Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 43(3); 2013 > Article
-
Original Article
- Effects of Tai Chi on Fall Risk Factors: A Meta-Analysis
- Moonkyoung Park, Rhayun Song
-
Journal of Korean Academy of Nursing 2013;43(3):341-351.
DOI: https://doi.org/10.4040/jkan.2013.43.3.341
Published online: June 28, 2013
College of Nursing, Chungnam National University, Daejeon, Korea.
- Address reprint requests to: Song, Rhayun. College of Nursing, Chungnam National University, 266 Munhwa-ro, Jung-gu, Daejeon 301-747, Korea. Tel: +82-42-580-8331, Fax: +82-42-580-8309, songry@cnu.ac.kr
© 2013 Korean Society of Nursing Science
Abstract
-
Purpose
- This study was done to analyze the effects of Tai Chi on fall-related risk factors through meta-analysis of randomized clinical trials published in English and Korean between 2000 and 2010.
-
Methods
- Using health related database and hand search of references and Google, 28 randomized studies were collected from doctoral dissertation and published peer reviewed articles. The Comprehensive Meta-analysis version 2.0 was used for the analysis.
-
Results
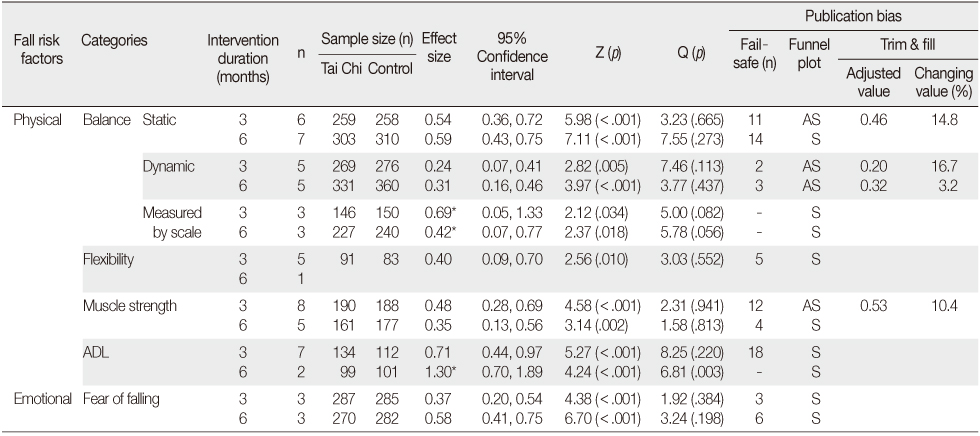
- The effect sizes for Tai Chi for 3 months were significant with ES=0.54 for static balance, ES=0.24 for dynamic balance, ES=0.69 for balance measured by scale, and ES=0.40 for flexibility, ES=0.48 for muscle strength, ES=0.71 for ADL, and ES=0.37 for fear of falling. Also, the effect sizes of Tai Chi for 6 months were significant for most fall-related variables. The 6 month data for flexibility was not analyzed since only one study was published.
-
Conclusion
- The analysis of studies of randomized clinical trials indicate that Tai Chi is effective in improving balance, flexibility, muscle strength, activities of daily living, and fear of falling when applied for 3 or 6 months. The findings provide the objective evidence to apply Tai Chi as a fall preventive intervention.
This manuscript is a condensed form of the first author's doctoral dissertation from Chungnam National University.
This study was supported by the research assistance fund of Korean Society of Adult Nursing in 2010.
- 1. American Geriatrics Society, British Geriatrics Society. American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49(5):664–672.ArticlePubMed
- 2. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester, WS: Wiley; 2009.
- 3. Carter ND, Kannus P, Khan KM. Exercise in the prevention of falls in older people: A systematic literature review examining the rationale and the evidence. Sports Med. 2001;31(6):427–438.PubMed
- 4. Choi JH, Lee EO, Lee HY, Eun Y. Analysis of the effects of Tai Chi on muscle strength and flexibility. J Rheumatol Health. 2005;12(1):69–80.
- 5. Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Academic Press; 1977.
