt.2017.12.011ArticlePubMed
- 48. Bimray P, Jooste K, Julie H. Professionalism experiences of undergraduate learner nurses during their 4-year training programme at a Higher Education Institution in the Western Cape, South Africa. Curationis. 2019;42(1):e1-e8. https://doi.org/10.4102/curationis.v42i1.2030ArticlePubMedPMC
- 49. Park HR, Jun H, Ban MK. The effects of transitional shock and incivility experienced by nursing student on nursing professionalism. J East West Nurs Res. 2021;27(1):78-86. https://doi.org/10.14370/jewnr.2021.27.1.78Article
- 50. Miao C, Liu C, Zhou Y, Zou X, Song L, Chung JW, et al. Nurses’ perspectives on professional self-concept and its influencing factors: a qualitative study. BMC Nurs. 2024;23(1):237. https://doi.org/10.1186/s12912-024-01834-yArticlePubMedPMC
References
Figure & Data
REFERENCES
Citations

- Self-Determination Theory in Return to Work Interventions: A Scoping Review
Kexin Chen, Ling Yang, Jiajia Tu
Journal of Multidisciplinary Healthcare.2025; Volume 18: 7539. CrossRef
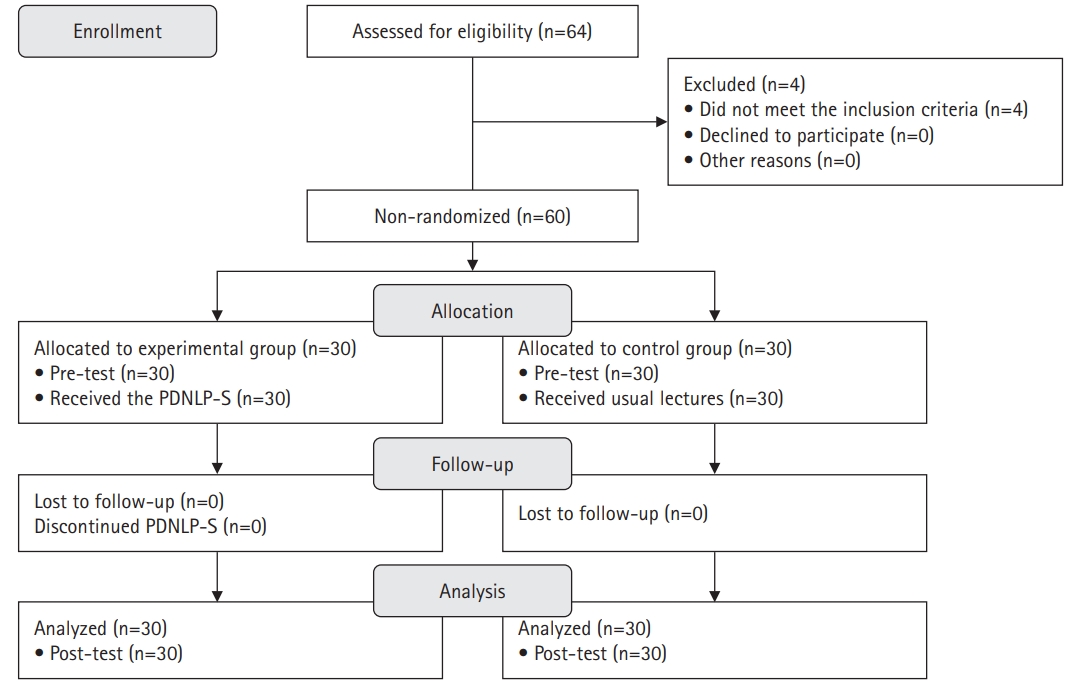
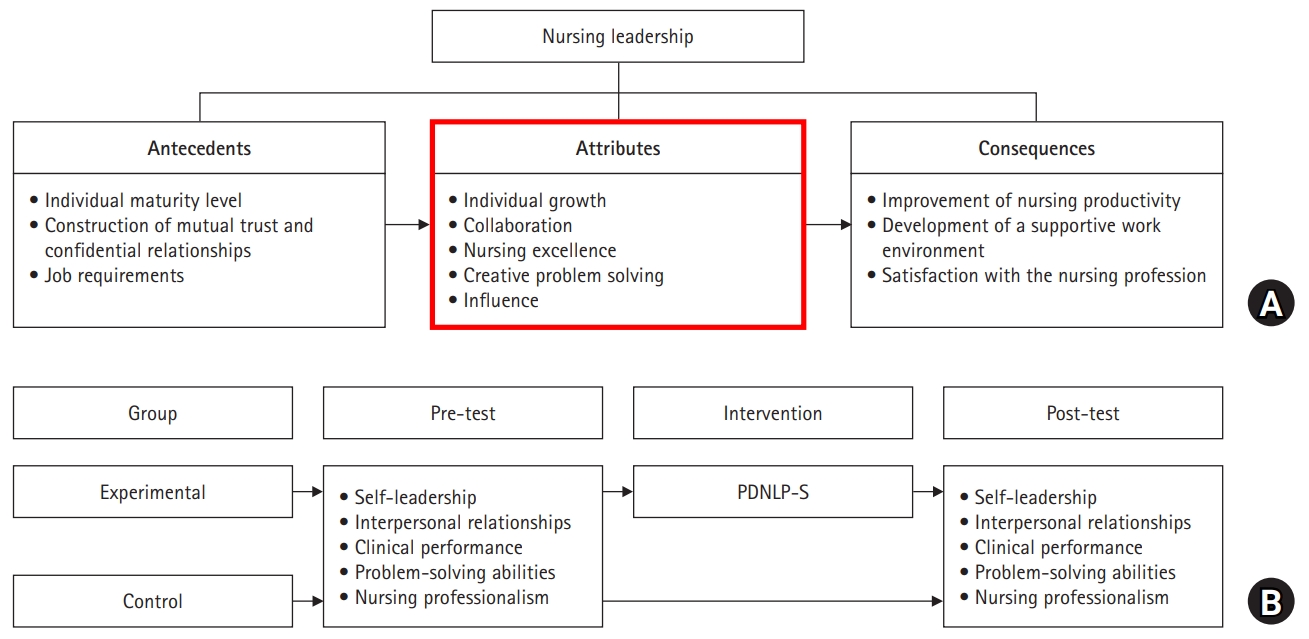
Fig. 1.
Fig. 2.
| Session | Activity name | Learning objectives | Key themes | Methods | Main contents | Tool | Duration (min) |
|---|---|---|---|---|---|---|---|
| 1 | Understanding leadership | • Understand the concept of leadership. | • Concept and rationale for leadership | • Lecture | • Introduction to the program | • PPT | 20 |
| • Understand theories of leadership. | • Understanding of leadership theories | • Team discussion and team presentations | • Lecture | • PPT | 30 | ||
| • Team activities: Team building, introduction of self, team activity plan | • Notebook; Smartphone | 50 | |||||
| • Team presentation: Topic selection and sharing | |||||||
| 2 | Empathy class: Understanding others’ leadership styles | • Understand leadership. | • Understanding of leadership | • Key summary | • Summary of leadership theories | • PPT | 20 |
| • Recognize the importance of teamwork. | • Teamwork training | • Team presentations | • Team activities: Share each leadership style and team discussion for understanding the nursing leadership | • PPT; Video | 60 | ||
| • Communicate effectively with team members. | • Communication | • Feedback | • Team presentation: Leadership styles and survey results; Introduce persons based on leadership styles | ||||
| • Feedback: Sharing and empathizing with team presentations | - | 20 | |||||
| 3 | Discovering myself: Understanding my leadership style | • Understand nursing leadership. | • Understanding of nursing leadership | • Key summary | • Summary of self-understanding and self-exploration | • PPT | 20 |
| • Communicate effectively with team members. | • Communication | • Individual activities and presentations | • Individual activity: Identifying one’s leadership style | • Survey | 20 | ||
| • Feedback | • Individual leadership development plan: Goal setting; SMART planning (specific, measurable, action-oriented, realistic, time-bound) | • Notebook; Smartphone | 40 | ||||
| • Feedback: Sharing and empathizing with individual activities | - | 20 | |||||
| 4 | My commitment | • Recognize the importance of self-understanding. | • Self-understanding and self-analysis | • Key summary | • Summary of the importance of self-understanding | - | 20 |
| • Establish nursing leadership development plans. | • Living with others | • Individual presentations and feedback | • Individual presentations: Leadership development plan; Reflecting on self; Understanding and exploring your current leadership; Setting your own visions and goals for a nurse leader; Understanding others | • PPT; Smartphone | 60 | ||
| • Self-leadership development plans | • Feedback: Sharing and empathizing with leadership plans | - | 20 | ||||
| 5–7 | Understanding and practicing nursing leadership 1 | • Understand the attributes of nursing leadership. | • Develop and apply nursing leadership: Individual growth; Collaboration; Nursing excellence | • Lecture | • Lecture: Nursing leadership: Understand individual growth, collaboration and nursing excellence; Learn about success stories | • PPT; Video | 30 |
| • Execute nursing leadership development plans. | • Individual growth, collaboration and nursing excellence development plans | • Team discussion and presentations | • Team activity: Discussion about cases based on individual growth, collaboration or nursing excellence | • Notebook; Textbook; Worksheet | 50 | ||
| • Recognize the importance of self-management. | • Feedback | • Individual activity: Doing develops plans for individual growth, collaboration and nursing excellence; Self-monitoring and activity records | • Self-record for leadership improvement: Vlog, gratitude journal, exercise log, nursing policy scrapbook, study plan, etc. | 20 | |||
| 8–9 | Understanding and practicing nursing leadership 2 | • Understand the attributes of nursing leadership. | • Develop and apply nursing leadership: Creative problem solving; Influence | • Lecture | • Lecture: Nursing leadership: Understanding creative problem solving and influence; Learn about success stories | • PPT; Video | 30 |
