Search
- Page Path
- HOME > Search
- Reliability and validity of the Korean version of the Nurses Professional Values Scale-3 for nursing students: a methodological study
- Eun Hee Yang, Mi Yu
- J Korean Acad Nurs 2025;55(1):93-106. Published online February 20, 2025
- DOI: https://doi.org/10.4040/jkan.24113
-
 Abstract
Abstract
 PDF
PDF ePub
ePub - Purpose
This study aimed to adapt the Nurses Professional Values Scale-3 (NPVS-3) for Korean nursing students and assess its reliability and validity.
Methods
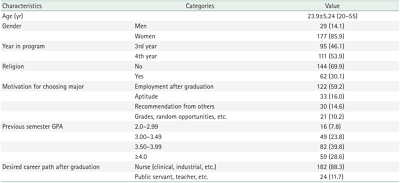
The NPVS-3 was translated into Korean using forward and back translation with expert review. Data from 206 nursing students at four universities were analyzed to assess content, construct, discriminant, and criterion validity, as well as internal consistency.
Results
The Korean version (NPVS-3K) consisted of 21 items in three subscales: caring (eight items), activism (eight items), and professionalism (five items), explaining 60.9% of the total variance. For convergent validity, standardized coefficients for the items ranged from .56 to .81, construct reliability ranged from .89 to .95, and the average variance extracted ranged from .61 to .72. The model was validated by confirmatory factor analysis (χ2=526.00 [p<.001], χ2/degrees of freedom=2.83, standardized root mean residual=.03, goodness of fit index=.81, comparative fit index=.87, Turker Lewis index=.85). Discriminant validity was confirmed using a multi-trait and multi-item matrix. Criterion validity showed positive correlations between the three NPVS-3K factors and professional identity (factor 1: r=.40, p<.001; factor 2: r=.55, p<.001; factor 3: r=.43, p<.001). Internal consistency, as measured by Cronbach’s α, was .94 overall, with subscale values of .90 for caring, .92 for activism, and .78 for professionalism.
Conclusion
The NPVS-3K demonstrated satisfactory validity and reliability, establishing it as a valuable tool for assessing the professional values of Korean nursing students. Additionally, it can aid in developing educational strategies to strengthen these values, although further research is required to confirm its broader applicability.
- 4,322 View
- 349 Download

- Types of Perception toward Ethical Issues in Perioperative Nurses: Q-Methodological Approach
- Jin Nam Kim, Seok Hee Jeong
- J Korean Acad Nurs 2018;48(6):679-691. Published online January 15, 2018
- DOI: https://doi.org/10.4040/jkan.2018.48.6.679
-
 Abstract
Abstract
 PDF
PDF Abstract Purpose This study was aimed at identifying the types of perceptions of ethical issues among perioperative nurses.
Methods Q-methodology focusing on individual subjectivity was used with data collected in November 2016. Thirty-four Q-statements were selected and scored by the 35 participants on a 9-point scale with normal distribution. Participants were perioperative nurses working in advanced general hospitals and general hospitals. The data were analyzed using the PC-QUANL program.
Results A total of 35 perioperative nurses were classified into 4 factors based on the following viewpoints: self-centered (type 1), onlooking and avoiding (type 2), patient-centered (type 3), and problem-centered (type 4). The 4 factors accounted for 57.84% of the total variance. Individual contributions of factors 1, 2, 3, and 4 were 41.80%, 7.18%, 5.20%, and 3.66%, respectively.
Conclusion The major contribution of this study is the clarification of perioperative nurses’ subjective perceptions of ethical issues. These findings can be used in formulating effective strategies for nursing educators, professional nurses, and nursing administrators to improve ethical decision-making abilities and to perform ethical nursing care by the appropriate management of ethical issues in everyday nursing practice.
