Search
- Page Path
- HOME > Search
- Media discourse on physician assistant nurses in South Korea: a text network and topic modeling approach
- Young Gyu Kwon, Daun Jeong, Song Hee Park, Mi Kyung Kim, Chan Woong Kim
- J Korean Acad Nurs 2025;55(3):388-399. Published online July 30, 2025
- DOI: https://doi.org/10.4040/jkan.25038
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study quantitatively examined the portrayal of physician assistant (PA) nurses in Korean media by integrating text network analysis with latent Dirichlet allocation (LDA) topic modeling.
Methods
A total of 3,564 news articles published by nine major Korean media outlets between 2020 and 2024 were analyzed. Content analysis was conducted using term frequency-inverse document frequency calculations, network centrality analysis, and LDA topic modeling to extract key terms, map discourse structures, and identify latent topics.
Results
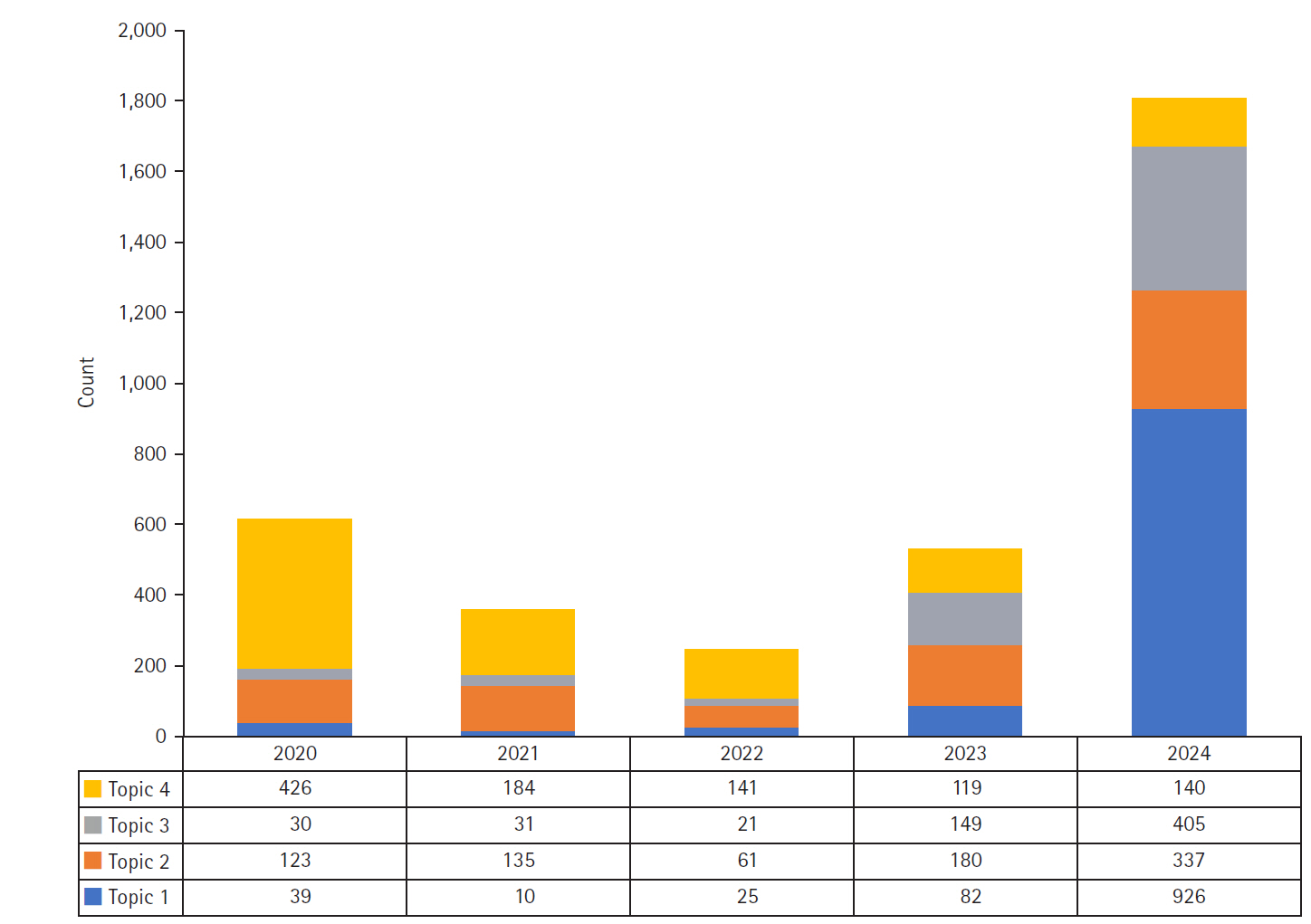
The analysis identified four primary topics in Korean media discourse: “healthcare workforce expansion policies” (30.4%), “hospital clinical practice and operational management” (23.5%), “institutionalization of the PA nursing role” (17.8%), and “COVID-19 response and public health crisis management” (28.3%). High-centrality keywords included “hospital,” “medical,” “patient,” “physician,” “government,” and “nurse,” indicating that the discourse primarily focused on clinical settings. Topic modeling revealed a major shift from pandemic-centered coverage in 2020 to a focus on healthcare workforce policy and PA nurse institutionalization in 2024, coinciding with the passage of the Nursing Act.
