Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 45(6); 2015 > Article
-
Original Article
- Ecological Correlates of Cardiovascular Disease Risk in Korean Blue-collar Workers: A Multi-level Study
- Won Ju Hwang1, Yunhee Park2
-
Journal of Korean Academy of Nursing 2015;45(6):857-867.
DOI: https://doi.org/10.4040/jkan.2015.45.6.857
Published online: December 15, 2015
1College of Nursing Science· East-west Nursing Research Institute, Kyung Hee University, Seoul
2Department of Nursing, Youngdong University, Youngdong, Korea
1College of Nursing Science· East-west Nursing Research Institute, Kyung Hee University, Seoul
2Department of Nursing, Youngdong University, Youngdong, Korea
- Address reprint requests to : Park, Yunhee Department of Nursing, Youngdong University, 310 Taehak-ro, Youngdong-eup, Youndong 29131, Korea Tel: +82-43-740-1386 Fax: +82-43-740-1389 E-mail: yhpark118@gmail.com
Copyright © 2015 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
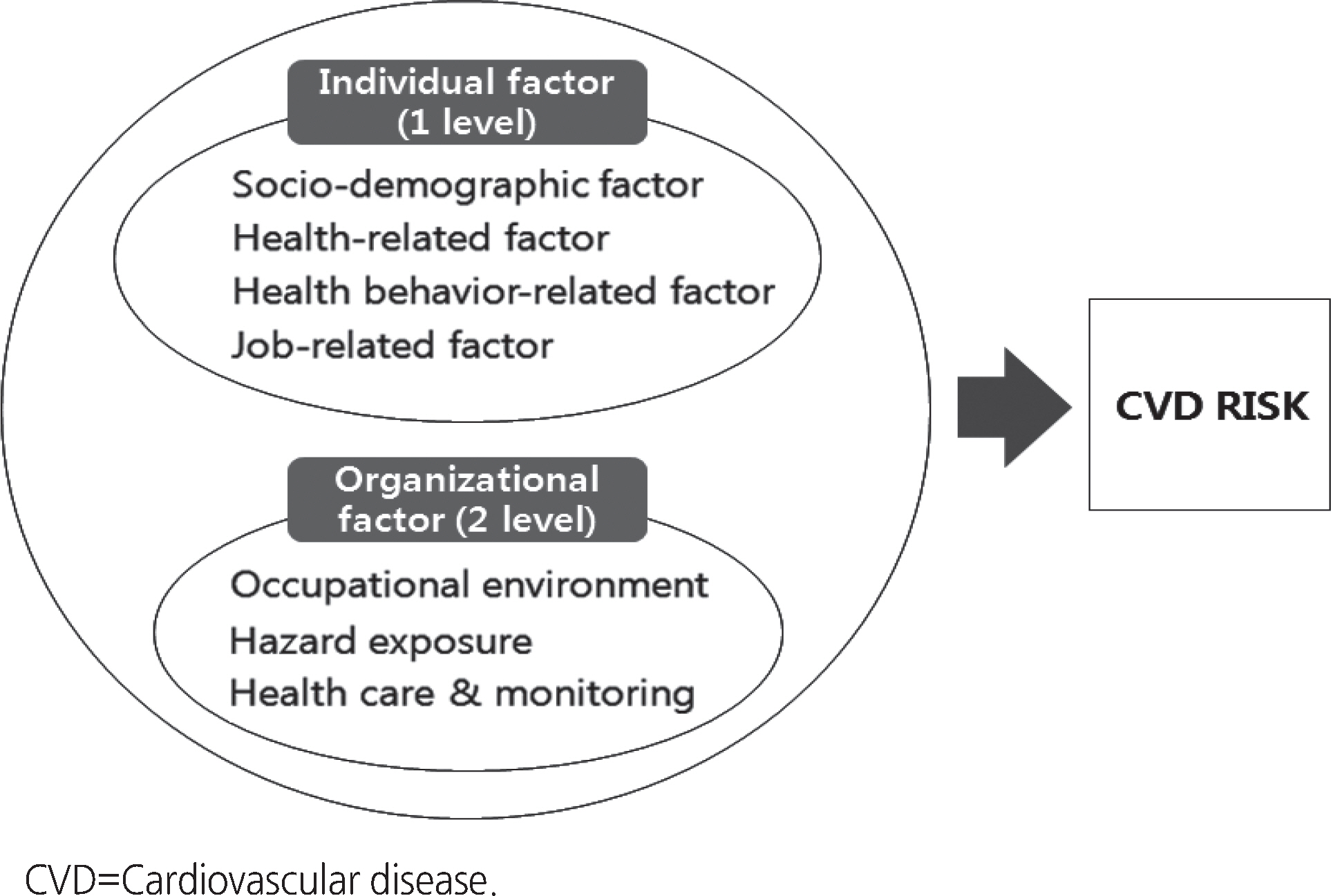
- The purpose of this study was to investigate individual and organizational level of cardiovascular disease (CVD) risk factors associated with CVD risk in Korean blue-collar workers working in small sized companies.
-
Methods
- Self-report questionnaires and blood sampling for lipid and glucose were collected from 492 workers in 31 small sized companies in Korea. Multilevel modeling was conducted to estimate effects of related factors at the individual and organizational level.
-
Results
- Multilevel regression analysis showed that workers in the workplace having a cafeteria had 1.81 times higher CVD risk after adjusting for factors at the individual level (p=.022). The explanatory power of variables related to organizational level variances in CVD risk was 17.1%.
-
Conclusion
- The results of this study indicate that differences in the CVD risk were related to organizational factors. It is necessary to consider not only individual factors but also organizational factors when planning a CVD risk reduction program. The factors caused by having cafeteria in the workplace can be reduced by improvement in the CVD-related risk environment, therefore an organizational-level intervention approach should be available to reduce CVD risk of workers in small sized companies in Korea.
| Variables | Characteristics | Categories |
Organizations |
Workers |
CVD risk |
t | p |
|---|---|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | M± SD | |||||
| Occupational | Number of employee | 76.87± 73.08 | − 0.27* | .145 | |||
| environment | Having cafeteria in | No | 10 (32.3) | 62 (12.6) | 5.44±5.32 | − 1.61 | .090 |
| workplace | Yes | 21 (67.7) | 430 (87.4) | 6.58±4.88 | |||
| Having resting area in | No | 18 (58.1) | 461 (93.7) | 6.60±3.41 | 1.96 | .050 | |
| workplace | Yes | 13 (41.9) | 31 (6.3) | 5.04±1.39 | |||
| Hazard exposure | Chemical hazard exposure | No | 29 (93.5) | 440 (89.4) | 5.80±3.57 | − 0.74 | .581 |
| Yes | 2 (6.5) | 52 (10.6) | 6.54±3.01 | ||||
| Noise exposure | No | 19 (61.3) | 258 (52.4) | 5.06±4.79 | − 2.30 | .022 | |
| Yes | 12 (38.7) | 234 (47.6) | 6.16±5.71 | ||||
| Health care & | Managed by occupational | No | 13 (41.9) | 221 (44.9) | 6.20±5.86 | 2.31 | .021 |
| monitoring | health nurse | Yes | 18 (58.1) | 271 (55.1) | 5.08±4.68 |
- 1. Korea Occupational Safety and Health Agency. Occupational injuries and illnesses for 2011 [Internet]. Gwacheon: Ministry of Employment and Labor; 2012.[cited 2015 February 25]. Available from:. http://www.kosha.or.kr/www/boardView.do?contentId=343906&menuId=554&boardType=A2
- 2. Kim CJ, Kang S. Development and a pilot test of an internet-based cardiovascular risk reduction program for Korean male workers with metabolic syndrome. Computers Informatics Nursing. 2013;31(4):157–166. http://dx.doi.org/10.1097/NXN.0b013e3182812829Article
- 3. Kim EY, Hwang SY. Development and evaluation of a small group-based cardiocerebrovascular disease prevention education program for male bus drivers. Journal of Korean Academy of Nursing. 2012;42(3):322–332. http://dx.doi.org/10.4040/jkan.2012.42.3.322ArticlePubMed
- 4. Hwang WJ, Hong O. Work-related cardiovascular disease risk factors using a socioecological approach: Implications for practice and research. European Journal of Cardiovascular Nursing. 2012;11(1):114–126. http://dx.doi.org/10.1177/1474515111430890ArticlePubMedPDF
- 5. Won JU, Hong OS, Hwang WJ. Actual cardiovascular disease risk and related factors: A cross-sectional study of Korean blue collar workers employed by small businesses. Workplace Health & Safety. 2013;61(4):163–171. http://dx.doi.org/10.3928/21650799-20130327-17Article
- 6. Hwang WJ, Hong O, Kim MJ. Factors associated with blue-collar workers’ risk perception of cardiovascular disease. Journal of Korean Academy of Nursing. 2012;42(7):1095–1104. http://dx.doi.org/10.4040/jkan.2012.42.7.1095ArticlePubMed
- 7. Kim CJ, Kim DJ, Park HR. Effects of a cardiovascular risk reduction intervention with psychobehavioral strategies for Korean adults with type 2 diabetes and metabolic syndrome. The Journal of Cardiovascular Nursing. 2011;26(2):117–128. http://dx.doi.org/10.1097/JCN.0b013e3181ec02aeArticlePubMed
- 8. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15(4):351–377.ArticlePubMedPDF
- 9. Ahn YH, Ham OK, Kim SH, Park CG. Multilevel analysis of health care service utilization among medical aid beneficiaries in Korea. Journal of Korean Academy of Nursing. 2012;42(7):928–935. http://dx.doi.org/10.4040/jkan.2012.42.7.928ArticlePubMed
- 10. Raudenbush SW, Bryk AS. A hierarchical model for studying school effects. Sociology of Education. 1986;59(1):1–17. http://dx.doi.org/10.2307/2112482Article
- 11. Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London, UK: Sage; 1999.
- 12. D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation.
- 13. World Health Organization Western Pacific Region. The Asia-pacific perspective: Redefining obesity and its treatment [Internet]. Geneva, CH: World Health Organization; 2000.[cited 2015 February 15]. Available from:. http://www.wpro.who.int/nutrition/doc-uments/docs/Redefiningobesity.pdf?ua=1
- 14. International Physical Activity Questionnaire. International Physical Activity Questionnaire (IPAQ) short form: Korean version [Internet]. Solna, SE: Author; 2006.[cited 2015 February 15]. Available from:. https://docs.google.com/viewer?a=v&pid=sites&srcid=ZGVmYXVsdGRvbWFpbnx0aGVpcGFxfGd4OjViMGM2OWI3Mjc5NjBjMTE
- 15. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96. http://dx.doi.org/10.1161/circulationaha.106.176158ArticlePubMed
- 16. Ruidavets JB, Ducimeti re P, Evans A, Montaye M, Haas B, Bingham A, et al. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: The prospective epidemiological study of myocardial infarction (PRIME). BMJ: British Medical Journal. 2010;341:c6077http://dx.doi.org/10.1136/bmj.c6077Article
- 17. Liu Y, Tanaka H. Overtime work, insufficient sleep, and risk of non-fatal acute myocardial infarction in Japanese men. Occupational and Environmental Medicine. 2002;59(7):447–451. http://dx.doi.org/10.1136/oem.59.7.447ArticlePubMedPMC
- 18. The National Institute for Occupational Safety and Health. Criteria for a recommended standard: Occupational noise exposure [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; 1998.[cited 2015 July 11]. Available from:. http://www.cdc.gov/niosh/docs/98-126/
- 19. Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4):488–495. http://dx.doi.org/10.1097/EDE.0b013e3181a819a1ArticlePubMedPMC
- 20. Park K, Hwang SY. 10-year risk for cardiovascular disease among male workers in small-sized industries. The Journal of Cardiovascular Nursing. 2015;30(3):267–273. http://dx.doi.org/10.1097/jcn.0000000000000146ArticlePubMed
- 21. Atella V, Kopinska J. Body weight, eating patterns, and physical activity: The role of education. Demography. 2014;51(4):1225–1249. http://dx.doi.org/10.1007/s13524-014-0311-zArticlePubMedPDF
- 22. Kim JH. A meta-analysis of effects of job stress management interventions (SMIs). Journal of Korean Academy of Nursing. 2007;37(4):529–539.ArticlePubMedPDF
- 23. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA: Journal of the American Medical Association. 2009;301(19):2024–2035. http://dx.doi.org/10.1001/jama.2009.681
- 24. Organisation for Economic Co-operation and Development. ALFS summary tables: Annual civilian labour force [Internet]. Paris, FR: Author; 2013.[cited 2015 March 9]. Available from:. http://stats.oecd.org/index.aspx?queryid=27359#
- 25. Kang DR, Ha Y, Hwang WJ. Prevalence and associated risk factors of the metabolic syndrome in the Korean workforce. Industrial Health. 2013;51(3):256–265. http://dx.doi.org/10.2486/indhealth.2012-0044ArticlePubMed
- 26. Jee SH, Batty GD, Jang Y, Oh DJ, Oh BH, Lee SH, et al. The Korean heart study: Rationale, objectives, protocol, and preliminary results for a new prospective cohort study of 430,920 men and women. European Journal of Preventive Cardiology. 2014;21(12):1484–1492. http://dx.doi.org/10.1177/2047487313497602ArticlePubMedPDF
- 27. Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health. 2010;10:62http://dx.doi.org/10.1186/1471-2458-10-62PubMedPMC
- 28. Goetzel RZ, Baker KM, Short ME, Pei X, Ozminkowski RJ, Wang S, et al. First-year results of an obesity prevention program at The Dow Chemical Company. Journal of Occupational and Environmental Medicine. 2009;51(2):125–138. http://dx.doi.org/10.1097/JOM.0b013e3181954b03ArticlePubMedPMC
- 29. Ministry of Health & Welfare, Korea Centers for Disease Control & Prevention. Korea health statistics 2013: Korea national health and nutrition examination survey (KNHANES VI-1). Sejong: Ministry of Health & Welfare; 2014.
- 30. Carlsson AC, Riserus U, rnl v J, Born Y, Leander K, Gigante B, et al. Prediction of cardiovascular disease by abdominal obesity measures is dependent on body weight and sex-results from two community based cohort studies. Nutrition Metabolism and Cardiovascular Diseases. 2014;24(8):891–899. http://dx.doi.org/10.1016/j.numecd.2014.02.001Article
REFERENCES
Figure & Data
REFERENCES
Citations

- Multilevel Analysis of Factors Affecting Health-Related Quality of Life of the Elderly
Hyunjung Moon, Sunkyung Cha
Journal of Korean Academy of psychiatric and Mental Health Nursing.2022; 31(3): 391. CrossRef - Socioeconomic Disparities in Cardiovascular Health in South Korea
Chi-Young Lee, Eun-Ok Im
Journal of Cardiovascular Nursing.2021; 36(1): 8. CrossRef - Health promotion program for office workers with SEM based on the WHO’s healthy workplace framework
Hosihn Ryu, Jiyeon Jung, Jihyun Moon
Health Promotion International.2020; 35(6): 1369. CrossRef - Effects of a Yoga Program in Reducing Cardiovascular Disease Risk Factors in Workers of Small Workplaces: A Pilot Test
Won Ju Hwang, Jin Ah Kim, Ji Sun Ha
Sustainability.2020; 12(23): 10038. CrossRef - An Exploration of Contextual Aspects that Influence Cardiovascular Disease Risks Perceived by Workers in a Small–Medium-Sized Workplace
Jin Ah Kim, Won Ju Hwang, Juhye Jin
International Journal of Environmental Research and Public Health.2020; 17(14): 5155. CrossRef - Measurement of Socioeconomic Position in Research on Cardiovascular Health Disparities in Korea: A Systematic Review
Chi-Young Lee, Yong-Hwan Lee
Journal of Preventive Medicine and Public Health.2019; 52(5): 281. CrossRef - Developing a Health-Promotion Program Based on the Action Research Paradigm to Reduce Cardiovascular Disease Risk Factors among Blue Collar Workers
Won Ju Hwang, Jin Ah Kim
International Journal of Environmental Research and Public Health.2019; 16(24): 4958. CrossRef - Regional Factors on the Self-rated Health of Wage Workers
Minjung Kwon, Eunsuk Choi
Journal of Korean Academy of Community Health Nursing.2018; 29(1): 21. CrossRef - A Systematic Review of Interventions for Workers with Cardiovascular Disease Risk Factors: Using an Ecological Model
Won Ju Hwang, Yunhee Park, Jin Ah Kim
Korean Journal of Occupational Health Nursing.2016; 25(1): 41. CrossRef - CVD-related Knowledge, Perception, Belief and Prevention Behaviors of Korean Blue-collar Workers: Needs Assessment for Developing the Intervention Program through Qualitative Approach
Won Ju Hwang, Yunhee Park
Korean Journal of Occupational Health Nursing.2016; 25(4): 362. CrossRef
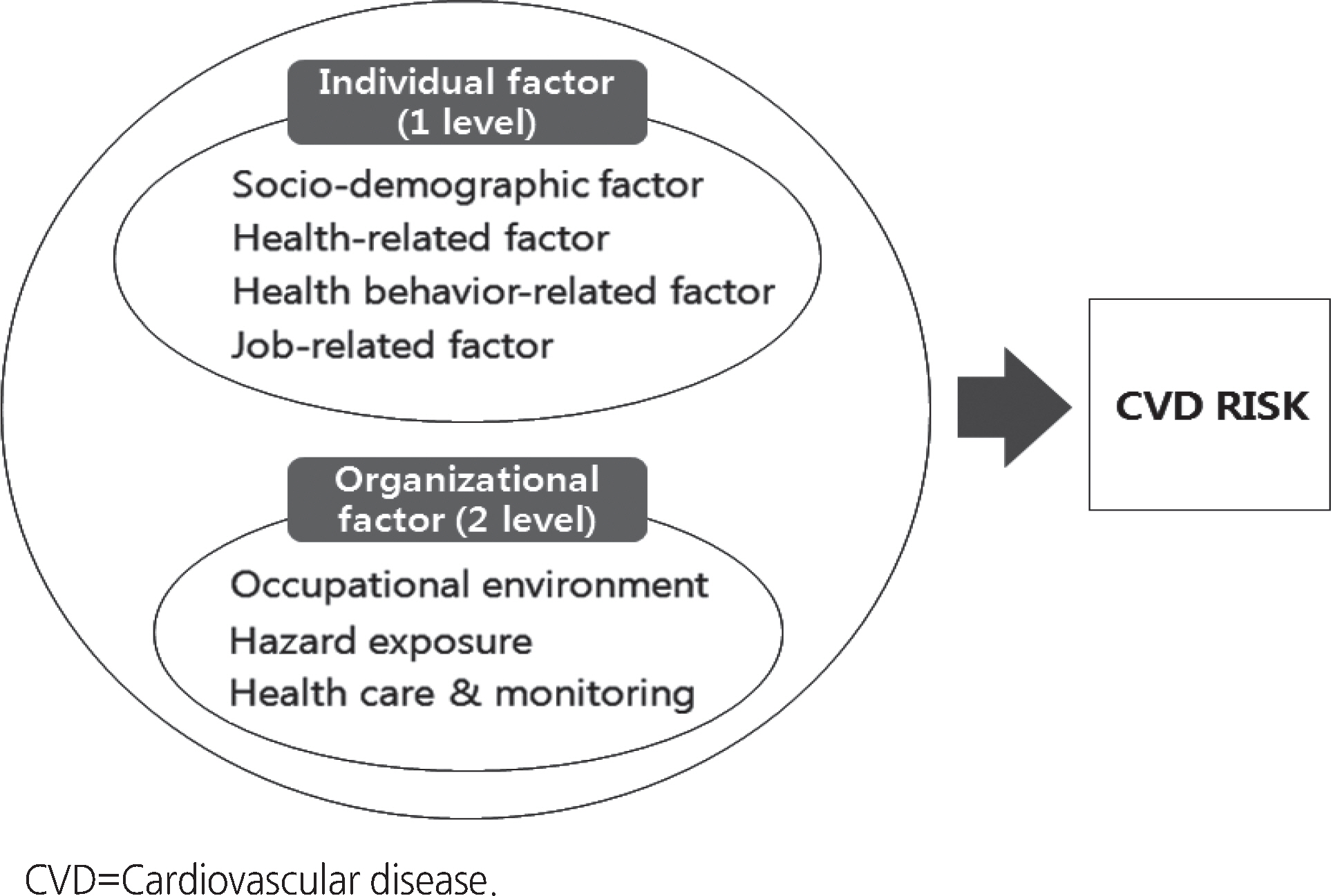
Figure 1.
| Variables | Total (N=492) |
Male (n=215) |
Female (n=277) |
|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | n (%) or M±SD | |
| CVD risk | 5.58±5.27 | 8.01±6.52 | 3.70±2.88 |
| Low risk | 421 (85.6) | 159 (74.0) | 262 (94.6) |
| Intermediate risk | 57 (11.6) | 42 (19.5) | 15 (5.4) |
| High risk | 14 (2.8) | 14 (6.5) | 0 (0.0) |
| Variables | Characteristics | Categories | n (%) or M±SD | CVD Risk | t or F | p |
|---|---|---|---|---|---|---|
| Socio-demographic | Age (yr) | 43.95±9.80 | 0.47* | <.001 | ||
| factors | Gender | Male | 215 (43.7) | 8.01±6.52 | 9.03 | <.001 |
| Female | 277 (56.3) | 3.70±2.88 | ||||
| Marital status | Single | 107 (21.7) | 4.08±3.88 | 8.50† | <.001 | |
| Married | 349 (71.0) | 5.86±5.24 | ||||
| Divorce or bereaved | 36 (7.3) | 7.38±7.73 | ||||
| Monthly income (10,000 KRW) | 294.27±133.85 | 0.09* | .037 | |||
| Education level | ≤Middle school | 86 (17.5) | 7.51±6.73 | 5.11† | .007 | |
| Highschool | 320 (65.0) | 5.29±4.79 | ||||
| ≥College | 86 (17.5) | 4.72±4.92 | ||||
| Health-related factors | Health status | 2.78±0.78 | 0.14 | .002 | ||
| Disease history | No | 426 (86.6) | 5.44±5.03 | − 1.22 | .225 | |
| Yes | 66 (13.4) | 6.48±6.61 | ||||
| CVD-related family history | No | 368 (74.8) | 5.49±5.22 | − 0.68 | .496 | |
| Yes | 124 (25.2) | 5.86±5.45 | ||||
| Hypertension history | No | 444 (90.2) | 4.95±4.58 | − 5.80 | <.001 | |
| Yes | 48 (9.8) | 11.14±7.39 | ||||
| DM history | No | 485 (97.4) | 5.25±4.80 | − 6.05 | <.001 | |
| Yes | 13 (2.6) | 17.75±7.41 | ||||
| BMI | Underweight | 16 (3.3) | 4.46±5.04 | 1.42† | .253 | |
| Normal | 333 (67.7) | 5.35±5.29 | ||||
| Overweight | 126 (25.6) | 6.01±5.15 | ||||
| Obesity | 17 (3.4) | 7.48±5.57 | ||||
| Health behavior-related factors | Physical activity‡ | Low | 163 (33.8) | 5.14±4.88 | 0.84 | .433 |
| Moderate | 187 (38.8) | 5.81±5.75 | ||||
| High | 132 (27.4) | 5.80±5.03 | ||||
| Healthy eating | 18.38±5.09 | 0.02* | .737 | |||
| Smoking | No | 378 (76.8) | 4.30±3.74 | − 7.91 | <.001 | |
| Yes | 114 (23.2) | 9.73±7.10 | ||||
| Binge drink | No | 346 (70.3) | 4.90±4.50 | − 3.83 | <.001 | |
| Yes | 146 (29.7) | 7.13±6.50 | ||||
| Job-related factors | Overtime work (hrs) | ≤60 | 419 (85.2) | 5.41±5.24 | − 1.74 | .082 |
| > 60 | 73 (14.8) | 6.57±5.40 | ||||
| Shift work§ | No | 443 (93.1) | 5.63±5.44 | 1.33 | .191 | |
| Yes | 33 (6.9) | 4.86±2.98 |
| Variables | Characteristics | Categories | Organizations |
Workers |
CVD risk |
t | p |
|---|---|---|---|---|---|---|---|
| n (%) or M±SD | n (%) or M±SD | M± SD | |||||
| Occupational | Number of employee | 76.87± 73.08 | − 0.27 |
.145 | |||
| environment | Having cafeteria in | No | 10 (32.3) | 62 (12.6) | 5.44±5.32 | − 1.61 | .090 |
| workplace | Yes | 21 (67.7) | 430 (87.4) | 6.58±4.88 | |||
| Having resting area in | No | 18 (58.1) | 461 (93.7) | 6.60±3.41 | 1.96 | .050 | |
| workplace | Yes | 13 (41.9) | 31 (6.3) | 5.04±1.39 | |||
| Hazard exposure | Chemical hazard exposure | No | 29 (93.5) | 440 (89.4) | 5.80±3.57 | − 0.74 | .581 |
| Yes | 2 (6.5) | 52 (10.6) | 6.54±3.01 | ||||
| Noise exposure | No | 19 (61.3) | 258 (52.4) | 5.06±4.79 | − 2.30 | .022 | |
| Yes | 12 (38.7) | 234 (47.6) | 6.16±5.71 | ||||
| Health care & | Managed by occupational | No | 13 (41.9) | 221 (44.9) | 6.20±5.86 | 2.31 | .021 |
| monitoring | health nurse | Yes | 18 (58.1) | 271 (55.1) | 5.08±4.68 |
| Parameter | Categories | Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|---|---|
| Null model |
Individual model |
Individual-organizational model | ||||||
| β | p | β | p | β | p | |||
| Fixed effect | Level 1 | Intercept | 6.03 | < .001 | 8.48 | <.001 | 8.09 | <.001 |
| Female (ref: Man) | − 5.94 | <.001 | − 6.16 | <.001 | ||||
| Married (ref: Single) | 3.36 | <.001 | 3.38 | <.001 | ||||
| Divorced/separated (ref: Single) | 4.46 | <.001 | 4.46 | <.001 | ||||
| Highschool education (ref: Middle school) | − 2.45 | <.001 | − 2.58 | <.001 | ||||
| College education (ref: Middle school) | − 3.98 | <.001 | − 4.06 | <.001 | ||||
| Overtime work | 0.53 | .399 | 0.34 | .590 | ||||
| Binge drinking | 0.11 | .822 | 0.10 | .834 | ||||
| Level 2 | Having resting area | − 0.50 | .619 | |||||
| Noise exposure | − 0.08 | .886 | ||||||
| Managed by occupational health nurse | − 0.80 | .164 | ||||||
| Having cafeteria in workplace | 1.81 | .022 | ||||||
| Random effect | Level 1, δ2 | 23.72 | 18.29 | 18.10 | ||||
| Level 2, μ0 (τ) | 4.89 | 1.02 | 0.65 | |||||
| χ2 | 36.53 | 4.01 | 2.25 | |||||
| p | <.001 | .023 | .066 | |||||
| ICC (%) | 17.10 | 5.31 | 3.45 | |||||
CVD=Cardiovascular disease; CVD Risk=10~year likelihood of developing CVD by Framingham risk score.
*Spearman's correlation coefficient; †Welch estimate coefficient; ‡n=482, excluded cases by analysis; §n=476, excluded cases by analysis; CVD Risk=10-year likelihood of developing CVD by Framingham risk score; PA=Physical activity; SB=Sedentary behavior; KRW=Korean won.
Spearman’s correlation coefficient; CVD Risk=10~year likelihood of developing CVD by Framingham risk score.
CVD Risk=10-year likelihood of developing CVD by Framingham risk score; ICC=Intra-class correlation coefficient; t: variance of μ0j.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

