Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 44(2); 2014 > Article
-
Original Article
- Outcomes of Home Monitoring after Palliative Cardiac Surgery in Infants with Congenital Heart Disease
- Sang Wha Kim, Ju-Yeon Uhm, Yu Mi Im, Tae-Jin Yun, Jeong-Jun Park, Chun Soo Park
-
Journal of Korean Academy of Nursing 2014;44(2):228-236.
DOI: https://doi.org/10.4040/jkan.2014.44.2.228
Published online: April 30, 2014
1Department of Nursing, Asan Medical Center, Seoul, Korea.
2College of Medicine, Ulsan University, Seoul, Korea.
- Address reprint requests to: Uhm, Ju-Yeon. Department of Nursing, Asan Medical Center, 88 Olympic-ro, 43-gil, Songpa-gu, Seoul 138-736, Korea. Tel: +82-10-2571-2137, Fax: +82-2-3010-6108, jyuhm@amc.seoul.kr
© 2014 Korean Society of Nursing Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0/) If the original work is properly cited and retained without any modification or reproduction, it can be used and re-distributed in any format and medium.
Abstract
-
Purpose
- Common conditions, such as dehydration or respiratory infection can aggravate hypoxia and are associated with interstage mortality in infants who have undergone palliative surgery for congenital heart diseases. This study was done to evaluate the efficacy of a home monitoring program (HMP) in decreasing infant mortality.
-
Methods
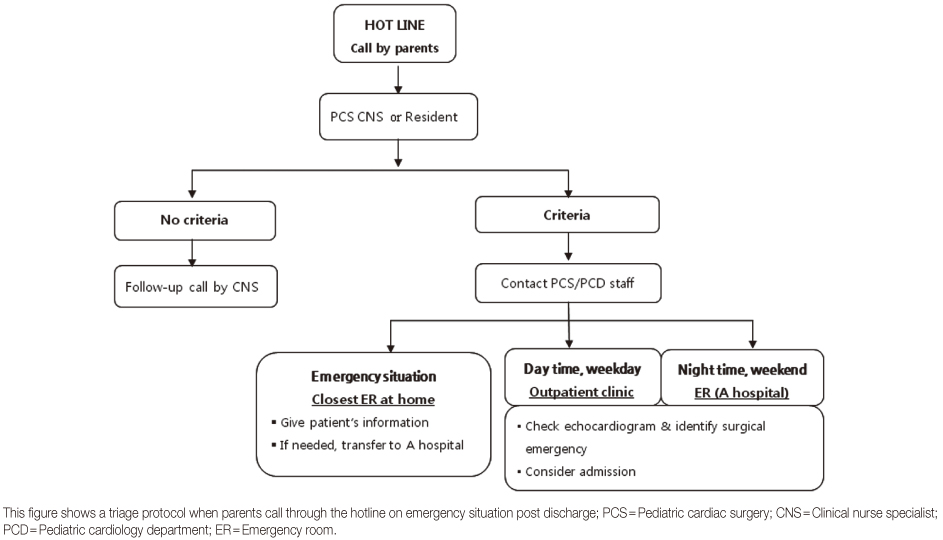
- Since its inception in May 2010, all infants who have undergone palliative surgery have been enrolled in HMP. This study was a prospective observational study and infant outcomes during HMP were compared with those of previous comparison groups. Parents were trained to measure oxygen saturation, body weight and feeding volume and to contact the hospital through the hotline for emergency situations. Telephone counseling was conducted by clinical nurse specialists every week post discharge.
-
Results
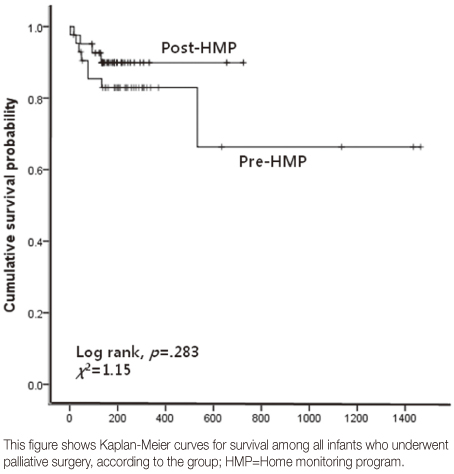
- Forty-one infants were enrolled in HMP. Nine hundred telephone counseling sessions were conducted. Seventy-three infants required telephone triage with the most common conditions being gastrointestinal (50.7%) and respiratory symptoms (32.9%). With HMP intervention, interstage mortality decreased from 18.6% (8/43) to 9.8% (4/41) (χ2=1.15, p=.283).
-
Conclusion
- Results indicate that active measures and treatments using the HMP decrease mortality rates, however further investigation is required to identify various factors that contribute to hemodynamic complications during the interstage period.
- 1. McElhinney DB, Wernovsky G. Outcomes of neonates with congenital heart disease. Curr Opin Pediatr. 2001;13(2):104–110.ArticlePubMed
- 2. Fricke TA, d'Udekem Y, Richardson M, Thuys C, Dronavalli M, Ramsay JM, et al. Outcomes of the arterial switch operation for transposition of the great arteries: 25 years of experience. Ann Thorac Surg. 2012;94(1):139–145. http://dx.doi.org/10.1016/j.athoracsur.2012.03.019ArticlePubMed
- 3. Kobayashi M, Ando M, Wada N, Takahashi Y. Outcomes following surgical repair of aortic arch obstructions with associated cardiac anomalies. Eur J Cardiothorac Surg. 2009;35(4):565–568. http://dx.doi.org/10.1016/j.ejcts.2008.09.052ArticlePubMed
- 4. Rodefeld MD, Ruzmetov M, Schamberger MS, Girod DA, Turrentine MW, Brown JW. Staged surgical repair of functional single ventricle in infants with unobstructed pulmonary blood flow. Eur J Cardiothorac Surg. 2005;27(6):949–955. http://dx.doi.org/10.1016/j.ejcts.2005.01.066ArticlePubMed
- 5. Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, et al. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362(21):1980–1992. http://dx.doi.org/10.1056/NEJMoa0912461PubMedPMC
- 6. Lee JR, Choi JS, Kang CH, Bae EJ, Kim YJ, Rho JR. Surgical results of patients with a functional single ventricle. Eur J Cardiothorac Surg. 2003;24(5):716–722.ArticlePubMed
- 7. Hehir DA, Dominguez TE, Ballweg JA, Ravishankar C, Marino BS, Bird GL, et al. Risk factors for interstage death after stage 1 reconstruction of hypoplastic left heart syndrome and variants. J Thorac Cardiovasc Surg. 2008;136(1):94–99. 99.e1–99.e3. http://dx.doi.org/10.1016/j.jtcvs.2007.12.012ArticlePubMed
- 8. Mahle WT, Spray TL, Wernovsky G, Gaynor JW, Clark BJ 3rd. Survival after reconstructive surgery for hypoplastic left heart syndrome: A 15-year experience from a single institution. Circulation. 2000;102:19 Suppl 3. III136–III141.ArticlePubMed
- 9. Gedicke M, Morgan G, Parry A, Martin R, Tulloh R. Risk factors for acute shunt blockage in children after modified Blalock-Taussig shunt operations. Heart Vessels. 2010;25(5):405–409. http://dx.doi.org/10.1007/s00380-009-1219-1ArticlePubMedPDF
- 10. Mackie AS, Gauvreau K, Newburger JW, Mayer JE, Erickson LC. Risk factors for readmission after neonatal cardiac surgery. Ann Thorac Surg. 2004;78(6):1972–1978. http://dx.doi.org/10.1016/j.athoracsur.2004.05.047ArticlePubMed
- 11. Ghanayem NS, Hoffman GM, Mussatto KA, Frommelt MA, Cava JR, Mitchell ME, et al. Perioperative monitoring in high-risk infants after stage 1 palliation of univentricular congenital heart disease. J Thorac Cardiovasc Surg. 2010;140(4):857–863. http://dx.doi.org/10.1016/j.jtcvs.2010.05.002ArticlePubMed