| • Execute nursing leadership development plans. | • Creative problem solving and influence development plans | • Team discussion and presentations | • Team activity and presentation: Discussion about cases based on creative problem solving and influence; Introducing influential figures | • Notebook; Textbook; Worksheet | 50 | ||
| • Recognize the importance of self-management. | • Feedback | • Individual activity: Doing develops plans of creative problem solving and influence; Self-monitoring and activity records | • Self-record for leadership improvement: Vlog, gratitude journal, exercise log, nursing policy scrapbook, study plan, etc. | 20 | |||
| 10 | Reflecting on myself | • Attain the core nursing leadership competencies. | • Evaluate nursing leadership | • Key summary | • Explanation of nursing leadership | - | 10 |
| • Individual activities and presentations | • Individual presentations and feedback: Sharing results based on individual leadership development action plans | • PPT; Self-record for leadership improvement: Vlog, gratitude journal, exercise log, nursing policy scrapbook, study plan, etc. | 70 | ||||
| • Feedback | • Evaluate program: Reflecting on the program and setting future goals | - | 20 |
| Variable | Experimental (n=30) | Control (n=30) | χ2 or t or U | p |
|---|---|---|---|---|
| Gender | 0.22a) | .500 | ||
| Women | 27 (90.0) | 28 (93.3) | ||
| Men | 3 (10.0) | 2 (6.7) | ||
| Age (yr) | 23.6±1.10 (22–27) | 23.6±1.99 (22–32) | 0.01 | .500 |
| Religion | 0.08 | .391 | ||
| Yes | 10 (33.3) | 9 (30.0) | ||
| No | 20 (66.7) | 21 (70.0) | ||
| Satisfaction with the nursing major | 1.31a) | .171 | ||
| Satisfied | 17 (56.7) | 19 (63.3) | ||
| Neutral | 8 (26.7) | 10 (33.3) | ||
| Dissatisfied | 5 (16.6) | 1 (3.4) | ||
| Academic achievement | 1.30a) | .309 | ||
| High | 13 (43.3) | 14 (46.7) | ||
| Middle | 16 (53.3) | 13 (43.3) | ||
| Low | 1 (3.4) | 3 (10.0) | ||
| Self-leadership (range, 1–5) | 3.43±0.32 | 3.46±0.42 | –0.29 | .387 |
| Interpersonal relationships (range, 1–5) | 3.37±0.57 | 3.49±0.46 | –0.87 | .194 |
| Clinical performance (range, 1–5) | 3.65±0.52 | 3.85±0.61 | 343.00b) | .057 |
| Problem-solving abilities (range, 1–5) | 3.75±0.72 | 3.85±0.63 | –0.58 | .282 |
| Nursing professionalism (range, 1–5) | 3.75±0.57 | 3.73±0.51 | 0.16 | .437 |
| Variable | Pre-test | Post-test | Difference | t or U | p | Effect size d | Power |
|---|---|---|---|---|---|---|---|
| Self-leadership | 3.28 | .001 | .82 | .93 | |||
| Exp. (30) | 3.43±0.32 | 4.15±0.38 | 0.72±0.39 | ||||
| Con. (30) | 3.46±0.42 | 3.89±0.48 | 0.44±0.29 | ||||
| Interpersonal relationships | 3.07 | .002 | .78 | .91 | |||
| Exp. (30) | 3.37±0.57 | 3.77±0.66 | 0.40±0.68 | ||||
| Con. (30) | 3.49±0.46 | 3.46±0.57 | -0.03±0.37 | ||||
| Clinical performance | 268.50a) | .004 | .73 | .88 | |||
| Exp. (30) | 3.65±0.52 | 4.07±0.58 | 0.42±0.58 | ||||
| Con. (30) | 3.85±0.61 | 3.94±0.59 | 0.09±0.26 | ||||
| Problem solving abilities | 2.20 | .017 | .57 | .71 | |||
| Exp. (30) | 3.75±0.72 | 4.16±0.50 | 0.41±0.76 | ||||
| Con. (30) | 3.85±0.63 | 3.92±0.69 | 0.07±0.36 | ||||
| Nursing professionalism | 0.50 | .311 | .13 | .13 | |||
| Exp. (30) | 3.75±0.57 | 3.90±0.53 | 0.15±0.56 | ||||
| Con. (30) | 3.73±0.51 | 3.82±0.47 | 0.09±0.33 |
PPT, PowerPoint presentations.
Values are presented as number (%) or mean±standard deviation (range). PDNLP-S, Practice-Driven Nursing Leadership Program for Students. a)By Fisher’s exact test. b)By Mann-Whitney U test.
Values are presented as number (%) or mean±standard deviation (range). PDNLP-S, Practice-Driven Nursing Leadership Program for Students; Exp, Experimental Group; Con, Control Group. a)By Mann-Whitney U test.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 ePub Link
ePub Link Cite
Cite