-
Citations
Citations to this article as recorded by- Ethical issues in the operating room: A scoping review
Heejung Jeon, Sanghee Kim, Yuha Shon
Nursing Ethics.2024; 31(4): 472. CrossRef - The Psychological Responses of Nurses Caring for COVID-19 Patients: A Q Methodological Approach
Kyung Hyeon Cho, Boyoung Kim
International Journal of Environmental Research and Public Health.2021; 18(7): 3605. CrossRef - Development of Ethical Nursing Competence Self-rating Scale for Clinical Nurses
Borah Kang, Heeyoung Oh
Korean Journal of Adult Nursing.2020; 32(5): 482. CrossRef
- Ethical issues in the operating room: A scoping review
- 1,517 View
- 17 Download
- 2 Web of Science
- 3 Crossref

- Aesthetical-ethical Paradigm of Care Ethics in Nursing
- Byung Hye Kong
- Journal of Korean Academy of Nursing 2002;32(3):364-372. Published online March 29, 2017
- DOI: https://doi.org/10.4040/jkan.2002.32.3.364
-
 Abstract
Abstract
 PDF
PDF PURPOSE: The purposes of this study was to find aesthetical-ethical paradigm of care ethics by understanding the unique moral character of care as an art and to suggest the optimal direction of nursing ethics. METHOD: This study used meaning-heuristic and -interpretive methods of hermeneutics based on philosophical aesthetic theory; Baumgarten's aesthetics, Schiller's theory of aesthetical education and Kant's theory of aesthetical judgement. RESULT: The concept of care implied aesthetical and ethical character; caring as an art was related to moral feeling based on human dignity und emotional communication in interpersonal-relationship. Caring as an art was interpreted as a moral ideal for the promotion of the humanity und the interaction in personal-relationship according to nursing theories. Philosophical aesthetics could provide the theoretical base for the interpretation of caring as an art. The proper paradigm of care ethics in nursing could be found in character-trait ethics and communication ethics according to the philosophical aesthetics. CONCLUSION: This study could show aesthetical-ethical paradigm of care ethics in nursing by the heuristic interpretation of caring as an art according to the philosophical aesthetics.
-
Citations
Citations to this article as recorded by- Aesthetic Attitude Based on Kant’s Aesthetics of Caring Relationships in Nursing
Byunghye Kong, Younjae Oh
Healthcare.2023; 11(16): 2324. CrossRef - The Quality of Patient-centered Nursing Care Perceived by Cancer Patients Who Have Had an Operation
Keum Hyun Wang, Eun Young Park
Asian Oncology Nursing.2021; 21(2): 65. CrossRef - Intraoperative Caring Behavior and Anxiety as Perceived by Patients Undergoing Spinal Surgery under Local Anesthesia
Jung Suck Ha, Eun Nam Lee
Journal of muscle and joint health.2015; 22(2): 96. CrossRef - Development of an Instrument to Measure Intra-Operative Caring Behaviors Perceived by Regional Anesthesia Patients
Mi-Jung Kim, Eun-Nam Lee
Journal of Korean Academy of Nursing.2012; 42(5): 749. CrossRef - Effects of Compassion Satisfaction and Social Support in the Relationship between Compassion Fatigue and Burnout in Hospital Nurses
Young-Hee Yom, Hyun-Jung Kim
Journal of Korean Academy of Nursing.2012; 42(6): 870. CrossRef - Hospital Nurses' Experience of Do-Not-Resuscitate in Korea
Myungsun Yi, Sang Eun Oh, Eun Ok Choi, In Gak Kwon, Sungbok Kwon, Kyung-mi Cho, Youngah Kang, Jeonghui Ok
Journal of Korean Academy of Nursing.2008; 38(2): 298. CrossRef
- Aesthetic Attitude Based on Kant’s Aesthetics of Caring Relationships in Nursing
- 823 View
- 1 Download
- 6 Crossref

- Effect of Ethics Education on Nurse's Moral Judgement
- Yong Soon Kim
- Journal of Korean Academy of Nursing 2000;30(1):183-193. Published online March 29, 2017
- DOI: https://doi.org/10.4040/jkan.2000.30.1.183
-
 Abstract
Abstract
 PDF
PDF This main purpose of this study was to assess the effects of two different types of ethics education on the moral judgement of clinical nurses. One type was free discussions among nurses with given specific moral issues and the other type was discussions guided by experts on specific moral issues. The study employed a quasi-experimental, nonequivalent pre test-post test design using two different control groups. The conceptual framework of the study was derived from the Kohlberg's Moral Development Theory (1969) and the Greipp's Ethical Decision-Making Model (1992). The data was collected during the period of October 14 through December 15, 1998. Sample consists of 32 nurses working in the ICU who met research criteria. 16 nurses were assigned to the free discussion group and 16 nurses to the group for the guided discussion with experts group. For the pre-test, the DIT which was developed by Rest (1984) and JAND by Ketefian (1998) were used with some modification by the author. After the education, only JAND was used to assess the changes in moral judgement. The collected data was analysed using SPSS PC program. The findings are as follows: 1. There was no significant difference between two groups in their general characteristics. Only difference which was statistically significant between two groups was that realistic score on Case 3/Medical Research and Autopsy was higher in the free discussion group. 2. Hypothesis 1: "There will be a difference on the moral judgement of nurses before and after they receive an ethics education". This hypothesis was supported partially. Those who had low scores on moral judgement before the education tended to have higher scores after the education on the same issues. And, after the education, the nurses tend to give lower scores on the dilemmas they had experienced frequently at work; while giving higher scores on those dilemmas they had no prior experience. 3. Hypothesis 2: "The effect of education may differ depended upon the moral development index [P(%)] score of nurses". The effect of education was different depend on moral development level. The group who's P(%) scores was low at the pretest has higher scores in realistic moral judgement after the education, while the groups with middle or high P(%) scores went down after the education. These changes were statistically significant in some cases, thus, the Hypothesis 2 was partially supported 4. Hypothesis 3: "The method of ethics education will have different effects on the moral judgement of nurses". Even though several nurses attended the guided discussion stated that the education program broadend their perspectives the difference between two groups was not significant and this hypothesis was not supported. In conclusion, both types of ethics education had helped the nurses to acquire the skills to deal some nursing dilemmas. The effects of ethics education may differ according to the moral development index - P(%) score. However, because of some of the limitations of this study, mainly small sample size, short term education, unable to control other variables which may affect moral judgement of nurses, further research is warranted.
-
Citations
Citations to this article as recorded by- Effects of ethics education on moral sensitivity of nursing students
Hye-A Yeom, Sung-Hee Ahn, Su-Jeong Kim
Nursing Ethics.2017; 24(6): 644. CrossRef - The Effect of Biomedical Ethics Education Program for Nursing Students Freshman
Gye Seon Jeong
The Journal of Korean Academic Society of Nursing Education.2016; 22(3): 376. CrossRef - Nursing Students' Awareness of Human Rights and Influencing Factors
Sun-Woo Hong, Ji-Soo Kim, Hye-Jin Hyun
The Journal of the Korea Contents Association.2011; 11(6): 260. CrossRef - Performance Evaluation of Transmitting Brainwave Signals for Driver's Safety in Urban Area Vehicular Ad-Hoc Network
Jun-Mo Jo
The Journal of the Korea Contents Association.2011; 11(6): 26. CrossRef - Validation of a Korean version of the Moral Sensitivity Questionnaire
Sung-Suk Han, Juhu Kim, Yong-Soon Kim, Sunghee Ahn
Nursing Ethics.2010; 17(1): 99. CrossRef - Hospital Nurses' Experience of Do-Not-Resuscitate in Korea
Myungsun Yi, Sang Eun Oh, Eun Ok Choi, In Gak Kwon, Sungbok Kwon, Kyung-mi Cho, Youngah Kang, Jeonghui Ok
Journal of Korean Academy of Nursing.2008; 38(2): 298. CrossRef
- Effects of ethics education on moral sensitivity of nursing students
- 883 View
- 9 Download
- 6 Crossref

- A Philosophical Inquiry into Caring in Nursing: Based on Ricoeur's Narrative Ethics
- Byung Hye Kong
- Journal of Korean Academy of Nursing 2005;35(7):1333-1342. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2005.35.7.1333
-
 Abstract
Abstract
 PDF
PDF Purpose This paper was aimed to inquire into Ricoeur's self -hermeneutics and narrative ethics, and apply it to personal identity constituting caring and care ethics in the practice of nursing. Its purpose is to provide a philosophical foundation for caring in nursing.
Methods According to Ricoeur's narrative identity, ontological caring was interpreted as personal identity constituting caring. His ethics were described as care ethics, which contributed to preserving and promoting the personal dignity of the client, as self in search for the good life in the nursing practice.
Results Narrative understanding of the client pointed to the ontological role of care in the constitution of personal identity. From an ethical aspect of the narrative, respect for personal identity and personal dignity of the client was crucial to an ethical caring attitude, promoting self-esteem in the nursing practice.