- 6. Erim Z, Beg MF, Burke DT, de Luca CJ. Effects of aging on motor-unit control properties. J Neurophysiol. 1999;82(5):2081–2091.ArticlePubMed
- 7. Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57(3):407–414. http://dx.doi.org/10.1002/art.22621ArticlePubMed
- 8. Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. http://dx.doi.org/10.1002/14651858.CD007146.pub3Article
- 9. Glass GV. Primary, secondary, and meta-analysis of research. Educ Res. 1976;5(10):3–8.ArticlePDF
- 10. Harling A, Sompson JP. A systematic review to determine the effectiveness of Tai Chi in reducing falls and fear of falling in older adults. Phys Ther Rev. 2008;13(4):237–248.Article
- 11. Health Insurance Review & Assessment Service. 2011 statistics indicators of medical expenses. 2012;Retrieved December 26, 2012. from http://www.hira.or.kr/dummy.do?pgmid=HIRAA020045030000&cmsurl=/cms/information/05/03/03/1214408_13609.html&subject=2011%eb%85%84+%ec%9d%98%eb%a3%8c%ea%b8%89%ec%97%ac+%ec%a7%84%eb%a3%8c%eb%b9%84+%ed%86%b5%ea%b3%84%ec%a7%80%ed%91%9c
- 12. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions: Cochrane book series. Chichester, WS: John Wiley & Sons Ltd; 2008.
- 13. Lam P. A handbook for Tai Chi for arthritis. Narwee: East Acton Publishing; 2000.
- 14. Lee YJ. The effects of Tai Chi exercise program using transtheoretical model applied to degressive arthritis patients. Seoul, Hanyang University. 2008;Unpublished doctoral dissertation.
- 15. Liu B, Liu ZH, Zhu HE, Mo JC, Cheng DH. Effects of tai chi on lower-limb myodynamia in the elderly people: A meta-analysis. J Tradit Chin Med. 2011;31(2):141–146.ArticlePubMed
- 16. Logghe IH, Verhagen AP, Rademaker AC, Bierma-Zeinstra SM, van Rossum E, Faber MJ, et al. The effects of Tai Chi on fall prevention, fear of falling and balance in older people: A meta-analysis. Prev Med. 2010;51(3-4):222–227. http://dx.doi.org/10.1016/j.ypmed.2010.06.003ArticlePubMed
- 17. Low S, Ang LW, Goh KS, Chew SK. A systematic review of the effectiveness of Tai Chi on fall reduction among the elderly. Arch Gerontol Geriatr. 2009;48(3):325–331. http://dx.doi.org/10.1016/j.archger.2008.02.018ArticlePubMed
- 18. Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: A prospective study. J Gerontol A Biol Sci Med Sci. 2006;61(8):866–870.ArticlePubMed
- 19. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. http://dx.doi.org/10.1371/journal.pmed.1000097ArticlePubMedPMC
- 20. Orwin RG. A fail-safe N for effect size in meta-analysis. J Educ Stat. 1983;8(2):157–159.ArticlePDF
- 21. Rand D, Miller WC, Yiu J, Eng JJ. Interventions for addressing low balance confidence in older adults: A systematic review and meta-analysis. Age Ageing. 2011;40(3):297–306. http://dx.doi.org/10.1093/ageing/afr037ArticlePubMed
- 22. Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis, prevention, assessment and adjustments. New York, NY: John Wiley and Sons Ltd; 2005.
- 23. Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24. http://dx.doi.org/10.1093/ageing/afm169ArticlePubMed
- 24. Scottish Intercollegiate Guidelines Network. SIGN 50; A guideline developer's handbook. 2008;Retrieved July 1, 2010. from http://www.sign.ac.uk/guidelines/fulltext/50/
- 25. Song R, Lee EO, Lam P, Bae SC. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: A randomized clinical trial. J Rheumatol. 2003;30(9):2039–2044.PubMed
- 26. Stump TE, Clark DO, Johnson RJ, Wolinsky FD. The structure of health status among Hispanic, African American, and white older adults. J Gerontol B Psychol Sci Soc Sci. 1997;52(Spec No):49–60.ArticlePubMed
- 27. Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ. 2000;320(7249):1574–1577.ArticlePubMedPMC
- 28. Tideiksaar R. Falls in older people: Prevention and management. 3rd ed. Baltimore, MD: Health Professions Press; 2002.
