Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 54(4); 2024 > Article
-
Research Paper
- Perceptual Factors Associated with Gestational Weight Gain: A Cross-Sectional Survey
-
Sehee Kim1
 , Sukhee Ahn2
, Sukhee Ahn2
-
Journal of Korean Academy of Nursing 2024;54(4):495-508.
DOI: https://doi.org/10.4040/jkan.24052
Published online: November 1, 2024
1Department of Nursing, Pai Chai University, Daejeon, Korea
2College of Nursing, Chungnam National University, Daejeon, Korea
- Address reprint requests to : Ahn, Sukhee College of Nursing, Chungnam National University, 266 Munhwa-ro, Jung-gu, Daejeon 35015, Korea Tel: +82-42-580-8324 Fax: +82-42-580-8309 E-mail: sukheeahn@cnu.ac.kr
© 2024 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License (http://creativecommons.org/licenses/by-nd/4.0) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- Recent years have seen an increase in the number of pregnant women whose weight gain during pregnancy exceeds the recommended range. This study was intended to determine the relationships among demographic attributes, key perceptual factors, and gestational weight gain (GWG).
-
Methods
- This cross-sectional study was conducted between April and July 2022. First-time pregnant women beyond 36 weeks of gestation who were recruited via social media completed an online survey. Data were analyzed using one-way ANOVA, chi-square test, and logistic regression, all performed using SPSS software.
-
Results
- Of the 369 participants, 63 (17.1%) exceeded the recommended GWG guidelines, while 148 (40.1%) fell within the recommended range, and the remaining 158 (42.8%) had inadequate GWG. Being overweight or obese before pregnancy significantly increased the risk of excessive GWG (p < .001). This risk was also significantly greater for women with low internal weight locus of control (OR = 0.58, 95% CI 0.41~0.82), high external weight locus of control (OR = 1.75, 95% CI 1.31~2.34), and negative body image (OR = 0.62, 95% CI 0.51~0.75).
-
Conclusion
- The growing trend of excessive GWG among pregnant women is influenced by a combination of prepregnancy body mass index (BMI) and perceptual factors, including weight locus of control and body image. These findings underscore the need to implement weight management intervention strategies before pregnancy, taking into consideration BMI, and to enhance positive body image and internal locus of control.
INTRODUCTION
METHODS
1) Questionnaire on perceptions related to weight
2) Weight and demographic measures
RESULTS
DISCUSSION
CONCLUSION
-
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
-
ACKNOWLEDGEMENTS
None.
-
FUNDING
This work was supported by the National Research Foundation of Korea (NRF No. 2020R1A2C201086511).
-
DATA SHARING STATEMENT
Please contact the corresponding author for data availability.
-
AUTHOR CONTRIBUTIONS
Conceptualization or/and Methodology: Kim S & Ahn S.
Data curation or/and Analysis: Kim S.
Funding acquisition: Ahn S.
Investigation: Kim S.
Project administration or/and Supervision: Kim S & Ahn S.
Resources or/and Software: Kim S.
Validation: Kim S. Visualization: Kim S.
Writing original draft or/and Review & Editing: Kim S & Ahn S.
Article Information
| Characteristics |
