Articles
- Page Path
- HOME > J Korean Acad Nurs > Volume 42(2); 2012 > Article
-
Original Article
- Breast Feeding Rates and Factors Influencing Breast Feeding Practice in Late Preterm Infants: Comparison with Preterm Born at Less than 34 Weeks of Gestational Age
- Gun Ja Jang, Sang Lak Lee, Hyeon Mi Kim
-
Journal of Korean Academy of Nursing 2012;42(2):181-189.
DOI: https://doi.org/10.4040/jkan.2012.42.2.181
Published online: April 30, 2012
1Assistant Professor, Department of Nursing, Daegu University, Daegu, Korea.
2Professor, Department of Pediatrics, School of Medicine, Keimyung University, Daegu, Korea.
3Assistant professor, Department of Nursing, Taegu Science College, Daegu, Korea.
- Address reprint requests to: Kim, Hyeon Mi. Department of Nursing, Taegu Science College, 47 Yeongsong-ro, Book-gu, Daegu 702-723, Korea. Tel: +82-53-320-1064, Fax: +82-53-320-1761, hyeonmi@paran.com
© 2012 Korean Society of Nursing Science
- 179 Views
- 0 Download
- 20 Crossref
Abstract
-
Purpose
- This study was done to compare breast feeding rates and factors influencing feeding practice between late preterm (34≤GA<37) and preterm infants (GA<34).
-
Methods
- A survey was done of 207 late preterm and 117 preterm infants in neonatal intensive care units (NICU) of 4 university hospitals in D city. Data were collected from July 2009 to June 2010 from 324 medical records in the NICU. Breast-feeding at home was checked either by telephone survey or questioning during hospital visits.
-
Results
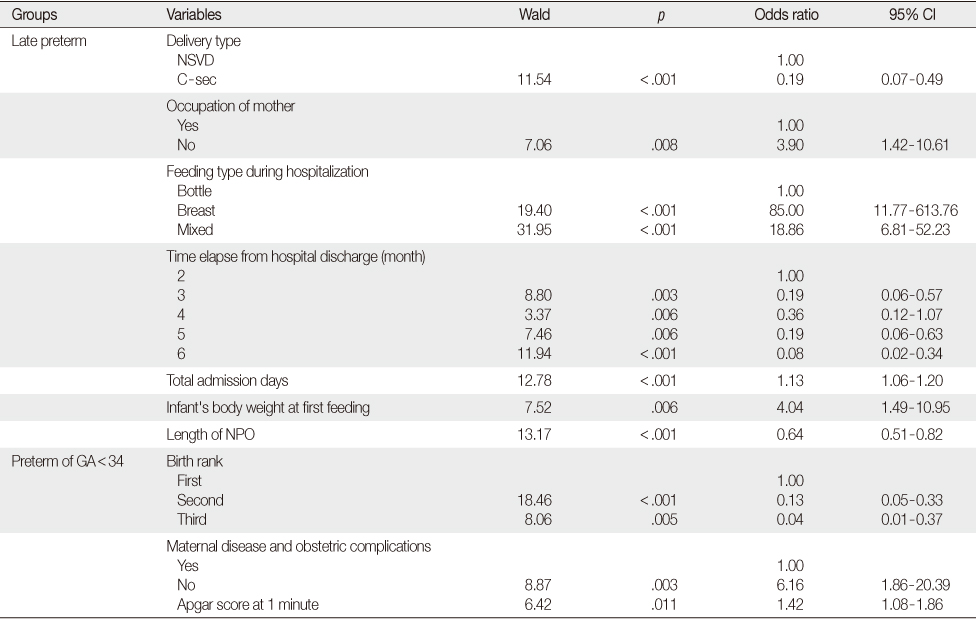
- Rate of breast feeding for late preterm infants was significantly lower than for preterm infants. There was no significant difference in breast-feeding at home. We found differences in factors influencing breast feeding between the two groups. Factors influencing feeding for late preterm infants were type of delivery, mothers' occupation, feeding type during hospitalization, time elapse from hospital discharge, total admission days, infant's body weight at first feeding and length of NPO (nothing by mouth). Factors influencing feeding for preterm infants were birth order, maternal disease and obstetric complications, and one-minute Apgar score.
-
Conclusion
- Results of the study show low rates of breast-feeding for late preterm infants indicating a need for breast-feeding education for mothers of these infants.
This work was supported by the Korea Research Foundation (KRF) grant funded by the Korea government (MEST)(2009-0070334)
- 1. Adamkin D.H. Feeding problems in the late preterm infant. Clinics in Perinatology. 2006;33:831–837. http://dx.doi.org/10.1016/j.clp.2006.09.003.ArticlePubMed
- 2. Cohen J. Statistical power analysis for the behavioral science. 1988;2nd ed. Hillsdale, NJ, Lawrence Erlbaum Associates.