Conclusion This paper suggested that Ricoeur's ethics could provide a philosophical basis for understanding ontological and ethical caring in nursing. This contributed to protection of the client from the threat of personal identity, as well as respecting their personal dignity.
- 667 View
- 2 Download

- A Q-methodological Study on Nursing Students' Attitudes toward Nursing Ethics
- Eun Ja Yeun, Young Mi Kwon, Hung Kyu Kim
- Journal of Korean Academy of Nursing 2004;34(8):1434-1442. Published online March 28, 2017
- DOI: https://doi.org/10.4040/jkan.2004.34.8.1434
-
 Abstract
Abstract
 PDF
PDF Purpose Professional nursing ethics is a living, dynamic set of standards for nurses'professional moral behavior. Furthermore, in daily clinical nursing training, nursing students are constantly confronted with decisionmaking that is moral in nature. The aim of this study was to identify the perceived ethical attitudes in the clinical training process of senior nursing students using Q-methodology to offer basic strategies for nursing ethics education and thereby improve patients'care.
Methods Q-methodology provides a scientific method for identifying perception structures that exist within certain individuals or groups. Thirty-seven participants in a university rated 38 selected Q-statements on a scale of 1-9. The collected data were analyzed using pc-QUNAL software.
Results Principal component analysis identified 3 types of ethical attitudes in nursing students in Korea. The categories were labeled Sacred-life, Science-realistic and Humane-life. Sacred-life individuals think that a life belongs to an absolute power (God), not a man, and a human life is a high and noble thing. Science-realistic individuals disagreed that allowing an induced abortion or embryo (human) duplication is unethical behavior that provokes a trend, which takes the value of a life lightly; most of them took a utilitarian position with respect to ethical decisions. Humane-life individuals exhibit a tendency toward human-centered thought with respect to ethical attitudes.
Conclusion This study will be of interest to educators of students of nursing and hospital nursing administrators. Also, the findings may provide the basis for the development of more appropriate strategies to improve nursing ethics education programs.
- 648 View
- 2 Download

- Path analysis of the Influence of Hospital Ethical Climate Perceived by Nurses on Supervisor Trust and Organizational Effectiveness
- Yoon Goo Noh, Myun Sook Jung
- J Korean Acad Nurs 2016;46(6):824-835. Published online December 30, 2016
- DOI: https://doi.org/10.4040/jkan.2016.46.6.824
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of this study was to analyze the paths of influence that a hospital's ethical climate exerts on nurses' organizational commitment and organizational citizenship behavior, with supervisor trust as the mediating factor, and verify compatibility of the models in hospital nurses.
Methods The sample consisted of 374 nurses recruited from four hospitals in 3 cities in Korea. The measurements included the Ethical Climate Questionnaire, Supervisor Trust Questionnaire, Organizational Commitment Questionnaire and Organizational Citizenship Behavior Questionnaire. Ethical Climate Questionnaire consisted of 6 factors; benevolence, personal morality, company rules and procedures, laws and professional codes, self-interest and efficiency. Data were analysed using SPSS version 18.0 and AMOS version 18.0.
Results Supervisor trust was explained by benevolence and self-interest (29.8%). Organizational commitment was explained by benevolence, supervisor trust, personal morality, and rules and procedures (40.4%). Organizational citizenship behavior was explained by supervisor trust, laws and codes, and benevolence (21.8%).
Conclusion Findings indicate that managers need to develop a positive hospital ethical climate in order to improve nurses' trust in supervisors, organizational commitment and organizational citizenship behavior.
-
Citations
Citations to this article as recorded by- “How does workplace spirituality influence organizational citizenship behavior in the hospitality industry?”: a person-organization fit perspective
Shalini Srivastava, Pavitra Dhamija, Poornima Madan
Journal of Asia Business Studies.2025; 19(2): 339. CrossRef - EXAMINING THE MEDIATING ROLE OF ORGANIZATIONAL TRUST ON THE EFFECT OF ETHICAL CLIMATE ON EMPLOYEE VOICE IN THE HEALTH SECTOR
Gül Bilen, İbrahim Yıkılmaz, Lütfi Sürücü
Elektronik Sosyal Bilimler Dergisi.2023; 22(88): 2117. CrossRef - Social Influencing Factors of Clinical Nurses’ Patient Advocacy
Myungji Kim, Hyunkyung Choi
Journal of Korean Academy of Nursing Administration.2023; 29(4): 363. CrossRef - Relationship between Ethical Climate, Workplace Bullying, and Turnover Intention of Hospital Nurses in Korea
Mi-Aie Lee, Hyun Ju Park, Bonghwa Kim
Journal of Korean Academy of Nursing Administration.2023; 29(4): 457. CrossRef - Relationships between job burnout, ethical climate and organizational citizenship behaviour among registered nurses: A cross‐sectional study
Lyu Wang, Xiaoyu Dong, Yan An, Cancan Chen, Marion Eckert, Greg Sharplin, Jennifer Fish, Xiuzhen Fan
International Journal of Nursing Practice.2023;[Epub] CrossRef - Ethical Climate of Nurses in Korea: A Scoping Review
Yoon Goo Noh, Oi Sun Lee
Journal of Korean Academy of Nursing Administration.2022; 28(5): 487. CrossRef - The impact of clinical nurses’ perception of hospital ethical climates on their organizational citizenship behavior
Lu Wang, Dan Li, Wanhong Wei, Ting Zhang, Wenjuan Tang, Qunfeng Lu
Medicine.2022; 101(4): e28684. CrossRef - The mediating effect of ethical climate on religious orientation and ethical behavior
Zahra Marzieh Hassanian, Arezoo Shayan
Nursing Ethics.2019; 26(4): 1114. CrossRef
- “How does workplace spirituality influence organizational citizenship behavior in the hospitality industry?”: a person-organization fit perspective
- 1,261 View
- 5 Download
- 8 Crossref

- Bioethical Approach for Nursing Research -Focused on the Use of Research Ethics Committees
- Ihn Sook Jeong
- J Korean Acad Nurs 2015;45(3):315-322. Published online June 30, 2015
- DOI: https://doi.org/10.4040/jkan.2015.45.3.315
-
 Abstract
Abstract
 PDF
PDF Purpose This paper was written to introduce methods of using the research ethics committee (RES) from requesting the initial review to reporting the close-out for nursing researchers.
Methods General ethical principles were described by reviewing the 'Bioethics and Safety Act' and other related guidelines, and constructing some questions and answers.
Results The results were composed of three parts; definition of RES, steps in using RES, and archiving. The 7 steps for using RES were; identifying whether the study needed to be reviewed, by the RES identifying whether the study could be exempted, requesting the initial review after preparing documents, requesting the re-review, requesting an amendment review, requesting a continuing review and reporting the close-out.
Conclusion Nursing researchers need to receive RES approval before starting nursing research involving human subjects. Nursing researchers are urged to use the steps reported in this paper to receive RES approval easily and quickly.
-
Citations
Citations to this article as recorded by- Nursing Faculties’ Knowledge of and Attitudes Toward Research Ethics According to Demographic Characteristics and Institutional Environment in Korea
Sukhee Ahn, Geum Hee Jeong, Hye Sook Shin, Jeung-Im Kim, Yunmi Kim, Ju-Eun Song, Sun-Hee Kim, Ju Hee Kim, Yun Jung Lee, Young A. Song, Eun Hee Lee, Myoung-Hee Kim
Sage Open.2020;[Epub] CrossRef
- Nursing Faculties’ Knowledge of and Attitudes Toward Research Ethics According to Demographic Characteristics and Institutional Environment in Korea
- 1,065 View
- 5 Download
- 1 Crossref

- Educational Needs Assessment on Research Ethics among Nursing Researchers
- Ihn Sook Jeong, Mee Ock Gu, Keum Soon Kim, Kwang Ja Lee, Soo Yang
- J Korean Acad Nurs 2010;40(4):515-523. Published online August 31, 2010
- DOI: https://doi.org/10.4040/jkan.2010.40.4.515
-
 Abstract
Abstract
 PDF
PDF Purpose This study aimed to investigate the educational needs of research ethics among nursing researchers.
Methods Convenience sample of 161 nursing professors and 262 master or doctoral nursing students participated in the study. Data was collected with self-reported questionnaire from June to August 2009, and analyzed with descriptive statistics using SPSS WIN (version 14.0).
Results Among 161 nursing professors, about 31.7% has educated nursing ethics in the postgraduate course. The most common course was nursing research or methodology (62.7%), and median education time was 2 hr. Areas that showed difficulty in understanding was the conflict of interest and plagiarism for professors and falsification and fabrication for graduate students. Average knowledge on the research ethics was 75.4 points for professors and 61.6 points for students based on the 100 points.
Conclusion Educational needs of research ethics among nursing professors and students in the postgraduate course was high. We recommend both basic and advanced research ethics educational programs for the nursing researchers. The basic course should be at least 6 hr and include various cases and something to discuss.
-
Citations
Citations to this article as recorded by- Nurses’ Experience and Satisfaction as Research Participants in Nursing Research - A View of Protecting Vulnerable Populations: A Cross-sectional Descriptive Study
Go-Eun Lee, Sanghee Kim
Korean Journal of Adult Nursing.2022; 34(6): 565. CrossRef - Nursing Faculties’ Knowledge of and Attitudes Toward Research Ethics According to Demographic Characteristics and Institutional Environment in Korea
Sukhee Ahn, Geum Hee Jeong, Hye Sook Shin, Jeung-Im Kim, Yunmi Kim, Ju-Eun Song, Sun-Hee Kim, Ju Hee Kim, Yun Jung Lee, Young A. Song, Eun Hee Lee, Myoung-Hee Kim
Sage Open.2020;[Epub] CrossRef - Knowledge and Attitudes of Social Behavioral Researchers on Institutional Review Board (IRB) Reviews*
Go-Eun LEE, Sanghee KIM, Min-Shik KIM, Eui Geum OH
Korean Journal of Medical Ethics.2017; 20(3): 287. CrossRef - Effects of Nursing Research Support Program on the Attitudes and the Barriers of the Nurse
Young-Ok Yang
Journal of the Korea Academia-Industrial cooperation Society.2015; 16(12): 8556. CrossRef - Operational effectiveness of blended e-learning program for nursing research ethics
Kap-Chul Cho, Gisoo Shin
Nursing Ethics.2014; 21(4): 484. CrossRef - A Study on the Research Ethics of Occupational Therapy Researchers
So-Yeon Park, Jin-Kyung Kim
Journal of Korean Society of Occupational Therapy.2014; 22(1): 97. CrossRef - Level of Awareness, Self-efficacy and Knowledge of Research Ethics among Nursing Graduate Students*
Eui Geum OH, Sang Hee KIM, Jae Yong YOO
Korean Journal of Medical Ethics.2012; 15(2): 244. CrossRef - The Development and Evaluation of a Research Ethics Course for a Graduate-level Educational Program in Nursing
Euigeum OH, Sanghee KIM, Jae Yong YOO, Sosun KIM, Sunah KIM, Eunhee CHO
Korean Journal of Medical Ethics.2011; 14(4): 482. CrossRef
- Nurses’ Experience and Satisfaction as Research Participants in Nursing Research - A View of Protecting Vulnerable Populations: A Cross-sectional Descriptive Study
- 931 View
- 4 Download
- 8 Crossref

- Hospital Nurses' Experience of Do-Not-Resuscitate in Korea
- Myungsun Yi, Sang Eun Oh, Eun Ok Choi, In Gak Kwon, Sungbok Kwon, Kyung-mi Cho, Youngah Kang, Jeonghui Ok
- Journal of Korean Academy of Nursing 2008;38(2):298-309. Published online April 30, 2008
- DOI: https://doi.org/10.4040/jkan.2008.38.2.298
-
 Abstract
Abstract
 PDF
PDF Purpose The purpose of the study was to describe the experiences of do-not-resuscitate (DNR) among nurses.
Methods Data were collected by in-depth interviews with 8 nurses in 8 different hospitals. Conventional qualitative content analysis was used to analyze the data.
Results Eight major themes emerged from the analysis: DNR decision-making bypassing the patient, inefficiency in the decision-making process of DNR, negative connotation of DNR, predominance of verbal DNR over written DNR, doubts and confusion about DNR, least amount of intervention in the decision for DNR change of focus in the care of the patient after a DNR order, and care burden of patients with DNR. Decision-making of DNR occurred between physicians and family members, not the patients themselves. Often high medical expenses were involved in choosing DNR, thus if choosing DNR it was implied the family members and health professionals as well did not try their best to help the patient. Verbal DNR permission was more popular in clinical settings. Most nurses felt guilty and depressed about the dying/death of patients with DNR.
Conclusion Clearer guidelines on DNR, which reflect a family-oriented culture, need to be established to reduce confusion and to promote involvement in the decision-making process of DNR among nurses.
-
Citations
Citations to this article as recorded by- Reliability and Validity of an Instrument Assessing Advance Directives for Nurse
Hojung Cheon, Eunha Kim
The Korean Journal of Hospice and Palliative Care.2019; 22(3): 134. CrossRef - Intensive Care Nurses’ Experiences of Death of Patients with DNR Orders
Ji Yun Lee, Yong Mi Lee, Jae In Jang
The Korean Journal of Hospice and Palliative Care.2017; 20(2): 122. CrossRef - Attitudes and Type Analysis of Cardiopulmonary Resuscitation among Hospital Nurses in Emergency Room and Intensive Care Units
Eun-Ho Ha, Kyoung-Soon Hyun
Korean Journal of Adult Nursing.2017; 29(5): 484. CrossRef - Attitude, Role Perception and Nursing Stress on Life Sustaining Treatment among Intensive Care Unit Nurses
Su Jeong Lee, Hye Young Kim
Korean Journal of Adult Nursing.2017; 29(2): 131. CrossRef - Withdrawal of Life-Sustaining Treatment from Children: Experiences of Nurses Caring for the Children
So Yeon Park, Hyeon Ok Ju, Ga Eon Lee
Child Health Nursing Research.2017; 23(3): 364. CrossRef - Changes of Nursing Activities on Patients with DNR Orders
Ji Yun Lee, Jae In Jang
The Korean Journal of Hospice and Palliative Care.2017; 20(1): 46. CrossRef - Experience of Life-sustaining Treatment in Patient Care among Intensive Care Unit Nurses: Phenomenological Approach
Su Jeong Lee, Hye Young Kim
Journal of Korean Academy of Fundamentals of Nursing.2016; 23(2): 172. CrossRef - Comparison of attitudes towards death and perceptions of do‐not‐resuscitate orders between older Korean adults residing in a facility and at home
Soon Young Park, Ok Sun Kim, Nam Hyun Cha, Sohyune R Sok
International Journal of Nursing Practice.2015; 21(5): 660. CrossRef - Application of Animation Mobile Electronic Informed Consent in Inpatient of Long-term Care Hospital: Focused on DNR Informed Consent
Ji-Kyeong Park, Ji-On Kim
Journal of Digital Convergence.2015; 13(11): 187. CrossRef - Ethical Attitudes, Perceptions of DNR and Advance Directives of General Population
Kyung Ja Kang, Se Jin Ju
Journal of Korean Academy of Psychiatric and Mental Health Nursing.2014; 23(2): 113. CrossRef - Nurses' Experiences of Do-Not-Resuscitate (DNR) by the Narrative Inquiry
Mi Kyung Woo, Miyoung Kim
Korean Journal of Adult Nursing.2013; 25(3): 322. CrossRef - Nurses’ Emotional Responses and Ethical Attitudes towards Elderly Patients’ DNR Decision
Junghee Mun, Sumi Kim
The Korean Journal of Hospice and Palliative Care.2013; 16(4): 216. CrossRef - Comparing the Preference for Terminal Care in Nurses and Patients
Dong Soon Kim, AeYoung So, Kyung-Sook Lee, Jung Sook Choi
Journal of muscle and joint health.2013; 20(3): 214. CrossRef - Family factors affecting on withdrawal of life‐sustaining treatment in Korea
Kae‐Hwa Jo, Gyeong‐Ju An, Kyung Su Han
International Journal of Nursing Practice.2012; 18(6): 552. CrossRef - Development of Implementation Strategies for u-Health Services Based on the Healthcare Professionals' Experiences
Jeongeun Kim, Sukwha Kim, Heechan Kim, Kyungwhan Kim, Sukchul Yang, Yoonju Shin
Telemedicine and e-Health.2011; 17(2): 80. CrossRef
- Reliability and Validity of an Instrument Assessing Advance Directives for Nurse
- 1,349 View
- 7 Download
- 15 Crossref

 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION

 First
First Prev
Prev