Gestational weight gain |
p-value | ||
|---|---|---|---|---|
|
Inadequate (n = 158) |
Normal (n = 148) |
Excessive (n = 63) |
||
| M ± SD or n (%) | ||||
| Age (yr)† | 33.1 ± 3.16 | 33.4 ± 3.51 | 33.6 ± 2.90 | .569 |
| Gestational age (wk)† | 37.3 ± 0.94 | 37.5 ± 1.01 | 37.4 ± 1.10 | .330 |
| Prepregnancy BMI (kg/m2)†† | ||||
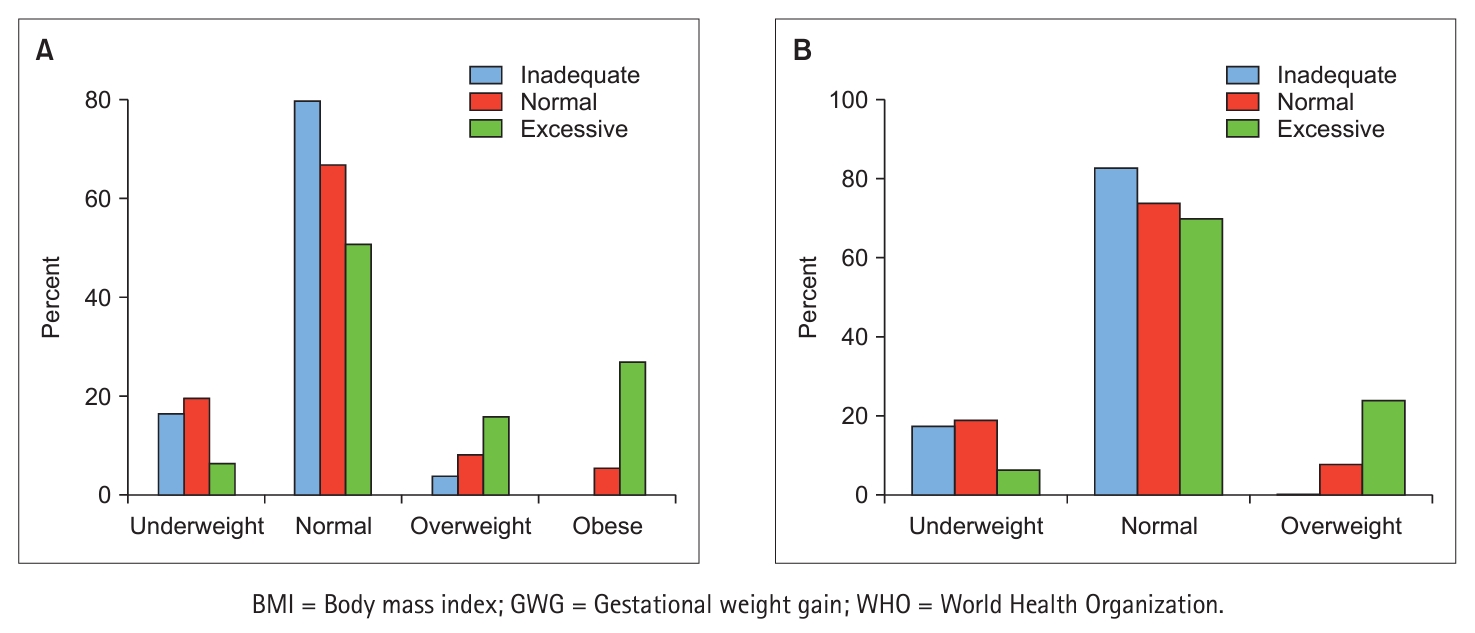
| < 18.5 | 26 (16.5) | 29 (19.6) | 4 (6.3) | < .001 |
| 18.5~22.9 | 126 (79.7) | 99 (66.9) | 32 (50.8) | |
| 23.0~24.9 | 6 (3.8) | 12 (8.1) | 10 (15.9) | |
| ≥ 25.0 | 0 (0.0) | 8 (5.4) | 17 (27.0) | |
| Education†† | ||||
| Secondary | 9 (5.7) | 8 (5.4) | 8 (12.7) | .085 |
| College | 120 (75.9) | 124 (83.8) | 48 (76.2) | |
| Graduate | 29 (18.4) | 16 (10.8) | 7 (11.1) | |
| Income (10,000 KRW/mo)†† | ||||
| < 200 | 7 (4.4) | 8 (5.4) | 2 (3.2) | .748 |
| 200~399 | 55 (34.8) | 56 (37.8) | 27 (42.8) | |
| 400~599 | 56 (35.5) | 56 (37.8) | 19 (30.2) | |
| ≥ 600 | 40 (25.3) | 28 (19.0) | 15 (23.8) | |
| Occupation†† | ||||
| Yes | 43 (27.2) | 35 (23.6) | 17 (27.0) | .752 |
| No | 115 (72.8) | 113 (76.4) | 46 (73.0) | |
| Drinking†† | ||||
| Yes | 1 (0.6) | 1 (0.7) | 0 (0.0) | .812 |
| No | 157 (99.4) | 147 (99.3) | 63 (100.0) | |
| Smoking†† | ||||
| Yes | 1 (0.6) | 0 (0.0) | 2 (3.2) | .060 |
| No | 157 (99.4) | 148 (100.0) | 61 (96.8) | |
| Variables | Crude B | SE | Exp. (B) | 95% CI | p-value | Adjusted B | SE | Exp. (B) | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 0.04 | 0.04 | 1.04 | 0.95~1.13 | .404 | |||||
| Pre-pregnancy BMI (kg/m2) | ||||||||||
| < 18.5 | 1† | 1† | ||||||||
| 18.5~22.9 | 0.67 | 0.55 | 1.96 | 0.66~5.76 | .224 | 0.94 | 0.76 | 2.55 | 0.58~11.30 | .217 |
| 23.0~24.9 | 2.03 | 0.65 | 7.64 | 2.13~27.36 | .002 | 3.48 | 0.97 | 32.60 | 4.84~219.51 | < .001 |
| ≥ 25.0 | 3.38 | 0.67 | 29.22 | 7.82~109.13 | < .001 | 4.64 | 0.97 | 103.25 | 15.53~686.41 | < .001 |
| Education | ||||||||||
| Secondary | 1† | |||||||||
| College | – 0.87 | 0.46 | 0.42 | 0.17~1.02 | .056 | |||||
| Graduate | – 1.11 | 0.59 | 0.33 | 0.10~1.05 | .061 | |||||
| Income (10,000 KRW/mo) | ||||||||||
| < 200 | 1† | |||||||||
| 200~399 | 0.60 | 0.78 | 1.82 | 0.39~8.46 | .442 | |||||
| 400~599 | 0.24 | 0.79 | 1.27 | 0.27~6.02 | .761 | |||||
| ≥ 600 | 0.50 | 0.81 | 1.65 | 0.34~8.01 | .532 | |||||
| Occupation | ||||||||||
| Yes | 1† | |||||||||
| No | – 0.08 | 0.31 | 0.93 | 0.50~1.71 | .805 | |||||
| Self-efficacy | ||||||||||
| Healthy eating | – 0.04 | 0.01 | 0.96 | 0.93~0.99 | .003 | 0.01 | 0.03 | 1.01 | 0.96~1.06 | .619 |
| Physical activity | – 0.05 | 0.02 | 0.95 | 0.92~0.98 | < .001 | – 0.05 | 0.03 | 0.95 | 0.91~1.00 | .051 |
| Perceived barrier | ||||||||||
| Healthy eating | – 0.01 | 0.02 | 0.99 | 0.96~1.04 | .768 | |||||
| Physical activity | 0.02 | 0.02 | 1.02 | 0.99~1.05 | .290 | |||||
| Weight locus of control | ||||||||||
| Internal | – 0.72 | 0.11 | 0.49 | 0.39~0.61 | < .001 | – 0.55 | 0.18 | 0.58 | 0.41~0.82 | .002 |
| External | 0.58 | 0.10 | 1.78 | 1.47~2.14 | < .001 | 0.56 | 0.15 | 1.75 | 1.31~2.34 | < .001 |
| Body image | – 0.51 | 0.07 | 0.60 | 0.52~0.69 | < .001 | – 0.48 | 0.10 | 0.62 | 0.51~0.75 | < .001 |
| Knowledge | ||||||||||
| Maternal risk of EGWG | 0.07 | 0.22 | 1.07 | 0.70~1.63 | .758 | |||||