- 29. Wooton AC. An integrative review of Tai Chi research: An alternative form of physical activity to improve balance and prevent falls in older adults. Orthop Nurs. 2010;29(2):108–116. quiz 117-108. http://dx.doi.org/10.1097/NOR.0b013e3181d243b3PubMed
- 30. World Health Organization. Falls. 2012;Retrieved November 26, 2012. from http://www.who.int/mediacentre/factsheets/fs344/en/
REFERENCES
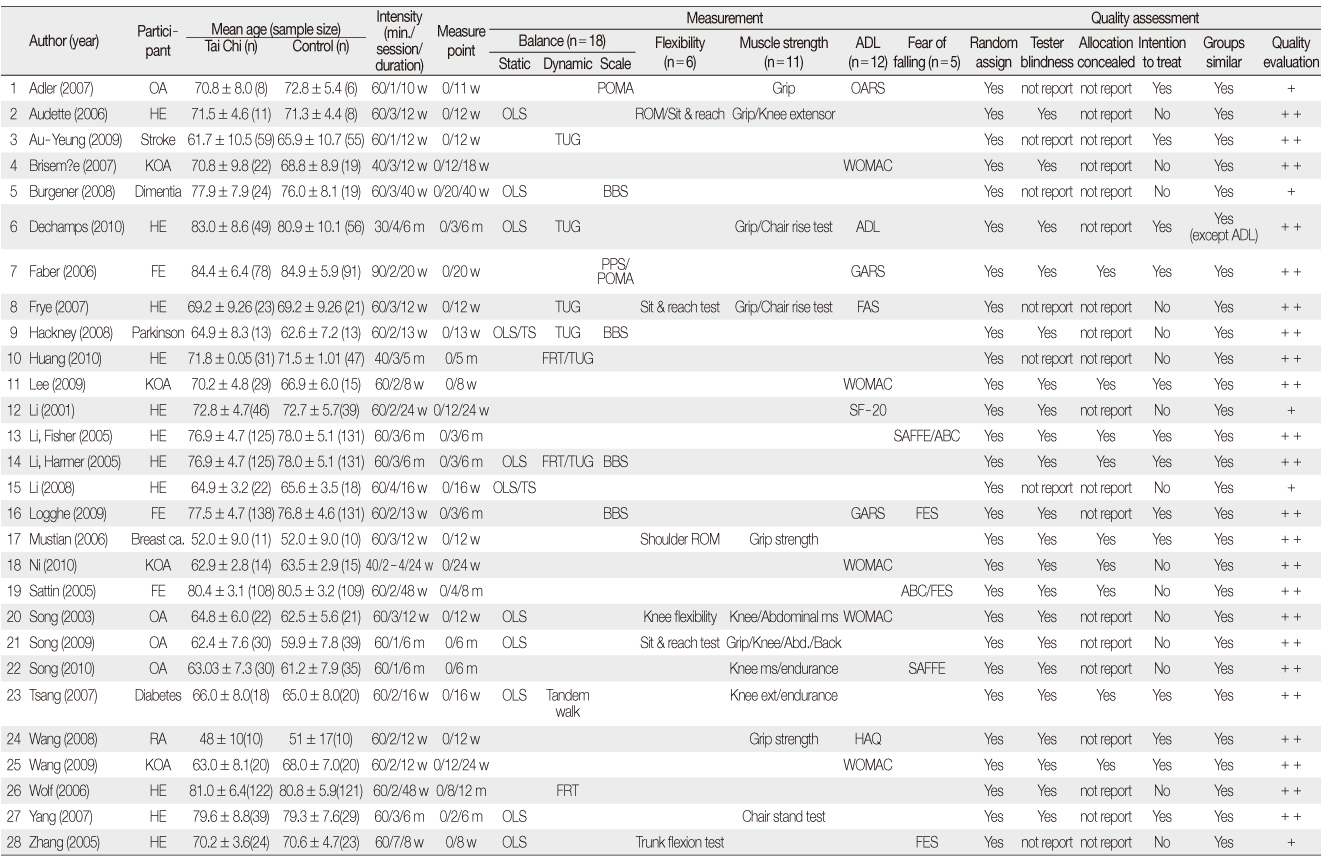
FE=Frail elderly; HE=Healthy elderly; OA=Osteoarthritis; AS=Ankylosing spondylitis; BBS=Berg balance scale; FRT=Functional reach test; OLS=One leg stance; POMA=Performance oriented mobility assessment; PPS=Physical performance scale; TS=Tandem stance; TUG=Timed up and go test; ROM=Range of motion; ADL=Activities of daily living; FAS=Functional ability scale; GARS=Groningen activity restriction scale; HAQ=Health assessment questionnaire; OARS=Older American resource survey; WOMAC=Western Ontario and McMaster University osteoarthritis index questionnaire; ABC=Activities-specific balance confidence scale; FES=Fall efficacy scale; SAFFE=Survey of activities and fear of falling in the elderly; MS=Muscle strength; Italic=No report about method of random assignment.