Conclusion
This study provides empirical evidence suggesting that the portrayal of PA nurses in Korean media discourse evolved from a peripheral regulatory issue to a central healthcare delivery solution, particularly in the contexts of workforce management, clinical practice, and crisis response. Our findings suggest that PA nurse institutionalization received broader attention when positioned as part of systemic healthcare improvements addressing concrete clinical needs. These results offer valuable insights for policymakers and administrators in framing and implementing workforce policy reforms. -
Citations
Citations to this article as recorded by- Impact of role conflict and job stress on turnover intention among Korean physician assistant nurses: A cross-sectional study
Jin-Won Lee, Eun-Hi Choi, Ji-Sun Back
International Journal of Nursing Sciences.2026;[Epub] CrossRef
- Impact of role conflict and job stress on turnover intention among Korean physician assistant nurses: A cross-sectional study
- 3,468 View
- 118 Download
- 1 Crossref

- The Effects of prompted Voiding Therapy on Urinary Incontinence Control of Elderly Patients
- Kyung Ja Lee, Mi Kyung Kim, Hee Young Song
- Journal of Nurses Academic Society 1997;27(4):943-952. Published online March 30, 2017
- DOI: https://doi.org/10.4040/jnas.1997.27.4.943
-
 Abstract
Abstract
 PDF
PDF This study was done to analyze the effects of prompted voiding therapy on urinary incontinence in elderly patients in an elderly care hospital. Specifically, this study looks to evaluate the effects of prompted voiding as an intervention for improving independent voiding and also identified the relationship of urinary continence to cognitive, emotional, and physical factors. The study was based on a pre-experimental design used to evaluate the effects of prompted voiding therapy on an experimental group without a control group. An experimental group of 143 patients was selected through convenience sampling from patients in an elderly care hospital. The data was collected from November 4 to December 14, 1996. Prompted voiding therapy is a behavioral therapy for managing incontinence and it is applied to patients who are cognitively impaired and dependent. In this study, the patients were asked at each designated time whether or not they had to urinate. If they answered yes, they were either given a bedpan or were assisted to the bathroom, and if the patient answered no, their diaper was checked to determine whether or not it was wet. The results were then recorded on the patients urinary voiding record. The urinary voiding score based on the model presented by Burton(1984), Burke and Walsh(1992), Chenitz, Stone and Salisbury(1991 was modified and used as a tool in this study. After forty six out of the total of 143 patients were selected for interviews through random sampling the levels of cognitive functions, mental depression and ADL(activities of daily life) within the given time frame were measured. In this study, the cognitive function was measured using the scale developed by Kabhn, Goldfarb, Pollack and Peck(1960), elderly mental depression, using the tool developed by Sheikh and Yesavage(1986), and the ADL(activities of daily living, through the Barthel Index. The data was analyzed through SPSS windows for descriptive statistics, repeated measured ANOVA and Pearson's correlation. According to the results of the study, the application of the prompted voiding therapy can improve the voiding pattern of patients. It was shown especially that incontinence could be controlled by the intervention developed according to the individual voiding pattern. In terms of the relationship between cognitive function, mental depression and ADL and the voiding function score, a close correlation was not found. It was shown that urinary incontinence can be improved through therapy even though patients have problems with their cognitive, mental and physical functions.
- 521 View
- 0 Download

- Effectiveness of a Behavioral Intervention Program for Urinary Incontinence in a Community Setting
- Hyun Soo Oh, Mi Kyung Kim, Wha Sook Seo
- Journal of Korean Academy of Nursing 2005;35(8):1476-1484. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.8.1476
-
 Abstract
Abstract
 PDF
PDF Purpose The purposes of this study were to examine the effectiveness of a behavioral intervention program combining pelvic floor muscle exercise with bladder training for urinary incontinence and also to conduct follow-up assessment after self-training.
Methods This study was conducted using a non-equivalent control group, pretest-posttest design. The subjects were 60 middle-aged women (control group, n=30; intervention group, n=30) who experienced an episode of urinary incontinence at least once a week. The program was run over a 4 week period (once a week) and composed of urinary incontinence education, pelvic floor muscle exercise, and bladder training.
Results Overall, there was a significant difference in urinary incontinence symptoms and psycho-social well-being related to urinary incontinence between the treatment and control group. Of the variables, weekly leakage frequencies, leakage amounts on each occasion, leakage index, frequencies of nocturia, and quality of life were significantly different between the groups. Follow-up assessment (9th week) indicated that overall incontinence symptoms and psycho-social well-being were significantly different between the posttest and follow-up assessments. Most variables of incontinence symptoms and psycho-social well-being were significantly improved at follow-up assessment versus posttest.
Conclusions The program was overall effective in terms of relieving symptoms and improving psycho-social well-being related to urinary incontinence, and this effect continued after a 4-weeks self-training period. In the respect that this is a community-based application study, the results can be meaningful and applicable.
-
Citations
Citations to this article as recorded by- Home-Based Self-Management Multimodal Pelvic Health Programs for Urinary Incontinence in Women: A Scoping Review
Rowa Al Momany, Sumaiyah Mat, Anan AL-Shdifat, Malak Omar Abbaas Alababseh, Enas Shaltaf, Saad Al-Nassan, Normala Mesbah, Devinder Kaur Ajit Singh
International Urogynecology Journal.2026;[Epub] CrossRef
- Home-Based Self-Management Multimodal Pelvic Health Programs for Urinary Incontinence in Women: A Scoping Review
- 758 View
- 5 Download
- 1 Crossref

- A Study of the Effects of Behavior Contact in Early Mother-Infant Attachment
- Mi Hae Sung, Mi Kyung Kim
- Journal of Korean Academy of Nursing 2005;35(5):842-849. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.5.842
-
 Abstract
Abstract
 PDF
PDF Purpose The main purpose of this study was to establish a nursing intervention data base to improve maternal attachment.
Method The first group of mothers(control group), experienced their first physical contact with their infants after being discharged from the hospital. The second group (experimental group) practiced early initial mother-infant postpartum contact known as the most sensitive period for founding maternal-infancy attachment. The subjects of this study gave birth to normal infants at M hospital from Aug.25 to Sept.30, 2004. During the same time, data was collected through direct observation, with instruments designed by Cropley et al., to assess the behaviors of normal attachment. The statistical methods for data analysis were percentage, mean, standard deviation and t-test with an SPSS program.
Result The group practicing initial mother-infant contact, showed a higher degree of physical and functional bonding than the group experiencing the first contact after discharge from the hospital (control group)(p<.01). The group practicing initial mother-infant contact, showed higher degrees of bonding attachment assessments than the group experiencing their first initial contact after their discharge from the hospital(p<.01).
Conclusion The group practicing early mother-infant contact, showed more maternal-infant interaction than the group experiencing their initial contact after their discharge from the hospital. These results show that maternal attachment behavior increases according with an early initial mother-infant contact.
-
Citations
Citations to this article as recorded by- Preterm Bebek Annelerinin Maternal Bağlanma, Emzirme Özyeterliliği ve Bakıma Katılım Düzeyleri
Tuğçe AĞAR, Ferdağ YILDIRIM
Cumhuriyet Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi.2023; 8(3): 466. CrossRef - Integrative Review of Nursing Intervention Studies on Mother-Infant Interactions.
Sun Jung Park, Shin Jeong Kim, Kyung Ah Kang
Child Health Nursing Research.2014; 20(2): 75. CrossRef - The Effects of Music Therapy on Postpartum Blues and Maternal Attachment of Puerperal Women
Sun Mi Lee
Journal of Korean Academy of Nursing.2010; 40(1): 60. CrossRef - Effects of Early Contact on Maternal Infant Attachment
Mi-Hae Sung, Myung-Ran Choi, Ok-Bong Um
Korean Journal of Women Health Nursing.2010; 16(2): 177. CrossRef - Effects of a Breast Feeding Promotion Program for Working Women
Ji-Won Yoon, Young-Joo Park
Journal of Korean Academy of Nursing.2008; 38(6): 843. CrossRef - Maternal Attachment Inventory: psychometric evaluation of the Korean version
Hyunjeong Shin, Young Hee Kim
Journal of Advanced Nursing.2007; 59(3): 299. CrossRef
- Preterm Bebek Annelerinin Maternal Bağlanma, Emzirme Özyeterliliği ve Bakıma Katılım Düzeyleri
- 702 View
- 8 Download
- 6 Crossref

- Factors Affecting the Severity of Urinary Incontinence and the Quality of Life of Women with Urinary Incontinence
- Hyun Soo Oh, Mi Kyung Kim
- Journal of Korean Academy of Nursing 2005;35(3):469-477. Published online June 30, 2005
- DOI: https://doi.org/10.4040/jkan.2005.35.3.469
-
 Abstract
Abstract
 PDF
PDF Purpose This study was conducted to investigate the factors that affect the severity of urinary incontinence and the quality of life of women with urinary incontinence.
Methods An exploratory correlation research design was applied and the sixty women who responded that they currently experience involuntary urine leakage at least once per week were invited to participate in the study.
Results According to the study results, the factors that significantly contribute to the severity of urinary incontinence were age, number of parity, and number of normal deliveries. Other influencing factors, such as obesity, menopausal state, hysterectomy, and number of episiotomies, were not significant to predict the severity of urinary incontinence. Urinary incontinence frequency per week and duration of experiencing urinary incontinence were shown to be factors that significantly affect quality of life.
Conclusion In women above 60 years old, multiparity, and multiple experiences of vaginal delivery tended to present a higher level of severity of urinary incontinence. In addition, women with higher frequencies of urinary incontinence per week and a longer duration of urinary incontinence showed a lower level of quality of life.
-
Citations
Citations to this article as recorded by- Effect of Pila-dance to Ease Urinary Incontinence of Middle-aged Women
Hye-Jeon Hong
The Korean Journal of Physical Education.2018; 57(2): 431. CrossRef - Health-related quality of life and mental health in older women with urinary incontinence
YeunHee Kwak, HaeJin Kwon, YoonJung Kim
Aging & Mental Health.2016; 20(7): 719. CrossRef - Association between Muscle Loss and Urinary Incontinence in Elderly Korean Women
Hyun-Jung Park, Se-Ryung Choo, Sang-Hyuk Kim, Hyun-Ki Lee, Ki Young Son
Korean Journal of Family Medicine.2015; 36(1): 22. CrossRef - A Study on Urinary Incontinence Related Health Problems in Women above Middle Age in Rural Areas and Their Coping with the Problems
Chunmi Kim, Hung Sa Lee, Eun Man Kim
Journal of Korean Academy of Community Health Nursing.2013; 24(3): 368. CrossRef - The Life Stories of Elderly Korean Women with Urinary Incontinence: A Narrative Study Approach
Bong-Sook Yih, Myungsun Yi
Journal of Korean Academy of Nursing.2009; 39(2): 237. CrossRef
- Effect of Pila-dance to Ease Urinary Incontinence of Middle-aged Women
- 839 View
- 0 Download
- 5 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