- 3. Colaizy T.T., Morriss F.H. Positive effect of NICU admission on breastfeeding of preterm US infants in 2000 to 2003. Journal of Perinatology. 2008;28:505–510. http://dx.doi.org/10.1038/jp.2008.32.ArticlePubMedPDF
- 4. Engle W.A. A recommendation for the definition of "late preterm" (near-term) and the birth weight-gestational age classification system. Seminars in Perinatology. 2006;30:2–7. http://dx.doi.org/10.1053/j.semperi.2006.01.007.ArticlePubMed
- 5. Espy K.A., Senn T.E. Incidence and correlates of breast milk feeding in hospitalized preterm infants. Social Science and Medicine. 2003;57:1421–1428. http://dx.doi.org/10.1016/s0277-9536(02)00542-7.ArticlePubMed
- 6. Flacking R., Nyqvist K.H., Ewald U., Wallin L. Long-term duration of breastfeeding in Swedish low birth weight infants. Journal of Human Lactation. 2003;19:157–165. http://dx.doi.org/10.1177/0890334403252563.ArticlePubMedPDF
- 7. Howe T.H., Sheu C.F., Hinojosa J., Lin J., Holzman I.R. Multiple factors related to bottle-feeding performance in preterm infants. Nursing Research. 2007;56:307–311. http://dx.doi.org/10.1097/01.NNR.0000289498.99542.dd.ArticlePubMed
- 8. Hurst N.M., Meier P.P. Riordan J., Wambach K. Breastfeeding the preterm infant. In: Breastfeeding and human lactation. 2009;Sudbury, MA, Jones and Bartlett. 425–470.
- 9. Hwang W.J. The study on the factors determining breastfeeding rate and duration. 2004;Seoul, Yonsei University. Unpublished master's thesis.
- 10. Jacknowitz A. Increasing breastfeeding rates: Do changing demographics explain them? Women's Health Issues. 2007;17:84–92. http://dx.doi.org/10.1016/j.whi.2007.02.010.Article
- 11. Jang G.J., Kim S.H. Effects of breast-feeding education and support services on breast-feeding rates and infant's growth. Journal of Korean Academy of Nursing. 2010;40:277–286. http://dx.doi.org/10.4040/jkan.2010.40.2.277.ArticlePubMed
- 12. Jang G.J., Kim S.H., Jeong K.S. Effect of postpartum breast-feeding support by nurse on the breast-feeding prevalence. Journal of Korean Academy of Nursing. 2008;38:172–179. http://dx.doi.org/10.4040/jkan.2008.38.1.172.ArticlePubMed
- 13. Jeong G.H. Effect of the nursing intervention program on promotion the breast-feeding practice in primipara. 1997;Seoul, Ewha Womans University. Unpublished doctoral dissertation.
- 14. Kim M.J. Readmission of late preterm infants after discharge from nursery. Korean Journal of Pediatrics. 2009;52:888–892. http://dx.doi.org/10.3345/kjp.2009.52.8.888.Article
- 15. Kim M.S., Kim J.U., An Y.M., Bae S.M., Kim M.J. The research on the breast feeding and its related factors of premature infant. Korean Journal of Child Health Nursing. 2003;9:272–284.
- 16. Population projection for Korea by age (whole country). Korean Statistical Information Service. 2010;Retrieved December 30, 2010. from http://kosis.kr.
- 17. Lee C.H. Research on breast feeding pattern and related factors of premature infant's mother. 2006;Seoul, Korea University. Unpublished master's thesis.
- 18. Ludwig S.M. Oral feeding and the late preterm infant. Newborn and Infant Nursing Reviews. 2007;7:72–75. http://dx.doi.org/10.1053/j.nainr.2007.05.005.Article
- 19. Na J.Y., Park N., Kim E.S., Lee H.J., Shim G.H., Lee J.A., et al. Short-term clinical outcomes of late preterm infants. Korean Journal of Pediatrics. 2009;52:303–309. http://dx.doi.org/10.3345/kjp.2009.52.3.303.Article
- 20. Nyqvist K.H. Genna C.W. Breastfeeding preterm infants. In: Supporting sucking skills in breastfeeding infants. 2008;Sudbury, MA, Jones and Bartlett. 153–180.
- 21. Park E.Y., Cho S.J., Lee K. Current understanding and practicesof breast feeding by mothers. Korean Journal of Pediatrics. 2005;48:1162–1165.
- 22. Tomashek K.M., Shapiro-Mendoza C.K., Weiss J., Kotelchuck M., Barfield W., Evans S., et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Seminars in Perinatology. 2006;30:61–68. http://dx.doi.org/10.1053/j.semperi.2006.02.003.ArticlePubMed
- 23. Walker M. Breastfeeding the late preterm infant. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2008;37:692–701. http://dx.doi.org/10.1111/j.1552-6909.2008.00293.x.Article
- 24. Walker M. Clinics in human lactation, breastfeeding the late infant: Improving care and outcomes. 2009;Amarillo, TX, Hale.
- 25. Yeo J.H., Hong S.C. The study on the knowledge, attitude and practice rate on breast feeding. Journal of the Korean Society of Maternal and Child Health. 2003;7:155–165.
REFERENCES
Figure & Data
REFERENCES
Citations

- Role of personal aptitudes as determinants of incident morbidity, lifestyles, quality of life, use of health services, and mortality (DESVELA cohort): quantitative study protocol for a prospective cohort study in a hybrid analysis
Ruth Martí-Lluch, Bonaventura Bolíbar, Joan Llobera, José A Maderuelo-Fernández, Rosa Magallón-Botaya, Álvaro Sánchez-Pérez, Ma José Fernández-Domínguez, Emma Motrico, Enric Vicens-Pons, Blanca Notario-Pacheco, Lia Alves-Cabratosa, Rafel Ramos
Frontiers in Public Health.2023;[Epub] CrossRef - A shorter breastfeeding duration in late preterm infants than term infants during the first year
Rakel B. Jonsdottir, Helga Jonsdottir, Brynja Orlygsdottir, Renée Flacking
Acta Paediatrica.2021; 110(4): 1209. CrossRef - Upper Lip Tie: Anatomy, Effect on Breastfeeding, and Correlation With Ankyloglossia
Shalini Shah, Paul Allen, Ryan Walker, Casey Rosen‐Carole, Margo K. McKenna Benoit
The Laryngoscope.2021;[Epub] CrossRef - Effects of a Breastfeeding Support Program on the Prevalence of Exclusive Breastfeeding and Growth in Late Preterm Infants
Gun Ja Jang, Yeon Ran Hong
Child Health Nursing Research.2020; 26(1): 90. CrossRef - Breastfeeding progression in late preterm infants from birth to one month
Rakel B. Jónsdóttir, Helga Jónsdóttir, Arna Skúladóttir, Thordur Thorkelsson, Renée Flacking
Maternal & Child Nutrition.2020;[Epub] CrossRef - Factors Influencing Breast Milk Feeding in Singleton Late Preterm Infants
Su Jin Kim, Gun Ja Jang
Journal of Health Informatics and Statistics.2020; 45(4): 311. CrossRef - Ankyloglossia and Other Oral Ties
Jonathan Walsh, Margo McKenna Benoit
Otolaryngologic Clinics of North America.2019; 52(5): 795. CrossRef - Utility Evaluation of Information from YouTube on Breastfeeding for Preterm Babies
Chae-Ku Jo, Sun-Young Lee, Myo-Jing Kim
Neonatal Medicine.2019; 26(4): 185. CrossRef - Defining Tip–Frenulum Length for Ankyloglossia and Its Impact on Breastfeeding: A Prospective Cohort Study
Ryan D. Walker, Susan Messing, Casey Rosen-Carole, Margo McKenna Benoit
Breastfeeding Medicine.2018; 13(3): 204. CrossRef - Factors associated with infants receiving their mother's own breast milk on discharge from hospital in a unit where pasteurised donor human milk is available
Didier Tshamala, Anita Pelecanos, Mark W Davies
Journal of Paediatrics and Child Health.2018; 54(9): 1016. CrossRef - Neurobehavioral response to multisensory stimulation programme in high-risk neonates
Eman K. Mohamed, Faten Abdelazeim, Mohamed A. Elshafey, Nehad Nasef
Bulletin of Faculty of Physical Therapy.2018; 23(1): 22. CrossRef - Breastfeeding Continuation Among Late Preterm Infants: Barriers, Facilitators, and Any Association With NICU Admission?
Laura R. Kair, Tarah T. Colaizy
Hospital Pediatrics.2016; 6(5): 261. CrossRef - Prevalence and Predictors of Exclusive Breastfeeding in Late Preterm Infants at 12 Weeks
Soo Yeon Lee, Gun Ja Jang
Child Health Nursing Research.2016; 22(2): 79. CrossRef - Effects of Massage Therapy on Feeding Intolerance and Physical Growth in Premature Infants
Hyun Young Seo, Young Hae Kim, Sung-Ju Kim
Child Health Nursing Research.2016; 22(4): 355. CrossRef - Comparing Factors Associated with Breastfeeding in Late Preterm Infants of Different Gestational Ages
Gun Ja Jang
Child Health Nursing Research.2015; 21(4): 302. CrossRef - Allaitement maternel chez le nouveau-né prématuré à l’âge de six mois au Maroc : prévalence et facteurs associés
H. Berrani, A. Mdaghri Alaoui, J. Kasouati, K. Alaoui, A. Thimou Izgua
Archives de Pédiatrie.2015; 22(2): 141. CrossRef - Electromyography of muscles involved in feeding premature infants
Camila Dantas Martins, Renata Maria Moreira Moraes Furlan, Andréa Rodrigues Motta, Maria Cândida Ferrarez Bouzada Viana
CoDAS.2015; 27(4): 372. CrossRef - Healthy late preterm infants and supplementary artificial milk feeds: Effects on breast feeding and associated clinical parameters
Elisabet Mattsson, Eva-Lotta Funkquist, Maria Wickström, Kerstin H. Nyqvist, Helena Volgsten
Midwifery.2015; 31(4): 426. CrossRef - Comparison of breast feeding practice rates and mothers' breast feeding empowerment in preterm, late preterm and early term infants
Taeim Kim, Gunja Jang
Journal of the Korean Data and Information Science Society.2013; 24(4): 713. CrossRef - A Study on Health-related Lifestyles and Intention Toward Breast-Feeding in Korean University Students
Jo Yoon Lee, Wha Jin Hyun, Kang Wook Lee
Journal of the Korean Society of Food Culture.2013; 28(2): 125. CrossRef
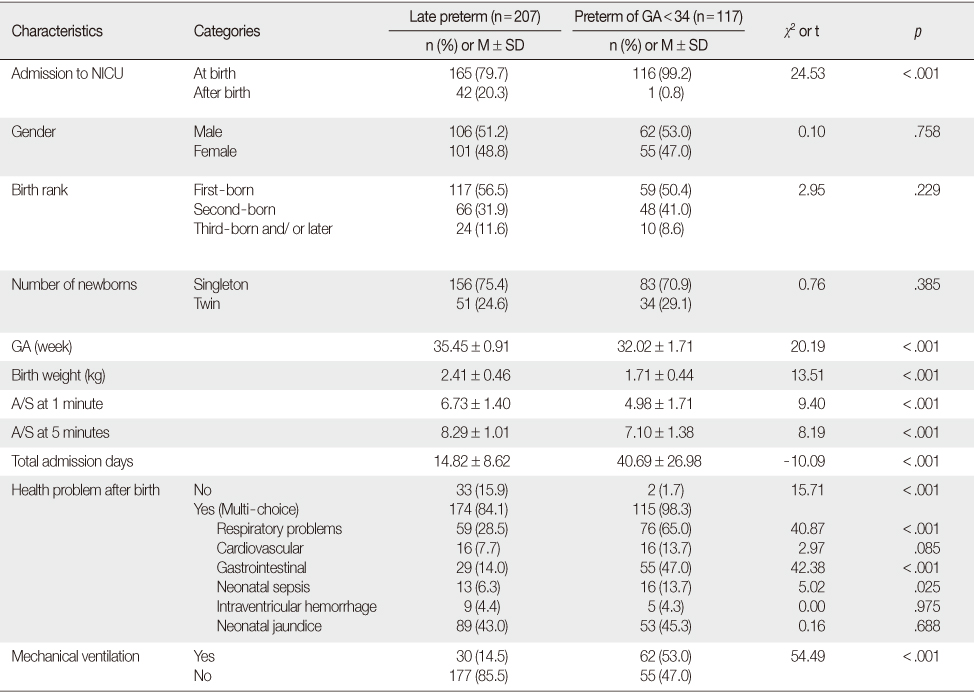
Comparison of General Characteristics between Late Preterm and Preterm Infant Group
NICU=Neonatal intensive care unit; GA=Gestational age; A/S=Apgar score.
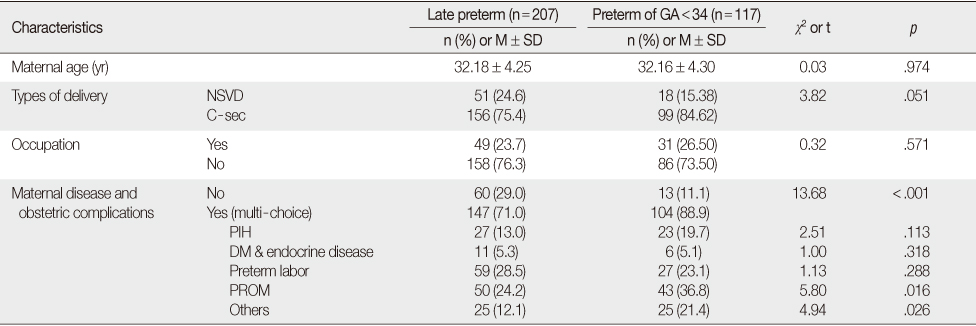
Comparison of Maternal Characteristics between Late Preterm and Preterm Infant Group
GA=Gestational age; NSVD=Normal spontaneous vaginal delivery; C-sec=Caesarean section; PIH=Pregnancy induced hypertension; DM=Diabetes mellitus; PROM=Premature rupture of membranes.
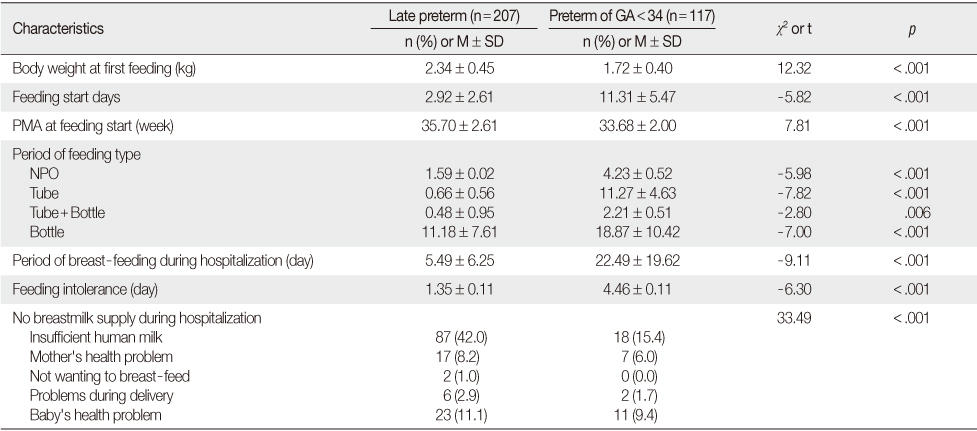
Comparison of Feeding Characteristics between Late Preterm and Preterm Infant Group
GA=Gestational age; PMA=Post menstrual age (GA+post natal age); NPO=Non per os (Nothing by mouth).
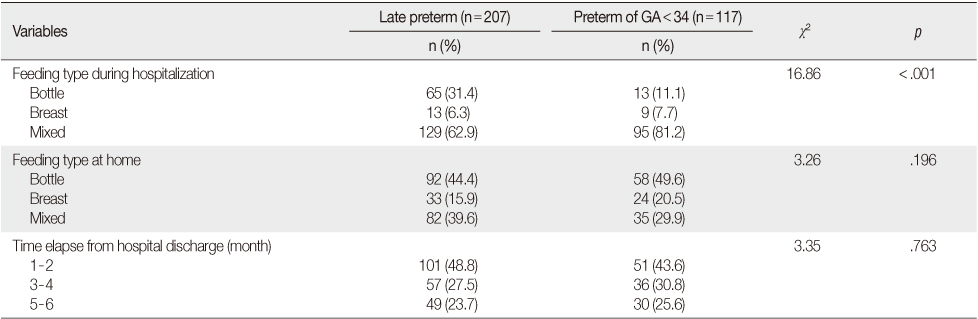
Comparison of Feeding Type between Late Preterm and Preterm Infant Group
GA=Gestational age.
Predictors related to Breast-feeding Performance in Late Preterm and Preterm Infant Group
GA=Gestational age; CI=Confidence interval; NPO=Non per os (Nothing by mouth); NSVD=Normal spontaneous vaginal delivery.
NICU=Neonatal intensive care unit; GA=Gestational age; A/S=Apgar score.
GA=Gestational age; NSVD=Normal spontaneous vaginal delivery; C-sec=Caesarean section; PIH=Pregnancy induced hypertension; DM=Diabetes mellitus; PROM=Premature rupture of membranes.
GA=Gestational age; PMA=Post menstrual age (GA+post natal age); NPO=Non per os (Nothing by mouth).
GA=Gestational age.
GA=Gestational age; CI=Confidence interval; NPO=Non per os (Nothing by mouth); NSVD=Normal spontaneous vaginal delivery.
 KSNS
KSNS
 E-SUBMISSION
E-SUBMISSION
 Cite
Cite

