Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 50(1); 2020 > Article
- Original Article Menstrual Cycle Characteristics and Premenstrual Syndrome Prevalence Based on the Daily Record of Severity of Problems in Korean Young Adult Women
- Yae-Ji Kim1, Young-Joo Park2,
-
Journal of Korean Academy of Nursing 2020;50(1):147-157.
DOI: https://doi.org/10.4040/jkan.2020.50.1.147
Published online: January 31, 2020
2College of Nursing, Korea University, Seoul,
-
Corresponding author:
Young-Joo Park,
Email: yjpark@korea.ac.kr
Abstract
This descriptive study aimed to identify the menstrual cycle characteristics and premenstrual syndrome (PMS) prevalence in Korean young adult women using the retrospective and prospective Daily Record of Severity of Problems (DRSP).
In the first stage, participants included 151 nursing students studying in a university located in Seoul. Data were collected from April 20 to June 2, 2017, using the questionnaire on menstrual characteristics, pictorial blood assessment chart, and retrospective DRSP. In the second stage, participants included 17 students with PMS, based on the screening conducted in the first stage. Data were collected using the prospective DRSP from May 29 to 2 September 2, 2017.
Of the study sample, 104 participants (68.9%) had regular periods. Those with regular periods had 11.97 periods annually with a menstrual cycle of 29.38 days and a period duration of 5.72 days. Fifty-five participants (37.4%) showed menorrhagia. Sixty-four participants (42.4%) were found to have PMS based on their retrospective DRSP. When the ratio of women (52.9%) with PMS shown in the prospective DRSP was used as a positive predictive value, the estimated PMS prevalence was 22.4%.
This study provides clinically significant PMS prevalence among Korean young adult women, positive predictive value of the retrospective DRSP, and valid data to basically understand the menstrual cycle characteristics experienced by these women.
Published online Feb 28, 2020.
https://doi.org/10.4040/jkan.2020.50.1.147
Menstrual Cycle Characteristics and Premenstrual Syndrome Prevalence Based on the Daily Record of Severity of Problems in Korean Young Adult Women
Abstract
Purpose
This descriptive study aimed to identify the menstrual cycle characteristics and premenstrual syndrome (PMS) prevalence in Korean young adult women using the retrospective and prospective Daily Record of Severity of Problems (DRSP).
Methods
In the first stage, participants included 151 nursing students studying in a university located in Seoul. Data were collected from April 20 to June 2, 2017, using the questionnaire on menstrual characteristics, pictorial blood assessment chart, and retrospective DRSP. In the second stage, participants included 17 students with PMS, based on the screening conducted in the first stage. Data were collected using the prospective DRSP from May 29 to 2 September 2, 2017.
Results
Of the study sample, 104 participants (68.9%) had regular periods. Those with regular periods had 11.97 periods annually with a menstrual cycle of 29.38 days and a period duration of 5.72 days. Fifty-five participants (37.4%) showed menorrhagia. Sixty-four participants (42.4%) were found to have PMS based on their retrospective DRSP. When the ratio of women (52.9%) with PMS shown in the prospective DRSP was used as a positive predictive value, the estimated PMS prevalence was 22.4%.
Conclusion
This study provides clinically significant PMS prevalence among Korean young adult women, positive predictive value of the retrospective DRSP, and valid data to basically understand the menstrual cycle characteristics experienced by these women.
INTRODUCTION
Menstruation, also known as menses or menstrual period, is a physiological condition experienced by a woman of reproductive age. During menstrual cycle, women may experience various symptoms repetitively and cyclically that may affect their daily lives.
The International Society for Premenstrual Disorders has categorized premenstrual disorders (PMDs), including various symptoms a woman experiences before her menstruation, into two groups: core PMD (typical, pure, or reference disorders associated with spontaneous ovulatory menstrual cycles) and variant PMD (more complex features, including premenstrual exacerbation, PMD with anovulation, PMD with absent menstruation, and progestogen-induced PMD). Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are distinguished as core PMD [1].
PMS is a type of PMD that is characterized by various physical and emotional symptoms that occur repetitively during the luteal phase before menstruation and resolve in a few days into the period. This is considered the basic definition of PMS [2]. More detailed criteria are used by different classifications. For example, the 10th revision International Classification of Diseases only requires one symptom to establish the diagnosis of PMS, while the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and the American Congress of Obstetricians and Gynecologists (ACOG) focus more on the control of symptoms and treatments to identify PMS/PMDD in more clinically significant way [2].
Not only sensitivity and specificity for the identification of women with PMS symptoms but also estimation of PMS prevalence are influenced by various definitions of PMS [3]. Certainly, a meta-analysis study on PMS prevalence has stated that pooled PMS prevalence globally, obtained from articles reviewed in that study is 47.8%, with large differences between countries (ranging from 12.0% to 98.0%) [4]. Conversely, PMS prevalence shown in studies using the Premenstrual Symptoms Screening Tools (PSST) or Daily Record of Severity of Problems (DRSP), tools used to assess the symptoms based on the definitions of PMS by the DSM-IV or ACOG to identify women with clinically significant PMS/PMDD, ranged from 20.7% to 30.4% [5, 6].
