Search
- Page Path
- HOME > Search
- Development of a scale to measure fear of falling in older adults: a psychometric validation study
- Dayeon Lee, Sunghee H Tak
- J Korean Acad Nurs 2025;55(3):413-424. Published online August 21, 2025
- DOI: https://doi.org/10.4040/jkan.25036
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to develop a scale to measure fear of falling in older adults and to validate its reliability and validity.
Methods
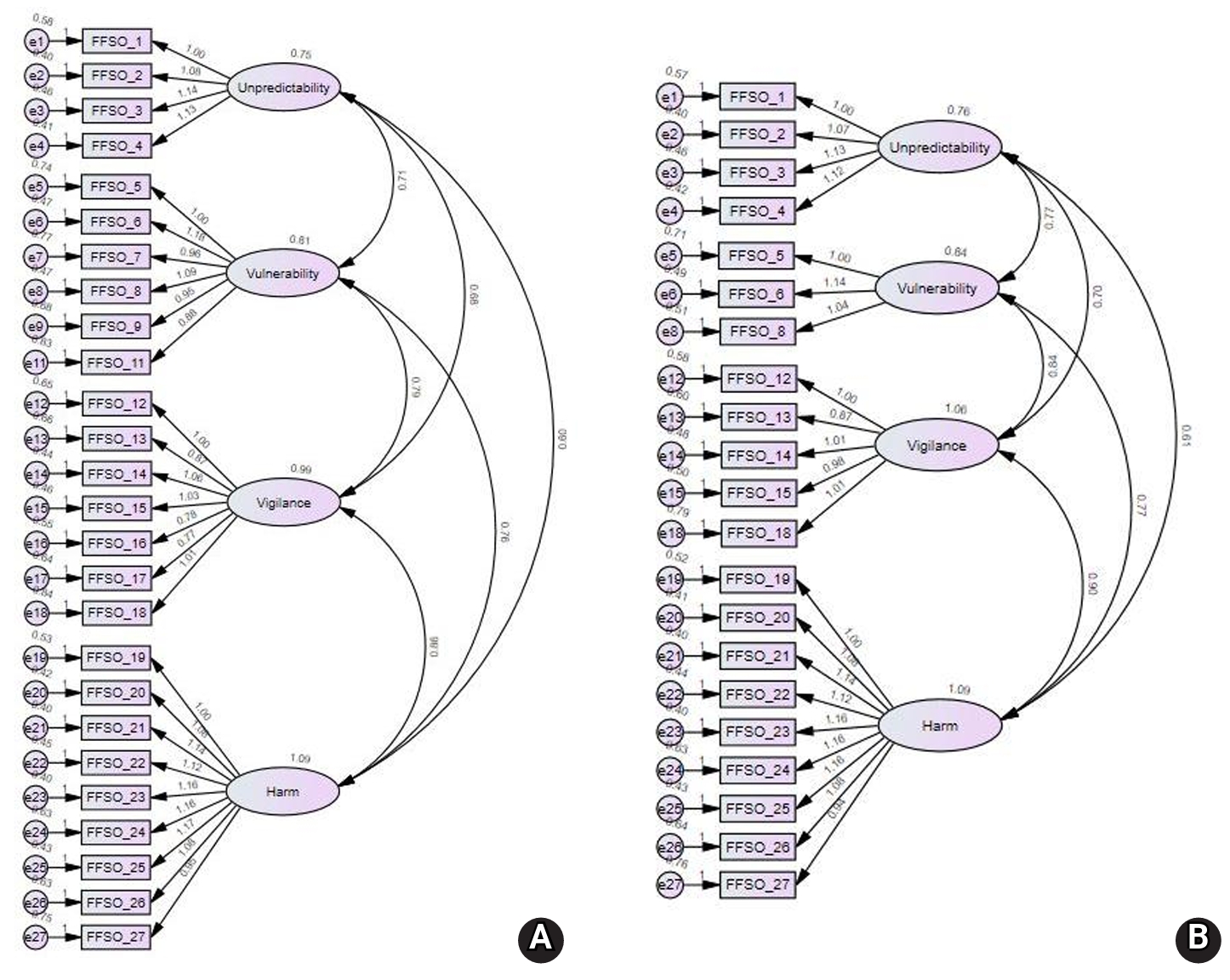
In total, 31 initial items were developed by referring to expressions from previous studies and items from existing instruments. After verifying content validity through expert evaluation, the remaining 27 items were used to construct a survey. Data from 252 participants recruited at three senior welfare centers in the metropolitan area were analyzed to examine item analysis, construct validity, convergent validity, discriminant validity, and reliability. Confirmatory factor analysis (CFA) was conducted to test construct validity. The correlation with the Korean version of the Falls Efficacy Scale-International (KFES-I) was used to assess convergent validity. Cronbach’s alpha was calculated to determine reliability.
Results
The final instrument consisted of 21 items. CFA confirmed acceptable model fit. Convergent validity was also acceptable and discriminant validity was partially supported. Correlations with the KFES-I ranged from .54 to .63. The Cronbach’s alpha coefficients for the total score and all factors ranged from .84 to .97.
Conclusion
The Fear of Falling Scale for Older Adults developed in this study is a validated tool capable of measuring various dimensions of fear of falling. It provides a foundation for accurately assessing fear of falling in older adults and addressing its specific aspects.
- 1,357 View
- 166 Download

- Psychometric Properties of the Fall Risk Perception Questionnaire-Short Version for Inpatients in Acute Care Hospitals
- Jeeeun Choi, Sujin Lee, Eunjin Park, Sangha Ku, Sunhwa Kim, Wonhye Yu, Eunmi Jeong, Sukhee Park, Yusun Park, Hye Young Kim, Sung Reul Kim
- J Korean Acad Nurs 2024;54(2):151-161. Published online May 31, 2024
- DOI: https://doi.org/10.4040/jkan.23127
-
 Abstract
Abstract
 PDF
PDF - Purpose
Patients’ perception of fall risk is a promising new indicator for fall prevention. Therefore, a fall risk perception questionnaire that can be used rapidly and repeatedly in acute care settings is required. This study aimed to develop a short version of the fall risk perception questionnaire (Short-FRPQ) for inpatients.
Methods
For the psychometric measurements, 246 inpatients were recruited from an acute care hospital. The construct (using confirmatory factor analysis and discriminant validity of each item), convergent, and known-group validities were tested to determine the validity of the Short-FRPQ. McDonald’s omega coefficient was used to examine the internal consistency of reliability.
Results
In the confirmatory factor analysis, the fit indices of the Short-FRPQ, comprising 14 items and three factors, appeared to be satisfactory. The Short-FRPQ had a significantly positive correlation with the original scale, the Korean Falls Efficacy Scale-International, and the Morse Fall Scale. The risk of falls group, assessed using the Morse Fall Scale, had a higher score on the Short-FRPQ. McDonald’s omega coefficient was .90.
Conclusion
The Short-FRPQ presents good reliability and validity. As patient participation is essential in fall interventions, evaluating the fall risk perception of inpatients quickly and repeatedly using scales of acceptable validity and reliability is necessary.
- 3,347 View
- 137 Download

- Development and Effects of a Person-Centered Fall Prevention Program for Older Adults with Dementia in Long-Term Care Hospitals: For Older Adults with Dementia and Caregivers in LongTerm Care Hospitals
- Jeong Ok Lim, Mee Ock Gu
- J Korean Acad Nurs 2022;52(3):341-358. Published online June 30, 2022
- DOI: https://doi.org/10.4040/jkan.21230
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the effects of a person-centered fall prevention program for older adults with dementia in long-term care hospitals.
Methods
A nonequivalent control group pretest-posttest design was used. The study sample included 42 older adults with dementia (experimental group: 21, control group: 21) and 42 caregivers (experimental group: 21, control group: 21). The program comprised 48 sessions held over 12 weeks and included exercise intervention with resistance and balance, dance walking (45~60 min, three times/week), cognitive and emotional intervention (35~50 min, once per week), and person-centered fall prevention education (10 min, once per week). The program for caregivers consisted of six educational sessions (i.e., fall prevention competency enhancement and person-centered care strategy education, 80 min, once per week) for six weeks. Data were collected before participation and 12 weeks after program completion from February 18 to May 12, 2019. Data analysis was conducted using the chi-square test, t-test, and Mann―Whitney U test with SPSS/WIN 21.0.
Results
The experimental group of older adults with dementia showed significant improvement in physical and cognitive functions, and a decrease in depression, and behavioral and psychological symptoms, when compared with the control group. caregivers in the experimental group exhibited significant improvement in fall-related knowledge and person-centered care of older adults with dementia compared to the control group.
Conclusion
The study findings indicate that this program was effective as a nursing intervention for fall prevention among older adults with dementia in long-term care hospitals. -
Citations
Citations to this article as recorded by- Influencing factors of depressive and anxiety symptoms among caregivers of Alzheimer's disease patients: A cross-sectional study
Chengfei Duan, Mo Zhu, Xia Li, Ling Yue
Journal of Alzheimer’s Disease.2026; 109(3): 1264. CrossRef - Factors Affecting Fall Incidents at Long-term Care Hospitals: Using Data from the Korea Patient Safety Reporting and Learning System
Soojin Chung, Jeongim Lee
Journal of Health Informatics and Statistics.2025; 50(1): 96. CrossRef - Current Trends of Exercise Programs for Improving Cognitive Function in Older Adults
Jae-Hyun Lee, Wooyeon Jo, Jaeho Jin, Yaxiong Zheng, Soyoon Lee, Se-Yeon Jang, Minseo Kim, Young-Jin Moon, Hye Gwang Jeong, Sang Ki Lee
Exercise Science.2024; 33(3): 254. CrossRef - Factors Influencing Dementia Care Competence among Care Staff: A Mixed-Methods Systematic Review Protocol
Jinfeng Zhu, Jing Wang, Bo Zhang, Xi Zhang, Hui Wu
Healthcare.2024; 12(11): 1155. CrossRef - Falls in Patients of Medical Institutions in South Korea: A Literature Review
Jongwon Choi, Woochol Joseph Choi
Physical Therapy Korea.2023; 30(1): 1. CrossRef - A Study on Emotions to Improve the Quality of Life of South Korean Senior Patients Residing in Convalescent Hospitals
Aeju Kim, Yucheon Kim, Jongtae Rhee, Songyi Lee, Youngil Jeong, Jeongeun Lee, Youngeun Yoo, Haechan Kim, Hyeonji So, Junhyeong Park
International Journal of Environmental Research and Public Health.2022; 19(21): 14480. CrossRef
- Influencing factors of depressive and anxiety symptoms among caregivers of Alzheimer's disease patients: A cross-sectional study
- 2,866 View
- 180 Download
- 3 Web of Science
- 6 Crossref