Figure & Data
REFERENCES
Citations

- Global research on Chinese martial arts (1974–2025): A bibliometric and visualization-based analysis using Web of Science
Wei Chen, Syahrul Ridhwan Morazuki
Medicine.2025; 104(32): e43769. CrossRef - Effects of Tai-Chi and Running Exercises on Cardiorespiratory Fitness and Biomarkers in Sedentary Middle-Aged Males: A 24-Week Supervised Training Study
Yi Wang, Xian Guo, Liangchao Liu, Minhao Xie, Wing-Kai Lam
Biology.2022; 11(3): 375. CrossRef - Mind-Body Therapies From Traditional Chinese Medicine: Evidence Map
Lissandra Zanovelo Fogaça, Caio Fabio Schlechta Portella, Ricardo Ghelman, Carmen Verônica Mendes Abdala, Mariana Cabral Schveitzer
Frontiers in Public Health.2021;[Epub] CrossRef - Tai Chi for improving balance and reducing falls: An overview of 14 systematic reviews
Dongling Zhong, Qiwei Xiao, Xili Xiao, Yuxi Li, Jing Ye, Lina Xia, Chi Zhang, Juan Li, Hui Zheng, Rongjiang Jin
Annals of Physical and Rehabilitation Medicine.2020; 63(6): 505. CrossRef - Exploring the Adaptability of Tai Chi to Stroke Rehabilitation
Inok Hwang, Rhayun Song, Sukhee Ahn, Myung-ah Lee, Peter M. Wayne, Min Kyun Sohn
Rehabilitation Nursing.2019; 44(4): 221. CrossRef - The association between Tai Chi exercise and safe driving performance among older adults: An observational study
Sally Miller, Ruth E. Taylor-Piliae
Journal of Sport and Health Science.2018; 7(1): 83. CrossRef - Adapting Tai Chi for Upper Limb Rehabilitation Post Stroke: A Feasibility Study
Shujuan Pan, Dahlia Kairy, Hélène Corriveau, Michel Tousignant
Medicines.2017; 4(4): 72. CrossRef - The Effects of Tai Chi Practice With Asynchronous Music on Compliance and Fall-Related Risk Factors in Middle-Aged and Older Women: A Pilot Study
Yan Du, Penny Roberts, Qingwen Xu
Journal of Holistic Nursing.2017; 35(2): 142. CrossRef - The Effects of Exercise Intervention for Fall Prevention in Persons with Arthritis: A Meta Analysis
Chun Hee Lee, Heeok Park
Korean Journal of Adult Nursing.2017; 29(6): 587. CrossRef - The correlation between white matter hyperintensity and balance disorder and fall risk: An observational, prospective cohort study
Dong‐Chao Shen, Shuo‐Lin Wu, Yu‐Zhi Shi, Shuo Wang, Yu‐Mei Zhang, Chun‐Xue Wang
Chronic Diseases and Translational Medicine.2016; 2(3): 173. CrossRef - Effects of Nursing Interventions for Fall Prevention in Hospitalized Patients: A Meta-analysis
Yoon Lee Kim, Seok Hee Jeong
Journal of Korean Academy of Nursing.2015; 45(4): 469. CrossRef - The effects of Tai‐Chi in conjunction with thera‐band resistance exercise on functional fitness and muscle strength among community‐based older people
Shu‐Fen Lin, Huei‐Chuan Sung, Tzai‐Li Li, Tsung‐Cheng Hsieh, Hsiao‐Chin Lan, Shoa‐Jen Perng, Graeme D. Smith
Journal of Clinical Nursing.2015; 24(9-10): 1357. CrossRef - Recent Literature
Focus on Alternative and Complementary Therapies.2014;[Epub] CrossRef
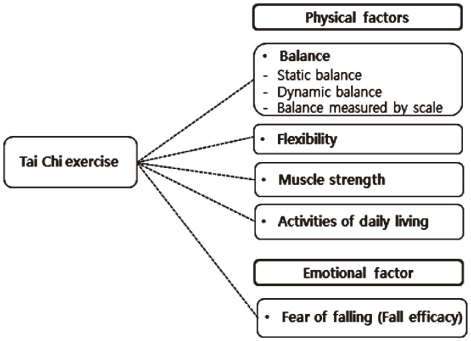
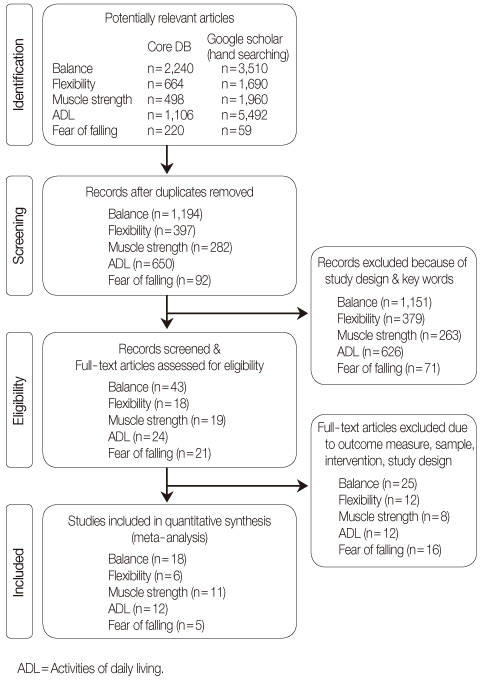
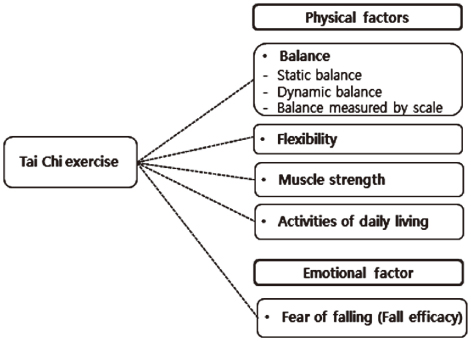
Figure 1
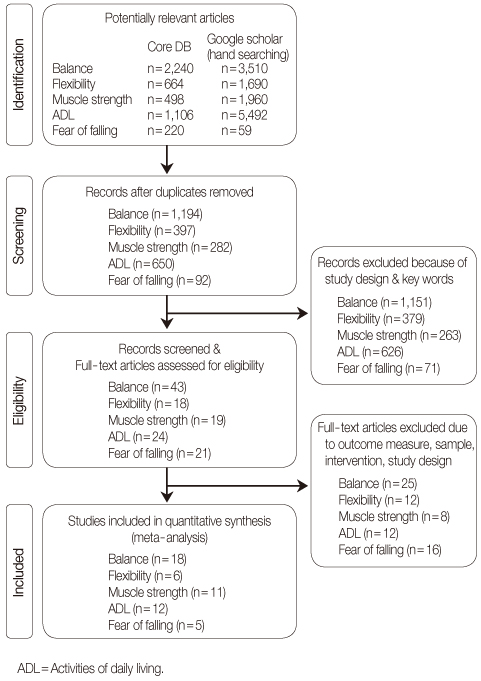
Figure 2
Characteristics of Included Studies in Meta-Analysis: Tai Chi for Fall Risk Factors
FE=Frail elderly; HE=Healthy elderly; OA=Osteoarthritis; AS=Ankylosing spondylitis; BBS=Berg balance scale; FRT=Functional reach test; OLS=One leg stance; POMA=Performance oriented mobility assessment; PPS=Physical performance scale; TS=Tandem stance; TUG=Timed up and go test; ROM=Range of motion; ADL=Activities of daily living; FAS=Functional ability scale; GARS=Groningen activity restriction scale; HAQ=Health assessment questionnaire; OARS=Older American resource survey; WOMAC=Western Ontario and McMaster University osteoarthritis index questionnaire; ABC=Activities-specific balance confidence scale; FES=Fall efficacy scale; SAFFE=Survey of activities and fear of falling in the elderly; MS=Muscle strength; Italic=No report about method of random assignment.
Effect Size of 3 and 6 Months Tai Chi Exercise for Fall Risk Factors
*Random effect model; AS=Asymmetric; S=Symmetric.
FE=Frail elderly; HE=Healthy elderly; OA=Osteoarthritis; AS=Ankylosing spondylitis; BBS=Berg balance scale; FRT=Functional reach test; OLS=One leg stance; POMA=Performance oriented mobility assessment; PPS=Physical performance scale; TS=Tandem stance; TUG=Timed up and go test; ROM=Range of motion; ADL=Activities of daily living; FAS=Functional ability scale; GARS=Groningen activity restriction scale; HAQ=Health assessment questionnaire; OARS=Older American resource survey; WOMAC=Western Ontario and McMaster University osteoarthritis index questionnaire; ABC=Activities-specific balance confidence scale; FES=Fall efficacy scale; SAFFE=Survey of activities and fear of falling in the elderly; MS=Muscle strength; Italic=No report about method of random assignment.
*Random effect model; AS=Asymmetric; S=Symmetric.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite