Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 52(1); 2022 > Article
- Research Paper Incidence and Predictors of Cataract among People with Type 2 Diabetes Mellitus: Using Secondary Data Analysis from the Ansan Cohort of the Korean Genome and Epidemiology Study
- Ihn Sook Jeong, Eun Joo Lee, Myo Sung Kim, Jung Ok Yu, Hae Sun Yun, Jeong Hee Jeong, Youn Sun 6 Hwang
-
Journal of Korean Academy of Nursing 2022;52(1):24-35.
DOI: https://doi.org/10.4040/jkan.21081
Published online: February 28, 2022
2Department of Nursing, Dong-Eui University, Busan
3College of Nursing, Dong-A University, Busan
4Department of Nursing Science, Kyungsung University, Busan
5Department of Nursing, Daedong College, Busan
6Department of Nursing, Dongseo University, Busan, Korea
Abstract
Purpose
This study investigated the incidence and risk factors of cataract in people with diabetes mellitus (DM) using data from Ansan cohort of the Korean Genome and Epidemiology Study (KoGES).
Methods
Data from a total of 329 patients with type 2 DM without cataract who participated in Ansan cohort of the KoGES from baseline survey (2001–2002) to fifth follow-up visit (2011–2012) were examined.
The characteristics of the subjects were analyzed with frequency and percentage, and mean and standard deviation. Cataract incidence was measured as incidence proportion (%). For risk factors of cataract, hazard ratio (HR) and 95% confidence interval (CI) were obtained using the Cox proportional hazard model.
Results
The cataract incidence over a 10-year follow-up period was 19.1% (15.1 in males and 25.8 in females), and mean age at the incidence of cataract was 63.48 years (61.58 years in males and 65.31 years in females). Age (HR=1.09, 95% CI=1.05–1.13) and HbA1c (HR=1.21, 95% CI=1.07–1.37) or the duration of DM (HR=1.05, 95% CI=1.00–1.09) were found to be independently associated with cataract development.
Conclusion
Cataract development in people with DM is common, and its likelihood increases with age, HbA1c, and the duration of DM. Considering negative effect of cataract on their quality of life and economic burden, nurses should identify people with DM at a higher risk of cataract development, and plan individual eye examination programs to detect cataract development as early as possible.
Published online Feb 09, 2022.
https://doi.org/10.4040/jkan.21081
Incidence and Predictors of Cataract among People with Type 2 Diabetes Mellitus: Using Secondary Data Analysis from the Ansan Cohort of the Korean Genome and Epidemiology Study
Abstract
Purpose
This study investigated the incidence and risk factors of cataract in people with diabetes mellitus (DM) using data from Ansan cohort of the Korean Genome and Epidemiology Study (KoGES).
Methods
Data from a total of 329 patients with type 2 DM without cataract who participated in Ansan cohort of the KoGES from baseline survey (2001–2002) to fifth follow-up visit (2011–2012) were examined. The characteristics of the subjects were analyzed with frequency and percentage, and mean and standard deviation. Cataract incidence was measured as incidence proportion (%). For risk factors of cataract, hazard ratio (HR) and 95% confidence interval (CI) were obtained using the Cox proportional hazard model.
Results
The cataract incidence over a 10-year follow-up period was 19.1% (15.1 in males and 25.8 in females), and mean age at the incidence of cataract was 63.48 years (61.58 years in males and 65.31 years in females). Age (HR=1.09, 95% CI=1.05–1.13) and HbA1c (HR=1.21, 95% CI=1.07–1.37) or the duration of DM (HR=1.05, 95% CI=1.00–1.09) were found to be independently associated with cataract development.
Conclusion
Cataract development in people with DM is common, and its likelihood increases with age, HbA1c, and the duration of DM. Considering negative effect of cataract on their quality of life and economic burden, nurses should identify people with DM at a higher risk of cataract development, and plan individual eye examination programs to detect cataract development as early as possible.
INTRODUCTION
With changing lifestyles and aging populations, the prevalence of diabetes mellitus (DM) is increasing worldwide. Globally, the overall DM population in 2014 was approximately 422 million, corresponding to 8.5% of all adults aged 18 years or older [1]. This ratio is predicted to reach 10.9% by 2,045 [2]. In South Korea, the prevalence of DM in adults aged 30 years or older increased from 11.8% in 2012 to 13.8% in 2018 [3]. Long-term hyperglycemia due to DM can lead to various complications, and cataract is a diabetic complication of the eye. According to the pathogenesis of diabetic cataract, hyperglycemia induces changes in lens metabolism, which is initiated by the polyol pathway, resulting in osmotic stress, generation of free radicals, and damage to lens fibers [4].
The cataract incidence was 20.4 per 1,000 person-year (95% confidence interval [CI] = 19.8~20.9) for people with DM aged 40 years or older, and who participated in the 2000~2015 UK-based Clinical Practice Research Datalink (CPRD). This number was almost double the cataract incidence of people without DM; that is, 10.8 per 1,000 person-year (95% CI = 10.5~11.2) [5]. Similarly, in a meta-analysis, people with DM were found to have a cataract incidence twice as high as those without DM [6]. As the incidence of cataracts varies according to the World Health Organization regions [7]—even among Asian ethnicities [8]—it is necessary to identify the incidence of, and factors related to, cataract in Korean people with DM. Notably, among people with DM in Korea, only 32.2% had annual eye examinations [9], less than those in the United States, at 63.4% [10]; Norway, 61.0% [11]; and France, 47.9% [12]. One reason people with DM do not undergo an annual eye examination is that it is unnecessary at a younger age, for instance, below age 70 [13]; therefore, knowledge of the age of onset of cataracts in people with DM can promote eye examinations among those at risk.
In 2020, cataract was the leading global cause of blindness in those aged 50 years and older (15.2 million cases) [14]; it affects not only an individual’s quality of life, but also their direct and indirect costs to increase quality-adjusted life years [15]. Therefore, there is a strong nursing implication for postponing or preventing cataract development in people with DM, through better risk factor management. A study conducted in India showed that the risk of developing cataracts in people with type 2 DM was 1.7 times higher for females. Compared with those in their 40s, the risk was 2.7~3.3 times and 3.3~3.9 times higher for those in their 50s and 60s, respectively [16]. The UK-based CPRD reported that DM lasting 10 years or more increased the risk of cataract 5.14 times. Moreover, higher HbA1c levels, insulin use, past smoking, and comorbidities such as dyslipidemia, hypertension, and heart diseases were found to be potential risk factors for cataract development [5].
However, a recent systematic review conducted on 13 different populations in the United States, Europe, India, and Taiwan found that risk factors for cataract development were not consistent across the studies except for age and glycemic control [17]. Dyslipidemia and smoking were considered potentially contributing variables, as their role was not well established because of insufficient published evidence and inconsistency in the study results. Moreover, few studies have assessed the association between cataract development and obesity (body mass index [BMI]) or comorbidities such as heart diseases in people with DM [17]. Therefore, to identify significant risk factors for cataract development in populations with DM, a well-conducted, long-term study is necessary. It is important to assess all the potential risk factors in various aspects, including not only demographic characteristics but also modifiable factors, to provide accurate and specific information to people with DM, properly screen those at high risk of developing cataracts, monitor the change in risk regularly, and provide interventions to prevent or delay cataract development.
The Korean Genome and Epidemiology Study (KoGES) is a large prospective cohort study initiated by the Korean government (National Research Institute of Health, Korea Disease Control and Prevention Agency, and the Ministry of Health Welfare, Korea) [18]. The KoGES data have been used to investigate the genetic and environmental etiology of non-communicable chronic diseases such as type 2 DM, hypertension, cardiovascular diseases, metabolic syndrome, cancer, and so on, with long-term follow-up [19]. Of all reported studies using the KoGES, only one was related to cataract, which did not target people with DM [20].
Therefore, this study examined the incidence of cataracts and its associated risk factors in people with DM living in the community, using the community-based cohort study of the KoGES. The objectives were to 1) investigate cataract incidence-related characteristics, 2) compare the baseline characteristics of study subjects with or without cataract development, and 3) identify the factors related to cataract development.
METHODS
1. Study design
This study was a secondary analysis of the data from the Ansan cohort of the KoGES, which was a community-based cohort study conducted by the Korea Disease Control and Prevention Agency.
For this study, the application documents for data sharing were submitted through online data sharing service of the division of epidemiology and health index, the National Institute of Health, the Korea Disease Control and Prevention Agency. The epidemiologic data of the Ansan cohort of the KoGES from baseline survey (2001~2002) to fifth follow-up visit (2011~2012) were downloaded after approval notification.
2. Study participants
The Ansan cohort represented small/medium-sized cities in Korea and comprised 5,012 adult males and females aged between 40 and 69 years. The baseline survey of the Ansan cohort was completed in 2001 and 2002, and follow-up surveys are conducted every other year. Details of the KoGES and Ansan cohort have been described previously [18, 21, 22, 23]. In brief, this study used a two-stage cluster sampling for subject enrollment at the Ansan site, based on the local telephone directory information and information on demographic characteristics from the 2000 census. Altogether, 10,957 eligible individuals were identified by telephone contact; 5,012 subjects participated in the baseline survey, and 3,052 subjects remained until the fifth follow-up survey (60.9% follow-up rate). The mean age ± standard deviation (SD) was 49.1 ± 7.9 for the 5,012 subjects at baseline and 58.3 ± 7.3 for the 3,052 subjects at the fifth visit. All subjects were surveyed for demographic and medical history, family history of disease, and lifestyle habits (including smoking, alcohol use, physical activity, and dietary intake) using an interview-based questionnaire and they underwent comprehensive health check-ups and provided bio-specimens for assays.
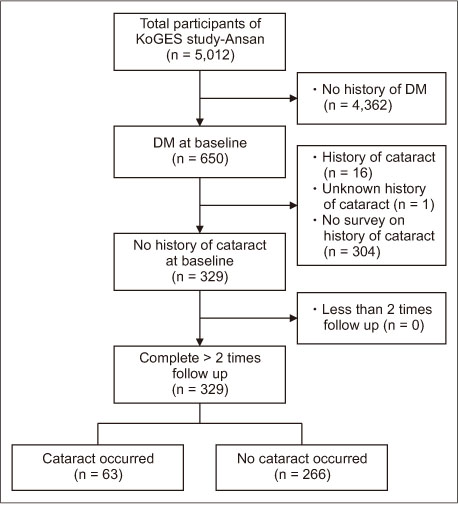
Subjects were included in this study upon meeting the following criteria: people with type 2 DM, without cataract at the baseline survey, and completed at least one follow-up survey. The sample size was calculated using the cohort study design of the Open Source Epidemiologic Statistics for Public Health [24], an online sample counting program. Based on the results of the duration of DM (< 10 years versus ≥ 10 years) in Becker et al. [5], a significance level (α) of .05, power (1 - β) = .85, percentage of unexposed with outcome= 20.5%, and percentage of exposed with outcome = 42.0% result in a minimum required sample size of 256 (Kelsey method) to 311 (Fleiss with correction method). Among 5,012 people who participated in the baseline survey, 329 who met the inclusion criteria were included in the analysis. Eventually, cataract occurred in 63 (19.1%) patients during the 10-year follow-up period (Figure 1).
Figure 1
Flow of participants through the study.
DM = Diabetes mellitus; KoGES = Korean Genome and Epidemiology Study.
3. Definition and variables
Following previous studies [21, 22, 23], DM subjects were defined as those who met at least one of the following four criteria: 1) self-reporting of DM, 2) undergoing insulin or oral hypoglycemic agent treatment, 3) with fasting plasma glucose (FPG) ≥ 126 mg/dL or postprandial 2-hour glucose (PP2) ≥ 200 mg/dL after a 75-g oral glucose tolerance test (OGTT), and 4) with HbA1c ≥ 6.5%.
Cataract subjects were classified according to their response to the questions in medical information section about the experience and timing of cataract diagnosis after DM diagnosis during the third to fifth follow-up surveys. The question was, “Have you been diagnosed with cataract in relation to DM after DM diagnosis?” Those who responded “No, I have never been diagnosed” to the question were classified as having “no cataract” while the rest were classified as having “cataract”. The timing of cataract diagnosis was coded as “before 2001”, “2001~2002”, “2003~2004”, “2005~2006”, “2007~2008”, “2009~2010”, and “2011~2012”. Meanwhile, if they responded “before 2001” or “2001~2002” to the question, did not respond to the question, or did not participate in the follow-up survey, they were classified as “having history of cataract at baseline”, “unknown cataract” or “no survey”, respectively, and all were excluded from the study.
The explanatory variables, selected based on previous studies on cataract-related factors [5, 16, 17, 25, 26, 27], were socio-demographics, health behaviors, and disease-related characteristics of the subjects measured at the baseline survey. For all characteristic variables, KoGES data were used as it was or re-categorized. They included sex, age, education, family income, smoking status, total smoking amount (pack-year), status of alcohol use, total alcohol intake (g/day), total physical activity, BMI, age at the initial diagnosis of DM, use of oral hypoglycemic agents, insulin treatment, FPG, PP2, HbA1c, fasting plasma insulin, comorbidities (hypertension, hyperlipidemia, asthma, ischemic heart disease, congestive heart failure, myocardial infarction, chronic obstructive pulmonary disease), systolic blood pressure, diastolic blood pressure, taking of lipid-lowering agents, steroid use, and lipids (total cholesterol, low-density lipoprotein cholesterol [LDLC], high-density lipoprotein cholesterol [HDLC], and triglycerides). Some of these variables were converted and used according to the purpose of this study. Regarding education, the subjects were divided into two categories: high school graduate or not. Family income per month was divided into two categories: below or above three million KRW which was the closest to the average family income in 2003 [28]. For smoking status and status of alcohol use, the subjects were divided into two categories: current smoking or not and current alcohol use or not, respectively. Physical activity was measured using the metabolic equivalent of task. BMI was calculated using height and weight which were measured using standard methods (weight divided by height squared, kg/m2). The duration of DM was calculated by subtracting participants’ age at the initial diagnosis of DM from their age at the baseline survey, and those who met only the laboratory criterion of DM were classified into the “not applicable” group. FPG, fasting plasma insulin, and triglycerides were measured in the central laboratory by collecting blood after fasting for 12 hours. PP2 was checked by measuring plasma glucose at 2 hours by a 75 g OGTT. LDLC was calculated using three lipid data: LDLC = total cholesterol–[(triglyceride/5) + HDLC] [29]. Insulin resistance was calculated using the homeostasis model assessment of insulin resistance (HOMA-IR). The equation for HOMA-IR was “HOMA-IR = [fasting insulin (µIU) × fasting blood sugar (mg/dL)] / 405” [22, 30, 31]. Hypertension was defined as subjects who had left or right systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, or subjects who were taking anti-hypertensive agents [30, 32]. Meanwhile, steroid use and comorbidities except hypertension and hyperlipidemia were finally excluded from the explanatory variables because there was no or small subjects (1~6 cases) who took steroid or had those comorbidities.
4. Data analysis
Data were analyzed using IBM SPSS Statistics for Windows (version 23.0; IBM Corp., Armonk, NY, USA) and Open Source Epidemiologic Statistics for Public Health [24], and the significance level of the two-tailed statistical test was .05. The 10-year incidence of cataract was calculated as the incidence proportion (%) and incidence rate per 1,000 person-years with their respective 95% CIs. Person-years were calculated from the age at the baseline survey until the age at cataract development or the last survey.
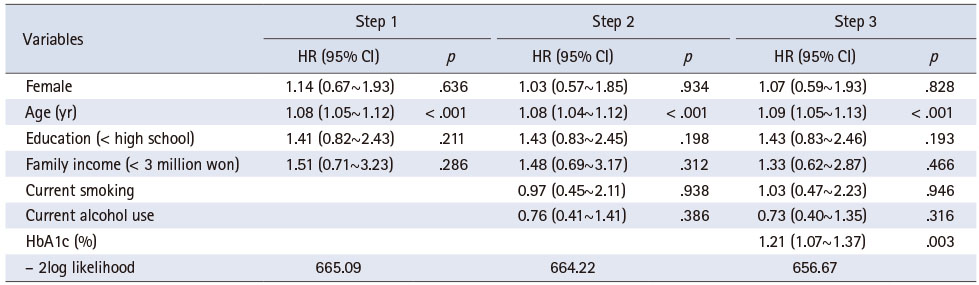
Hazard ratios (HRs) and 95% CIs were calculated using a simple Cox proportional hazards model to compare the survival patterns according to the study subjects’ baseline characteristics. A log minus log plot was used to confirm whether each variable met the proportional hazard assumption [33]. The survival time was defined as the period from the baseline survey to cataract occurrence, and calculated in units of year by subtracting the age at the time of the baseline survey from the age at the time of cataract occurrence. A multivariate Cox proportional hazards model was used to identify the factors related to cataract development with significant variables from the simple model as explanatory variables, except for the duration of DM. For the duration of DM, some data (163 in total) corresponding to the “not applicable” group were missing. Thus, demographic variables (sex, age, education, and family income), health behaviors (current smoking and current alcohol use), and disease-related variables (HbA1c) were entered into the model in a series of steps, the HRs and their 95% CIs and -2log likelihood values were calculated. The analysis results, including the duration of DM in the Cox model, are presented as a supplement. The correlation coefficient (Spearman’s rho) among the variables ranged from .02 to .48, which satisfied the assumption of multicollinearity.
Meanwhile, about half of the subjects with DM at baseline were excluded for “unknown cataract” or “no survey” on cataract history; a sensitivity analysis was performed to check the robustness of the findings. Specifically, we compared the baseline characteristics of those who were included (n = 329) and excluded (n = 305) in this study using the χ2 test, Fisher’s exact test, t-test, or Mann–Whitney U test.
5. Ethical consideration
This study was conducted after receiving approval for exempt review (PNU IRB No. 2018_24_HR) from the Institutional Review Board (IRB) of Pusan National University. Our data were received from the department in charge of KoGES in the KDCA after submission of the IRB approval letter and study proposal to the Department, and all data were anonymized.
RESULTS
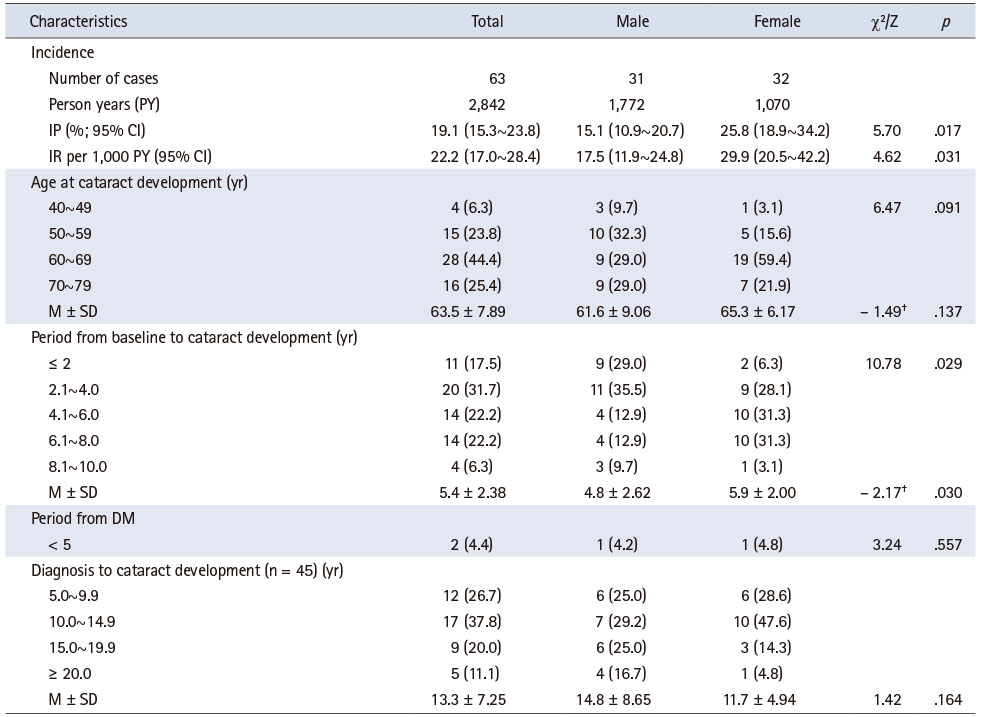
1. Cataract incidence
Among the 329 subjects, 63 developed cataracts, with an incidence proportion of 19.1% (Table 1). The incidence rate per 1,000 person-years was 22.2 (95% CI = 17.0~28.4), 17.5 (95% CI = 11.9~24.8) among males and 29.9 (95% CI = 20.5~42.2) among females. The mean age at the incidence of cataract was 63.5 years. The mean elapsed time from the baseline survey until cataract development was 5.4 years. For females, the elapsed time before contracting cataract (5.9 years) was significantly longer than for males (4.8 years; Z = -2.17, p = .030). Meanwhile, the mean elapsed time from DM diagnosis to cataract development was 13.3 years, and there was no difference by sex.
Table 1
Cataract Incidence-Related Characteristics of Study Subjects (N = 63)
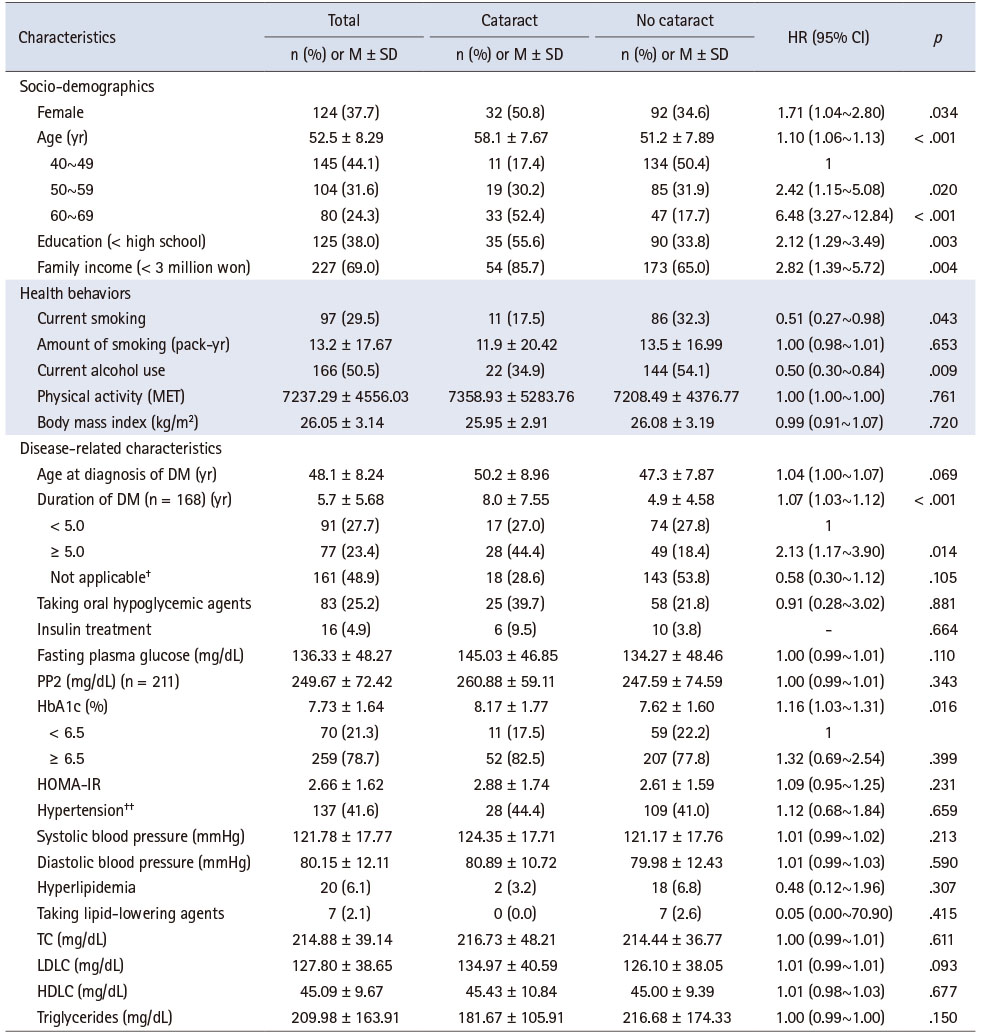
2. Cataract incidence according to the subjects’ characteristics at the baseline data
Table 2 shows that subjects with and without cataract were significantly different in their characteristics at baseline: females (p = .034), mean age (p < .001), education (p = .003), family income (p = .004), current smoking (p = .043), current alcohol use (p = .009), duration of DM (p < .001), and HbA1c (p = .016). In the cataract group at baseline, there were more females; more current smoking and fewer current alcohol use; the group members were older, less educated, and had less family income, longer duration of DM, and higher HbA1c than the no-cataract group members.
Table 2
Comparison of Baseline Characteristics of Study Subjects with or without Cataract Development (N = 329)
3. Factors related to cataract incidence
Among the seven variables, except for the duration of DM, which were significant in the simple model, age (HR = 1.09, 95% CI = 1.05~1.13) and HbA1c (HR = 1.21, 95% CI = 1.07~1.37) were independently associated with the development of cataracts in multiple models (Table 3). Meanwhile, in the additional analysis that included the duration of DM in the multiple model, age (HR = 1.08, 95% CI = 1.03~1.13) and the duration of DM (HR = 1.05, 95% CI = 1.00~1.09) were significantly related to the development of cataracts (Supplementary Table 1).
Table 3
Factors Related to the Cataract Development (N = 329)
4. Characteristics of the subjects included and excluded in the study
According to the sensitivity analysis, the characteristics of the subjects included in the study and those excluded were significantly different for several variables. The group included in the study had fewer females (p = .036), and compared with the excluded group, its members were less educated (p = .005), had hypertension (p = .010), lower HDLC (p = .013) but higher BMI (p = .025), FPG (p < .001), PP2 (p < .001), HbA1c (p < .001), and HOMA-IR (p = .007; Supplementary Table 2).
DISCUSSION
This study used the KoGES, a community-based cohort databases, to analyze aspects of cataract incidence in people with DM over a period of 10 years, and examine related factors. The 10-year-incidence proportion of cataract was approximately 19.1%, indicating that cataract occurred in approximately two in every ten people with DM. The incidence of cataracts among people without DM has not been reported in Korea. Instead, the prevalence of cataract among the general population (with and without DM) was reported to be 11% in a questionnaire-based study of 715,554 people aged 40 years or older in the period 2008~2012 [34]. Considering that approximately 10% of the general population had DM [35] and about 19% of them had cataracts, the estimated incidence proportion of cataracts among people without DM is around 10%. This finding is similar to the figure reported in a meta-analysis, that is 1.97 times [6]. We found the cataract incidence rate in people with DM to be 22.2 cases per 1,000 person-years. This is slightly higher than 20.4 (95% CI = 19.8~20.9) identified for people with DM aged 40 years or older who participated in the 2000~2015 UK-based CPRD [5], and more than double the cataract incidence rate of people without DM; 10.8 (95% CI = 10.5~11.2) per 1,000 person-years. The cataract incidence rate was 1.7 times higher in females than in males in this study, which aligns with the result in a previous study [5], specifically, 1.5 times higher in females than in males.
In this study, cataract development in people with DM was found to be associated with increased age, HbA1c level, and duration of DM. Age, a well-known risk factor for cataract in people with DM, was found to be increase the risk of cataract 1.03~1.27 times per year [17]. In this study, cataract risk rapidly increased in patients who were in their 50s at baseline, with a 1.09 times increase in cataract risk per year. This can be translated to an increase in risk by a factor of about 2.4 between the ages of 40s and 50s, and a factor of 5.6 between the ages of 40s and 60s. This finding is similar to that of the UK-based CPRD, where the incidence rate per 1,000 person-years was 2.62 cases for people in their 40s, 6.33 cases in their 50s, and 15.44 cases in their 60s. That is, people with DM in their 50s and 60s had 2.41 times and 5.89 times higher incidence rates of cataract, respectively [5]. Considering that cataract is one of the most common diseases that can lead to blindness in adults [14], regular eye check-ups to discover cataract at an early stage is very important for people with DM to maintain their quality of life and save medical costs. Therefore, according to the guidelines of the Korean Diabetes Association [36], nurses must encourage people with DM to undergo annual eye examinations at any age, including at the time of DM diagnosis.
In several studies, HbA1c has been identified as a risk factor for cataract in people with DM [17], and this study showed the same result. HbA1c reflects the average blood glucose level within three months prior to the test, and a higher HbA1c level indicates poorer glycemic control. Given that a strong positive relation exists between aqueous humor and blood glucose levels, prolonged exposure to high glucose levels is deemed to increase aqueous humor glucose levels [37]. A recent study reported an increase in the glycosylated amino acids in patients with DM compared with non-diabetic patients with cataract, which might be related to earlier cataract development in patients with DM [38]. However, HbA1c was identified as a factor related to cataract development in the model without the duration of DM, but not the one with it, and this may be related to a decrease in the statistical power attributable to substantial missing data on the duration of DM. Meanwhile, FPG, an indicator that reflects the blood glucose level or glycemic control, was found to be unrelated to cataracts. Given these results, regular HbA1c monitoring is considered more helpful in managing cataracts in patients with DM.
For the duration of DM, inconsistent results have been reported regarding its relationship with cataract development—a risk factor [5], a preventive factor [39], and an irrelevant factor [40]. In this study, the duration of DM was confirmed as a risk factor, increasing cataract risk by a factor of 1.05 when the duration of DM increases by one year. However, this finding differs considerably from the results of a study by Becker et al. [5], where the risk of cataract increased by a factor of 5.14 for a duration of DM < 2 years versus a duration of ≥ 10 years. The incidence of cataract was found to be higher in females than in males (25.8% vs. 15.1%), but there was no significant difference in the multivariate analysis, which was the same result as that of a previous systematic review reporting that sex was unlikely to be a risk factor for cataract in people with type 2 DM [17].
1. Strength and limitations
To our knowledge, this study is one of few studies that used a longitudinal study design to investigate cataract incidence and its predictive factors among people with DM. Considering that in South Korea, only about 60% of males and 68% of females aged ≥ 30 years with DM are aware of their DM status [41], the use of laboratory results as inclusion criteria may be helpful in minimizing the exclusion of DM patients. However, careful interpretation of the results is necessary because of the following limitations. First, because this study relied on self-reported cataract data, there may be problems with accuracy, as we could not validate the cataract diagnosis and underestimation and recall bias, compared with clinical tests [42]. Therefore, further studies are recommended to use objective outcome data. Second, the cataract type could not be considered in this study because of lack of data. Srinivasan et al. [16] analyzed subjects of the Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study and found that the incidence of cataract greatly differs between cataract types, that is, 7.3% for posterior subcapsular cataract and 70% for nuclear opalescence. This finding highlights the importance of further investigation into the incidence rate according to cataract type. Third, the time until cataract occurred, required for calculating cataract density, was measured using the difference in age between the time of the baseline survey and that of cataract incidence, entered in the KoGES. This is because it is difficult to identify the actual time of cataract incidence since KoGES is only conducted every other year. However, this method raises the possibility of recall bias because the age when cataract occurred was self-reported. Fourth, as the study subjects were those with prevalent type 2 DM, the duration of DM varied at the baseline survey. Accordingly, some of their characteristics at baseline might differ from those at the actual time of their DM development, although the duration of DM was used as an explanatory variable in the data analysis to control for the effect of DM progression. Further longitudinal studies with DM incident cases to identify factors related to cataract development are suggested. Fifth, the duration of DM was missing in about half of the participants because DM subjects were identified using self-report of DM diagnosis and medication as well as laboratory results based on previous studies [21, 22, 23]; this may lead to substantial loss of statistical power in multivariate regression analysis. Sixth, although compliance to treatment and follow-up in people with DM could affect glycemic control and in turn the occurrence of cataract, this dynamic could not be assessed here because of lack of data in the KoGES. Lastly, the generalizability of the findings to other population groups, except for the study subjects, is limited. A substantial proportion of individuals with DM at baseline (n = 305 [48%]) was excluded because of unknown, or no survey on, cataract history; the small sample size may decrease the representativeness of the study results. There were significant differences between included and excluded individuals on several characteristics, which may have increased selection bias. Therefore, caution should be exercised when interpreting and applying the results of this study to all people with DM living in Ansan as well as other small and medium-sized cities or rural areas in South Korea. The results of this study should be interpreted as being limited to the subjects of this study.
2. Clinical implications
Cataracts, one of the most common causes of blindness in adults, lead to a decrease in quality of life and an increase in economic burden. Considering that people with DM have twice as much risk of cataract development than those without DM, nurses working at hospitals or healthcare facilities in the community should educate people with DM about the major risk factors for cataract development based on the findings of this study, and recommend regular eye examinations so that cataracts can be identified as early as possible. Nursing researchers can help monitor continuously the magnitude of cataract risk in people with DM by constructing and validating a risk factor prediction model using the risk factors identified in this study. Finally, national health policy-makers can consider eye examinations in the health check-up items for those who have a high risk of cataract among people with DM or suspected to be in high glycemic condition.
CONCLUSION
The cataracts in people with DM is commonly occurred, at approximately two in every ten persons with DM over a ten-year period in South Korea. As age, HbA1c, and the duration of DM increase, the risk of cataract development also increases. These findings underscore the need for adherence to annual eye examination guidelines as age and the duration of DM increase, for the prevention and early detection of cataract. Considering negative effect of cataract on their quality of life and economic burden, nurses should identify people with DM at a higher risk of cataract development, and plan individual eye examination programs to detect cataract development as early as possible.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online at https://doi.org/10.4040/jkan.21081
Factors Related to the Cataract Development (N = 166)Supplementary Table 1
Comparison of Characteristics between the Included and the Excluded in the Study (N = 634)Supplementary Table 2
This work was presented at 2018 Winter Conference of Korean Academy of Community Health Nursing, December, 2018, Seoul, Korea.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization or/and Methodology: Jeong IS.
Data curation or/and Analysis: Jeong IS & Lee EJ & Kim MS & Yu JO & Yun HS & Jeong JH & Hwang YS.
Funding acquisition: None.
Investigation: None.
Project administration or/and Supervision: Jeong IS.
Resources or/and Software: Jeong IS.
Validation: Jeong IS & Lee EJ.
Visualization: Jeong IS & Lee EJ.
Writing original draft or/and Review & Editing: Jeong IS & Lee EJ & Kim MS & Yu JO & Yun HS & Jeong JH & Hwang YS.
ACKNOWLEDGEMENTS
None.
DATA SHARING STATEMENT
Data in this study were from the Korean Genome and Epidemiology Study (KoGES; 4851-302), National Research Institute of Health, Korea Disease Control and Prevention Agency, Ministry for Health and Welfare, Republic of Korea.
References
-
World Health Organization (WHO). Global report on diabetes [Internet]. Geneva: WHO; c2016 [cited 2021 Jun 22].Available from: https://www.who.int/publications/i/item/9789241565257.
-
-
International Diabetes Federation (IDF). Diabetes atlas 9th ed. [Internet]. Brussels: International Diabetes Federation; c2019 [cited 2021 Jun 22].Available from: https://www.diabetesatlas.org/en/resources.
-
-
Korean Diabetes Association (KDA). Diabetes fact sheet in Korea [Internet]. Seoul: KDA; c2020 [cited 2021 Jun 22].Available from: https://www.diabetes.or.kr/pro/news/admin.php?mode=list&category=A.
-
-
An S, Yu J. Factors influencing fundus examination in patients with diabetes. Journal of Korean Public Health Nursing 2018;32(1):44–55. [doi: 10.5932/JKPHN.2018.32.1.44]
-
-
Bakke Å, Cooper JG, Thue G, Skeie S, Carlsen S, Dalen I, et al. Type 2 diabetes in general practice in Norway 2005-2014: Moderate improvements in risk factor control but still major gaps in complication screening. BMJ Open Diabetes Research & Care 2017;5(1):e000459 [doi: 10.1136/bmjdrc-2017-000459]
-
-
Cougnard-Grégoire A, Korobelnik JF, Delyfer MN, Rigalleau V, Daien V, Creuzot-Garcher C, et al. Trends in the use of eye care services in adults treated for diabetes between 2008 and 2017 in France: A nationwide study. Ophthalmic Research 2020;63(5):452–459. [doi: 10.1159/000506136]
-
-
Lim HT, Choi KS. Factors associated with screening for diabetic retinopathy in diabetic patients aged > or = 40 years using the KNHANES IV. Journal of the Korean Ophthalmological Society 2012;53(4):516–521. [doi: 10.3341/jkos.2012.53.4.516]
-
-
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. The Lancet Global Health 2021;9(2):e144–e160. [doi: 10.1016/S2214-109X(20)30489-7]
-
-
Srinivasan S, Raman R, Swaminathan G, Ganesan S, Kulothungan V, Sharma T. Incidence, progression, and risk factors for cataract in type 2 diabetes. Investigative Ophthalmology & Visual Science 2017;58(13):5921–5929. [doi: 10.1167/iovs.17-22264]
-
-
National Institute of Health (NIH). KoGES scientific accomplishment [Internet]. Cheongju: NIH; 2020 [cited 2021 Jul 10].Available from: http://www.nih.go.kr/contents.es-
?mid=a50401010500#tabMenu.
-
-
Jee D, Park S. Hyperglycemia and Hypo-HDL-cholesterolemia are primary risk factors for age-related cataract, and a Korean-style balanced diet has a negative association, based on the Korean Genome and Epidemiology Study. Journal of Korean Medical Science 2021;36(23):e155 [doi: 10.3346/jkms.2021.36.e155]
-
-
Bae JC, Cho NH, Suh S, Kim JH, Hur KY, Jin SM, et al. Cardiovascular disease incidence, mortality and case fatality related to diabetes and metabolic syndrome: A community-based prospective study (Ansung-Ansan cohort 2001-12). Journal of Diabetes 2015;7(6):791–799. [doi: 10.1111/1753-0407.12248]
-
-
Dean AG, Sullivan KM, Soe MM. OpenEpi: Open source epidemiologic statistics for public health [computer Program]. Version. 3.01. Atlanta: OpenEpi; 2013Available from: http://www.openepi.com.
-
-
Tang Y, Wang X, Wang J, Jin L, Huang W, Luo Y, et al. Risk factors of age-related cataract in a Chinese adult population: The Taizhou Eye Study. Clinical & Experimental Ophthalmology 2018;46(4):371–379. [doi: 10.1111/ceo.13040]
-
-
Korean Statistical Information Service (KOSIS). Monthly average household balance per household by number of household members [Internet]. Daejeon: Statistics Korea; c2020 [cited 2021 Jun 22].
-
-
Ministry of Health and Welfare (MOHW). Korea health statistics 2012: Korea national health and nutrition examination survey. Sejong: MOHW; 2013 Dec.Report No.: 11-1351159-000027-10.
-
-
Korean Diabetes Association (KDA). Treatment guideline for diabetes. 6th ed. Seoul: KDA; 2019. pp. 129-130.
-
-
Pietrowska K, Dmuchowska DA, Krasnicki P, Bujalska A, Samczuk P, Parfieniuk E, et al. An exploratory LC-MS-based metabolomics study reveals differences in aqueous humor composition between diabetic and non-diabetic patients with cataract. Electrophoresis 2018;39(9-10):1233–1240. [doi: 10.1002/elps.201700411]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite