Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 39(4); 2009 > Article
-
Original Article
- Development and Application of a Feeding Program for Infants Postoperatively following Cardiac Surgery
- Ju Ryoung Moon, Yong Ae Cho, Sun In Min, Ji-Hyuk Yang, June Huh, Yeon Yi Jung
-
Journal of Korean Academy of Nursing 2009;39(4):508-517.
DOI: https://doi.org/10.4040/jkan.2009.39.4.508
Published online: August 31, 2009
1Critical Care Advanced Practice Nurse, Cardiac & Vascular Center, Samsung Medical Center, Seoul, Korea.
2Director of Nursing Staff Development, Samsung Medical Center, Seoul, Korea.
3Nursing Manager of Cardiac Intensive Care Unit, Samsung Medical Center, Seoul, Korea.
4Assistant Professor, Thoracic and Cardiovascular Surgery, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea.
5Associate Professor, Department of Pediatrics, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea.
6Director of Clinical Quality Improvement Team, Samsung Medical Center, Seoul, Korea.
- Address reprint requests to: Jung, Yeon Yi. Department of Quality Assurance, Samsung Medical Center, 50 Irwon-dong, Gangnam-gu, Seoul 135-710, Korea. Tel: 82-2-3410-3055, Fax: 82-2-3410-2850, yoenyi.jung@samsung.com
Copyright © 2009 Korean Society of Nursing Science
Abstract
-
Purpose
- Despite recent advances in the surgical and postoperative management of infants with congenital heart disease, nutritional support for this population is often suboptimal. The purpose of this study was to develop a nutritional program for the postoperative period for infants who have had cardiac surgery and to evaluate effects of the program.
-
Methods
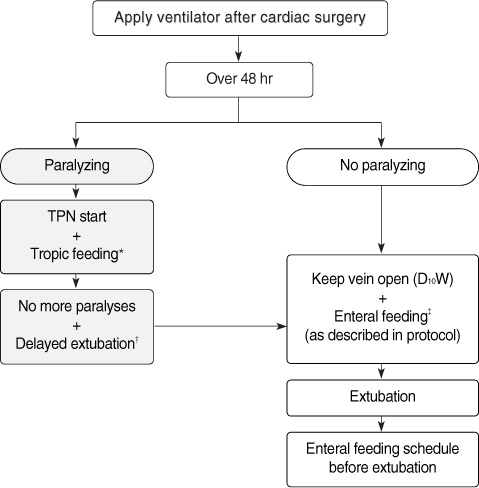
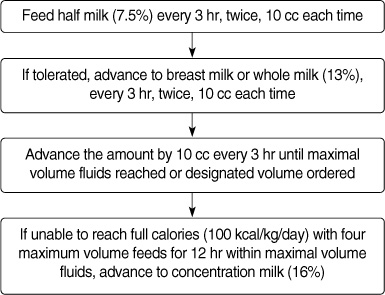
- A quasi-experimental design with pretest and posttest measures was used. A newly developed nutritional program including a feeding protocol and feeding flow was provided to the study group (n=19) and usual feeding care to the control group (n=19). The effects of the feeding program were analyzed in terms of total feed intake, total calorie intake, gastric residual volume, and frequency of diarrhea.
-
Results
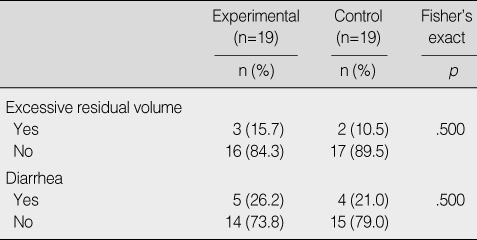
- Calorie intake and feeding amount in the study group were significantly increased compared to the control group. However, the two groups showed no significant differences in gastric residual volume and frequency of diarrhea.
-
Conclusion
- The results indicate that the nutritional program used in the study is an effective nursing intervention program in increasing feeding amount and calorie intake in infants postoperative to cardiac surgery and does not cause feeding-related complications.
This study was financially supported by the research fund of nursing department of Samsung Medical Center in 2006.
- 1. American Academy of Pediatrics Committee on Nutrition. Pediatric Nutrition Handbook. 1998;4th ed. Elk Grove Village, IL, American Academy of Pediatrics.
- 2. Beke DM, Braudis NJ, Lincolin P. Management of the pediatric postoperative cardiac surgery patient. Critical Care Nursing Clinics of North America. 2005;17:405–416.Article
- 3. Chan R, Jacobs S, Lee B. Gastrointestinal dysfunctionamong intensive care patients. Critical Care Medicine. 1987;10:909–914.
- 4. Ciotti G, Holzer R, Pozzi M, Dalzell M. Nutritional support via percutaneous endoscopic gastrostomy in children with cardiac disease experiencing difficulties with feeding. Cardiology in the Young. 2002;12:537–541.ArticlePubMed
- 5. Davey AM, Wagner CL, Cox C, Kendig JW. Feeding premature infants while low umbilical artery catheters are in place: A prospective, randomized trial. Journal of Pediatrics. 1994;124:795–799.ArticlePubMed
- 6. De Jonghe B, Appere-De-Vechi C, Fournier M, Tran B, Merrer J, Melchior JP, et al. A Prospective survey of nutritional support practices in intensive care unit patient: What is prescribed? What is delivered? Critical Care Medicine. 2001;29:8–12.ArticlePubMed
- 7. Frankenfield DC, Smith JS, Cooley RN. Accelerated nitrogen loss after traumatic injury is not attenuated by achievement of energy balance. Journal of Parenteral and Enteral Nutrition. 1997;21:324–329.ArticlePubMed
- 8. Hanekamp MN, Spoel M, Sharman-Koendjbiharie I, Jeroen WB, Albers MJ, Tibboel D. Routine enteral nutrition in neonates on extracorporeal membrane oxygenation. Pediatric Critical Care Medicine. 2005;6:275–279.ArticlePubMed
- 9. Kim JE, Choi BH, Kim KM, Ko JK, Seo DM. Analysis of malnutrition in children with congenital heart disease. Korean Journal of Pediatrics. 2001;44:161–165.
- 10. Kinney JM. Metabolic responses of the critically ill patient. Critical Care Clinics. 1995;11:569–585.ArticlePubMed
- 11. Lee SI, Choi HR. Nutrition for infants and children. 2003;Seoul, Kyomunsa.
- 12. McCulley ME, Jeffries HE, Wells WJ, Starnes VA, Castillo SL, Moromisato DY, et al. Effect of a standardized feeding protocol in infants with hypoplastic left ventricle following first stage palliation. Critical Care Medicine. 2005;33:A62. Article
- 13. Moon JR, Huh J, Lee HJ, Kang IS, Kim SH, Jun TG. Diagnosis of feeding difficulty and development of feeding protocol after cardiac surgery in infant. 2006;04;In: Paper presented at the annual meeting of the Korean Society of Quality Assurance in the Health Care; Jeju.
- 14. Ngdegger A, Eines E. Energy metabolism in infants with congenital heart disease. Nutrition. 2006;22:697–704.ArticlePubMed
- 15. Petrillo-Albarano T, Pettignano R, Asfaw M, Easley K. Use of a feeding protocol to improve nutritional support through early, aggressive, enteral nutrition in the pediatric intensive care unit. Pediatric Critical Care Medicine. 2006;7:340–344.ArticlePubMed
- 16. Pillo-Blocka F, Aditia I, Sharieff W. Rapid advancement to more concentrated formula in infants after surgery for congenital heart disease reduces duration of hospital stay: A randomized clinical trial. Journal of Pediatrics. 2004;145:761–766.PubMed
- 17. Rogers B, Arvedson J. Assessment of infant oral sensorimotor and swallowing function. Mental Retardation and Developmental Disabilities. 2005;35:74–82.
- 18. Samour PQ, Helm KK, Lang CE. Handbook of pediatric nutrition. 1999;2nd ed. Baltimore, MD, Aspen Publication.
- 19. Sanchez C, Lopez-Herce J, Carrillo A, Bustinza A, Sancho L, Vigil D. Transpyloric enteral feeding in the postoperativeof cardiac surgery in children. Pediatric Surgery. 2006;41:1096–1102.Article
- 20. Sinden AA, Sutphen JL. Pine JW. Growth and nutrition. In: Moss and Adams' heart disease in infants, children, and adolescent: Including the fetus and young adult. 1995;Baltimore, MD, Williams & Wilkins. 366–374.
- 21. Steltzer M, Rudd N, Pick B. Nutrition care for newborns with congenital heart disease. Clinics in Perinatology. 2005;32:1017–1030.ArticlePubMed
- 22. Verhoeven JJ, Hazelzet JA, van der Voort E, Joosten KF. Comparison of measured and predicted energy expenditure in mechanically ventilated children. Intensive Care Medicine. 1998;24:464–468.ArticlePubMedPDF
- 23. Wall RJ, Dittus RS, Ely EW. Protocol-driven carein the intensive care unit: A tool for quality. Critical Care. 2001;5:283–285.PubMedPMC
REFERENCES
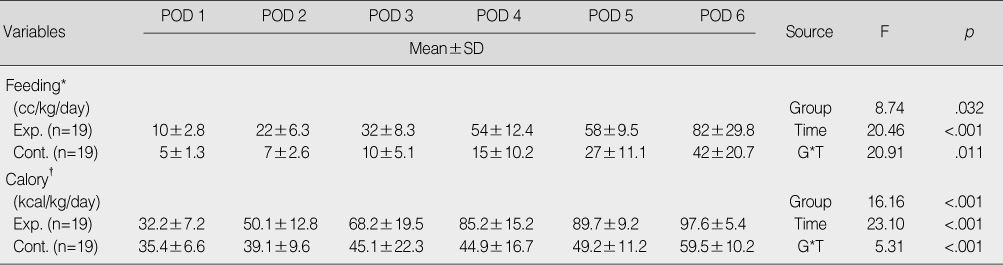
*Outcomes of 3rd, 4th, 5th, 6th day were significantly different from those of 2nd day by Bonferroni multiple comparison (p<.05) for experimental group; †Outcomes of 2nd, 3rd, 4th, 5th, 6th day were significantly different from those of 1st day by Bonferroni multiple comparison (p<.05) for experimental group.
POD=postoperative day; Exp.=experimental group; Con.=control group; G=group; T=time.
Figure & Data
REFERENCES
Citations

- Clinical Effect of an Improved Post-Operative Feeding Protocol “in Transition” Infants of Congenital Heart Disease with Pulmonary Hypertension
Huaying He, Zhiyong Lin, Yuelan Weng, Jianjie Zhou, Man Ye, Xiaowei Luo, Qifeng Zhao
Congenital Heart Disease.2021; 16(6): 655. CrossRef - Perioperative Nutritional Support and Malnutrition in Infants and Children with Congenital Heart Disease
Benjamin J. Toole, Lindsay E. Toole, Ursula G. Kyle, Antonio G. Cabrera, Renán A. Orellana, Jorge A. Coss-Bu
Congenital Heart Disease.2014; 9(1): 15. CrossRef - Development and Evaluation of an Enteral Nutrition Protocol for Dysphagia in Patients with Acute Stroke
Sung-Hee Yoo, So-Sun Kim
Journal of Korean Academy of Nursing.2014; 44(3): 280. CrossRef - Nutrition Supply, Biochemical Nutrition Indexes and Patient Outcomes in New Born Babies with Open Heart Surgery according to Post Operative Fasting Period
Ji-Young Jang, Myoung-Hee Kim
Journal of Korean Academy of Child Health Nursing.2012; 18(3): 119. CrossRef
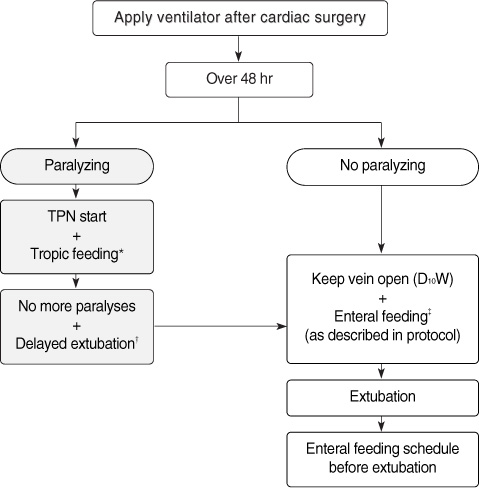
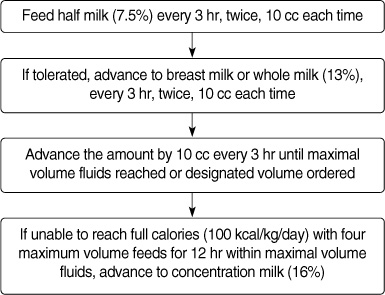
Figure 1
Figure 2
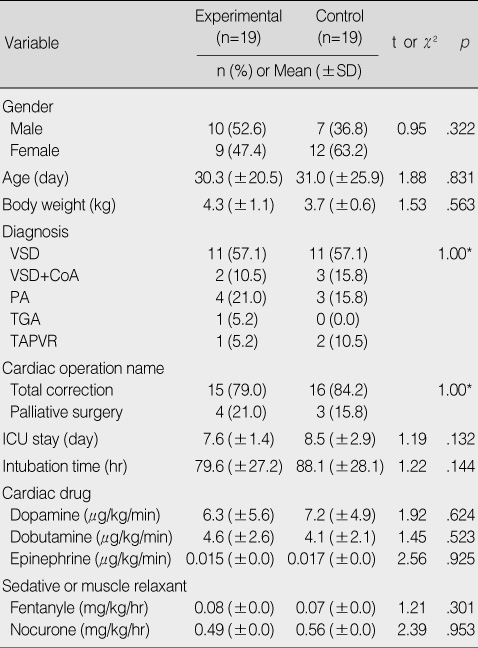
Homogeneity Test of General and Clinical Characteristics between Experimental and Control Group
*Fisher's exact test.
VSD=ventricular septal defect; CoA=coarctation of the aorta; PA=pulmonary atresia; TGA=transposition of the great arteries; TAPVR=total anomalous pulmonary venous return; ICU=intensive care unit.
Comparison of Intake between Experimental and Control Group
*Outcomes of 3rd, 4th, 5th, 6th day were significantly different from those of 2nd day by Bonferroni multiple comparison (p<.05) for experimental group; †Outcomes of 2nd, 3rd, 4th, 5th, 6th day were significantly different from those of 1st day by Bonferroni multiple comparison (p<.05) for experimental group.
POD=postoperative day; Exp.=experimental group; Con.=control group; G=group; T=time.
Incidence of Gastrointestinal Complication
*Fisher's exact test. VSD=ventricular septal defect; CoA=coarctation of the aorta; PA=pulmonary atresia; TGA=transposition of the great arteries; TAPVR=total anomalous pulmonary venous return; ICU=intensive care unit.
*Outcomes of 3rd, 4th, 5th, 6th day were significantly different from those of 2nd day by Bonferroni multiple comparison ( POD=postoperative day; Exp.=experimental group; Con.=control group; G=group; T=time.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