Currently, the definition of PMS by the ACOG is clinically accepted for its diagnosis. According to ACOG's definition, symptoms appeared during the luteal phase before menstruation and should disappear within 4 days after the start of the period without showing recurrence until at least the 13th day of the menstruation cycle. Moreover, retrospectively, at least one emotionally distressing symptom and one physically distressing symptom should be observed for 5 days before menstruation for three cycles in a row, while based on the prospective daily recording, the above-mentioned symptoms should be observed for 5 days before menstruation for two cycles in a row [2, 7]. In other words, this definition requires not only retrospective recalls of the symptoms but also prospective recording of symptoms for the diagnosis of PMS. An accurate diagnosis of the condition using defined classification and customized care based on patient's symptom profile are required for the control and treatment of PMS symptoms. This means specific timing and severity of PMS symptoms should be identified [7, 8]. In this regard, the use of DRSP is recommended as this tool is developed to obtain an accurate prospective recording of the severity and timing of symptoms [7, 8, 9, 10].
However, daily recording of symptoms for two cycles may be inconvenient and difficult to be used in a clinical setting. Borenstein et al. [6] have compared the retrospective observation of DRSP on the first day of the period and the prospective observation of DRSP for two cycles and found that the retrospective observation on the first day of the period can screen women with PMS symptoms. This results in a complementary method, where the retrospective DRSP is used for the initial identification of women with PMS while the additional DRSP observation for two cycles is performed on these women identified as having PMS to ensure accuracy [6]. Conversely, in a comparative study between the retrospective PSST and prospective DRSP of two cycles, the retrospective use of PSST underreported PMS but overreported PMDD with high sensitivity (79.0%) but low specificity (33.3%). This led to the study's suggestion to reevaluate the positive PMS/PMDD cases by PSST using DRSP [10]. Therefore, initially identifying women with PMS using the retrospective DRSP or PSST and additionally using DRSP for women with PMS for two cycles might be required for convenience and accuracy.
In this regard, the retrospective DRSP recording on the first day of menstruation and the prospective DRSP recording for two menstrual cycles should be applied sequentially to investigate clinically significant PMS prevalence. This approach provides basic data on the positive predictive value of the retrospective DRSP. However, there have been no studies reporting PMS prevalence and the positive predictive value of the retrospective DRSP in Korean women by applying both retrospective and prospective recordings of DRSP, which are recommended for the diagnosis of clinically significant PMS. Additionally, the basic data on the menstrual cycle characteristics (regularity, frequency, duration, and volume) and menarche age in Korean women of reproductive age should be continuously updated with more objective measures.
Therefore, the present study aimed to assess the characteristics of menstruation (volume of menstrual blood flow, menstrual cycle frequency, regularity in cycle-to-cycle variation, and duration of blood flow) and menarche age, to investigate PMS symptoms using the retrospective DRSP on the first day of the menstruation, and to estimate clinically significant PMS prevalence and positive predictive value of the retrospective DRSP in Korean young adult women.
METHODS
1. Study design
This study consisted of two stages. The first stage used a retrospective cross-sectional design to identify menstrual cycle characteristics and menarche age of Korean young adult women and screen women with PMS using their retrospective DRSP. The second stage used a prospective descriptive design on participants with PMS symptoms using their prospective DRSP.
2. Setting and samples
In the first stage, a total of 259 students (as of 2017) studying in the Department of Nursing at K University in Seoul were the target participants of this study. After obtaining permission from the administrative department of the university, the advertisement was posted to recruit study participants, explaining the purpose and procedures of this study and criteria in selecting the possible participants for this study. A total of 151 (58.3%) students agreed to participate in this study and were all included in the final analysis. Participants with the following characteristics were included in the study: (1) participants who voluntarily agreed to participate in this study and (2) participants who had no experience of giving birth. Conversely, participants with the following characteristics were excluded: (1) participants under hormone treatment using estrogen or progestin and (2) participants not fluent in Korean.
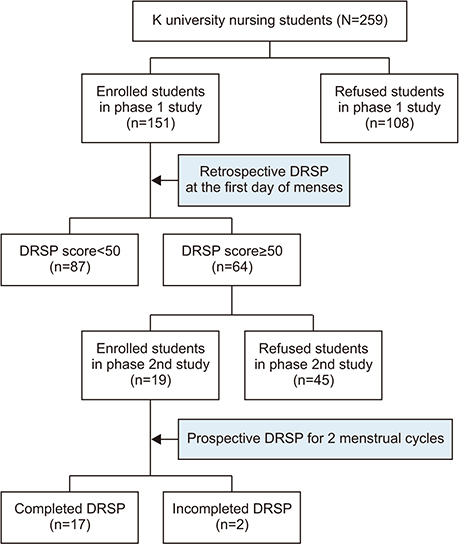
In the second stage, of the 151 participants in the first stage, 64 (42.4%) women were identified as having PMS symptoms. Of these 64 participants, 19 (29.7%) agreed to participate voluntarily in this stage. Two participants stopped recording their symptoms before the end of their first stage of the two menstrual cycles. Thus, the number of participants for the final analysis of the second study was 17 (Figure 1).