- 12. Kelleher DK, Laussen P, Teixeira-Pinto A, Duggan C. Growth and correlates of nutritional status among infants with hypoplastic left heart syndrome (HLHS) after stage 1 Norwood procedure. Nutrition. 2006;22(3):237–244. http://dx.doi.org/10.1016/j.nut.2005.06.008ArticlePubMed
- 13. Davis D, Davis S, Cotman K, Worley S, Londrico D, Kenny D, et al. Feeding difficulties and growth delay in children with hypoplastic left heart syndrome versus d-transposition of the great arteries. Pediatr Cardiol. 2008;29(2):328–333. http://dx.doi.org/10.1007/s00246-007-9027-9ArticlePubMedPDF
- 14. Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;8:CD007228. http://dx.doi.org/10.1002/14651858.CD007228.pub2Article
- 15. Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, et al. Home telemonitoring for congestive heart failure: A systematic review and meta-analysis. J Telemed Telecare. 2010;16(2):68–76. http://dx.doi.org/10.1258/jtt.2009.090406ArticlePubMedPDF
- 16. McCrossan BA, Grant B, Morgan GJ, Sands AJ, Craig B, Casey FA. Home support for children with complex congenital heart disease using videoconferencing via broadband: Initial results. J Telemed Telecare. 2008;14(3):140–142. http://dx.doi.org/10.1258/jtt.2008.003012ArticlePubMedPDF
- 17. Morgan GJ, Craig B, Grant B, Sands A, Doherty N, Casey F. Home videoconferencing for patients with severe congential heart disease following discharge. Congenit Heart Dis. 2008;3(5):317–324. http://dx.doi.org/10.1111/j.1747-0803.2008.00205.xArticlePubMed
- 18. Ghanayem NS, Hoffman GM, Mussatto KA, Cava JR, Frommelt PC, Rudd NA, et al. Home surveillance program prevents interstage mortality after the Norwood procedure. J Thorac Cardiovasc Surg. 2003;126(5):1367–1377. http://dx.doi.org/10.1016/s0022ArticlePubMed
- 19. Furck AK, Uebing A, Hansen JH, Scheewe J, Jung O, Fischer G, et al. Outcome of the Norwood operation in patients with hypoplastic left heart syndrome: A 12-year single-center survey. J Thorac Cardiovasc Surg. 2010;139(2):359–365. http://dx.doi.org/10.1016/j.jtcvs.2009.07.063ArticlePubMed
- 20. Srinivasan C, Sachdeva R, Morrow WR, Gossett J, Chipman CW, Imamura M, et al. Standardized management improves outcomes after the Norwood procedure. Congenit Heart Dis. 2009;4(5):329–337. http://dx.doi.org/10.1111/j.1747-0803.2009.00323.xArticlePubMed
- 21. Yun EK, Park HA. Strategy development for the implementation of telenursing in Korea. Comput Inform Nurs. 2007;25(5):301–306. http://dx.doi.org/10.1097/01.NCN.0000289167.38992.4bArticlePubMed
- 22. Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999;281(7):613–620.ArticlePubMed
- 23. Bergman K, Perhed U, Eriksson I, Lindblad U, Fagerström L. Patients' satisfaction with the care offered by advanced practice nurses: A new role in Swedish primary care. Int J Nurs Pract. 2013;19(3):326–333. http://dx.doi.org/10.1111/ijn.12072PubMed
- 24. Purc-Stephenson RJ, Thrasher C. Patient compliance with telephone triage recommendations: A meta-analytic review. Patient Educ Couns. 2012;87(2):135–142. http://dx.doi.org/10.1016/j.pec.2011.08.019ArticlePubMed
- 25. Smith K. Telephone health care: It's more than just a phone call. Pediatr Nurs. 1999;25(4):423–429.PubMed
- 26. Nauright LP, Moneyham L, Williamson J. Telephone triage and consultation: An emerging role for nurses. Nurs Outlook. 1999;47(5):219–226.ArticlePubMed
- 27. Polaschek L, Polaschek N. Solution-focused conversations: A new therapeutic strategy in well child health nursing telephone consultations. J Adv Nurs. 2007;59(2):111–119. http://dx.doi.org/10.1111/j.1365-2648.2007.04314.xArticlePubMed
- 28. Delgado-Passler P, McCaffrey R. The influences of postdischarge management by nurse practitioners on hospital readmission for heart failure. J Am Acad Nurse Pract. 2006;18(4):154–160. http://dx.doi.org/10.1111/j.1745-7599.2006.00113.xArticlePubMed
- 29. Dobrolet NC, Nieves JA, Welch EM, Khan D, Rossi AF, Burke RP, et al. New approach to interstage care for palliated high-risk patients with congenital heart disease. J Thorac Cardiovasc Surg. 2011;142(4):855–860. http://dx.doi.org/10.1016/j.jtcvs.2011.01.054ArticlePubMed
REFERENCES
Figure & Data
REFERENCES
Citations

- Preoperative Home Monitoring for Neonates and Young Infants With Tetralogy of Fallot
Yu-Mi Im, Jung A Kim, Su-Jin Kwon, Dong-Hee Kim, Tae-Jin Yun
Journal of Cardiovascular Nursing.2026; 41(1): 59. CrossRef - Association of nurse–mother partnerships with parenting stress and family resilience among South Korean mothers of children with congenital heart disease
Youna Chang, Jiyoung Lim, Hye Won Yoon
Journal of Pediatric Nursing.2024; 79: 16. CrossRef - High-risk obstetrical call center: a model for regions with limited access to care
Sarah J. Rhoads, Hari Eswaran, Christian E. Lynch, Songthip T. Ounpraseuth, Everett F. Magann, Curtis L. Lowery
The Journal of Maternal-Fetal & Neonatal Medicine.2018; 31(7): 857. CrossRef
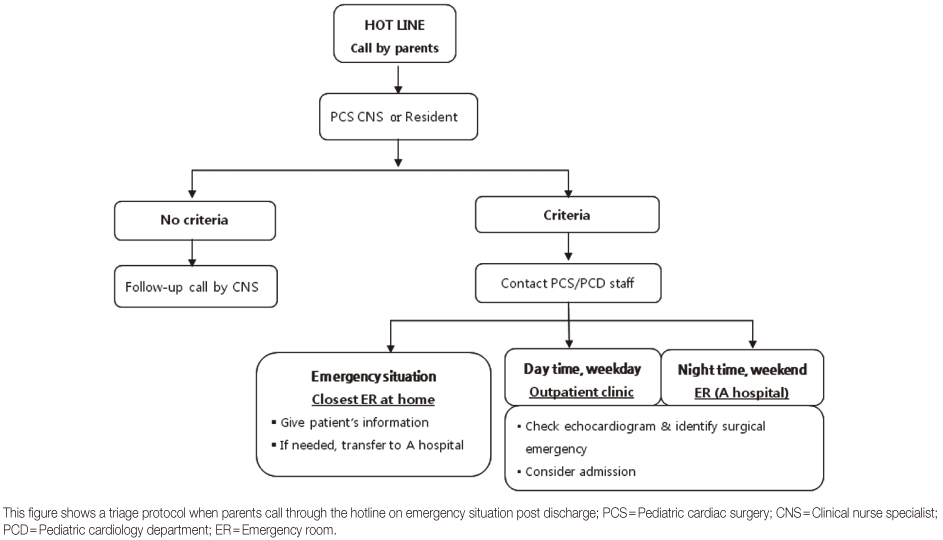
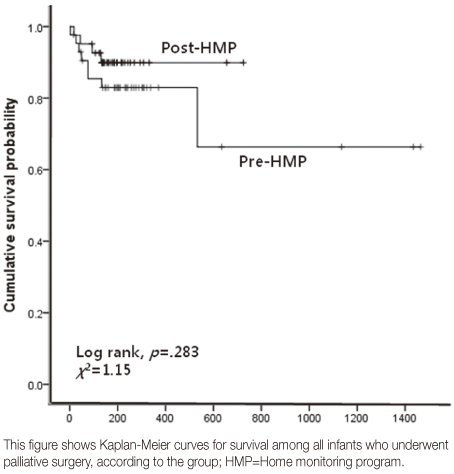
Figure 1
Figure 2
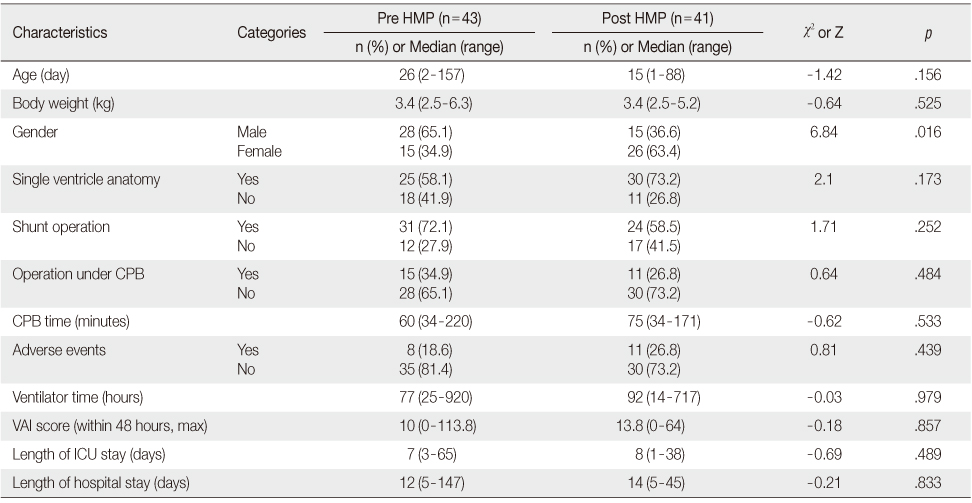
Homogeneity Test for General Characteristics of Infants (N=84)
HMP=Home monitoring program; CPB=Cardiopulmonary bypass; ICU=Intensive care unit; VAI=Vasoactive inotropes.
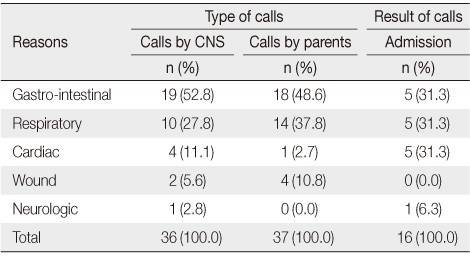
Reasons for Calling Telephone Health Care Services about Infant Health Problems and Frequency of Admission in Post HMP Group (N=41)
HMP=Home monitoring program; CNS=Clinical nurse specialist.
HMP=Home monitoring program; CPB=Cardiopulmonary bypass; ICU=Intensive care unit; VAI=Vasoactive inotropes.
HMP=Home monitoring program; CNS=Clinical nurse specialist.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