| Fetal risk of EGWG | – 0.15 | 0.07 | 0.86 | 0.76~0.99 | .032 | 0.02 | 0.11 | 1.02 | 0.83~1.25 | .853 |
- 1. Champion ML, Harper LM. Gestational weight gain: Update on outcomes and interventions. Current Diabetes Reports. 2020;20(3):11. https://doi.org/10.1007/s11892-020-1296-1ArticlePubMed
- 2. Institute of Medicine and National Research Council. Weight gain during pregnancy: Reexamining the guidelines [Internet]. The National Academies Press; c2009 [cited 2022 Sep 1]. Available from: https://nap.nationalacademies.org/catalog/12584/weight-gain-during-pregnancy-reexamining-the-guidelines
- 3. Haam JH, Kim BT, Kim EM, Kwon H, Kang JH, Park JH, et al. Diagnosis of obesity: 2022 update of clinical practice guidelines for obesity by the Korean Society for the Study of Obesity. Journal of Obesity & Metabolic Syndrome. 2023;32(2):121-129. https://doi.org/10.7570/jomes23031ArticlePubMedPMC
- 4. Arora P, Tamber Aeri B. Gestational weight gain among healthy pregnant women from Asia in comparison with Institute of Medicine (IOM) guidelines-2009: A systematic review. Journal of Pregnancy. 2019;2019:3849596. https://doi.org/10.1155/2019/3849596ArticlePubMedPMC
- 5. Bhavadharini B, Anjana RM, Deepa M, Jayashree G, Nrutya S, Shobana M, et al. Gestational weight gain and pregnancy outcomes in relation to body mass index in Asian Indian women. Indian Journal of Endocrinology and Metabolism. 2017;21(4):588-593. https://doi.org/10.4103/ijem.IJEM_557_16ArticlePubMedPMC
- 6. Choi SK, Lee G, Kim YH, Park IY, Ko HS, Shin JC. Determining optimal gestational weight gain in the Korean population: A retrospective cohort study. Reproductive Biology and Endocrinology. 2017;15(1):67. https://doi.org/10.1186/s12958-017-0280-3ArticlePubMedPMC
- 7. Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA. 2017;317(21):2207-2225. https://doi.org/10.1001/jama.2017.3635ArticlePubMedPMC
- 8. Goldstein RF, Abell SK, Ranasinha S, Misso ML, Boyle JA, Harrison CL, et al. Gestational weight gain across continents and ethnicity: Systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Medicine. 2018;16(1):153. https://doi.org/10.1186/s12916-018-1128-1ArticlePubMedPMC
- 9. Obisity rate 2024 [Internet]. Statistics KOREA; c2024 [cited 2024 Feb 1]. Available from: https://www.index.go.kr/unify/idx-info.do?idxCd=8021
- 10. Garay SM, Sumption LA, Pearson RM, John RM. Risk factors for excessive gestational weight gain in a UK population: A biopsychosocial model approach. BMC Pregnancy and Childbirth. 2021;21(1):43. https://doi.org/10.1186/s12884-020-03519-1ArticlePubMedPMC
- 11. Lewandowska M, Więckowska B, Sajdak S. Pre-pregnancy obesity, excessive gestational weight gain, and the risk of pregnancy-induced hypertension and gestational diabetes mellitus. Journal of Clinical Medicine. 2020;9(6):1980. https://doi.org/10.3390/jcm9061980ArticlePubMedPMC
- 12. McDowell M, Cain MA, Brumley J. Excessive gestational weight gain. Journal of Midwifery & Women’s Health. 2019;64(1):46-54. https://doi.org/10.1111/jmwh.12927ArticlePubMed
- 13. Nehring I, Schmoll S, Beyerlein A, Hauner H, von Kries R. Gestational weight gain and long-term postpartum weight retention: A meta-analysis. The American Journal of Clinical Nutrition. 2011;94(5):1225-1231. https://doi.org/10.3945/ajcn.111.015289ArticlePubMed
- 14. Gilmore LA, Klempel-Donchenko M, Redman LM. Pregnancy as a window to future health: Excessive gestational weight gain and obesity. Seminars in Perinatology. 2015;39(4):296-303. https://doi.org/10.1053/j.semperi.2015.05.009ArticlePubMedPMC
- 15. Rastogi S, Rastogi D. The epidemiology and mechanisms of lifetime cardiopulmonary morbidities associated with pre-pregnancy obesity and excessive gestational weight gain. Frontiers in Cardiovascular Medicine. 2022;9:844905. https://doi.org/10.3389/fcvm.2022.844905ArticlePubMedPMC
- 16. Fealy S, Attia J, Leigh L, Oldmeadow C, Hazelton M, Foureur M, et al. Demographic and social-cognitive factors associated with gestational weight gain in an Australian pregnancy cohort. Eating Behaviors. 2020;39:101430. https://doi.org/10.1016/j.eatbeh.2020.101430ArticlePubMed
- 17. O’Brien EC, Alberdi G, McAuliffe FM. The influence of socioeconomic status on gestational weight gain: A systematic review. Journal of Public Health. 2018;40(1):41-55. https://doi.org/10.1093/pubmed/fdx038ArticlePubMed
- 18. Feng YY, Yu ZM, van Blyderveen S, Schmidt L, Sword W, Vanstone M, et al. Gestational weight gain outside the 2009 Institute of Medicine recommendations: Novel psychological and behavioural factors associated with inadequate or excess weight gain in a prospective cohort study. BMC Pregnancy and Childbirth. 2021;21(1):70. https://doi.org/10.1186/s12884-021-03555-5ArticlePubMedPMC
- 19. Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2(4):328-335. https://doi.org/10.1177/109019817400200403Article
- 20. Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179-211. https://doi.org/10.1016/0749-5978(91)90020-TArticle
- 21. Steinmetz H, Knappstein M, Ajzen I, Schmidt P, Kabst R. How effective are behavior change interventions based on the theory of planned behavior? Zeitschrift für Psychologie. 2016;224(3):216-233. https://doi.org/10.1027/2151-2604/a000255Article
- 22. Kapadia MZ, Gaston A, Van Blyderveen S, Schmidt L, Beyene J, McDonald H, et al. Psychological antecedents of excess gestational weight gain: A systematic review. BMC Pregnancy and Childbirth. 2015;15:107. https://doi.org/10.1186/s12884-015-0535-yArticlePubMedPMC
- 23. de Jersey SJ, Mallan K, Callaway L, Daniels LA, Nicholson JM. A cross sectional comparison of predisposing, reinforcing and enabling factors for lifestyle health behaviours and weight gain in healthy and overweight pregnant women. Maternal and Child Health Journal. 2017;21(3):626-635. https://doi.org/10.1007/s10995-016-2148-0ArticlePubMed
- 24. Halili L, Liu RH, Weeks A, Deonandan R, Adamo KB. High maternal self-efficacy is associated with meeting Institute of Medicine gestational weight gain recommendations. PloS One. 2019;14(12):e0226301. https://doi.org/10.1371/journal.pone.0226301ArticlePubMedPMC
- 25. Hill IF, Angrish K, Nutter S, Ramos-Salas X, Minhas H, Nagpal TS. Exploring body dissatisfaction in pregnancy and the association with gestational weight gain, obesity, and weight stigma. Midwifery. 2023;119:103627. https://doi.org/10.1016/j.midw.2023.103627ArticlePubMed
- 26. Khair H, Bataineh MF, Zaręba K, Alawar S, Maki S, Sallam GS, et al. Pregnant women’s perception and knowledge of the impact of obesity on prenatal outcomes-a cross-sectional study. Nutrients. 2023;15(11):2420. https://doi.org/10.3390/nu15112420ArticlePubMedPMC
- 27. Vignoles VL, Owe E, Becker M, Smith PB, Easterbrook MJ, Brown R, et al. Beyond the ‘east-west’ dichotomy: Global variation in cultural models of selfhood. Journal of Experimental Psychology: General. 2016;145(8):966-1000. https://doi.org/10.1037/xge0000175ArticlePubMed
- 28. Lin D, Huang X, Fan D, Chen G, Li P, Rao J, et al. Association of optimal gestational weight gain ranges with perinatal outcomes across body mass index categories in twin pregnancies. JAMA Network Open. 2022;5(7):e2222537. https://doi.org/10.1001/jamanetworkopen.2022.22537ArticlePubMedPMC
- 29. Durst JK, Sutton AL, Cliver SP, Tita AT, Biggio JR. Impact of gestational weight gain on perinatal outcomes in obese women. American Journal of Perinatology. 2016;33(9):849-855. https://doi.org/10.1055/s-0036-1579650ArticlePubMed
- 30. Weinerová J, Szűcs D, Ioannidis JPA. Published correlational effect sizes in social and developmental psychology. Royal Society Open Science. 2022;9(12):220311. https://doi.org/10.1098/rsos.220311ArticlePubMedPMC
- 31. Saltzer EB. The weight locus of control (WLOC) scale: A specific measure for obesity research. Journal of Personality Assessment. 1982;46(6):620-628. https://doi.org/10.1207/s15327752jpa4606_11ArticlePubMed
- 32. Ledoux T, Van Den Berg P, Leung P, Berens PD. Factors associated with knowledge of personal gestational weight gain recommendations. BMC Research Notes. 2015;8:349. https://doi.org/10.1186/s13104-015-1306-6ArticlePubMedPMC
- 33. Ben-Tovim DI, Walker MK. The development of the Ben-Tovim Walker Body Attitudes Questionnaire (BAQ), a new measure of women’s attitudes towards their own bodies. Psychological Medicine. 1991;21(3):775-784. https://doi.org/10.1017/s0033291700022406ArticlePubMed
- 34. Fuller-Tyszkiewicz M, Skouteris H, Watson B, Hill B. Body image during pregnancy: An evaluation of the suitability of the Body Attitudes Questionnaire. BMC Pregnancy and Childbirth. 2012;12:91. https://doi.org/10.1186/1471-2393-12-91ArticlePubMedPMC
- 35. Nowak M, Kalwa M, Oleksy P, Marszalek K, Radon-Pokracka M, Huras H. The relationship between pre-pregnancy BMI, gestational weight gain and neonatal birth weight: A retrospective cohort study. Ginekologia Polska. 2019;90(1):50-54. https://doi.org/10.5603/GP.2019.0008ArticlePubMed
- 36. Suliga E, Rokita W, Adamczyk-Gruszka O, Pazera G, Cieśla E, Głuszek S. Factors associated with gestational weight gain: A cross-sectional survey. BMC Pregnancy and Childbirth. 2018;18(1):465. https://doi.org/10.1186/s12884-018-2112-7ArticlePubMedPMC
- 37. Sun Y, Shen Z, Zhan Y, Wang Y, Ma S, Zhang S, et al. Effects of pre-pregnancy body mass index and gestational weight gain on maternal and infant complications. BMC Pregnancy and Childbirth. 2020;20(1):390. https://doi.org/10.1186/s12884-020-03071-yArticlePubMedPMC
- 38. Ashagi MM, Malikeh B. The relationship between locus of control (internal - external) and self-efficacy beliefs of Yazd University of Medical Sciences. International Journal of Engineering and Applied Sciences. 2015;2(8):72-76.
- 39. Au EW. Locus of control, self-efficacy, and the mediating effect of outcome control: Predicting course-level and global outcomes in an academic context. Anxiety, Stress, & Coping. 2015;28(4):425-444. https://doi.org/10.1080/10615806.2014.976761ArticlePubMed
- 40. Sagone E, de Caroli ME. Locus of control and academic self-efficacy in university students: The effects of self-concepts. Procedia - Social and Behavioral Sciences. 2014;114:222-228. https://doi.org/10.1016/j.sbspro.2013.12.689Article
- 41. Açıkgöz Çepni S, Kitiş Y. Relationship between healthy lifestyle behaviors and health locus of control and health-specific self-efficacy in university students. Japan Journal of Nursing Science. 2017;14(3):231-239. https://doi.org/10.1111/jjns.12154ArticlePubMed
- 42. Marr J, Wilcox S. Self-efficacy and social support mediate the relationship between internal health locus of control and health behaviors in college students. American Journal of Health Education. 2015;46(3):122-131. https://doi.org/10.1080/19325037.2015.1023477Article
- 43. Bouzas C, Bibiloni MDM, Tur JA. Relationship between body image and body weight control in overweight ≥55-year-old adults: A systematic review. International Journal of Environmental Research and Public Health. 2019;16(9):1622. https://doi.org/10.3390/ijerph16091622ArticlePubMedPMC
- 44. Harvey MW, Chasan-Taber L. Effect of body image on gestational weight gain: A systematic review. Current Epidemiology Reports. 2023;10(4):196-209. https://doi.org/10.1007/s40471-023-00334-yArticle
- 45. Ouyang Y, Wang K, Zhang T, Peng L, Song G, Luo J. The influence of sports participation on body image, self-efficacy, and self-esteem in college students. Frontiers in Psychology. 2020;10:3039. https://doi.org/10.3389/fpsyg.2019.03039ArticlePubMedPMC
- 46. Alleva JM, Sheeran P, Webb TL, Martijn C, Miles E. A meta-analytic review of stand-alone interventions to improve body image. PloS One. 2015;10(9):e0139177. https://doi.org/10.1371/journal.pone.0139177ArticlePubMedPMC
- 47. Ardahan M, Temel AB. Body image perception and the effectiveness of a body image education in pregnant housewives. Journal of Nursing and Care. 2014;3(3):1000163. https://doi.org/10.4172/2167-1168.1000163Article
- 48. Papini NM, Mason TB, Herrmann SD, Lopez NV. Self-compassion and body image in pregnancy and postpartum: A randomized pilot trial of a brief self-compassion meditation intervention. Body Image. 2022;43:264-274. https://doi.org/10.1016/j.bodyim.2022.09.010ArticlePubMed
- 49. McPhail A, Hare ME, Talcott GW, Little MA, Bursac Z, Krukowski RA. Gestational weight gain during the COVID-19 Pandemic. Maternal and Child Health Journal. 2023;27(9):1454-1459. https://doi.org/10.1007/s10995-023-03730-4ArticlePubMedPMC
- 50. Lange RV, Tiggemann M. Dimensionality and reliability of the Rotter I-E locus of control scale. Journal of Personality Assessment. 1981;45(4):398-406. https://doi.org/10.1207/s15327752jpa4504_9ArticlePubMed
References
Figure & Data
REFERENCES
Citations

- Factors Associated With Gestational Weight Gain Among Nurses in Korea
Sook Jung Kang, Woon Young Hwang, Hyunju Dan, Sue Kim, Kwang-Pil Ko
Journal of Obstetric, Gynecologic, & Neonatal Nursing.2025; 54(5): 543. CrossRef - Attitudes toward body weight and shape during pregnancy among Japanese women who were underweight before pregnancy: A qualitative study
Chisato KOROGI, Mie SHIRAISHI, Kaori MATSUDA, Natsuki HORI, Hanna HORIGUCHI
Journal of Japan Academy of Midwifery.2025; 39(3): 456. CrossRef
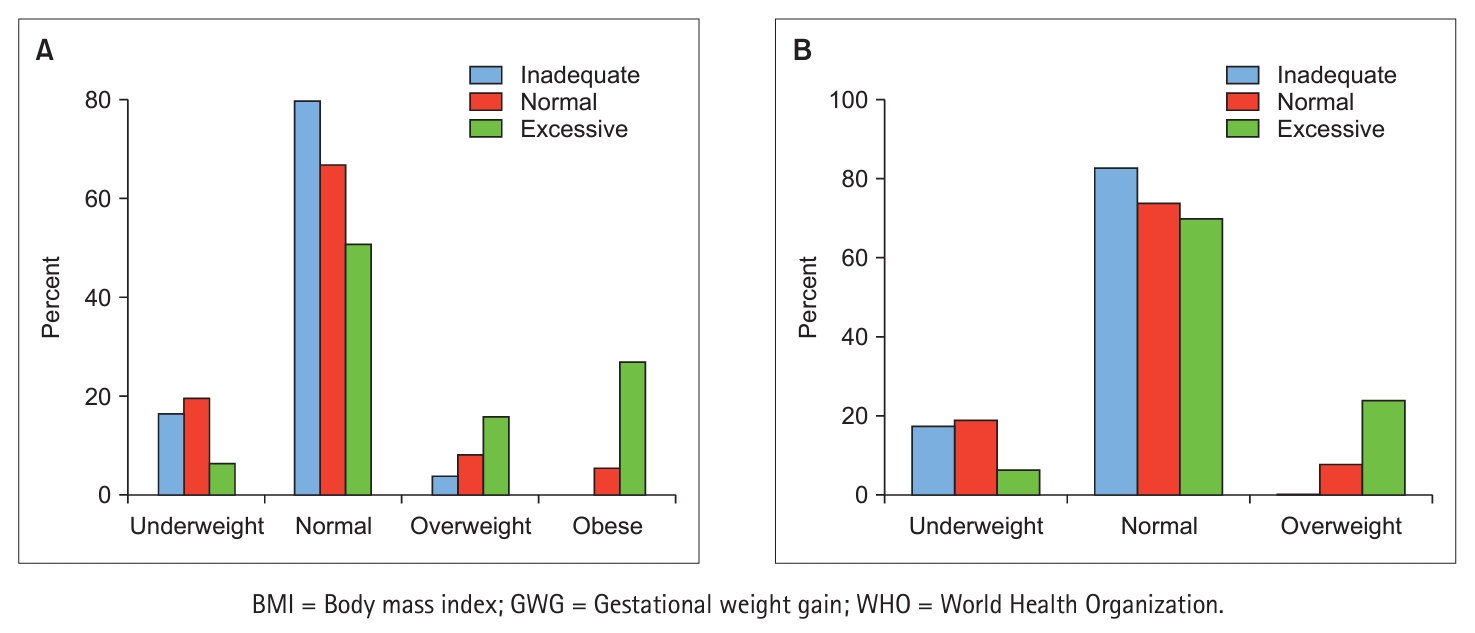
Fig. 1.
| Variables | Categories | M ± SD | n (%) |
|---|---|---|---|
| Age (yr) | 33.3 ± 3.26 | ||
| 25~34 | 239 (64.8) | ||
| 35~44 | 130 (35.2) | ||
| Gestational age (wk) | 36~41 | 37.4 ± 1.00 | |
| Education | Secondary | 25 (6.8) | |
| College | 292 (79.1) | ||
| Graduate | 52 (14.1) | ||
| Occupation | Full time | 74 (20.1) | |
| Part time (h) | 10 (2.7) | ||
| Self-employed | 11 (3.0) | ||
| Quitting work due to pregnancy | 74 (20.1) | ||
| Maternity leave | 137 (37.1) | ||
| Housewife (include students) | 63 (17.0) | ||
| Household income (10,000 KRW/mo) | < 200 | 17 (4.6) | |
| 200~399 | 138 (37.4) | ||
| 400~599 | 131 (35.5) | ||
| ≥ 600 | 83 (22.5) | ||
| Smoking | Yes | 3 (0.8) | |
| No | 366 (99.2) | ||
| Drinking | Yes | 2 (0.5) | |
| No | 367 (99.5) | ||
| Body weight (kg) | Prepregnancy | 55.04 ± 7.07 | |
| Current | 66.94 ± 7.91 | ||
| Prepregnancy BMI (kg/m2) | < 18.5 | 59 (16.0) | |
| 18.5~22.9 | 257 (69.6) | ||
| 23.0~24.9 | 28 (7.6) | ||
| ≥ 25.0 | 25 (6.8) | ||
| Gestational weight gain (kg) | Total | 11.90 ± 4.08 | 369 (100.0) |
| Inadequate | 8.80 ± 1.97 | 158 (42.8) | |
| Normal | 13.22 ± 2.09 | 148 (40.1) | |
| Excessive | 17.63 ± 3.86 | 63 (17.1) |
| Characteristics | Gestational weight gain |
p-value | ||
|---|---|---|---|---|
| Inadequate (n = 158) |
Normal (n = 148) |
Excessive (n = 63) |
||
| M ± SD or n (%) | ||||
| Age (yr) |
33.1 ± 3.16 | 33.4 ± 3.51 | 33.6 ± 2.90 | .569 |
| Gestational age (wk) |
37.3 ± 0.94 | 37.5 ± 1.01 | 37.4 ± 1.10 | .330 |
| Prepregnancy BMI (kg/m2) |
||||
| < 18.5 | 26 (16.5) | 29 (19.6) | 4 (6.3) | < .001 |
| 18.5~22.9 | 126 (79.7) | 99 (66.9) | 32 (50.8) | |
| 23.0~24.9 | 6 (3.8) | 12 (8.1) | 10 (15.9) | |
| ≥ 25.0 | 0 (0.0) | 8 (5.4) | 17 (27.0) | |
| Education |
||||
| Secondary | 9 (5.7) | 8 (5.4) | 8 (12.7) | .085 |
| College | 120 (75.9) | 124 (83.8) | 48 (76.2) | |
| Graduate | 29 (18.4) | 16 (10.8) | 7 (11.1) | |
| Income (10,000 KRW/mo) |
||||
| < 200 | 7 (4.4) | 8 (5.4) | 2 (3.2) | .748 |
| 200~399 | 55 (34.8) | 56 (37.8) | 27 (42.8) | |
| 400~599 | 56 (35.5) | 56 (37.8) | 19 (30.2) | |
| ≥ 600 | 40 (25.3) | 28 (19.0) | 15 (23.8) | |
| Occupation |
||||
| Yes | 43 (27.2) | 35 (23.6) | 17 (27.0) | .752 |
| No | 115 (72.8) | 113 (76.4) | 46 (73.0) | |
| Drinking |
||||
| Yes | 1 (0.6) | 1 (0.7) | 0 (0.0) | .812 |
| No | 157 (99.4) | 147 (99.3) | 63 (100.0) | |
| Smoking |
||||
| Yes | 1 (0.6) | 0 (0.0) | 2 (3.2) | .060 |
| No | 157 (99.4) | 148 (100.0) | 61 (96.8) | |
| Variables | Crude B | SE | Exp. (B) | 95% CI | p-value | Adjusted B | SE | Exp. (B) | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 0.04 | 0.04 | 1.04 | 0.95~1.13 | .404 | |||||
| Pre-pregnancy BMI (kg/m2) | ||||||||||
| < 18.5 | 1 |
1 |
||||||||
| 18.5~22.9 | 0.67 | 0.55 | 1.96 | 0.66~5.76 | .224 | 0.94 | 0.76 | 2.55 | 0.58~11.30 | .217 |
| 23.0~24.9 | 2.03 | 0.65 | 7.64 | 2.13~27.36 | .002 | 3.48 | 0.97 | 32.60 | 4.84~219.51 | < .001 |
| ≥ 25.0 | 3.38 | 0.67 | 29.22 | 7.82~109.13 | < .001 | 4.64 | 0.97 | 103.25 | 15.53~686.41 | < .001 |
| Education | ||||||||||
| Secondary | 1 |
|||||||||
| College | – 0.87 | 0.46 | 0.42 | 0.17~1.02 | .056 | |||||
| Graduate | – 1.11 | 0.59 | 0.33 | 0.10~1.05 | .061 | |||||
| Income (10,000 KRW/mo) | ||||||||||
| < 200 | 1 |
|||||||||
| 200~399 | 0.60 | 0.78 | 1.82 | 0.39~8.46 | .442 | |||||
| 400~599 | 0.24 | 0.79 | 1.27 | 0.27~6.02 | .761 | |||||
| ≥ 600 | 0.50 | 0.81 | 1.65 | 0.34~8.01 | .532 | |||||
| Occupation | ||||||||||
| Yes | 1 |
|||||||||
| No | – 0.08 | 0.31 | 0.93 | 0.50~1.71 | .805 | |||||
| Self-efficacy | ||||||||||
| Healthy eating | – 0.04 | 0.01 | 0.96 | 0.93~0.99 | .003 | 0.01 | 0.03 | 1.01 | 0.96~1.06 | .619 |
| Physical activity | – 0.05 | 0.02 | 0.95 | 0.92~0.98 | < .001 | – 0.05 | 0.03 | 0.95 | 0.91~1.00 | .051 |
| Perceived barrier | ||||||||||
| Healthy eating | – 0.01 | 0.02 | 0.99 | 0.96~1.04 | .768 | |||||
| Physical activity | 0.02 | 0.02 | 1.02 | 0.99~1.05 | .290 | |||||
| Weight locus of control | ||||||||||
| Internal | – 0.72 | 0.11 | 0.49 | 0.39~0.61 | < .001 | – 0.55 | 0.18 | 0.58 | 0.41~0.82 | .002 |
| External | 0.58 | 0.10 | 1.78 | 1.47~2.14 | < .001 | 0.56 | 0.15 | 1.75 | 1.31~2.34 | < .001 |
| Body image | – 0.51 | 0.07 | 0.60 | 0.52~0.69 | < .001 | – 0.48 | 0.10 | 0.62 | 0.51~0.75 | < .001 |
| Knowledge | ||||||||||
| Maternal risk of EGWG | 0.07 | 0.22 | 1.07 | 0.70~1.63 | .758 | |||||
| Fetal risk of EGWG | – 0.15 | 0.07 | 0.86 | 0.76~0.99 | .032 | 0.02 | 0.11 | 1.02 | 0.83~1.25 | .853 |
BMI = Body mass index; KRW = Korean won; M = Mean; SD = Standard deviation.
BMI = Body mass index; KRW = Korean won; M = Mean; SD = Standard deviation. One-way ANOVA. Chi-square test.
BMI = Body mass index; CI = Confidence interval; EGWG = Excessive gestational weight gain; Exp. = Exponential; KRW = Korean won; SE = Standard error. Reference.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 ePub Link
ePub Link Cite
Cite