Figure 1
Participants flow chart.
DRSP=Daily record of severity of problems.
3. Ethical considerations
This study was approved by the Institutional Review Board of K University (Approval No.: 1040548-KU-IRB-17-4-A-1). The purpose and the method of this study were comprehensively explained to the participants to ask for their cooperation. These participants signed the written consent agreement. The researchers explained that their names and contact information were needed in the first stage as these will be required in the second stage of this study, with the assurance of confidentiality of such information. These participants were informed that they could discontinue their participation in this study any time without any disadvantage. The researchers contacted those who were identified as having PMS symptoms in the first stage by phone to explain the purpose and procedure of the second stage of this study and ask for their participation. The researchers ensured these voluntary participants that their personal information would be treated confidentially. The researchers explained the purpose and the procedure of the study to the the participants who agreed to participate in the final stage of the study.
4. Measurements and instruments
Daily record of severity of problems (DRSP): This study used DRSP to measure symptoms experienced during a menstrual cycle. DRSP was developed and validated by Endicott et al. [11]. DRSP has been used in other research studies to diagnose clinically significant PMS and PMDD [6, 11]. To assess the symptoms of PMS/PMDD under criteria A and criteria B defined by the DSM-IV, DRSP included 21 questions on 11 emotional and physical symptoms of criteria A and three questions on functional impairment due to symptoms classified under criteria B. Answer scores ranged from one to six: “not at all (score of 1),” “minimal (score of 2),” “mild (score of 3),” “moderate (score of 4),” “severe (score of 5),” and “extreme (score of 6).” A higher total score indicated more PMS. In this study, DRSP was translated into Korean by the authors and translated back to English again to ensure accuracy. After translating into Korean, DRSP verified the items' content validity from five nursing professors and three nursing graduate students. Items with a content validity index of 0.75 or higher were taken, and all items were taken as a result.
For the retrospective recording of symptoms to identify women with PMS, DRSP was used on the first day of the period based on research finding that DRSP on the first day of the period could be used as a screening tool to identify women with PMS symptoms [6]. The criteria to diagnose women with PMS were based on the following research finding: a woman could be diagnosed with PMS if the sum of scores she gave to the 21 questions related to symptoms, excluding the three questions on functional impairment, was 50 or higher [6, 9]. The Cronbach's α for internal consistency reliability was .93.
The second stage of the study was designed to prospectively assess the daily symptoms for two menstrual cycles experienced by women who were identified as having PMS in the first stage. Participants started recording from the first day of the period and left a “V” mark on the dates of the period. The diagnosis of PMS in the second stage required that the following two criteria should be met for at least one menstruation cycle: (1) the average score of at least three symptoms in the luteal phase was at least 30% higher than the average score of at least three symptoms in the follicular phase, and (2) the average score of at least three questions in the luteal phase was 3 or higher. The luteal phase was defined as the period of 5 days before the start of menstruation, while the follicular phase was defined as the period of 6 to 10 days from the start of menstruation [6, 9].
Menstrual cycle characteristics and menarche age: The questionnaire on menstrual cycle characteristics and menarche age was composed of nine items assessing the menarche age of the participant, menstrual cycle characteristics (menstrual cycle frequency, duration of blood flow, regularity of cycle-to-cycle variation), and presence of distressing condition during the period. The items were developed by the authors. Regarding the menstrual cycle characteristics of the period, participants recorded regularity of their period in the recent 1 year (regularity), the total number of periods in the recent 1 year, the period from the first day of a menstruation to the day before the next menstruation (frequency), and the period from the start of a period to the end of the period (duration).
Pictorial blood assessment chart: The Pictorial Blood Assessment Chart (PBAC) was used to assess menstrual blood volume. It was developed by Higham et al. [12]. PBAC allows the visualized recording of blood volume in pads, tampons, and blood clots. For pads, participants gave a score of 1 if blood volume was “little,” a score of 5 if “normal,” and a score of 20 if “very much.” For tampons, participants gave a score of 1 if blood volume was “little,” a score of 5 if “normal,” and a score of 10 if “very much.” Scores of 1 and 5 were given to small blood and big clots, respectively. In this study, the questionnaire was revised to compare the size of a clot to a coin size to record the blood volume more accurately. A higher total score indicated more blood volume during the period. A score greater than 100 was defined as menorrhagia [12].
General characteristics: The general characteristics of the participants were collected in the following six areas: age, height, weight, marital status, subjective social and economic level, and grade. Height (measured in meters) and weight (measured in kilograms) were used to calculate participant's body mass index (BMI). This study followed the specification provided by the Korean Society for the Study of Obesity. BMI level less than 18.5 kg/m2 was categorized as underweight, equal to or greater than 18.5 kg/m2 as normal, equal to or greater than 23 kg/m2 as overweight, equal to or greater than 25 kg/m2 as obese, and equal to or greater than 30 kg/m2 as extreme or severe obesity.
5. Data collection and procedure
Data collection for the first stage of this study was performed from April 20, 2017 to June 2, 2017. The authors distributed the questionnaire to the voluntary participants so that they could start writing on the first day of their periods. Questionnaires were subsequently collected by the authors. These collected questionnaires were assigned with random numbers by the authors, stored at a safe location, coded, and analyzed. Participants took approximately 20 to 25 minutes to complete the questionnaire. They were given rewards for their participation.
Data collection for the second stage of this study was performed from May 29, 2017, to September 2, 2017. Each individual had different menstruation cycle. Therefore, the period of data collection from these participants ranged from 47 to 76 days. Since the participants had to record their condition every day for two periods, for their convenience, participants could choose between computer recording and manual handwriting recording. All participants chose computer recording. The researchers sent DRSP via e-mail to these participants. Participants subsequently sent their DRSP after their period back to the researchers via e-mail. The DRSP of each participant was assigned with a unique number and stored in a portable external hard drive of the researchers to protect personal information.
6. Data analysis
Data collected from the first and second stages of this study were analyzed using the PC-SPSS program (version 24). Descriptive statistics were used for frequency, percentage, mean, and standard deviation of demographic characteristics, menstrual characteristics, and PMS. The following procedure was used to estimate PMS prevalence: (a) the frequency and percentage of participants who gave a score of 50 or higher in their retrospective DRSP in the first stage of this study were calculated; (b) in the second stage, the frequency and percentage of participants who gave at least 30% greater score in average to the luteal phase than to the follicular phase, while giving an average score of 3 or higher in at least three questions of the luteal phase at the same time, were calculated; and (c) the percentage obtained from the second stage of the study was applied to the participants in the first stage.
RESULTS
1. General characteristics of the participants
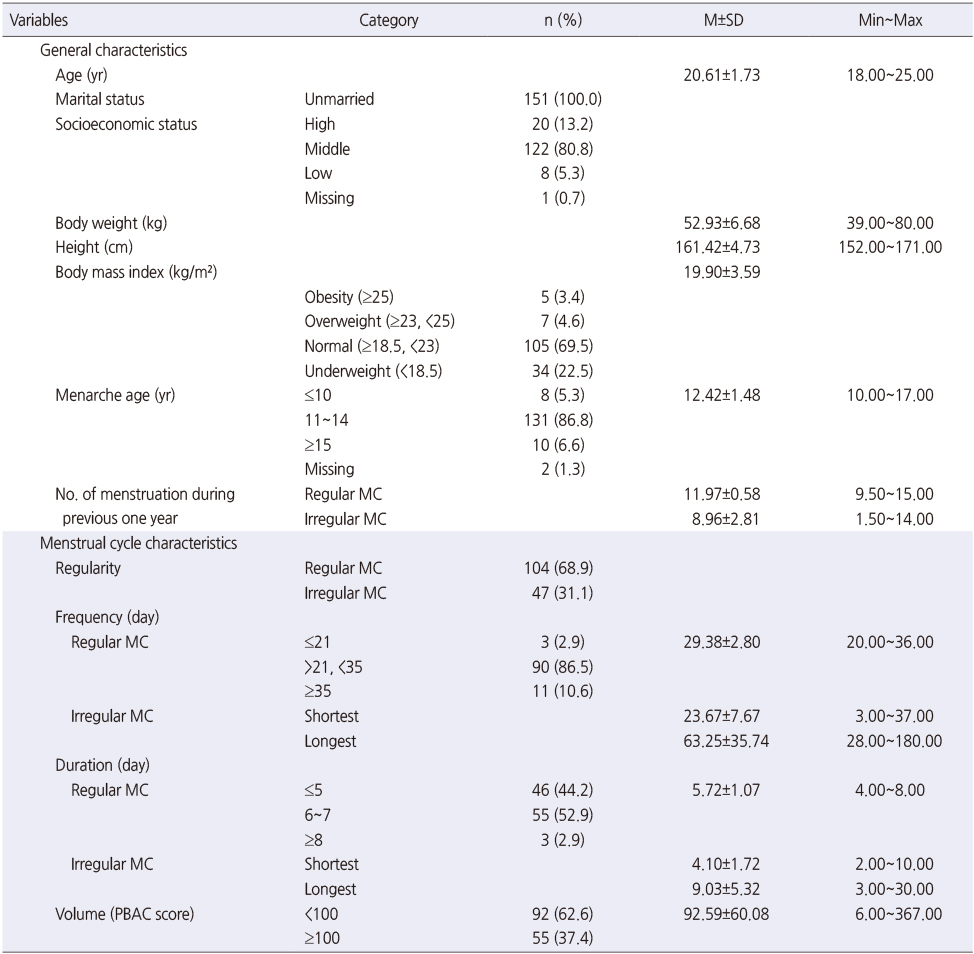
The mean age of the 151 participants included in this study was 20.61 years (range, 18 to 25 years). Their mean BMI was 19.90 kg/m2. BMI at normal range was the most common (69.5%), followed by underweight BMI (22.5%), overweight BMI (4.6%), and obese BMI (3.4%). All participants were unmarried. Most participants subjectively considered their socioeconomic level as “middle” (80.8%) (Table 1).
Table 1
General & Menstrual Cycle Characteristics of Young Adult Women (N=151)
2. Menstrual cycle characteristics and menarche age of the participants
Regarding the regularity of their periods, majority (68.9%) of the participants answered “generally regular,” while 31.1% answered “generally irregular.” The mean number of menses in the recent 1 year were 11.97 (range, 9.50 to 15.00) for women with regular periods and 8.96 (range, 1.50 to 14.00) for women with irregular periods.
The mean menstrual cycle frequency was 29.38 days (range, 20.00 to 36.00 days) long for participants with regular periods. Three (2.9%) participants answered that their cycles were shorter than 21 days, while 11 (10.6%) participants answered that their cycles were longer than 35 days. The shortest cycle among women with irregular menstruation cycle was 23.67 days, while the longest cycle was 63.25 days on average. The mean duration of a period of women with regular periods was 5.72 days. Among them, 44.2% (n=46), 52.9% (n=55), and 2.9% (n=3) answered that their periods lasted ≤5 days, 6 to 7 days, and ≥8 days, respectively. Among women with irregular periods, the mean shortest period was 4.10 days while the longest period was 9.03 days. The mean score given for blood volume using PBAC was 92.59. Fifty-five (37.4%) participants gave a score of 100 or higher, indicating menorrhagia.
The mean menarche age of the participants was 12.42 years, (range, 10~17 years). The most common menarche age was 11~14 years (86.8%), followed by 15 years or older (6.6%), and 10 years or younger (5.3%) (Table 1).
3. Premenstrual syndrome (PMS) symptoms by the retrospective DRSP
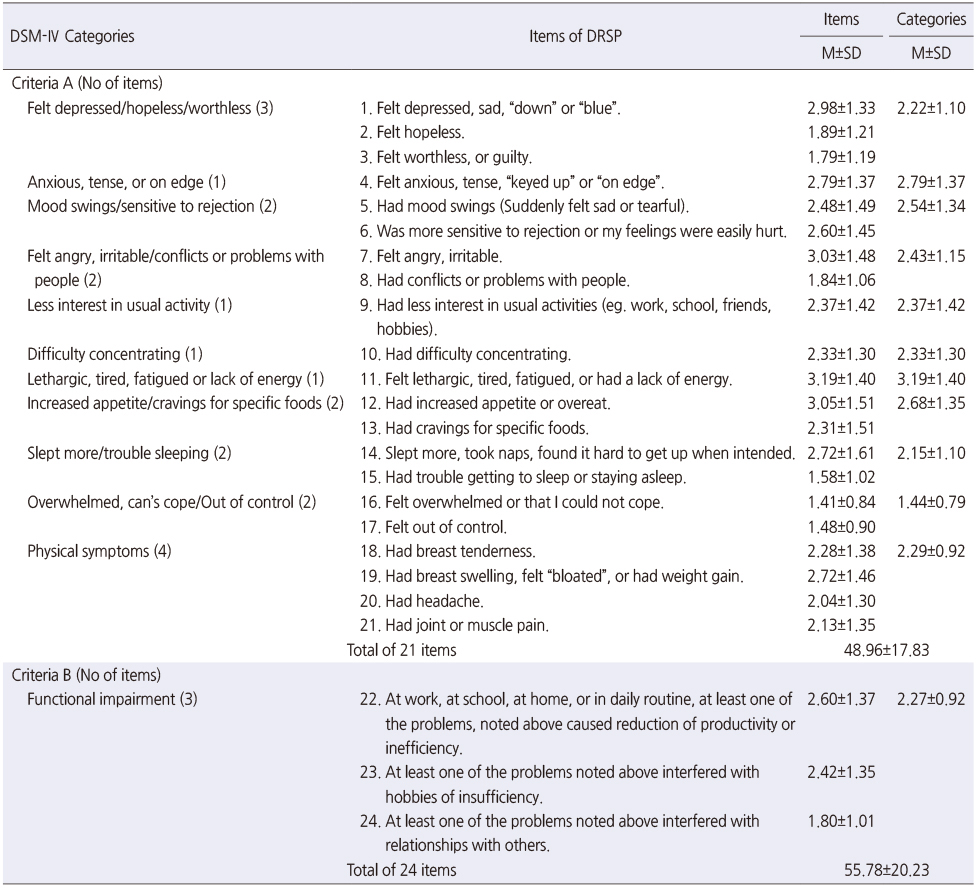
The mean retrospective DRSP score on the first day of the participants' periods, showing severity in the 11 physical and emotional symptoms (criteria A) defined by the DSM-IV, was 48.96. The mean score for the severity of functional impairment (criteria B) defined by the DSM-IV was 6.82, giving a total score of 55.78 in average.
More specifically, in criteria A, “lethargic, tired, fatigued, or average, followed by “anxious, tense, or on edge” symptom (2.79), “increased appetite/cravings for specific foods” symptom (2.68), “mood swings/sensitive to rejection” symptom (2.54), “felt angry, irritable/conflicts or problems with people” symptom (2.43), “less interest in usual activity” symptom (2.37), “difficulty concentrating” symptom (2.33), “physical symptoms” (2.29), “felt depressed/ hopeless/worthless” symptom (2.22), “slept more/trouble sleeping” symptom (2.15), and “overwhelmed, can't cope/out of control” symptom (1.44). In criteria B, the mean score of functional impairment (criteria B) was 2.29 (Table 2).
Table 2
Severity of Premenstrual Syndrome by Retrospective DRSP in Young Adult women (N=151)
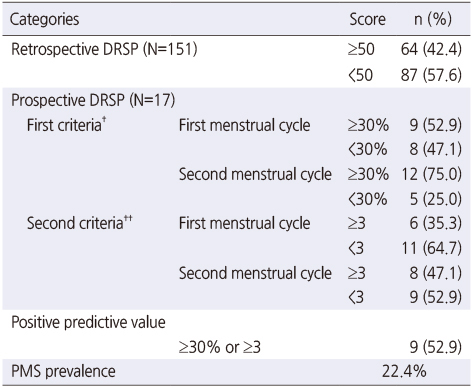
4. PMS prevalence and positive predictive value of the retrospective DRSP
Sixty-four (42.4%) participants with PMS had a total score of 50 or higher in the retrospective DRSP. Among these 64 women with PMS, 17 participated in the prospective DRSP for two periods, and 9 met both conditions (1) and (2) for the diagnosis of PMS for at least one period. When the ratio of women (9 out of 17, 52.9%) with PMS shown in the second stage of the study was used as a positive predictive value, PMS prevalence estimated from the total number of participants was 22.4% (Table 3).
Table 3
Positive Predictive Value of Prospective DRSP and PMS Prevalence
More specifically, the numbers of participants who met condition (1), who gave at least 30% higher score in average to the luteal phase score than to the follicular phase score in at least three symptoms, were 9 (52.9%) out of the 17 women in the first stage and 12 (75.0%) out of the 17 women in the second stage. The numbers of participants who met condition (2), with an average score of 3 or higher in at least three questions during the luteal phase, were 6 (35.3%) out of the 17 women in the first stage and 8 (47.1%) out of the 16 women in the second stage. Accordingly, the ratio of women with PMS shown in the second stage of the study, a positive predictive value, was 52.9% (9 out of 17) (Table 3).
DISCUSSION
The results of this study showed that the mean menarche age of the participants was 12.4 years. Of the total participants, 68.9% (104 women) reported that their periods were generally regular. The number of periods for those with regular intervals experienced in a year was 11.97 in average, ranging from 9.5 to 15. Their average menstrual cycle was 29.38 days, ranging from 20 to 36 days. In average, the period duration was 5.72 days long, ranging from 4 to 8 days.
In a recent study that analyzed the Fourth Korea National Health and Nutrition Examination Survey (2007~2009), women born between 1985~1989 and 1990~1994 (at the time of the survey, they had similar ages to the participants of this study) experienced their first stages of menstruation when they were 12.88 and 12.60 years old in average, respectively [13]. The mean menarche age of 538 women in another survey with an average age of 16.1 years was 12.6 years [14]. Compared to these studies, the mean menarche age of the participants in the present study was approximately 0.2 years younger. Regarding period characteristics, less number of women in this study had regular periods compared to 74.4% (1,940 in number) of 2,613 unmarried Danish women aged between 18 and 40 years. In that Danish study, women with a cycle shorter than 25 days accounted for 7.8% of women with regular periods, while 6.9% of women with regular periods reported a cycle longer than 33 days. Regarding the duration of a period, 35.8% of participants answered long periods lasting 5 days or longer [15]. A study with 4,892 Italian youth aged between 13 and 21 years showed a mean and median age of the first stage of 12.4. Of these participants, about 9% reported irregular periods, 3.0% had short menstrual cycles of 21 days or less, 3.4% had longer cycles of 35 days or more, 3.2% had period lasting ≤4 days, while 19% had period lasting ≥7 days [16]. Conversely, in a study conducted in women in North India, after 131 participants who did not answer the survey were excluded, 74.1% of the participants reported regular periods, with period lasting 3.96 days in average [17]. Compared to these studies reported so far, Korean women experienced their first menstruation at similar ages to other women worldwide. However, significantly higher number of Korean women reported irregular periods. Direct comparison with the Italian study was not possible since that study did not analyze the duration of a period and menstrual cycle separately for regular and irregular periods. However, it seems that a relatively lower percentage of Korean women falls under the “normal” range of menstrual cycle or duration of a period. On the contrary, the Fifth National Health and Nutrition Examination Survey (2010~2012) on Korean women aged between 19 and 40 years reported that 14.3% of 3,194 women had irregular periods [18]. Among those aged between 19 and 29 years, 18.4% had irregular periods [19]. According to Lee et al.'s study [14], 32.3% of participants answered that they had irregular periods.
However, most of the previous studies in Korea used multiple-choice questions to measure menstrual cycles and duration of a period. Moreover, even if the studies reported the menstrual characteristics of Korean women with large samples, they were based on secondary data analysis [18, 20, 21]. Therefore, these studies did not clearly present the menstrual characteristics of Korean women. Additionally, a study analyzing the menstrual cycles and duration of periods based on regularity of a period has not been conducted yet. This study presents some advantages in this regard by showing more accurate characteristics of periods experienced by Korean women. However, this study has the following limitation: it has a small sample size. Further improvements can be made by conducting studies with larger sample sizes to provide more accurate data to comprehensively understand the menstrual cycle characteristics of women with regular and irregular periods.
In particular, this study used PBAC scoring to more objectively evaluate the blood volume during a period. Results showed that 37.4% of young adult women who participated in the study gave a PBAC score higher than 100, indicating the presence of menorrhagia. Regarding the volume of blood flow, most Korean studies [14] subjectively measured the blood volume as “little,” “normal,” and “much.” Even when the volume was measured in an objective manner, the above mentioned studies had the following limitation: they used sanitary pads to measure blood volume. The study conducted in 376 female university students used the same PBAC scoring as this study, showing that 21.8% (n=82) of participants gave a PBAC score higher than 100, which indicated blood loss >80 mL during a period [22]. Compared to that study, it seems that menorrhagia is more common in Korean women. Additionally, the study cited above conducted pelvic examination on 82 women who were diagnosed with menorrhagia. Among the 76 women who received pelvic examination, 11 (14.5%) were found to have bleeding disorders including platelet function disorder and von Willebrand disease [22]. However, this study could not further examine women found to have menorrhagia. Therefore, the presence of menorrhagia should be screened using PBAC scoring, and the cause should be investigated in future studies.
In the present study, PMS prevalence was 42.4% based on the retrospective DRSP on the first day of a period. PMS prevalence was 22.5% when the positive predictive value (52.9%) obtained from the two prospective DRSP was applied to the second stage of the study.
In the study conducted in 897 Iranian youth aged between 12 and 18 years, PMS prevalence was 47.3%, among which 37.3% required drug to relieve their symptoms [23]. However, the tool used to screen PMS in that study was developed by the researcher. It required only one physical symptom and one emotional symptom to establish the diagnosis of PMS. A study conducted in 258 Ethiopian women aged between 18 and 25 years using the DSM-IV definition for PMS has reported a prevalence of 37.0% [24]. However, a study conducted in Chinese women having regular cycles (25 to 35 days) showed a PMS/PMDD prevalence of 21.1% with PMS under the ACOG definition and 2.1% with PMS under the prospective DRSP (the one used in the present study) [25]. A Korean study conducted in 934 women with an average age of 15.9 years who were retrospectively diagnosed with PMS using PSST and analyzed participant responses by four groups (PMDD, subthreshold PMDD, moderate/severe PMS, and no/mild PMS) has found that the percentage of women with PMS/PMDD women (i.e., women who gave responses other than no/mild PMS) was 20.0% [26]. Thus, PMS prevalence of 22.4% found in this study by identifying women with PMS using the retrospective DRSP on the first day of the period and having prospective DRSP on those women with PMS can be interpreted as a reliable result. However, the sample size was relatively small. Hence, studies with larger sample sizes are required in the future. Additionally, the positive predictive value of 52.9% found in this study was similar to a value of 53.8% found in international studies [6]. However, additional local studies should be conducted to add validity to the positive/negative predictive values in Korea.
Difficulties experienced by PMS/PMDD symptoms can negatively affect women in reaching academic and social achievements, resulting in decreased quality of life [24, 26]. Additionally, these symptoms have significant association with the occurrence of physical disorders such as high blood pressure and irritable bowel syndrome [27, 28]. PMS/PMDD symptoms are also known to be associated with dangerous impulse of committing suicide since these symptoms are related to impulsive emotions and anger [29]. Therefore, clear categorization of clinically significant PMS/PMDD and careful plan for treatment are required. In this regard, this study aimed to accurately measure and diagnose the period characteristics and PMS of young adult Korean women. However, this study has the following limitation: it has a small sample size. This needs to be improved by future studies.
Consequently, this study provide basic data on the PMS prevalence of women who require clinical management and the positive predictive value of the retrospective DRSP in Korean young adult women. Additionally, it provides basic data on the four parameters (regularity, frequency, duration, and volume of menstrual blood flow) of menstrual cycle characteristics surveyed by more accurate and objective measures in Korean young adult women.
CONCLUSION
In the first stage of this study, a retrospective cross-sectional design was used to determine the menstrual cycle characteristics and to determine Korean young adult women with PMS. In the second stage of this study, daily prospective DRSP recording was established for two menstruation cycles to identify clinically significant PMS prevalence. In conclusion, this study shows clinically significant PMS prevalence among Korean young adult women and positive predictive value of the retrospective DRSP. It provides reliable and valid data to basically understand the characteristics and the nature of a menstrual period experienced by Korean young adult women. A more extensive study with a larger sample size is required in the future to overcome the limitations of the current study.
This manuscript was based on a part of the first author's master's thesis from Korea University. Year of approval 2018.
CONFLICTS OF INTEREST:The authors declared no conflict of interest.
AUTHOR CONTRIBUTIONS:
Conceptualization and Methodology: Park YJ.
Data curation or/and Analysis: Kim YJ & Park YJ.
Funding acquisition: Kim YJ & Park YJ.
Investigation: Kim YJ.
Project administration or/and Supervision: Kim YJ & Park YJ.
Resources or/and Software: Kim YJ.
Validation: Park YJ.
Visualization: Kim YJ & Park YJ.
Writing original draft or/and Review & editing: Kim YJ & Park YJ.
References
-
Dean BB, Borenstein JE, Knight K, Yonkers K. Evaluating the criteria used for identification of PMS. Journal of Women's Health 2006;15(5):546–555. [doi: 10.1089/jwh.2006.15.546]
-
-
Direkvand-Moghadam A, Sayehmiri K, Delpisheh A, Kaikhavandi S. Epidemiology of premenstrual syndrome (PMS)-a systematic review and meta-analysis study. Journal of Clinical and Diagnostic Research 2014;8(2):106–109. [doi: 10.7860/JCDR/2014/8024.4021]
-
-
Steiner M, Macdougall M, Brown E. The premenstrual symptoms screening tool (PSST) for clinicians. Archives of Women's Mental Health 2003;6(3):203–209. [doi: 10.1007/s00737-003-0018-4]
-
-
Nevatte T, O'Brien PMS, Bäckström T, Brown C, Dennerstein L, Endicott J, et al. ISPMD consensus on the management of premenstrual disorders. Archives of Women's Mental Health 2013;16(4):279–291. [doi: 10.1007/s00737-013-0346-y]
-
-
Biggs WS, Demuth RH. Premenstrual syndrome and premenstrual dysphoric disorder. American Family Physician 2011;84(8):918–924.
-
-
Henz A, Ferreira CF, Oderich CL, Gallon CW, Castro JRS, Conzatti M, et al. Premenstrual syndrome diagnosis: A comparative study between the daily record of severity of problems (DRSP) and the premenstrual symptoms screening tool (PSST). Revista Brasileira de Ginecologia e Obstetricia 2018;40(1):20–25. [doi: 10.1055/s-0037-1608672]
-
-
Endicott J, Nee J, Harrison W. Daily record of severity of problems (DRSP): Reliability and validity. Archives of Women's Mental Health 2006;9(1):41–49. [doi: 10.1007/s00737-005-0103-y]
-
-
Kumar D, Goel NK, Puri S, Pathak R, Sarpal SS, Gupta S, et al. Menstrual pattern among unmarried women from Northern India. Journal of Clinical and Diagnostic Research 2013;7(9):1926–1929. [doi: 10.7860/JCDR/2013/6702.3359]
-
-
Jung EK, Kim SW, Ock SM, Jung KI, Song CH. Prevalence and related factors of irregular menstrual cycles in Korean women: The 5th Korean national health and nutrition examination survey (KNHANES-V, 2010–2012). Journal of Psychosomatic Obstetrics and Gynecology 2018;39(3):196–202. [doi: 10.1080/0167482X.2017.1321631]
-
-
Jung AN, Park JH, Kim J, Kim SH, Jee BC, Cha BH, et al. Detrimental effects of higher body mass index and smoking habits on menstrual cycles in Korean women. Journal of Women's Health 2017;26(1):83–90. [doi: 10.1089/jwh.2015.5634]
-
-
Bahrami A, Bahrami-Taghanaki H, Afkhamizadeh M, Avan A, Mazloum Khorasani Z, Esmaeili H, et al. Menstrual disorders and premenstrual symptoms in adolescents: Prevalence and relationship to serum calcium and vitamin D concentrations. Journal of Obstetrics and Gynaecology 2018;38(7):989–995. [doi: 10.1080/01443615.2018.1434764]
-
-
Tolossa FW, Bekele ML. Prevalence, impacts and medical managements of premenstrual syndrome among female students: Cross-sectional study in College of Health Sciences, Mekelle University, Mekelle, Northern Ethiopia. BMC Women's Health 2014;14:52. [doi: 10.1186/1472-6874-14-52]
-
-
Qiao M, Zhang H, Liu H, Luo S, Wang T, Zhang J, et al. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample in China. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2012;162(1):83–86. [doi: 10.1016/j.ejogrb.2012.01.017]
-
-
Bertone-Johnson ER, Whitcomb BW, Rich-Edwards JW, Hankinson SE, Manson JE. Premenstrual syndrome and subsequent risk of hypertension in a prospective study. American Journal of Epidemiology 2015;182(12):1000–1009. [doi: 10.1093/aje/kwv159]
-
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 Cite
Cite

