Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 40(3); 2010 > Article
-
Original Article
- The Effect of Pre-warming for Patients under Abdominal Surgery on Body Temperature, Anxiety, Pain, and Thermal Comfort
- Ok Bun Park, Heejung Choi
-
Journal of Korean Academy of Nursing 2010;40(3):317-325.
DOI: https://doi.org/10.4040/jkan.2010.40.3.317
Published online: June 30, 2010
1Head Nurse, Operation Room, Konkuk University Hospital, Seoul, Korea.
2Professor, Department of Nursing, Konkuk University, Chungju, Korea.
- Address reprint requests to: Park, Ok Bun. Operation Room, Konkuk University Hospital, 4-12 Hwayang-dong, Gwangjin-gu, Seoul 143-729, Korea. Tel: 82-2-2030-5463, Fax: 82-2-2030-5422, bada@kuh.ac.kr
Copyright © 2010 Korean Society of Nursing Science
Abstract
-
Purpose
- The purpose of this study was to examine the effect of pre-warming on body temperature, anxiety, pain, and thermal comfort.
-
Methods
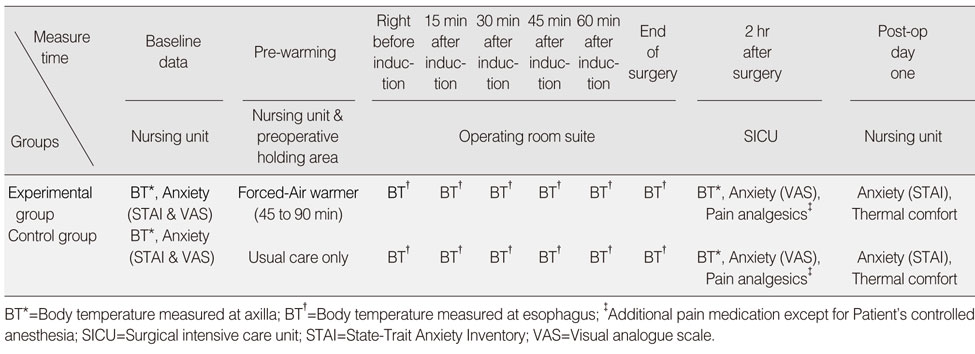
- Forty patients who were scheduled for abdominal surgery were recruited as study participants and were assigned to the experimental or control group. For the experimental group, a forced air warmer was applied for 45-90 min (M=68.25, SD=15.50) before surgery. Body temperature and anxiety were measured before and after the experiment, but pain and thermal comfort were assessed only after the surgery. Hypotheses were tested using t-test and repeated measured ANOVA.
-
Results
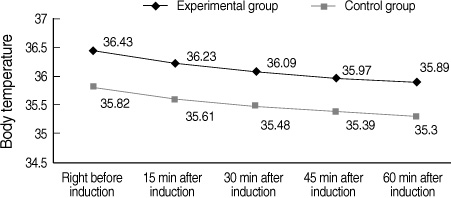
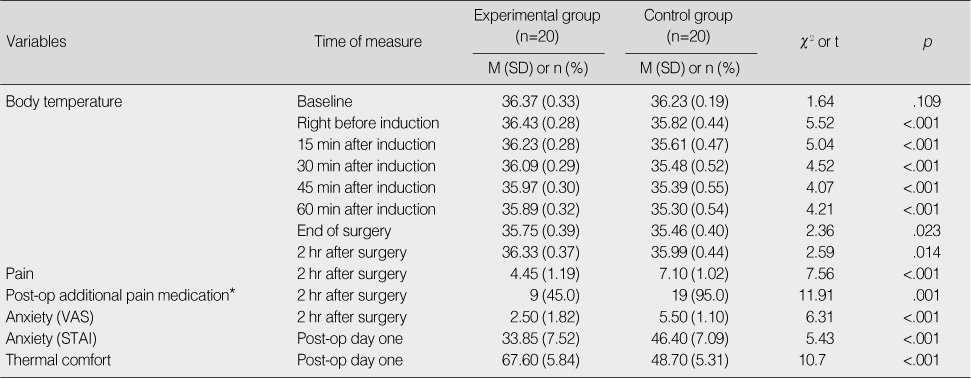
- The experimental group showed higher body temperature than the control group from right before induction to two hours after surgery. Post-operative anxiety and pain in the experimental group were less than those of the control group. In addition, the score of thermal comfort was significantly higher in the experiment group.
-
Conclusion
- Pre-warming is effective in maintaining body temperature, lowering sensitivity to pain and anxiety, and promoting thermal comfort. Therefore, pre-warming can be recommended as a preoperative nursing intervention.
- 1. Andrzejowski J, Hoyle J, Eapen G, Turnbull D. Effect of prewarming on post-induction core temperature and the incidence of inadvertent perioperative hypothermia in patients undergoing general anaesthesia. British Journal of Anaesthesia. 2008;101:627–631.ArticlePubMed
- 2. Berman A, Snyder S, Kozier B, Erb G. Kozier & Erb's fundamentals of nursing: Concepts, process, and practice. 2008;8th ed. Upper Saddle River, NJ, Prentice Hall Health.
- 3. Berti M, Casati A, Torri G, Aldegheri G, Lugani D, Fanelli G. Active warming, not passive heat retention, maitains normothermia during combined epidural-general anesthesia for hip and knee arthroplasty. Journal of Clinical Anesthesia. 1997;9:482–486.ArticlePubMed
- 4. Borms S, Engelen S, Himpe D, Suy C, Theunissen W. Bair hugger forced-air warming maintains normothermai more effectively than thermo-lite insulation. Journal of Clinical Anesthesia. 1994;6:303–307.ArticlePubMed
- 5. Camus Y, Delva E, Sessler D, Lienhart A. Pre-induction skin-surface warming minimizes intraoperative core hypotheria. Journal of Clinical Anesthesia. 1995;7:384–388.ArticlePubMed
- 6. Cooper S. The effect of preoperative warming on patients' postoperative temperatures. AORN Journal. 2006;83:1074–1076. 1079–1084.
- 7. Fanelli A, Danelli G, Ghisi D, Ortu A, Moschini E, Fanelli G. The efficacy of a resistive heating under-patient blanket versus a forced-air warming system: A randomized controlled trial. Anesthesia and Analgesia. 2009;108:199–201.ArticlePubMed
- 8. Fossum S, Hays J, Henson MM. A comparison study on the effects of prewarming patients in the outpatient surgery setting. Journal of Perianesthesia Nursing. 2001;16:187–194.ArticlePubMed
- 9. Insler SR, Sessler DI. Perioperative thermoregulation and temperature monitoring. Anesthesiology Clinics. 2006;24:823–837.ArticlePubMed
- 10. Kiekkas P, Karga M. Prewarming: Preventing intraoperative hypothermia. British Journal of Perioperative Nursing. 2005;15:444446–447. 449–451.ArticlePubMedPDF
- 11. Kim C, Baek W, Hong J, Park J, Kim B. Temperature changes during general anesthesia. Korean Journal of Anesthesiology. 1988;21:27–32.Article
- 12. Kim JY, Shinn H, Oh YJ, Hong YW, Kwak HJ, Kwak YL. The effect of skin surface warming during anesthesia preparation on preventing redistribution hypothermia in the early operative period of off-pump coronary artery bypass surgery. European Journal of Cardiothoracic Surgery. 2006;29:343–347.ArticlePubMed
- 13. Kolcaba K. Comfort theory and practice: A vision for holistic health care and research. 2003;New York, NY, Springer Publishing Co..
- 14. Lim S, Cho M, Choi K. The effect of preoperative warming on reducing rectal temperature drop in surgical patients. Journal of Korean Academy of Adult Nursing. 1997;9:55–69.
- 15. Murat I, Berniere J, Constant I. Evaluation of the efficacy of a forced-air wamer (Bair Hugger) during spinal surgery in children. Journal of Clinical Anesthesia. 1994;6:425–429.ArticlePubMed
- 16. Negishi C, Hasegawa K, Mukai S, Nakagawa F, Ozaki M, Sessler DI. Resistive-heating and forced-air warmingare comparably effective. Anesthesia and Analgesia. 2003;96:1683–1687.PubMed
- 17. Odom M. Maintaining intraoperative normothermia: Ameta-analysis of outcomes with costs. AANA Journal. 1999;67:155–164.PubMed
- 18. Putzu M, Casati A, Berti M, Pagliarini G, Fanelli G. Clinical complications, monitoring and management of perioperative mild hypothermia: Anesthesiological features. Acta Biomedica. 2007;78:163–169.PubMed
- 19. Robinson S, Benton G. Warm blankets. Geriatric Nursing. 2002;23:320–323.ArticlePubMed
- 20. Rose DK, Cohen MM, Soutter DI. Laparoscopic cholecystectomy: The anaesthetist's point of view. Canadian Journal of Anaesthesia. 1992;39:809–815.ArticlePubMedPDF
- 21. Sessler DI. Perioperative heat balance. Anesthesiology. 2000;92:578–596.ArticlePubMedPDF
- 22. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109:318–338.ArticlePubMedPDF
- 23. Spielberger C, Gorsuch R, Lushene R, Vagg P, Jacobs G. Manual for the state-trait anxiety inventory for adults. 1983;Palo Alto, CA, Consulting Psychologists Press.
- 24. Vanni SM, Braz JR, Modolo NS, Amorim RB, Rodrigues GR Jr. Preoperative combined with intraoperative skin-surface warming avoids hypothermia caused by generalanesthesia and surgery. Journal of Clinical Anesthesia. 2003;15:119–125.ArticlePubMed
- 25. Wagner D, Byrne M, Kolcaba K. Effects of comfort warming on preoperative patients. AORN Journal. 2006;84:427–448.ArticlePubMed
- 26. Wilson L, Kolcaba K. Practical application of comfort theory in the perianesthesia setting. Journal of Perianesthesia Nursing. 2004;19:164–173.ArticlePubMed
REFERENCES
Figure & Data
REFERENCES
Citations

- The Relationship of Perioperative Inadvertent Hypothermia with Anxiety and Comfort
Zehra Bozkurt, Özlem Şahin Akboğa
Therapeutic Hypothermia and Temperature Management.2025; 15(1): 31. CrossRef - Effects of Forced-Air Warming Blanket on Anxiety Reduction and Thermal Comfort Improvement With Physical Indicators for Patients Undergoing Abdominal Surgery: A Quasi-experimental Study
Shu-Mei Wang, Chung-Ying Lin, Musheer A. Aljaberi, Chiu-Hsiang Lee, Ying-Hsiang Chou, Mark D. Griffiths
Journal of PeriAnesthesia Nursing.2025; 40(5): 1300. CrossRef - Barriers and Solutions in Implementing Evidence-Based Recommendations to Prevent Intraoperative Inadvertent Hypothermia: A Qualitative Study
Ozlem Sahin Akboga, Yesım Dikmen Aydin
Therapeutic Hypothermia and Temperature Management.2024; 14(4): 282. CrossRef - Effects of Active Heating Methods on Body Temperature, Shivering, Thermal Comfort, Pain, Nausea and Vomiting During General Anesthesia: A Randomized Controlled Trial
Özlem Şahin Akboğa, Aysel Gürkan
Therapeutic Hypothermia and Temperature Management.2024; 14(4): 269. CrossRef - Effect of Active and Passive Heating Methods Used in Different Areas of Perioperative Processes on Thermal Comfort and Anxiety: A Randomized Control Trial
Pınar TUNÇ TUNA, Şerife KURŞUN, İnci KARA
Journal of Basic and Clinical Health Sciences.2022; 6(1): 225. CrossRef - Influence of Gas Pain, Post-operative Resilience, and Body Temperature Discomfort in Laparoscopic Myomectomy Patients after Thermotherapy
JeongAe Lee, MyoungHwa Jeon, EunJu Park, JinAh Lee, GonMyoung Ahn, SeungShin Lee, JiIn Kim
Korean Journal of Women Health Nursing.2019; 25(1): 4. CrossRef - Do Warmed Blankets Change Pain, Agitation, Mood or Analgesic Use Among Nursing Home Residents?
Christine R. Kovach, Michelle Putz, Barbara Guslek, Robert McInnes
Pain Management Nursing.2019; 20(6): 526. CrossRef - Forced-Air Warming for Rewarming and Comfort Following Laparoscopy: A Randomized Controlled Trail
Hsiao-Chi Nieh, Shu-Fen Su
Clinical Nursing Research.2018; 27(5): 540. CrossRef - Effects of Forced Air Warming on Body Temperature, Shivering and Pain in Laparoscopic Cholecystectomy Patients*
Sung Joo Park, Sook Young Kim
Journal of Korean Academy of Fundamentals of Nursing.2015; 22(3): 287. CrossRef - Evaluating of Validity on Peri-operative Hypothermia Management Evidence Based Guideline
Sung-Jung Hong, Eunjoo Lee
Journal of the Korea Academia-Industrial cooperation Society.2014; 15(1): 331. CrossRef - The Effect of Hand Holding and Nei-Guan Acupressure on Anxiety and Pain under Local Anesthetic Patients during Surgery
Sun Hee Park, Hee Jung Jang
The Journal of the Korea Contents Association.2014; 14(11): 378. CrossRef - Effects of ASPAN's Evidence-based Clinical Practice Guidelines for Promotion of Hypothermia of Patients with Total Knee Replacement Arthroplasty
Je Bog Yoo, Hyun Ju Park, Ji Yeoun Chae, Eun Ju Lee, Yoo Jung Shin, Justin Sangwook Ko, Nam Cho Kim
Journal of Korean Academy of Nursing.2013; 43(3): 352. CrossRef - Effect of Pre-warming on Reducing the Incidence of Inadvertent Peri-operative Hypothermia for Patients Undergoing General Anaesthesia: A Mini-review
Lucie Llewellyn
British Journal of Anaesthetic and Recovery Nursing.2013; 14(1-2): 3. CrossRef
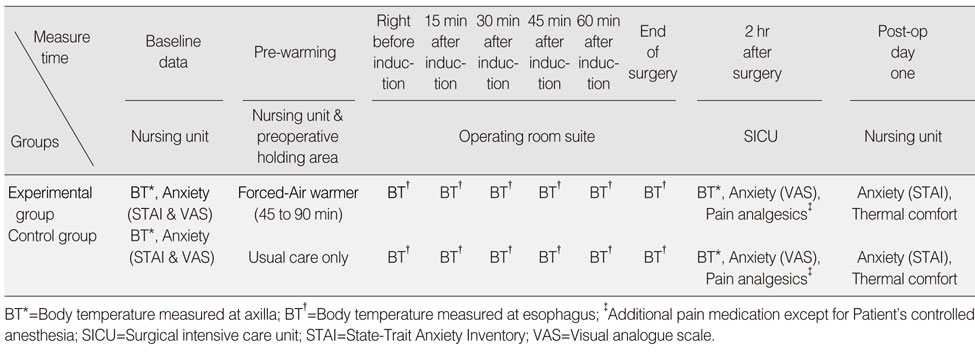
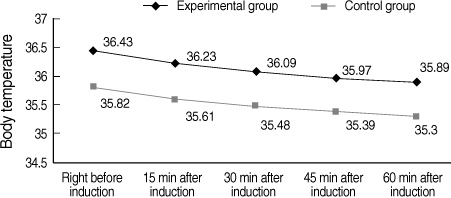
Figure 1
Figure 2
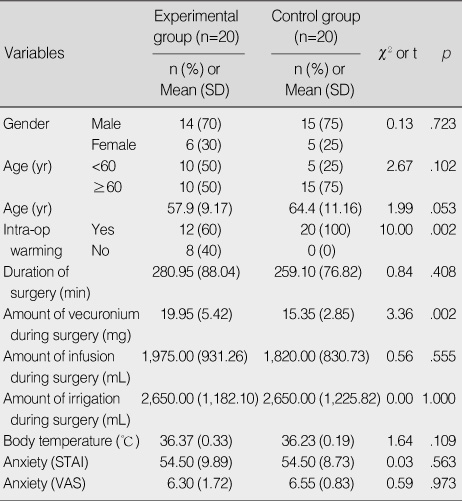
Homogeneity between Experimental Group and Control Group
STAI=State-Trait Anxiety Inventory; VAS=Visual analogue scale.
Mean differences in Body Temperature (℃), Anxiety, Pain and Thermal Comfort
*The number of person who was taken the additional pain medicine for 2 hr since end of surgery.
VAS=Visual analogue scale; STAI=State-Trait Anxiety Inventory.
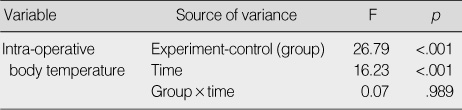
Repeated Measure ANOVA of Intra-operative Body Temperature
STAI=State-Trait Anxiety Inventory; VAS=Visual analogue scale.
*The number of person who was taken the additional pain medicine for 2 hr since end of surgery. VAS=Visual analogue scale; STAI=State-Trait Anxiety Inventory.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