- Comparison of the Effects of Education Only and Exercise Training Combined with Education on Fall Prevention in Adults Aged 70 Years or Older Residing in Elderly Residential Facilities
- Chahwa Hong, Haejung Lee, Misoon Lee
- J Korean Acad Nurs 2021;51(2):173-187. Published online April 30, 2021
- DOI: https://doi.org/10.4040/jkan.20203
-
 Abstract
Abstract
 PDF
PDF - Purpose
To compare the effects of education only and exercise training combined with education on fall knowledge, fall efficacy, physical activity, and physical function in adults aged 70 years or older residing in elderly residential facilities.
Method
A three-group pre- and posttest design was utilized: education only (EO; n = 23), education and TheraBand (ET; n = 22), and education and walking (EW; n = 22). Fall education was provided for all three groups. In addition, TheraBand exercise training was provided for the ET and a walking exercise for the EW. Data were collected from November 1st, 2017 to February 15th, 2019 and analyzed with χ2 test, paired t-test, and one-way ANOVA using IBM SPSS/WIN ver. 22.0.
Results
Compared with the EO, the ET and the EW were more effective in terms of fall efficacy, physical activity, and lower extremity muscle strength. The EW showed higher improvement in walking abilities than the EO and the ET.
Conclusion
Exercise training combined with education is more effective in preventing falls among community-dwelling adults aged 70 years or older. When considering fall prevention programs for older adults, both TheraBand and walking exercise training combined with education can be chosen based on the participant’s physical status. Aggressive strategies to improve daily walking are required to maintain walking abilities among community-dwelling adults aged 70 years or older. -
Citations
Citations to this article as recorded by- Falls caused by balance disorders in the elderly with multiple systems involved: Pathogenic mechanisms and treatment strategies
Liwei Xing, Yi Bao, Binyang Wang, Mingqin Shi, Yuanyuan Wei, Xiaoyi Huang, Youwu Dai, Hongling Shi, Xuesong Gai, Qiu Luo, Yong Yin, Dongdong Qin
Frontiers in Neurology.2023;[Epub] CrossRef
- Falls caused by balance disorders in the elderly with multiple systems involved: Pathogenic mechanisms and treatment strategies
- 2,312 View
- 101 Download
- 1 Web of Science
- 1 Crossref

- Development and Effect of a Fall Prevention Program Based on the King's Goal Attainment Theory for Fall High-Risk Elderly Patients in Long-Term Care Hospital
- Bom Mi Park, Ho Sihn Ryu, Kyeung Eun Kwon, Chun Young Lee
- J Korean Acad Nurs 2019;49(2):203-214. Published online April 30, 2019
- DOI: https://doi.org/10.4040/jkan.2019.49.2.203
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study to develop a fringed fall prevention program based on King's goal attainment theory and education. This study is applied to the personal, interpersonal, and social systems of fall high-risk patients to test its effects.
Methods This study was a nonequivalent control group pre- and post-test design. There were 52 fall high-risk patients in the experimental group and 45 in the control group. The experimental group received six sessions, with the group sessions lasting 60 minutes and the individual sessions lasting 20~30 minutes. Data were analyzed using descriptive statistics, an χ2-test, a paired sample t-test, and a Wilcoxon signed-ranks test utilizing IBM SPSS software.
Results For the 3-month intervention period, the fall prevention program was found to be particularly effective for patients in the experimental group (from 3.38 to 1.69 per 1000 patient days;
p =.044), as opposed to the control group (from 1.94 to 1.49 per 1000 patient days;p =.300). For the 6-month follow up period, the fall prevention program was again found to be effective for patients in the experimental group (from 3.26 to 0.76 per 1000 patient days;p =.049) compared to the control group (from 1.98 to 1.01 per 1000 patient days;p =.368).Conclusion These results indicate that the fringed fall prevention program is very effective in reducing falls, not only during the intervention period, but also after the intervention period has ended. We can therefore recommend this program for use concerning fall high-risk patients in long-term care hospitals.
-
Citations
Citations to this article as recorded by- Recent advances in the identification of related factors and preventive strategies of hip fracture
Yaohui Yu, Yudan Wang, Xiaoli Hou, Faming Tian
Frontiers in Public Health.2023;[Epub] CrossRef - Falls in Patients of Medical Institutions in South Korea: A Literature Review
Jongwon Choi, Woochol Joseph Choi
Physical Therapy Korea.2023; 30(1): 1. CrossRef - Effects of a Fall Prevention Program Based on Goal Attainment Theory for Homebound Older Adults With Osteoarthritis of the Lower Extremities
Chunhee Lee, Heeok Park
Orthopaedic Nursing.2022; 41(6): 414. CrossRef - Effects of Nurse-Led Intervention Programs Based on Goal Attainment Theory: A Systematic Review and Meta-Analysis
Bom-Mi Park
Healthcare.2021; 9(6): 699. CrossRef - EFFECTIVENESS OF EDUCATIONAL INTERVENTIONS FOR FALL PREVENTION: A SYSTEMATIC REVIEW
Maria Aline Moreira Ximenes, Maria Girlane Sousa Albuquerque Brandão, Thiago Moura de Araújo, Nelson Miguel Galindo Neto, Lívia Moreira Barros, Joselany Áfio Caetano
Texto & Contexto - Enfermagem.2021;[Epub] CrossRef - Application Value of Rehabilitation Nursing in Patients with Stroke Based on the Theory of Interactive Standard: A Randomized Controlled Study
Ningning Li, Jun Wang, Mei Zheng, Qunying Ge, Mozaniel Oliveira
Evidence-Based Complementary and Alternative Medicine.2021; 2021: 1. CrossRef - A prospective cohort study of the risk factors for new falls and fragility fractures in self-caring elderly patients aged 80 years and over
Jian Zhou, Bo Liu, Ming-Zhao Qin, Jin-Ping Liu
BMC Geriatrics.2021;[Epub] CrossRef - Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study
Bom-Mi Park
Healthcare.2021; 9(6): 715. CrossRef - Development of Fall Inducement System based on Pedestrian Biological Data for Fall Reproduction
Jong-il Lee, Jong-Boo Han, Jae Wan Koo, Seokjae Lee, Dong-Seop Sohn, Kap-Ho Seo
Journal of Korea Robotics Society.2020; 15(3): 286. CrossRef
- Recent advances in the identification of related factors and preventive strategies of hip fracture
- 3,095 View
- 106 Download
- 6 Web of Science
- 9 Crossref

- Characteristics and Risk Factors for Falls in Tertiary Hospital Inpatients
- Eun-Ju Choi, Young-Shin Lee, Eun-Jung Yang, Ji-Hui Kim, Yeon-Hee Kim, Hyeoun-Ae Park
- J Korean Acad Nurs 2017;47(3):420-430. Published online January 15, 2017
- DOI: https://doi.org/10.4040/jkan.2017.47.3.420
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The aim of this study was to explore characteristics of and risk factors for accidental inpatient falls.
Methods Participants were classified as fallers or non-fallers based on the fall history of inpatients in a tertiary hospital in Seoul between June 2014 and May 2015. Data on falls were obtained from the fall report forms and data on risk factors were obtained from the electronic nursing records. Characteristics of fallers and non-fallers were analyzed using descriptive statistics. Risk factors for falls were identified using univariate analyses and logistic regression analysis.
Results Average length of stay prior to the fall was 21.52 days and average age of fallers was 61.37 years. Most falls occurred during the night shifts and in the bedroom and were due to sudden leg weakness during ambulation. It was found that gender, BMI, physical problems such elimination, gait, vision and hearing and medications such as sleeping pills, antiarrhythmics, vasodilators, and muscle relaxant were statistically significant factors affecting falls.
Conclusion The findings show that there are significant risk factors such as BMI and history of surgery which are not part of fall assessment tools. There are also items on fall assessment tools which are not found to be significant such as mental status, emotional unstability, dizziness, and impairment of urination. Therefore, these various risk factors should be examined in the fall risk assessments and these risk factors should be considered in the development of fall assessment tools.
-
Citations
Citations to this article as recorded by- Perceptions and practices of rehabilitation specialist nurses in fall management: a qualitative study
Heli Zhang, Jianfen Luo, Xiaotian Zhang, Yuting Jiang, Xiaoyu Sun, Qi Tang, Xin Wang, Baohua Li
Frontiers in Public Health.2026;[Epub] CrossRef - Evaluation of intrinsic and extrinsic fall risk factors in hospitals, long-term facilities, and homes: A narrative review
A.C. Dondi, K.G. Davis
Human Factors in Healthcare.2026; 9: 100125. CrossRef - Prevalence of bed falls among inpatients in Iranian hospitals: A meta-analysis
Parvaneh Isfahani, Mohammad Sarani, Mina Salajegheh, Somayeh Samani, Aliyeh Bazi, Mahdieh Poodineh Moghadam, Fatemeh Boulagh, Mahnaz Afshari
Human Factors in Healthcare.2025; 7: 100093. CrossRef - Evaluation of Risk Factors for Fall Incidence Based on Statistical Analysis
Da Hye Moon, Tae-Hoon Kim, Myoung-Nam Lim, Seon-Sook Han
International Journal of Environmental Research and Public Health.2025; 22(5): 748. CrossRef - Experiences of nurse managers in preventing and managing inpatient falls: a qualitative descriptive study
Erge Jia, Yan Kang, Runv Zhou, Weiying Zhang, Xueyan Li
BMJ Open.2025; 15(12): e106509. CrossRef - Sensitivity of Fall Risk Perception and Associated Factors in Hospitalized Patients with Mental Disorders
Ji Young Kim, Sung Reul Kim, Yusun Park, Jin Kyeong Ko, Eunmi Ra
Asian Nursing Research.2024; 18(5): 443. CrossRef - Psychometric Properties of the Fall Risk Perception Questionnaire-Short Version for Inpatients in Acute Care Hospitals
Jeeeun Choi, Sujin Lee, Eunjin Park, Sangha Ku, Sunhwa Kim, Wonhye Yu, Eunmi Jeong, Sukhee Park, Yusun Park, Hye Young Kim, Sung Reul Kim
Journal of Korean Academy of Nursing.2024; 54(2): 151. CrossRef - The Impact of Physical Performance and Fear of Falling on Fall Risk in Hemodialysis Patients: A Cross-Sectional Study
Jiwon Choi, Sun-Kyung Hwang
Korean Journal of Adult Nursing.2024; 36(1): 63. CrossRef - The Impact of Possible Sarcopenia and Obesity on the Risk of Falls in Hospitalized Older Patients
Kahyun Kim, Dukyoo Jung
The Korean Journal of Rehabilitation Nursing.2023; 26(1): 18. CrossRef - Analysis of Data on Accidental Falls from the Hospital Incident Reporting in a General Hospital
Yu-ri Jang, Jeong Yun Park
Quality Improvement in Health Care.2023; 29(1): 15. CrossRef - Predication of Falls in Hospitalized Cancer Patients
Jun-Nyun Kim, Sun-Hwa Beak, Bo-Seop Lee, Mi-Ra Han
Asian Oncology Nursing.2023; 23(2): 56. CrossRef - Nurses’ Burden of Elimination Care: Sequential Explanatory Mixed-Methods Design
Se Young Jung, Hui-Woun Moon, Da Som Me Park, Sumi Sung, Hyesil Jung
International Journal of General Medicine.2023; Volume 16: 4067. CrossRef - Clinical study of falls among inpatients with hematological diseases and exploration of risk prediction models
Jing Wang, Bin Chen, Fang Xu, Qin Chen, Jing Yue, Jingjing Wen, Fang Zhao, Min Gou, Ya Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - A Clinical Data Warehouse Analysis of Risk Factors for Inpatient Falls in a Tertiary Hospital: A Case-Control Study
Eunok Kwon, Sun Ju Chang, Mikyung Kwon
Journal of Patient Safety.2023; 19(8): 501. CrossRef - Z-drugs and falls in nursing home patients: data from the INCUR study
Sarah Damanti, Moreno Tresoldi, Philipe de Souto Barreto, Yves Rolland, Matteo Cesari
Aging Clinical and Experimental Research.2022; 34(12): 3145. CrossRef - The Fall Risk Screening Scale Is Suitable for Evaluating Adult Patient Fall
Li-Chen Chen, Yung-Chao Shen, Lun-Hui Ho, Whei-Mei Shih
Healthcare.2022; 10(3): 510. CrossRef - Comparisons of Fall Prevention Activities Using Electronic Nursing Records: A Case-Control Study
Hyesil Jung, Hyeoun-Ae Park, Ho-Young Lee
Journal of Patient Safety.2022; 18(3): 145. CrossRef - Risk Factors according to Fall Risk Level in General Hospital Inpatients
Yeon Hwa Lee, Myo Sung Kim
Journal of Korean Academy of Fundamentals of Nursing.2022; 29(1): 35. CrossRef - Development and validation of the fall risk perception questionnaire for patients in acute care hospitals
Jieun Choi, Se Min Choi, Jeong Sin Lee, Soon Seok Seo, Ja Yeon Kim, Hye Young Kim, Sung Reul Kim
Journal of Clinical Nursing.2021; 30(3-4): 406. CrossRef - Factors Affecting the Degree of Harm from Fall Incidents in Hospitals
Shinae Ahn, Da Eun Kim
Journal of Korean Academy of Nursing Administration.2021; 27(5): 334. CrossRef - A Machine Learning–Based Fall Risk Assessment Model for Inpatients
Chia-Hui Liu, Ya-Han Hu, Yu-Hsiu Lin
CIN: Computers, Informatics, Nursing.2021; 39(8): 450. CrossRef - Factors Influencing Falls in High- and Low-Risk Patients in a Tertiary Hospital in Korea
Young-Shin Lee, Eun-Ju Choi, Yeon-Hee Kim, Hyeoun-Ae Park
Journal of Patient Safety.2020; 16(4): e376. CrossRef - Impact of Hearing Loss on Patient Falls in the Inpatient Setting
Victoria L. Tiase, Kui Tang, David K. Vawdrey, Rosanne Raso, Jason S. Adelman, Shao Ping Yu, Jo R. Applebaum, Anil K. Lalwani
American Journal of Preventive Medicine.2020; 58(6): 839. CrossRef - Improving Prediction of Fall Risk Using Electronic Health Record Data With Various Types and Sources at Multiple Times
Hyesil Jung, Hyeoun-Ae Park, Hee Hwang
CIN: Computers, Informatics, Nursing.2020; 38(3): 157. CrossRef - Triggers and Outcomes of Falls in Hematology Patients: Analysis of Electronic Health Records
Min Kyung Jung, Sun-Mi Lee
Journal of Korean Academy of Fundamentals of Nursing.2019; 26(1): 1. CrossRef - Incidence of Falls and Risk Factors of Falls in Inpatients
Soo-Jin Yoon, Chun-Kyon Lee, In-Sun Jin, Jung-Gu Kang
Quality Improvement in Health Care.2018; 24(2): 2. CrossRef
- Perceptions and practices of rehabilitation specialist nurses in fall management: a qualitative study
- 2,667 View
- 44 Download
- 26 Crossref

- Effects of Nursing Interventions for Fall Prevention in Hospitalized Patients: A Meta-analysis
- Yoon Lee Kim, Seok Hee Jeong
- J Korean Acad Nurs 2015;45(4):469-482. Published online August 31, 2015
- DOI: https://doi.org/10.4040/jkan.2015.45.4.469
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to identify which nursing interventions are the most effective in fall prevention for hospitalized patients.
Methods From 3,675 papers searched, 34 were selected for inclusion in the meta-analysis. Number of fallers, falls, falls per 1,000 hospital-days, and injurious falls, fall protection activity, knowledge related to falls, and self-efficacy about falls were evaluated as outcome variables. Data were analyzed using the Comprehensive Meta Analysis (CMA) 2.2 Version program and the effect sizes were shown as the Odd Ratio (OR) and Hedges's g.
Results Overall effect size of nursing interventions for fall prevention was OR=0.64 (95% CI: 0.57~0.73,
p <.05) and Hedges's g= - 0.24. The effect sizes (OR) of each intervention ranged from 0.34 to 0.93, and the most effective nursing intervention was the education & environment intervention (OR=0.34, 95% CI: 0.28~0.42,p <.001), followed by education intervention (OR=0.57, 95% CI: 0.50~0.67,p =.001). Subgroup analyses showed that multifaceted interventions (OR=0.76, 95% CI: 0.73~0.79,p <.001) were more effective than unifactorial interventions, and that activities for prevention of falls (OR=0.08, 95% CI: 0.05~0.15,p <.001) showed the largest effect size among outcome variables.Conclusion Falls in hospitalized patients can be effectively prevented using the nursing interventions identified in this study. These findings provide scientific evidence for developing and using effective nursing interventions to improve the safety of hospitalized patients.
-
Citations
Citations to this article as recorded by- Characteristics and Effects of Fall Prevention Interventions among the Korean Older Adults: A Systematic Review
Jeong Ha Park, Hee Ju Kim
Journal of Korean Gerontological Nursing.2022; 24(1): 65. CrossRef - Internet-Delivered Cognitive Behavioral Therapy in Patients With Irritable Bowel Syndrome: Systematic Review and Meta-Analysis
Hyunjung Kim, Younjae Oh, Sun Ju Chang
Journal of Medical Internet Research.2022; 24(6): e35260. CrossRef - Validity and Reliability of Turkish Version of the Self- Awareness of Falls in Elderly Scale Among Elderly Inpatients
Fatma Birgili, Seda Kılınç, Nezihe Bulut Uğurlu
Cyprus Journal of Medical Sciences.2022; 7(7): 69. CrossRef - Validity of the Morse Fall Scale and the Johns Hopkins Fall Risk Assessment Tool for fall risk assessment in an acute care setting
Young Ju Kim, Kyoung‐Ok Choi, Suk Hyun Cho, Seok Jung Kim
Journal of Clinical Nursing.2022; 31(23-24): 3584. CrossRef - An Educational Intervention to Improve Staff Collaboration and Enhance Knowledge of Fall Risk Factors and Prevention Guidelines
Kimberly A. DiGerolamo, Mei Lin Chen-Lim
Journal of Pediatric Nursing.2021; 57: 43. CrossRef - Trends of Nursing Research on Accidental Falls: A Topic Modeling Analysis
Yeji Seo, Kyunghee Kim, Ji-Su Kim
International Journal of Environmental Research and Public Health.2021; 18(8): 3963. CrossRef - Analysis of Fall Incident Rate among Hospitalized Korean Children Using Big Data
Eun Joo Kim, Anna Lee
Journal of Pediatric Nursing.2021; 61: 136. CrossRef - Development and Effect of a Fall Prevention Program Based on the King's Goal Attainment Theory for Fall High-Risk Elderly Patients in Long-Term Care Hospital
Bom Mi Park, Ho Sihn Ryu, Kyeung Eun Kwon, Chun Young Lee
Journal of Korean Academy of Nursing.2019; 49(2): 203. CrossRef - Use of the Nursing Outcomes Classification for Falls and Fall Prevention by Nurses in South Korea
Eunjoo Lee
International Journal of Nursing Knowledge.2019; 30(1): 28. CrossRef - Development and Validation of the Self-Awareness of Falls in Elderly Scale Among Elderly Inpatients
Meei-Ling Shyu, Hui-Chuan Huang, Mei-Jung Wu, Hsiu-Ju Chang
Clinical Nursing Research.2018; 27(1): 105. CrossRef - The effectiveness of intervention programs for preventing patients from falls
Jana Horová, Iva Brabcová, Jitka Krocová
Kontakt.2017; 19(2): e105. CrossRef - Effect of Strength Exercise on Patient Fall Prevention Program: Focusing on the Fall High Risk Group Elderly Patients
Hyun-Ok Lee, Byung-Hwa Lee, Chang-Hee Lee
Journal of Health Informatics and Statistics.2017; 42(4): 338. CrossRef - The Effect of Pediatric Inpatient Fall Prevention Education on Caregivers' Fall-related Knowledge and Preventive Behaviors
So Yeon Park, Hyeon Ok Ju
Journal of Korean Academic Society of Nursing Education.2017; 23(4): 398. CrossRef
- Characteristics and Effects of Fall Prevention Interventions among the Korean Older Adults: A Systematic Review
- 4,028 View
- 108 Download
- 13 Crossref

- Effects of Community-based Comprehensive Fall Prevention Program on Muscle Strength, Postural Balance and Fall Efficacy in Elderly People
- Jeongyee Bae, Seong-il Cho
- J Korean Acad Nurs 2014;44(6):697-707. Published online December 31, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.6.697
-
 Abstract
Abstract
 PDF
PDF Purpose The purposes of this study was to develop a comprehensive community-based fall prevention program and to test the effects of the program on the muscle strength, postural balance and fall efficacy for elderly people.
Methods The design of this study was a nonequivalent control group pretest-posttest design. There were 28 participants in the experimental group and 29 in the control group. The program consisted of balance exercises, elastic resistance exercises and prevention education. The program was provided five times a week for 8 weeks and each session lasted 90 minutes. Data were analyzed using χ2-test, independent t-test and paired t-test using the SPSS program.
Results Muscle strength of the lower extremities, postural balance and fall efficacy scores significantly improved in the experimental group compared to the control group.
Conclusion These results suggest that this program can improve lower extremity muscle strength, postural balance and fall efficacy in elders. Therefore, this program is recommended for use in fall prevention programs for elders living in the community.
-
Citations
Citations to this article as recorded by- Muscle Strengthening Exercises for the Foot and Ankle: A Scoping Review Exploring Adherence to Best Practice for Optimizing Musculoskeletal Health
John W. A. Osborne, Hylton B. Menz, Glen A. Whittaker, Matthew Cotchett, Karl B. Landorf
Journal of Foot and Ankle Research.2025;[Epub] CrossRef - Developing a Theory-Integrated VR Information Platform for Age-Friendly Housing Environments
Yeunsook Lee, Miseon Jang
Buildings.2025; 16(1): 63. CrossRef - The Impact of a Fall Prevention Education Program on Falls-related Knowledge, Prevention Behavior, and Falls Efficacy
Jieun Oh, Taeyoung Lee, Joohyun Kim, Hyeonsuk Park, Suyeong Park, Jihye Jeong, Yeongeun Lee, Sujin Son, Ju Young Park
Quality Improvement in Health Care.2024; 30(2): 62. CrossRef - Characteristics and Effects of Fall Prevention Interventions among the Korean Older Adults: A Systematic Review
Jeong Ha Park, Hee Ju Kim
Journal of Korean Gerontological Nursing.2022; 24(1): 65. CrossRef - Development and Effect of a Fall Prevention Program Based on King’s Theory of Goal Attainment in Long-Term Care Hospitals: An Experimental Study
Bom-Mi Park
Healthcare.2021; 9(6): 715. CrossRef - Effect of Action Observation Training Using Y-Balance on Balance Capability in Young Adults
Sung Min Son, Kyung Woo Kang
The Journal of Korean Physical Therapy.2020; 32(2): 65. CrossRef - Development and Effect of a Fall Prevention Program Based on the King's Goal Attainment Theory for Fall High-Risk Elderly Patients in Long-Term Care Hospital
Bom Mi Park, Ho Sihn Ryu, Kyeung Eun Kwon, Chun Young Lee
Journal of Korean Academy of Nursing.2019; 49(2): 203. CrossRef - The Effect of Vibration Foam Roll and Flossing Band Exercise on Muscle Strengthing and Balance in Olders
Sangwan Han
Archives of Orthopedic and Sports Physical Therapy.2019; 15(2): 1. CrossRef - Classification of Chronic Dizziness in Elderly People and Relation with Falls
Dong-Suk Yang, Da-Young Lee, Sun-Young Oh, Ji-Yun Park
Research in Vestibular Science.2018; 17(1): 13. CrossRef - The Effect of Different Exercise-based Interventions on Senior Fitness Test of Elderly
KiHoon Han, Kang-Ho Bae
The Korean Journal of Physical Education.2018; 57(2): 635. CrossRef - Risk of Falls in Dizzy Patients
Sung Kyun Kim, Gi Jung Im
Research in Vestibular Science.2017; 16(1): 10. CrossRef - Analysis of Fall Accidents of Dizzy Patients in a Tertiary Hospital in South Korea (2011-2015)
Sung Kyun Kim, Sung Ho Lee, Seon Heui Lee, Jae Jun Song, Mi Jung Gwak, Hee Seon Lee, Gi Jung Im
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2017; 60(6): 271. CrossRef - Comparison of rhythmic and non-rhythmic aerobic exercises on depression and balance in the elderly
Il-Ho Kwon, Jun-Young Song, Do-Ye Kim, Je-Yeong Son, Yu-Jin Shim, Won-Seob Shin
Physical Therapy Rehabilitation Science.2017; 6(3): 146. CrossRef - Effect of Strength Exercise on Patient Fall Prevention Program: Focusing on the Fall High Risk Group Elderly Patients
Hyun-Ok Lee, Byung-Hwa Lee, Chang-Hee Lee
Journal of Health Informatics and Statistics.2017; 42(4): 338. CrossRef
- Muscle Strengthening Exercises for the Foot and Ankle: A Scoping Review Exploring Adherence to Best Practice for Optimizing Musculoskeletal Health
- 1,564 View
- 34 Download
- 14 Crossref

- A Predictive Model of Fall Prevention Behaviors in Postmenopausal Women
- Hyun-Jung Jang, Sukhee Ahn
- J Korean Acad Nurs 2014;44(5):525-533. Published online October 15, 2014
- DOI: https://doi.org/10.4040/jkan.2014.44.5.525
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose This study was done to propose and test a predictive model that would explain and predict fall prevention behaviors in postmenopausal women. The health belief model was the theoretical basis to aid development of a nursing intervention fall prevention program.
Methods Data for 421 postmenopausal women were selected from an original data set using a survey design. The structural equation model was tested for 3 constructs: modifying factors, expectation factors, and threat factors. Expectation factors were measured as relative perceived benefit (perceived benefit minus perceived barrier), self-efficacy, and health motivation; threat factors, as perceived susceptibility (fear of falling) and perceived severity (avoiding activity for fear of falling); and modifying factors: level of education and knowledge about fall prevention. Data were analyzed using SPSS Windows and AMOS program.
Results Mean age was 55.7 years (range 45-64), and 19.7% had experienced a fall within the past year. Fall prevention behaviors were explained by expectation and threat factors indicating significant direct effects. Mediating effect of health beliefs was significant in the relationship between modifying factors and fall prevention behaviors. The proposed model explained 33% of the variance.
Conclusion Results indicate that fall prevention education should include knowledge, expectation, and threat factors based on health belief model.
-
Citations
Citations to this article as recorded by- Construction and validation of a nomogram for predicting fear of falling related activity restrictions in community-dwelling older adults
Yuxin Zhang, Rong Xue, Yuxiu Zhou, Yu Liu, Yumeng Li, Xiaoyue Zhang, Kaili Zhang
Geriatric Nursing.2024; 55: 286. CrossRef - Osteoporosis or fracture risk associated with thiazolidinedione and proton pump inhibitor co‐administration in patients with type 2 diabetes mellitus
Miyoung Ock, Sera Lee, Hyunah Kim
Journal of Clinical Pharmacy and Therapeutics.2022; 47(7): 1028. CrossRef - Associations between sleep duration, midday napping, depression, and falls among postmenopausal women in China: a population-based nationwide study
Zonglei Zhou, Yu Yu, Ruzhen Zhou, Rongsheng Luan, Kunpeng Li
Menopause.2021; 28(5): 554. CrossRef - Exploring Fear of Falling Related Activity Avoidance among Postmenopausal Women
Sukhee Ahn, Rhayun Song
International Journal of Environmental Research and Public Health.2021; 18(8): 4042. CrossRef - Effects of a health-belief-model-based osteoporosis- and fall-prevention program on women at early old age
Sukhee Ahn, Jiwon Oh
Applied Nursing Research.2021; 59: 151430. CrossRef - Identification of risk factors for falls in postmenopausal women: a systematic review and meta-analysis
J. Zhao, G. Liang, H. Huang, L. Zeng, W. Yang, J. Pan, J. Liu
Osteoporosis International.2020; 31(10): 1895. CrossRef - Structural Analysis of Variables related to Fall Prevention Behavior of Registered Nurses in Small-to-Medium Sized Hospitals
Ji Hyun Park, Jung Tae Son
Journal of Korean Academy of Fundamentals of Nursing.2018; 25(4): 269. CrossRef - Relationships among Knowledge, Self-efficacy, and Health Behavior of Osteoporosis and Fall Prevention in Old Aged Women
Sukhee Ahn, Jiwon Oh
Korean Journal of Women Health Nursing.2018; 24(2): 209. CrossRef - The Mediating Effect of Fall Risk Perception on the Relationship between Fracture Risk and Fall Prevention Behaviors in Women with Osteoporosis
Eun Nam Lee, Eun Jung Choi, Moon Jung Jang, Hyun Ju Hwang
Journal of muscle and joint health.2015; 22(2): 130. CrossRef - An Equation Model Development and Test based on Health Belief Model Regarding Osteoporosis Prevention Behaviors among Postmenopausal Women
Hyun-Jung Jang, Sukhee Ahn
Korean Journal of Adult Nursing.2015; 27(6): 624. CrossRef - A Structural Equation Model of Fall Prevention Behavior among Community-dwelling Older Adults with Osteoarthritis
Keong Sook Jang, Rhayun Song
Korean Journal of Adult Nursing.2015; 27(6): 684. CrossRef
- Construction and validation of a nomogram for predicting fear of falling related activity restrictions in community-dwelling older adults
- 1,116 View
- 9 Download
- 11 Crossref

- Effects of a Fall Prevention Program on Falls in Frail Elders Living at Home in Rural Communities
- Jae-Soon Yoo, Mi Yang Jeon, Chul-Gyu Kim
- J Korean Acad Nurs 2013;43(5):613-625. Published online October 31, 2013
- DOI: https://doi.org/10.4040/jkan.2013.43.5.613
-
 Abstract
Abstract
 PDF
PDF Purpose This study was conducted to determine the effects of a fall prevention program on falls, physical function, psychological function, and home environmental safety in frail elders living at home in rural communities.
Methods The design of this study was a nonequivalent control group pre posttest design. The study was conducted from July to November, 2012 with 30 participants in the experimental group and 30 in the control group. Participants were registered at the public health center of E County. The prevention program on falls consisted of laughter therapy, exercise, foot care and education. The program was provided once a week for 8 weeks and each session lasted 80 minutes.
Results The risk score for falls and depression in the experimental group decreased significantly compared with scores for the control group. Compliance with prevention behavior related to falls, knowledge score on falls, safety scores of home environment, physical balance, muscle strength of lower extremities, and self-efficacy for fall prevention significantly increased in the experimental group compared with the control group.
Conclusion These results suggest that the prevention program on falls is effective for the prevention of falls in frail elders living at home.
-
Citations
Citations to this article as recorded by- Situational and environmental risk factors associated with home falls among community-dwelling older adults: Visualization of disparities between actual and perceived risks
Gwang Suk Kim, Min Kyung Park, Jae Jun Lee, Layoung Kim, Ji Yeon Lee, Namhee Kim
Geriatric Nursing.2025; 62: 221. CrossRef - Effectiveness of a University-Community Partnership Health Program for Older Adults: A Community-Based Rehabilitation Approach to Pain and Obesity Management
Gyeongseop Sim, Donghoon Kim
Physical Therapy Rehabilitation Science.2025; 14(3): 401. CrossRef - A Falls Prevention Program for People After Stroke in Guyana: An International Collaboration
Maureen Romanow Pascal, Barbara Lawrence, Stephanie Pires, Elton Newton, Deoranie Babulall, Kelly Saroka, Megan Shaver, Mackenzie Schanzlin, Kristi Pearage
Physical Therapy.2024;[Epub] CrossRef - Understanding the Home Environment as a Factor in Mitigating Fall Risk among Community-Dwelling Frail Older People: A Systematic Review
Gwang Suk Kim, Namhee Kim, Mi-So Shim, Jae Jun Lee, Min Kyung Park, Qing-Wei Chen
Health & Social Care in the Community.2023; 2023: 1. CrossRef - The Effect of Convergence Gamification Training in Community-Dwelling Older People: A Multicenter, Randomized Controlled Trial
Eun-Lee Lee, Myoung-Hwan Ko, Myung-Jun Shin, Byeong-Ju Lee, Da Hwi Jung, Kap-Soo Han, Jin Mi Kim
Journal of the American Medical Directors Association.2022; 23(3): 373. CrossRef - The Effects of the Fall Prevention Education Using the Kirkpatrick Model : For the Students Majoring in Housing Design
Yeunsook Lee, Min-Gi Kim, Eun-Jung Jung, Mi-Seon Jang
Journal of the Korean Housing Association.2022; 33(3): 61. CrossRef - Older Adults With Hip Arthroplasty: An Individualized Transitional Care Program
YoungJi Ko, JuHee Lee, EuiGeum Oh, MoNa Choi, ChangOh Kim, KiWol Sung, SeungHoon Baek
Rehabilitation Nursing.2019; 44(4): 203. CrossRef - Effects of a Stim up Mat Walking Exercise Program on Balance, Gait Function and Joint Motion Range of the Frail Elderly
Gyeong Ran Kim, Mi Sook Song
Journal of Korean Academy of Community Health Nursing.2019; 30(1): 47. CrossRef - Effect of Strength Exercise on Patient Fall Prevention Program: Focusing on the Fall High Risk Group Elderly Patients
Hyun-Ok Lee, Byung-Hwa Lee, Chang-Hee Lee
Journal of Health Informatics and Statistics.2017; 42(4): 338. CrossRef - The Effect of a Comprehensive Intervention Program on the Functional Status and Bone Density of the Socially-Vulnerable and Frail Elderly
In Sook Lee, Kwang Ok Lee
Journal of Korean Academy of Community Health Nursing.2016; 27(1): 51. CrossRef - The Effects of Home Visit Healthcare Using a Complex Program on Community-dwelling Frail Elders' Strength, Frailty, and Depression
Hee Gerl Kim
Journal of Korean Academy of Community Health Nursing.2015; 26(4): 405. CrossRef - Effects of Nordic walking on physical functions and depression in frail people aged 70 years and above
Han Suk Lee, Jeung Hun Park
Journal of Physical Therapy Science.2015; 27(8): 2453. CrossRef - Effects of Community-based Comprehensive Fall Prevention Program on Muscle Strength, Postural Balance and Fall Efficacy in Elderly People
Jeongyee Bae, Seong-il Cho
Journal of Korean Academy of Nursing.2014; 44(6): 697. CrossRef
- Situational and environmental risk factors associated with home falls among community-dwelling older adults: Visualization of disparities between actual and perceived risks
- 1,491 View
- 31 Download
- 13 Crossref

- Risk Factors for Pediatric Inpatient Falls
- Myung Sook Cho, Mi Ra Song, Sun Kyung Cha
- J Korean Acad Nurs 2013;43(5):595-604. Published online October 15, 2013
- DOI: https://doi.org/10.4040/jkan.2013.43.5.595
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to identify risk factors for pediatric inpatients falls.
Methods The study was a matched case-control design. The participants were 279 patients under the age of 6 who were admitted between January 1, 2004 and December 31, 2009. Through chart reviews, 93 pediatric patients who fell and 186 ones who did not fall were paired by gender, age, diagnosis, and length of stay. Five experts evaluated the 38 fall risk factors selected by the researchers.
Results In a general hospital, pediatric patients with secondary diagnosis, tests that need the patient to be moved, intravenous lines, hyperactivity, anxiolytics, sedatives and hypnotics, and general anesthetics showed significance for falls on adjusted-odds ratios. Conditional logistic regression analysis was performed to elucidate the factors that influence pediatric inpatient falls. The probability of falls increased with hyperactivity and general weakness. Patients who didn't have tests that required them to be moved and intravenous line had a higher risk of falls.
Conclusion These findings provide information that is relevant in developing fall risk assessment tools and prevention programs for pediatric inpatient falls.
-
Citations
Citations to this article as recorded by- Risk factors for falls among children aged 0–18 years: a systematic review
Lan Wang, Mao-Lin Qian, Xiao Shan, Xiao-Qin Liu
World Journal of Pediatrics.2022; 18(10): 647. CrossRef - Analysis of Fall Incident Rate among Hospitalized Korean Children Using Big Data
Eun Joo Kim, Anna Lee
Journal of Pediatric Nursing.2021; 61: 136. CrossRef - A Systematic Review and Meta-Analysis of Fall Prevention Programs for Pediatric Inpatients
Eun-Joo Kim, Geun-Myun Kim, Ji-Young Lim
International Journal of Environmental Research and Public Health.2021; 18(11): 5853. CrossRef - An electronic medical record-based fall risk assessment tool for pediatric inpatients in South Korea: Improved sensitivity and specificity
Eun Joo Kim, Ji Young Lim, Geun Myun Kim, Junghyun Min
Child Health Nursing Research.2021; 27(2): 137. CrossRef - Reliability and Validity of a Pediatric Fall Risk Assessment Scale for Hospitalized Patients in Taiwan
Ching-Mei Chang, Cheng-Fan Wen, Hsien-Feng Lin
Quality Management in Health Care.2021; 30(2): 121. CrossRef - Development and Effects of a Mobile Application for Safety Incident Prevention among Hospitalized Korean Children: A pilot Study of Feasibility and Acceptability
Jihee Han, Won-Oak Oh, Il Tae Park, Anna Lee
Journal of Pediatric Nursing.2020; 51: e69. CrossRef - Risk factors of falls among inpatients with cancer
M.D. Jun, K.M. Lee, S.A. Park
International Nursing Review.2018; 65(2): 254. CrossRef - Predictive Factors for Inpatient Falls among Children with Cerebral Palsy
Ebru Alemdaroğlu, Sibel Demir Özbudak, Sibel Mandiroğlu, Seda Alakoç Biçer, Neşe Özgirgin, Halil Uçan
Journal of Pediatric Nursing.2017; 32: 25. CrossRef - The Effect of Pediatric Inpatient Fall Prevention Education on Caregivers' Fall-related Knowledge and Preventive Behaviors
So Yeon Park, Hyeon Ok Ju
Journal of Korean Academic Society of Nursing Education.2017; 23(4): 398. CrossRef - A Pediatric Fall-Risk Assessment Tool for Hospitalized Children.
Hyeon Ju Shin, Young Nam Kim, Ju Hee Kim, In Sook Son, Kyung Sook Bang
Child Health Nursing Research.2014; 20(3): 215. CrossRef
- Risk factors for falls among children aged 0–18 years: a systematic review
- 1,611 View
- 30 Download
- 10 Crossref

- Fall Prediction Model for Community-dwelling Elders based on Gender
- Eun Suk Yun
- J Korean Acad Nurs 2012;42(6):810-818. Published online December 31, 2012
- DOI: https://doi.org/10.4040/jkan.2012.42.6.810
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to explore factors relating to number of falls among community-dwelling elders, based on gender.
Methods Participants were 403 older community dwellers (male=206, female=197) aged 60 or above. In this study, 8 variables were identified as predictive factors that can result in an elderly person falling and as such, supports previous studies. The 8 variables were categorized as, exogenous variables; perceived health status, somatization, depression, physical performance, and cognitive state, and endogenous variables; fear of falling, ADL & IADL and frequency of falls.
Results For men, ability to perform ADL & IADL (β32=1.84,
p <.001) accounted for 16% of the variance in the number of falls. For women, fear of falling (β31=0.14,p <.05) and ability to perform ADL & IADL (β32=1.01,p <.001) significantly contributed to the number of falls, accounting for 15% of the variance in the number of falls.Conclusion The findings from this study confirm the gender-based fall prediction model as comprehensive in relation to community-dwelling elders. The fall prediction model can effectively contribute to future studies in developing fall prediction and intervention programs.
-
Citations
Citations to this article as recorded by- Development of a fall prediction model for community-dwelling older adults in South Korea using machine learning: a secondary data analysis
Minhee Suh, Hyesil Jung, Juli Kim
Journal of Korean Biological Nursing Science.2024; 26(4): 288. CrossRef - Risk Factors for Falls or Fractures in Stroke Patients: An Analysis of 2020 Patient Sample Data
Miso Lee, Mikyung Moon
The Korean Journal of Rehabilitation Nursing.2024; 27(1): 58. CrossRef - Fear of falling and related factors during everyday activities in patients with chronic stroke
Suna Park, Ok-Hee Cho
Applied Nursing Research.2021; 62: 151492. CrossRef - Association between Falls and Nutritional Status of Community-Dwelling Elderly People in Korea
Ah-Ra Jo, Mi-Jeong Park, Byung-Gue Lee, Young-Gyun Seo, Hong-Ji Song, Yu-Jin Paek, Kyung-Hee Park, Hye-Mi Noh
Korean Journal of Family Medicine.2020; 41(2): 111. CrossRef - The Physical Activity and Fall Risk Among Iranian Older Male Adults
Mehdi Kushkestani, Mohsen Parvani, Shiva Ebrahimpour Nosrani, Sohrab Rezaei
The Open Nursing Journal.2020; 14(1): 159. CrossRef - Predictors of Accidental Falls in the Community-dwelling Elderly by Age
Nan Ju Park, Yong Soon Shin
Journal of Korean Academy of Community Health Nursing.2019; 30(2): 141. CrossRef - Tool for Categorizing Remaining Functional Ability of Nursing Home Residents
Hyun Ju Kim, Sung Ok Chang
Journal of Korean Gerontological Nursing.2019; 21(1): 1. CrossRef - Relationships between falls, age, independence, balance, physical activity, and upper limb function in elderly Brazilians
Daniel Marinho Cezar da Cruz, Tatiane de Carvalho Lima, Lauren Jane Nock, Mirela de Oliveira Figueiredo, Debora Caires Paulisso, Albert Lee
Cogent Medicine.2017; 4(1): 1367058. CrossRef - Effects of a Randomized Controlled Recurrent Fall Prevention Program on Risk Factors for Falls in Frail Elderly Living at Home in Rural Communities
JongEun Yim
Medical Science Monitor.2014; 20: 2283. CrossRef - Comparisons of the Falls and Intrinsic Fall Risk Factors according to Gender in the elderly at Ttransitional Periods of Life
Eunshil Yim, Dosuk Kim, Bohwan Kim
The Journal of the Korea Contents Association.2013; 13(12): 276. CrossRef - Risk Factors for Recurrent Falls Among Community-dwelling Elderly in Rural Areas
Mi-Yang Jeon, Sun Hee Yang
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(12): 6353. CrossRef - Safety Consciousness of the Elderly Living Alone
Youngsil Kang, Sun Jae Jung
Journal of muscle and joint health.2013; 20(3): 180. CrossRef
- Development of a fall prediction model for community-dwelling older adults in South Korea using machine learning: a secondary data analysis
- 951 View
- 3 Download
- 12 Crossref

- Effects of a Fall Prevention Program on Physical Fitness and Psychological Functions in Community Dwelling Elders
- Myung Soon Kwon
- J Korean Acad Nurs 2011;41(2):165-174. Published online April 30, 2011
- DOI: https://doi.org/10.4040/jkan.2011.41.2.165
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to identify effects of a fall prevention program on physical fitness and psychological functions in community dwelling elders.
Methods A quasi-experimental study was carried out with a nonequivalent control group pre & post-test design. The program, which included exercises and education, consisted of a 12-week group program and an 8-week self-management program using a health calendar. An experimental group (32) and a control group (21) participated.
Results There were significant differences in SPPB (t=-3.92,
p <.001), TUG test (t=4.94,p <.001), standing with right leg (t=-3.60,p =.001), standing with left leg (t=-3.74,p <.001), front and rear maximum step length test (t=-4.34,p <.001), right-left maximum step length test (t=-2.65,p =.011), and fall efficacy (t=-2.42,p =.019). Fall efficacy, fear of falling and depression showed significant differences following the 12-week exercise program and 8-week self-management program in the experimental group.Conclusion Study findings indicate that the fall prevention program is an effective nursing intervention to enhance physical fitness and psychological functions for elders. Using a health calendar, the self-management program was more effective for psychological functions compared to only the group program. Therefore, health providers should develop diversified fall prevention programs which include motivation plans to encourage clients in participating.
-
Citations
Citations to this article as recorded by- Effects of a fall prevention exercise regimen on physical and psychosocial outcomes in elderly community dwellers: a randomized comparative study
Ji-Yeon Sim, Jung-Wan Koo, Yeon-Gyu Jeong
Physiotherapy Theory and Practice.2025; 41(2): 252. CrossRef - Effectiveness of exercise prescription variables to reduce fall risk among older adults: a meta-analysis
Tian-Rui Zhu, Hong-Qi Xu, Jin-Peng Wei, He-Long Quan, Xue-Jiao Han, Tian-Xiang Li, Ji-Peng Shi
European Review of Aging and Physical Activity.2025;[Epub] CrossRef - Effects of Fall Prevention Exercise on Fall-Related Physical Fitness and Quality of Life in Elderly Women
Jin-Gu Ji, Yi-Sub Kwak
The Asian Journal of Kinesiology.2025; 27(4): 16. CrossRef - Effects of Fall Prevention Elastic Band Exercise on Physical Function Test, Grasp Power, Flexibility, and Muscle Volume in Older Women
Young-Eun Song
Journal of Korean Association of Physical Education and Sport for Girls and Women.2023; 37(1): 37. CrossRef - Cognitive behavioural therapy (CBT) with and without exercise to reduce fear of falling in older people living in the community
Eric Lenouvel, Phoebe Ullrich, Waldemar Siemens, Dhayana Dallmeier, Michael Denkinger, Gunver Kienle, G A Rixt Zijlstra, Klaus Hauer, Stefan Klöppel
Cochrane Database of Systematic Reviews.2023;[Epub] CrossRef - Effects of a Stim up Mat Walking Exercise Program on Balance, Gait Function and Joint Motion Range of the Frail Elderly
Gyeong Ran Kim, Mi Sook Song
Journal of Korean Academy of Community Health Nursing.2019; 30(1): 47. CrossRef - Effect of Strength Exercise on Patient Fall Prevention Program: Focusing on the Fall High Risk Group Elderly Patients
Hyun-Ok Lee, Byung-Hwa Lee, Chang-Hee Lee
Journal of Health Informatics and Statistics.2017; 42(4): 338. CrossRef - Effects of elastic-band resistance exercise on balance, mobility and gait function, flexibility and fall efficacy in elderly people
Cheol-Jin Kwak, You Lim Kim, Suk Min Lee
Journal of Physical Therapy Science.2016; 28(11): 3189. CrossRef - The Effect of a Comprehensive Intervention Program on the Functional Status and Bone Density of the Socially-Vulnerable and Frail Elderly
In Sook Lee, Kwang Ok Lee
Journal of Korean Academy of Community Health Nursing.2016; 27(1): 51. CrossRef - Effect of Tai-Chi on Grip Power, Pain and Fear of Falling in Elderly Person
Chung-uk Oh
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(5): 631. CrossRef - Effects of a Thera-Band Exercise Program on Pain, Knee Flexion ROM, and Psychological Parameters Following Total Knee Arthroplasty
Ji Yeong Yun, Jong Kyung Lee
Journal of Korean Academy of Nursing.2015; 45(6): 823. CrossRef - Strategies on fall prevention for older people living in the community: A report from a round-table meeting in IAGG 2013
Eun Joo Kim, Hidenori Arai, Piu Chan, Liang-Kung Chen, Keith D. Hill, Bernard Kong, Philip Poi, Maw Pin Tan, Hyung Joon Yoo, Chang Won Won
Journal of Clinical Gerontology and Geriatrics.2015; 6(2): 39. CrossRef - Fall Risk in the Community-dwelling Elderly who Received Home Care Services: Focused on Residential Environment and Perception of Fall Risk
Chong Mi Lee, Bok-Hee Cho
Journal of muscle and joint health.2014; 21(1): 36. CrossRef - Exercise for reducing fear of falling in older people living in the community
Denise Kendrick, Arun Kumar, Hannah Carpenter, G A Rixt Zijlstra, Dawn A Skelton, Juliette R Cook, Zoe Stevens, Carolyn M Belcher, Deborah Haworth, Sheena J Gawler, Heather Gage, Tahir Masud, Ann Bowling, Mirilee Pearl, Richard W Morris, Steve Iliffe, Kim
Cochrane Database of Systematic Reviews.2014;[Epub] CrossRef - Effects of Community-based Comprehensive Fall Prevention Program on Muscle Strength, Postural Balance and Fall Efficacy in Elderly People
Jeongyee Bae, Seong-il Cho
Journal of Korean Academy of Nursing.2014; 44(6): 697. CrossRef - Effects of a Randomized Controlled Recurrent Fall Prevention Program on Risk Factors for Falls in Frail Elderly Living at Home in Rural Communities
JongEun Yim
Medical Science Monitor.2014; 20: 2283. CrossRef - Fall Experience and Risk Factors for Falls among the Community-dwelling Elderly
Young Hee Kim, Kyung Hee Yang, Kum Sook Park
Journal of muscle and joint health.2013; 20(2): 91. CrossRef - Risk Factors for Recurrent Falls Among Community-dwelling Elderly in Rural Areas
Mi-Yang Jeon, Sun Hee Yang
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(12): 6353. CrossRef - Factors Associated with Nurses' Activities for Hospital Fall Prevention
In Kyoung Lee, Ja Yun Choi
The Korean Journal of Rehabilitation Nursing.2013; 16(1): 55. CrossRef - Effects of a Fall Prevention Program on Falls in Frail Elders Living at Home in Rural Communities
Jae-Soon Yoo, Mi Yang Jeon, Chul-Gyu Kim
Journal of Korean Academy of Nursing.2013; 43(5): 613. CrossRef - Effects of a Fall Prevention Program on Physical Functions and Psychological Functions in Rural Elderly Women
Sung-Min Kim, Go-Ya Choi
The Korean Journal of Rehabilitation Nursing.2012; 15(1): 63. CrossRef - Effect of the Tai Chi Fall Prevention Program for Elderly Women Living in the Community
In Sook Park, Hee Young So, Rhayun Song, Hyunli Kim, Sukhee Ahn
Journal of muscle and joint health.2012; 19(3): 282. CrossRef - Effects of a Health Diary Program on Fall-Related Outcomes in Low-Income Elderly Women with Osteoarthritis
Myung-Suk Lee
Journal of agricultural medicine and community health.2011; 36(3): 167. CrossRef
- Effects of a fall prevention exercise regimen on physical and psychosocial outcomes in elderly community dwellers: a randomized comparative study
- 1,740 View
- 19 Download
- 23 Crossref

- Analysis of Multi-variate Recurrent Fall Risk Factors in Elderly People Using Residential Assessment Instrument-Home Care - Comparisons between Single and Recurrent Fallers -
- In-Young Yoo
- J Korean Acad Nurs 2011;41(1):119-128. Published online February 28, 2011
- DOI: https://doi.org/10.4040/jkan.2011.41.1.119
-
 Abstract
Abstract
 PDF
PDF Purpose This study was done to determine the risk factors for recurrent fallers (2+falls) compared to single fallers.
Methods Participants were 104 community-dwelling people 65 yr of age or older. The data were collected from June 1, 2008 to June 30, 2009 using the Residential Assessment Instrument-Home Care.
Results Over the past 90 days, 55.7% of the 104 participants fell once, and 44.2% experienced recurrent falls (2+falls). In comparison of recurrent fallers with single fallers, there were significant differences in scores on the following factors: gender (χ2=4.22,
p =.040), age (χ2=5.74,p =.017), educational level (χ2=5.22,p =.022), living arrangements (χ2=35.02,p <.001), cardiovascular diseases (χ2=17.10,p <.001), hypertension (χ2=4.43,p =.035), diabetes mellitus (χ2=4.44,p =.035), glaucoma (χ2=13.95,p <.001), Minimal Data Set (MDS)-Pain (t=-2.56,p =.012), fear of falling (χ2=4.08,p =.034), reduced vision (t=-3.06,p =.003), MDS-activity of daily living (t=3.46,p =.001), MDS-Instrumental Activities of daily living (t=3.24,p =.002), cognition (MDS-Cognition Performance Scale) (t=3.40,p =.001), and 'difficulties entering and leaving the house' (χ2=4.53,p =.033).Conclusion It is important to assess the risk factors for recurrent falls and develop differentiated strategies that will help prevent recurrent falls. Additionally, utilizing a standardized tool, such as RAI-HC, would help health professionals assess multi-variate fall risk factors to facilitate comparisons of different community care settings.
-
Citations
Citations to this article as recorded by- Social Determinants of Health and Falls Among Community‐Dwelling Older Adults: A Zero‐Inflated Negative Binomial Regression Analysis
Eunjin Kim, Dahee Wi, Jiae Lee, Chang Park, Yoonjung Kim
Journal of Nursing Scholarship.2026;[Epub] CrossRef - Incident and recurrent falls among non-Hispanic Black and Hispanic men with chronic conditions
Temitope Olokunlade, Ledric D. Sherman, Mark E. Benden, Gang Han, Caroline D. Bergeron, Matthew Lee Smith
Journal of Safety Research.2025; 95: 416. CrossRef - Prediction of Recurrent Falls in Community-dwelling Older Adults Using Machine Learning Techniques
Jin Hyun Son, Wooseok Ryu
Journal of Health Informatics and Statistics.2025; 50(4): 305. CrossRef - Determining the Health Care Behavior Needs of Older Adults Based on the Omaha System
Nazmiye Kızılkaya, Gulumser Kubilay, Gulten Sucu Dag
Sage Open.2024;[Epub] CrossRef - The geographic environment and the frequency of falling: a study of mortality outcomes in elderly people in China
Yi Huang, Chen Li, Xianjing Lu, Yue Wang
Geospatial Health.2023;[Epub] CrossRef - Environmental Factors Influencing the Prevalence of Falls in South Korea
Beomryong Kim, Kwangsun Do, Jongeun Yim
Physical Therapy Rehabilitation Science.2022; 11(1): 66. CrossRef - The effects of mental health on recurrent falls among elderly adults, based on Korean Community Health Survey data
Kyung Hee Jo, Jong Park, So Yeon Ryu
Epidemiology and Health.2020; 42: e2020005. CrossRef - Fall Risk Classification in Community-Dwelling Older Adults Using a Smart Wrist-Worn Device and the Resident Assessment Instrument-Home Care: Prospective Observational Study
Yang Yang, John P Hirdes, Joel A Dubin, Joon Lee
JMIR Aging.2019; 2(1): e12153. CrossRef - Risk factors of repeated falls in the community dwelling old people
Jae Soon Yoo, Chul Gyu Kim, Jong Eun Yim, Mi Yang Jeon
Journal of Exercise Rehabilitation.2019; 15(2): 275. CrossRef - Zero-Inflated Poisson Modeling of Fall Risk Factors in Community-Dwelling Older Adults
Dukyoo Jung, Younhee Kang, Mi Young Kim, Rye-Won Ma, Pratibha Bhandari
Western Journal of Nursing Research.2016; 38(2): 231. CrossRef - The Comparison of Risk Factors for Falls in the Community-Dwelling Elderly
Soo-Min Kim
Journal of the Korean Proprioceptive Neuromuscular Facilitation Association.2016; 14(2): 93. CrossRef - Fall Risk in the Community-dwelling Elderly who Received Home Care Services: Focused on Residential Environment and Perception of Fall Risk
Chong Mi Lee, Bok-Hee Cho
Journal of muscle and joint health.2014; 21(1): 36. CrossRef - Effects of a Randomized Controlled Recurrent Fall Prevention Program on Risk Factors for Falls in Frail Elderly Living at Home in Rural Communities
JongEun Yim
Medical Science Monitor.2014; 20: 2283. CrossRef - RAI-HC as an innovative tool for future practice in home care
Helena Kisvetrová, Yukari Yamada
Journal of Nursing, Social Studies, Public Health and Rehabilitation.2014; 5(1-2): 16. CrossRef - Risk Factors for Recurrent Falls Among Community-dwelling Elderly in Rural Areas
Mi-Yang Jeon, Sun Hee Yang
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(12): 6353. CrossRef - Home environmental and health‐related factors among home fallers and recurrent fallers in community dwelling older Korean women
Young Mi Lim, Mi Hae Sung
International Journal of Nursing Practice.2012; 18(5): 481. CrossRef - Fall Prediction Model for Community-dwelling Elders based on Gender
Eun Suk Yun
Journal of Korean Academy of Nursing.2012; 42(6): 810. CrossRef - Telemonitoring System of Fall Detection for the Elderly
Yong-Gyu Lee, Dae-Jin Cheon, Gil-Won Yoon
Journal of Sensor Science and Technology.2011; 20(6): 420. CrossRef
- Social Determinants of Health and Falls Among Community‐Dwelling Older Adults: A Zero‐Inflated Negative Binomial Regression Analysis
- 1,101 View
- 9 Download
- 18 Crossref

- Fall Risk in Low-Income Elderly People in One Urban Area
- Kyung Won Choi, In-Sook Lee
- J Korean Acad Nurs 2010;40(4):589-598. Published online August 31, 2010
- DOI: https://doi.org/10.4040/jkan.2010.40.4.589
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to investigate the factors that increase of the risk for falls in low-income elders in urban areas.
Methods The participants were elderly people registered in one of public health centers in one city. Data were collected by interviewing the elders, assessing their environmental risk factors, and surveying relevant secondary data from the public health center records. For data analysis, descriptive statistics and multiple logistic regression were performed using SPSS version 14.
Results Stroke, diabetes, visual deficits, frequency of dizziness, use of assistive devices and moderate depression were statistically significant risk factors. The comorbidity of chronic diseases with other factors including depression, visual deficit, dizziness, and use of assistive devices significantly increased the risk of falls. From multiple logistic regression analysis, statistically significant predictors of falls were found to be stroke, total environmental risk scores, comorbiditiy of diabetes with visual deficits, and with depression.
Conclusion Fall prevention interventions should be multifactorial, especially for the elders with stroke or diabetes, who were identified in this study as the high risk group for falls. A fall risk assessment tool for low-income elders should include both the intrinsic factors like depression, dizziness, and use of assistive devices, and the extrinsic factors.
-
Citations
Citations to this article as recorded by- Linkages of quality of life with falls and injuries among older people in India
Anil Kumar Pal, Sanjay Kumar Pal
Scientific Reports.2025;[Epub] CrossRef - Understanding the Home Environment as a Factor in Mitigating Fall Risk among Community-Dwelling Frail Older People: A Systematic Review
Gwang Suk Kim, Namhee Kim, Mi-So Shim, Jae Jun Lee, Min Kyung Park, Qing-Wei Chen
Health & Social Care in the Community.2023; 2023: 1. CrossRef - Environmental Factors Influencing the Prevalence of Falls in South Korea
Beomryong Kim, Kwangsun Do, Jongeun Yim
Physical Therapy Rehabilitation Science.2022; 11(1): 66. CrossRef - The association between falls and anxiety among elderly Chinese individuals: The mediating roles of functional ability and social participation
Zhang Yue, Hang Liang, Xuyao Gao, Xigang Qin, Huwei Li, Nan Xiang, Erpeng Liu
Journal of Affective Disorders.2022; 301: 300. CrossRef - Epidemiology of fall and its socioeconomic risk factors in community-dwelling Korean elderly
Taekyoung Kim, Sang D. Choi, Shuping Xiong, Kyoung-Sae Na
PLOS ONE.2020; 15(6): e0234787. CrossRef - Comparison of falls-related physical fitness and fall experience characteristics of the elderly between Ulsan, Korea and Gifu, Japan
Sohee Shin
Korean Journal of Sport Science.2017; : 566. CrossRef - The elderly and falls: Factors associated with quality of life A cross-sectional study using large-scale national data in Korea
Jin-Won Noh, Kyoung-Beom Kim, Ju Hyun Lee, Byeong-Hui Lee, Young Dae Kwon, Seon Heui Lee
Archives of Gerontology and Geriatrics.2017; 73: 279. CrossRef - Falls among the non-institutionalized elderly in northern Minas Gerais, Brazil: prevalence and associated factors
Jair Almeida Carneiro, Gizele Carmen Fagundes Ramos, Ana Teresa Fernandes Barbosa, Élen Débora Souza Vieira, Jéssica Santos Rocha Silva, Antônio Prates Caldeira
Revista Brasileira de Geriatria e Gerontologia.2016; 19(4): 613. CrossRef - The Comparison of Risk Factors for Falls in the Community-Dwelling Elderly
Soo-Min Kim
Journal of the Korean Proprioceptive Neuromuscular Facilitation Association.2016; 14(2): 93. CrossRef - Effect of Tai-Chi on Grip Power, Pain and Fear of Falling in Elderly Person
Chung-uk Oh
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(5): 631. CrossRef - Relation of the Physical Performance and Fear of Falls of the Elderly
Eun-Suk Yun, Jisook An
Journal of the Korea Academia-Industrial cooperation Society.2014; 15(10): 6242. CrossRef - The Effects of the Urinary Incontinence and Quality of Sleep on Fall Efficacy of the Community Dwelling Elderly
Eun-Suk Yun
Journal of the Korea Academia-Industrial cooperation Society.2014; 15(4): 2142. CrossRef - Fall Risk in the Community-dwelling Elderly who Received Home Care Services: Focused on Residential Environment and Perception of Fall Risk
Chong Mi Lee, Bok-Hee Cho
Journal of muscle and joint health.2014; 21(1): 36. CrossRef - Factors Associated with Senile Macular Degeneration in Elders within Communities
Chul-Gyu Kim, Yungeong Park, Seungmi Park
Journal of Korean Academy of Community Health Nursing.2013; 24(1): 1. CrossRef - Safety Consciousness of the Elderly Living Alone
Youngsil Kang, Sun Jae Jung
Journal of muscle and joint health.2013; 20(3): 180. CrossRef - The Prevalence and Factors of Falls among the Community-Dwelling Elderly
Insun Jang, Eunok Park
Journal of Korean Public Health Nursing.2013; 27(1): 89. CrossRef - Fall Experience and Risk Factors for Falls among the Community-dwelling Elderly
Young Hee Kim, Kyung Hee Yang, Kum Sook Park
Journal of muscle and joint health.2013; 20(2): 91. CrossRef - Fear of Falling and Related Factors in Elderly Living Alone Based on Fall Experience
Myungsuk Lee, Yunbok Lee
Journal of agricultural medicine and community health.2013; 38(4): 243. CrossRef - Effect of the Tai Chi Fall Prevention Program for Elderly Women Living in the Community
In Sook Park, Hee Young So, Rhayun Song, Hyunli Kim, Sukhee Ahn
Journal of muscle and joint health.2012; 19(3): 282. CrossRef - Home environmental and health‐related factors among home fallers and recurrent fallers in community dwelling older Korean women
Young Mi Lim, Mi Hae Sung
International Journal of Nursing Practice.2012; 18(5): 481. CrossRef - Incidence and Predictors of Falls in Institutionalized Elderly
Ae-Ja Park, Nan-Young Lim, Yoon-Shin Kim, Yoon-Kyoung Lee, Jung-Hee Song
Journal of muscle and joint health.2011; 18(1): 50. CrossRef - Effects of a Health Diary Program on Fall-Related Outcomes in Low-Income Elderly Women with Osteoarthritis
Myung-Suk Lee
Journal of agricultural medicine and community health.2011; 36(3): 167. CrossRef
- Linkages of quality of life with falls and injuries among older people in India
- 1,187 View
- 10 Download
- 22 Crossref

- The Mediating Effect of Depression in the Relationship between Muscle Strength of Extremities and Falls among Community-Dwelling Elderly
- Hyoung-Sook Park, Kyung-Yeon Park
- J Korean Acad Nurs 2008;38(5):730-738. Published online October 12, 2008
- DOI: https://doi.org/10.4040/jkan.2008.38.5.730
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose The purpose of this study was to identify the mediating effect of depression in the relationship between muscle strength of extremities and falls among community-dwelling elderly.
Methods Two hundred forty-seven participants were recruited from a public health center, a hall for the aged and a school for the aged in B city. Face-to-face interviews were conducted using questionnaires from May to September of 2007. Data was analyzed with descriptive statistics, Pearson correlation, and multiple regression using the SPSS WIN 14.0 program.
Results There was a significantly negative relationship between muscle strength of lower extremities and falls, muscle strength of left upper extremity and falls, and muscle strength of right upper extremity and falls. Depression positively correlated with falls. Depression showed mediating effects between muscle strength of extremities and falls. Weakness of muscle strength of extremities increased depression and the increased depression increased the frequencies of falls.
Conclusion For the effective management and prevention of community-dwelling older adults’ falls, exercise programs including depression-decreasing strategies should be established. These exercise programs can decrease depression which is the mediator role between the degrees of muscle strength of extremities and falls.
-
Citations
Citations to this article as recorded by- A Study on the Depression, Family Support and Life Satisfaction in the Elderly
Sunsook Sim, Miran Bang
The Korean Journal of Rehabilitation Nursing.2017; 20(2): 122. CrossRef - The Effects of a Regular Walking Program on Body Composition, Functional Fitness, and Anxiety and Depression in Elderly Women
Samcheol Lee
Journal of The Korean Society of Integrative Medicine.2016; 4(2): 67. CrossRef - Study on the Preference Survey for Developing the Fall Impact Protective Clothing - Targeting Women ages of 50s to 70s -
Jung Hyun Park, Jeong Ran Lee
Fashion & Textile Research Journal.2014; 16(1): 101. CrossRef - Unhealthy and unsafe practices associated with symptoms of depression among injured patients
Sara L. Cooper, Allan W. Graham, Cynthia W. Goss, Carolyn DiGuiseppi
International Journal of Injury Control and Safety Promotion.2011; 18(3): 243. CrossRef - Impact of depression and activities of daily living on the fear of falling in Korean community‐dwelling elderly
Kyung Rim Shin, Younhee Kang, Mi Young Kim, Dukyoo Jung, Jeong Soo Kim, Chong Min Hong, Eun Suk Yun, Rye Won Ma
Nursing & Health Sciences.2010; 12(4): 493. CrossRef - Prevalence and Predictors of Geriatric Depression in Community-Dwelling Elderly
Jeung-Im Kim, Myoung-Ae Choe, Young Ran Chae
Asian Nursing Research.2009; 3(3): 121. CrossRef - Força muscular de idosos com e sem depressão participantes de um programa de ginástica
Vanessa Helena Santana Dalla Déa, Edison Duarte, José Rubens Rebelatto, Alessandra Paiva de Castro
Acta Ortopédica Brasileira.2009; 17(6): 322. CrossRef
- A Study on the Depression, Family Support and Life Satisfaction in the Elderly
- 968 View
- 4 Download
- 4 Web of Science
- 7 Crossref

- Effects of Tai Chi Exercise in Elderly with Knee Osteoarthritis
- Hea-Young Lee, Keum Jae Lee
- Journal of Korean Academy of Nursing 2008;38(1):11-18. Published online February 29, 2008
- DOI: https://doi.org/10.4040/jkan.2008.38.1.11
-
 Abstract
Abstract
 PDF
PDF Purpose This study was to determine whether the Sun-style 24 forms of Tai Chi exercise improve pain, stiffness, disability, knee joint motion, mobility, balance or falling.
Methods Forty-six community-dwelling elderly subjects (mean age, 75.46±6.28) voluntarily participated in an intervention group of either 24 forms of Sun-style Tai Chi for 60 min, 2 times per week for 12 weeks or a control group. A on-equivalent pretest-posttest design was used. Independent t-test and ANCOVA were used to examine group differences by using SPSS12.0.
Results The experimental group had significantly less pain (F=7.60, p=.008) and stiffness (t=-3.19, p=.003) than the control group. Also there were significant improvements in knee joint motion on the right knee (t=2.44, p=.019), left knee (t=2.30, p=.026), rising time (F=8.03, p=.07), balance on the left single leg test (t=2.20, p=.033), and fear of falling (t=-2.33, p=.024) in the Tai Chi exercise group. No significant group differences were found in disability and falls efficacy.
Conclusion The Sun-style 24 forms Tai Chi exercise is effective in decreasing pain, stiffness, fear of falling and it improves balance, rising time, and knee joint motion. We suggest a continuing long term intervention to decrease disability and increase efficacy concerning falls.
-
Citations
Citations to this article as recorded by- A Scoping Review of Interventions Aimed at Reducing Fear of Falling in Older Adults With Orthopedic Conditions
Sahar Johari, Joy MacDermid, Pulak Parikh, Ruby Grewal
Journal of Geriatric Physical Therapy.2025; 48(1): 42. CrossRef - The impact of community-based Tai Chi exercise on intrinsic capacity improvement in the elderly: a meta-analysis of randomized controlled trials
Yanzhi Lan, Jordan Tovera Salvador, Sa Zhang, Meng Wu
Postgraduate Medical Journal.2025;[Epub] CrossRef - Tai-Chi Exercise Training And Its Promising Therapeutic Impacts Among Older Community Dwelling Adults With Painful Knee Osteoarthritis
Ray Marks
Journal of Aging Research and Healthcare.2024; 5(1): 1. CrossRef - Bibliometric Analysis of Research on Traditional Chinese Exercise and Osteoarthritis
Qiu Zeng, Xiaoyi Liu, Lina Li, Qin Zhang, Chengping Luo, Shu Yang, Shuqiang Wu, An Yang, Jie Li
Journal of Pain Research.2024; Volume 17: 559. CrossRef - Effects of Taichi exercise on knee and ankle proprioception among individuals with knee osteoarthritis
Xiaoyue Hu, Zhangqi Lai, Lin Wang
Research in Sports Medicine.2020; 28(2): 268. CrossRef - Factors Affecting the Participation in Leisure Activities by Elderly Women Living Alone
Min Kyung Gu
Journal of Korean Academy of Community Health Nursing.2018; 29(3): 257. CrossRef - Influence of Leisure Activity Participation Between Genders Among Korean Older Adults
Min Kyung Gu, Sohyune R. Sok
Journal of Gerontological Nursing.2018; 44(11): 51. CrossRef - Effect of Tai-Chi on Grip Power, Pain and Fear of Falling in Elderly Person
Chung-uk Oh
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(5): 631. CrossRef - Effects of Tai Chi on Balance and Muscle Activity of Ankle Joints with USN sensor in Elderly People
Jeong-Il Kang, Hye-Min Kwon
The Journal of the Korea institute of electronic communication sciences.2015; 10(3): 425. CrossRef - Relations among Fall Efficacy, Perception of Fall Risk and Fall Prevention Behavior in the Frail Elderly at Home
Young-Hee Kim
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(7): 3383. CrossRef - Effects of Taekwondo Exercise Program in Women with Osteoarthritis
Young-Jae Kim, Nam-Sook Seo, Young-Nan Lim, Hyun-Sook Kim, Yun-Sung Kim, Sea-Ja Kim
Journal of muscle and joint health.2012; 19(2): 210. CrossRef - The Effects of an Aerobic Exercise Program on Mobility, Fall Efficacy, Balance, and Stress in the Elderly at Senior Centers
Su Kyung Chu, Chung Yul Lee, Jang Hak Yoo
Journal of Korean Academy of Community Health Nursing.2012; 23(1): 22. CrossRef - Complementary and Alternative Exercises for Management of Osteoarthritis
Ming-Chien Chyu, Vera von Bergen, Jean-Michel Brismée, Yan Zhang, James K. Yeh, Chwan-Li Shen
Arthritis.2011; 2011: 1. CrossRef - The Effects of a Case Management Program of Customized Home Visiting Health Service for Clients with Arthritis
Soon-Ok Yang, Myung Soon Kwon, Yong-Jun Choi, Seung-Hee Lee
Journal of Korean Academy of Community Health Nursing.2011; 22(2): 151. CrossRef - The Effects of a Tai Chi Exercise Program for Patients with Arthritis in Rural Areas
Aeyoung So, Kyung-Sook Lee, Jung Sook Choi, Eun Hee Lee
Journal of Korean Academy of Community Health Nursing.2010; 21(1): 118. CrossRef - Effects of Tai-Chi Exercise and Self-help Management Program Applying Laughter Therapy in Patients with Osteoarthritis
Keum-Soon Kim, Jeong-A Yu, Jin-A Kim, Yim-Sun Lee, In-Ok Lee
Journal of muscle and joint health.2010; 17(1): 68. CrossRef
- A Scoping Review of Interventions Aimed at Reducing Fear of Falling in Older Adults With Orthopedic Conditions
- 1,397 View
- 26 Download
- 16 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev